Abstract
Extramammary Paget disease (EMPD) is a rare cutaneous, intraepithelial adenocarcinoma. Because of its rarity, little is known about the value of fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) in evaluating this disease. Our case report aims to increase current knowledge of FDG PET/CT in EMPD as a noninvasive imaging tool for assessing the extension of the disease and detecting distant metastases.
We reported a 64-year-old Chinese man who presented with a slowly progressive, ill-margined erythematous lesion with a crusted, eroded, and scaly surface involving multiple sites of penis, scrotum, left pelvic wall, hip, groin, and thigh for >4 years, which became extensive in the past 1 year. He was referred for an FDG PET/CT examination to further evaluate the lesions. A following skin biopsy was performed to obtain a definitive histological diagnosis.
FDG PET/CT imaging revealed mild FDG uptake at the extensive cutaneous lesion with subcutaneous invasion, involvement of lymph nodes, and multiple intense FDG-avid of skeletal metastases. According to the appearance of FDG PET/CT, a provisional diagnosis of advanced cutaneous malignancy was made. Histopathology findings indicated characteristic of EMPD. The patient was treated with radiation therapy and died from complications 2 months after the last dose of radiotherapy.
Our case highlighted that a whole-body FDG PET/CT should be incorporated into the diagnostic algorithm of EMPD to give a comprehensive assessment of this disease.
INTRODUCTION
Extramammary Paget disease (EMPD) is a rare cutaneous malignancy. The disease is often limited to the epidermis and mucosa, without invasion.1 In rare instances, EMPD is reported to become invasive, occasionally infiltrating the dermis and even be highly metastatic to the regional lymph nodes and distant sites.2,3 Factors such as dermal invasion, involvement of regional lymph node, and distant metastases are indicators of poor prognosis and closely related to the management of the disease.4 Fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) is of proved value in nodal staging and detection of distant involvement for malignant tumors. However, to our knowledge, the value of FDG PET/CT on evaluating EMPD has occasionally been reported in the literature.5–7
In this report, we describe a case of an old man with extensive invasive EMPD, in whom F-18 FDG PET/CT was valuable in assessing the extension of the disease and detecting distant metastases.
CASE REPORT
A 64-year-old Chinese man presented with a slowly progressive, ill-margined erythematous lesion with a crusted, eroded, and scaly surface involving multiple sites of penis, scrotum, left pelvic wall, hip, groin, and thigh for >4 years, which became extensive in the past 1 year (Figure 1). The obvious presenting features included pruritus and painful burning sensation. He also complained of swelling in the left thigh for >3 months and a history of muscular atrophy of disuse in the right leg due to encephalitis when he was 2 years old. He was admitted with complaints of progressive pain in shoulder, chest, and back for nearly 2 months’ duration.
FIGURE 1.

Clinical features of the patient with extensive invasive EMPD. Ill-margined infiltrative erythematous lesion with a crusted, eroded, and scaly surface is covering on the extensive sites of penis, scrotum, left pelvic wall, hip, groins, and thigh. EMPD = extramammary Paget disease.
He was referred for an F-18 FDG PET/CT imaging to further evaluate the lesions. Whole-body PET/CT imaging was performed 60 minutes after the intravenous injection of 370Mbq (10mCi) F-18 FDG and 8 hours fast using a PET/CT scanner (DiscoveryTM ST-16;General Electric Medical Systems, Milwaukee, WI, USA). The anteroposterior 3-D maximum intensity projection (Figure 2A) image demonstrated extensive and invasive abnormal FDG-avid lesions in the body. Selected coronal (Figure 2B) and transaxial (Figure 2C–M) views of CT (left column), PET (middle column), and PET/CT (right column) fusion images revealed mild FDG uptake at the extensive cutaneous lesion with subcutaneous invasion (Figure 2B–E), involvement of lymph nodes (Figure 2 F–I), and multiple intense FDG-avid of skeletal metastases (Figure 2J–M). It was highly suggestive of malignancy, and a provisional diagnosis of advanced cutaneous malignancy was made.
FIGURE 2.
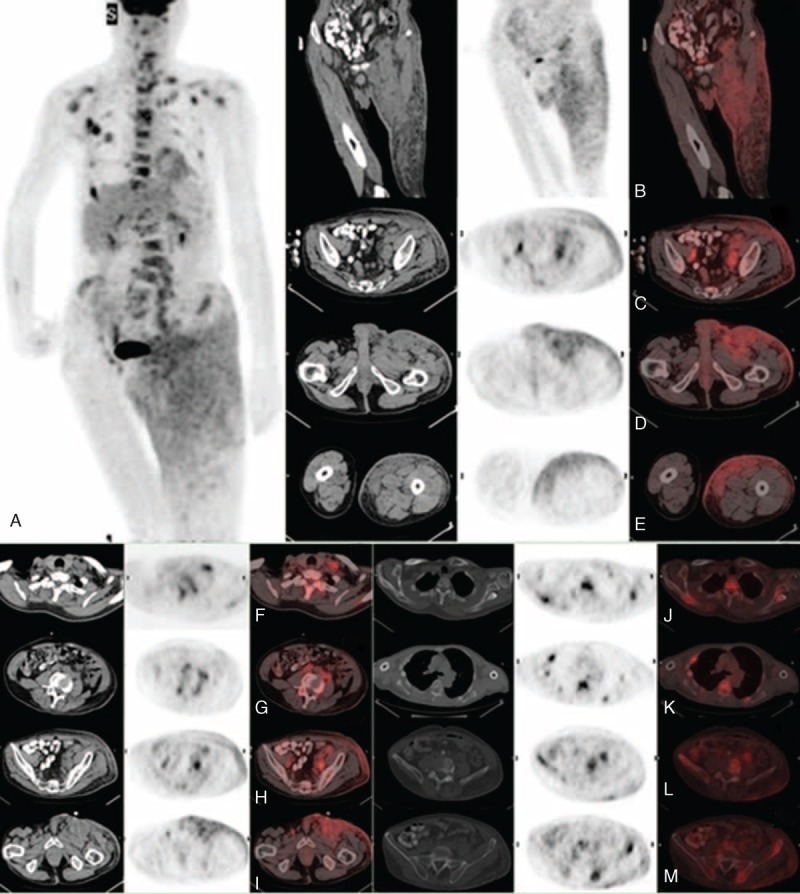
Whole-body FDT PET/CT images demonstrated the presence of multiple FDG-avid lesions in the (A) anteroposterior 3D-MIP. The selected (B) coronal and (C–M) transaxial images revealed mild FDG uptake at the extensive cutaneous lesion with (B–E) subcutaneous invasion, involvement of (F–I) regional lymph nodes, and (J–M) multiple intense FDG-avid of skeletal metastases. 3D-MIP = 3-dimensional maximum intensity projection, FDG = fluorodeoxyglucose, PET/CT = positron emission tomography/computed tomography.
These appearances of FDG PET/CT were not unique to EMPD and could also be seen in other cutaneous malignancies, even in an inflammatory or infective disease. Therefore, biopsy of the FDG-avid lesion was suggested to make a differential diagnosis. A following skin biopsy was performed to obtain a definitive histological diagnosis. Hematoxylin and eosin stain showed that the tumors were composed of cells with prominent nuclei and abundant lightly stained cytoplasm (suggesting Paget cells) (Figure 3). These pathologic findings were consistent with the EMPD.
FIGURE 3.
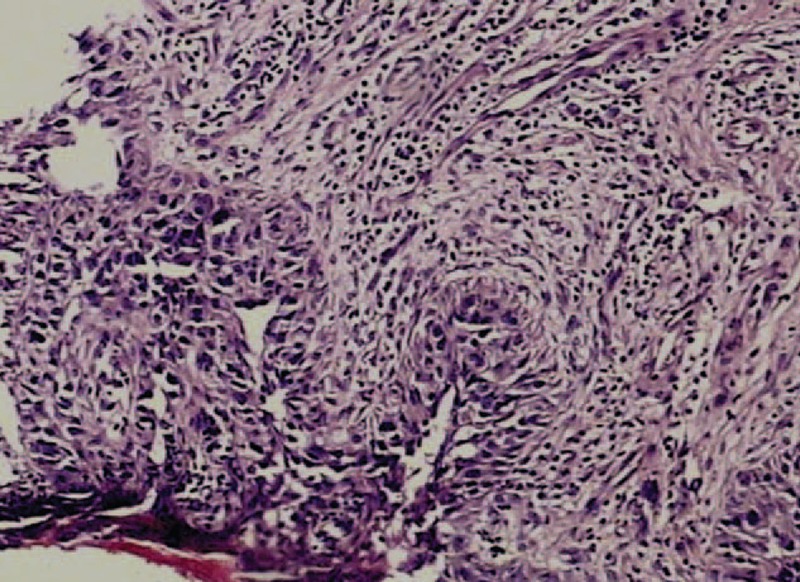
Histological assessment of EMPD. Hematoxylin and eosin stain (×200) showed that the tumors were composed of cells with prominent nuclei and abundant lightly stained cytoplasm (suggesting Paget cells). EMPD = extramammary Paget disease.
EMPD has been traditionally managed with surgery, especially in the early stage of this disease. In our case, wide local excision is not appropriate because of the advanced stage of the disease that was successfully assessed by FDG PET/CT imaging. The use of radiation therapy was considered in this case. After receiving 4 weeks of radiotherapy, the patient suffered from anemia, hypoproteinemia, and sustained high fever probably caused by systemic metastases and died from complications 2 months after the last dose of radiotherapy.
Institutional approval was given by the head of the department, and informed consent was given by the patient.
DISCUSSION
EMPD is a rare cutaneous, intraepithelial adenocarcinoma involving primarily the epidermis but occasionally extending into the underlying dermis.2 The clinical features of EMPD can be nonspecific and that misdiagnosis as an inflammatory or infective condition (eczema, psoriasis, or moniliasis) is very common. It was originally described in 1889 by Crocker,8 and it is most often observed in areas of apocrine gland-bearing, including the scrotum, penis, vulva, and perineal and perianal region. Other rare sites of involvement, such as eyelids, axilla, external auditory canal, and prostate have been reported.9,10 EMPD is often limited to the epidermis and mucosa1; however, it can also become invasive, infiltrating the dermis and even metastasizing to the regional lymph nodes and distant sites, which is also uncommon.
Factors such as dermal invasion, presence of nodules in the primary lesion, and regional lymph node involvement are indicators of poor prognosis.4 The prognosis is good when the disease is confined to the epidermis and when it does not metastasize. However, in the presence of dermal invasion, the prognosis is poor.11
Moreover, EMPD is sometimes associated with a concurrent underlying internal malignancy in nearly 20% of cases.12,13 Therefore, a thorough search for the metastatic lesions and underlying malignancy should be recommended before the treatment of EMPD.12,14,15
Whole-body F-18 FDG PET/CT has the ability to identify foci of abnormally high metabolism, and FDG PET/CT has established itself as a valuable noninvasive imaging tool for diagnosing and staging, as well as a prognostic indictor of oncological patients; however, little is known about the use of FDG PET/CT imaging in evaluation of EMPD. Although increased FDG uptake on skin can also be nonspecific, and it can mimic malignancies (cutaneous lymphoma, melanoma, and metastases from other internal malignancies), and an inflammatory or infective disease,16–21 our case indicated that FDG PET/CT is useful in evaluating EMPD by providing the extent of disease, lymph node involvement, and distant metastases, which is closely related to diagnosis, staging, management, and prognosis of this disease.
CONCLUSION
Extensive invasive EMPD is an extremely uncommon condition. Although the impact of FDG PET/CT on the staging and management of EMPD should be further evaluated, our case suggested that a whole-body FDG PET/CT should be incorporated into the diagnostic algorithm of EMPD to give a comprehensive assessment of disease and probably exclude the presence of coexisting internal malignancy.
Footnotes
Abbreviations: EMPD = extramammary Paget disease, FDG = fluorodeoxyglucose, PET/CT = positron emission tomography/computed tomography.
REFERENCES
- 1.Onaiwu CO, Ramirez PT, Kamat A, et al. Invasive extramammary Paget's disease of the bladder diagnosed 18 years after noninvasive extramammary Paget's disease of the vulva. Gynecol Oncol Case Rep 2014; 8:27–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ekwueme KC, Zakhour HD, Parr NJ. Extramammary Paget's disease of the penis: a case report and review of the literature. J Med Case Rep 2009; 3:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reddy IS, Swain M, Gowrishankar S, et al. Primary extramammary Paget's disease with extensive skeletal metastases. Indian J Dermatol Venereol 2012; 78:89–92. [DOI] [PubMed] [Google Scholar]
- 4.Cappucini F, Tewari K, Rogers LW, et al. Extramammary Paget's disease of the vulva: metastases to the bone marrow in the absence of an underlying adenocarcinoma—case report and literature review. Gynecol Oncol 1997; 66:146–150. [DOI] [PubMed] [Google Scholar]
- 5.Aoyagi S, Sato-Matsumura KC, Shimizu H. Staging and assessment of lymph node involvement by 18F-fluorodeoxyglucose-positron emission tomography in invasive extramammary Paget's disease. Dermatol Surg 2005; 31:595–598. [DOI] [PubMed] [Google Scholar]
- 6.Niederkohr RD, Gambhir SS. F-18 FDG PET/CT imaging of extramammary Paget disease of the perianal region. Clin Nucl Med 2006; 31:561–563. [DOI] [PubMed] [Google Scholar]
- 7.Cho SB, Yum M, Lee MG, et al. Variable patterns of positron emission tomography in the assessment of patients with extramammary Paget's disease. J Am Acad Dermatol 2005; 52:353–355. [DOI] [PubMed] [Google Scholar]
- 8.Crocker HR. Paget's disease affecting the scrotum and penis. Trans Pathol Soc Lond 1889; 40:187–191. [Google Scholar]
- 9.Lloyd J, Flanagan AM. Mammary and extramammary Paget's disease. J Clin Pathol 2000; 53:742–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yadav AK, Gupta R, Singh UR. Extramammary Paget's disease in prostate. Urol J 2009; 6:303–305. [PubMed] [Google Scholar]
- 11.Zhu Y, Ye DW, Chen ZW, et al. Frozen section-guided wide local excision in the treatment of penoscrotal extramammary Paget's disease. BJU Int 2007; 100:1282–1287. [DOI] [PubMed] [Google Scholar]
- 12.Chanda JJ. Extramammary Paget's disease: prognosis and relationship to internal malignancy. J Am Acad Dermatol 1985; 13:1009–1014. [DOI] [PubMed] [Google Scholar]
- 13.Kanitakis J. Mammary and extramammary Paget's disease. J Eur Acad Dermatol Venereol 2007; 21:581–590. [DOI] [PubMed] [Google Scholar]
- 14.Pang J, Assaad D, Breen D, et al. Extramammary Paget disease: review of patients seen in a non-melanoma skin cancer clinic. Curr Oncol 2010; 17:43–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Siesling S, Elferink MA, van Dijck JA, et al. Epidemiology and treatment of extramammary Paget disease in the Netherlands. Eur J Surg Oncol 2007; 33:951–955. [DOI] [PubMed] [Google Scholar]
- 16.Blumer SL, Scalcione LR, Ring BN, et al. Cutaneous and subcutaneous imaging on FDG-PET: benign and malignant findings. Clin Nucl Med 2009; 34:675–683. [DOI] [PubMed] [Google Scholar]
- 17.Kumar R, Xiu Y, Zhuang HM, et al. 18F-fluorodeoxyglucose-positron emission tomography in evaluation of primary cutaneous lymphoma. Br J Dermatol 2006; 155:357–363. [DOI] [PubMed] [Google Scholar]
- 18.Li Y, Berenji GR. Cutaneous sarcoidosis evaluated by FDG PET. Clin Nucl Med 2011; 36:584–586. [DOI] [PubMed] [Google Scholar]
- 19.Joyce JM, Carlos T. Herpes Zoster mimicking recurrence of lymphoma on PET/CT. Clin Nucl Med 2006; 31:104–105. [DOI] [PubMed] [Google Scholar]
- 20.Borkar S, Pandit-Taskar N. F-18 FDG uptake in cutaneous metastases from breast cancer. Clin Nucl Med 2008; 33:488–489. [DOI] [PubMed] [Google Scholar]
- 21.Egan C, Silverman E. Increased FDG uptake along dermatome on PET in a patient with herpes zoster. Clin Nucl Med 2013; 38:744–745. [DOI] [PubMed] [Google Scholar]


