Abstract
Strong primary care is in urgent need for the management and control of hypertension. This study aimed to compare the quality of hypertensive care delivered by community health centers (CHCs) in Shanghai and Shenzhen.
Multistage random sampling method was used to select 4 CHCs in each city as study settings. A cohort of hypertensive patients under the hypertensive management program in the CHCs was selected from the electronic information system by using a systematic random sampling method. Binary logistic regression models were constructed for comparison between the 2 cities.
A total of 3196 patients’ records were assessed. The proportions of hypertensive patients who received advice on smoking cessation (33.8 vs 7.7%, P < 0.001), increasing physical activity (52.4 vs 16.8%, P < 0.001), low-sodium diet (72.0 vs 64.1%, P < 0.001), and regular follow-up (37.8 vs 8.6%, P < 0.001) were higher in Shenzhen than in Shanghai. However, the drug treatment rate in Shenzhen was lower than that in Shanghai (74.2 vs 95.2%, P < 0.001). The hypertension control rate in Shenzhen was lower than that in Shanghai (76.3 vs 83.2%, P < 0.001). Better performance in the process of hypertensive care in terms of increasing physical activity advice, low-sodium diet advice, regular follow-up, and drug prescription was associated with a higher rate of hypertension control.
The study indicates that primary care is effective in managing hypertension irrespective of management and operation models of CHCs in urban China. Our study suggests that improvements in the process of hypertensive care may lead to better hypertension control.
INTRODUCTION
Hypertension is an important public health issue faced by policymakers in China. The prevalence of hypertension has increased sharply in the Chinese population, reaching a rate of 34% in 2010.1 Hypertension is the biggest contributor to cardiovascular diseases such as stroke and coronary heart diseases.2,3 It is estimated that about 50% of deaths in the Chinese population are attributable to prehypertension and hypertension.4 With the complexity of hypertension and the frequent involvement of >1 care provider and institution underlie the importance of primary care.5,6 The 2008 World Health Organization report clearly affirmed the central role of primary care in coping with the challenges arising from chronic diseases like hypertension.7
In urban China, community health centers (CHCs) are major primary care providers. Chronic disease management is designed to be 1 of the 6 integrated health services provided by CHCs. According to hypertension management guidelines, CHCs should establish health records for hypertensive patients.8 Patients are classified into different management groups, based on their blood pressure (BP) levels and coexisting cardiovascular risk factors. Patients need to be monitored regularly on the basis of their category of disease profiles. Lifestyle modification should be proposed to all hypertensive patients, whereas drug treatment is usually initiated in patients with persistent, suboptimally controlled BP (ie, ≥140/90 mm Hg). Through this strategy, it is hoped to minimize the adverse effects of hypertension.
Due to the socioeconomic variations in different urban regions, the local implementation of community-based primary care has led to the emergence of the 2 major models of CHCs, that is, government-managed CHCs (G-CHCs) and hospital-managed CHCs (H-CHCs), together accounting for about 86% of all CHCs. Shanghai and Shenzhen are 2 top-tier economically developed metropolitan cities in China, and also leaders in primary care development. CHCs in Shanghai are government-managed, which are independent entities from the public hospitals, and funded fully and managed directly by the government, whereas the CHCs in Shenzhen are hospital-managed, being established and managed directly by public hospitals as a department (Box 1).
Box 1.
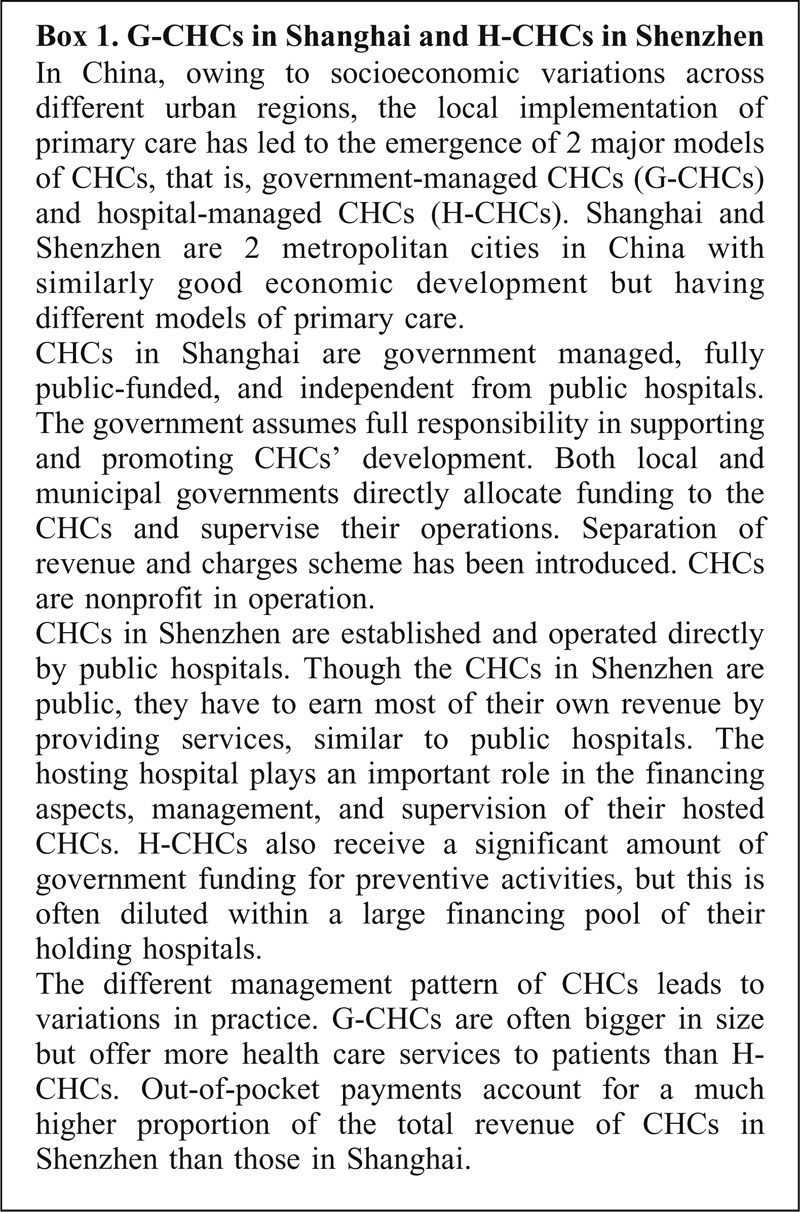
no caption available.
International studies have examined different segments of hypertensive care, including initial screening, diagnosis, treatment, case follow-up, and BP control.9–11 However, in China, most of the existing literature that assesses the quality of hypertension care covers only BP control. To the best of our knowledge, there are few studies that investigated the contribution of regular follow-up, pharmacological, and nonpharmacological therapies in the management of hypertension.12,13 Part of the rationale is the weak evidence for improvement in the quality of hypertensive care. Using comprehensive quality indicators, this study aimed to compare the quality of hypertensive care between CHCs in Shanghai and Shenzhen that covering both process and outcome indicators. A quality comparison between different primary care implementations in different local contexts—Shanghai and Shenzhen, which are leading sites of primary care development in China—can provide valuable feedbacks, which other cities can use as benchmarks to assess their own quality of hypertension management.
METHODS
Study Settings
This is a cohort study conducted in Shanghai and Shenzhen. Employing multistage random sampling methods, we chose CHCs as study settings. In each city, 4 urban districts were first randomly selected in each geographical part of the city, that is, Jing’an, Changning, Xuhui, and Pudong in Shanghai, and Futian, Luohu, Bao’an, and Longgang in Shenzhen. In the second stage, we selected 1 CHC in each randomly drawn district by simple random sampling. In total, 8 CHCs were selected.
Data Sources
We used data from the electronic information system, which is a large database of routine hypertensive patient management records. Hypertensive patients managed by CHCs were either detected by health examinations or during outpatient consultations. Patients under management were assigned into different management categories based on their BP levels and risk factor profile. Lifestyle consultations and drug treatments were initiated when appropriate. Follow-up was conducted through patients’ CHC visits, or home visits by CHC staff when the patient did not show up in CHCs. In each individual follow-up, information on drug prescriptions, lifestyle modifications, and BP values were input into the information system by primary care providers as part of routine practice. BP was measured by mercury sphygmomanometers according to the protocol recommended by the national guidelines for hypertension management. The database also contains records of patient characteristics such as sex, age, height, weight, and smoking status. The data provided a longitudinal record of hypertensive patients’ management with information on the process of service delivery and intermediate outcomes (ie, BP control) of care. It documented the hypertension management system under which hypertensive care was delivered in the real world setting. Thus, the implications were such that any measurement of variation in performance illustrated via quality indicators was more likely to be attributable to the health care provider or system of care.
Subjects
The study period was between January 2010 and December 2011. The target population consisted of all registered patients aged ≥18 years old and with confirmed diagnosis of hypertension. With a proportion difference of (25.0%–20.0%) for hypertension control rate,13 we estimated that a minimum sample size of 1504 in each city was needed to generate a 95% confidence interval (CI) and 90% statistical power. We then aimed to obtain 400 patients from each CHC for the current study. We excluded patients who had passed away or moved out of the catchment area of the CHCs.
Data Collection
Employing a systematic sampling method, we selected participants from all the eligible hypertensive patients with a random start. Using a computerized abstraction form, trained abstractors commenced data extraction from the electronic information system. Data included all BP measurements performed between January 2010 and December 2011, all drugs prescribed, dates on which follow-up was conducted, and initiatives on lifestyle modification. In addition, patient information was collected, including sex, age, height, weight, complications (including cerebrovascular disease, heart disease, and kidney disease), family history (ie, hypertension, diabetes, stroke, coronary heart disease), smoking status, alcohol drinking, and exercising habits. The collected data were recorded in such a manner that the corresponding patients could not be identified.
Quality of Care Indicators for Hypertension
We assessed the quality of hypertension management by obtaining the recorded results on 7 indicators, including 6 care process indicators and 1 intermediate outcome indicator. The indicators were selected on the basis of a review of scientific literature, availability of data from hypertension management records, and indicators suggested by guidelines from various countries.2,14–17 The process indicators included patient counseling for nonpharmacological hypertension management (indicators 1–4, covering the importance of lifestyle modification in the management of hypertension), drug treatment (indicator 5, referring to the prescription of at least 1 medication during the study period), and intensity of follow-up (indicator 6, reflecting the importance of regular monitoring of hypertensive patients to control the disease). The outcome indicator (indicator 7) was the hypertension control (Box 2).
Box 2.

no caption available.
The records under assessment covered a period of 12 months, which began from the date of the first coding in 2010. Performance relating to each care process indicator was determined by a patient's eligibility for an indicator and whether he/she received the indicated care. We considered that the patient had received the indicated care if the patient was recommended advice on smoking cessation, alcohol intake reduction, increasing physical activity, and low-sodium diet, and prescribed antihypertensive drugs at any individual follow-up during the study period. According to the national guidelines for hypertension management, the patient should be followed-up at least 4 times in a period of 12 months with the interval of any 2 consecutive follow-ups not exceeding 3 months. Hypertension control rate was calculated as the proportion of all patients with BP <140/90 mm Hg for those aged <65-year, whereas with BP <150/90 mm Hg for those aged ≥65-year. For each patient, we used the BP values coded in the latest follow-up visit during the study period to measure BP control.
Statistical Analysis
The missing values were <3% for all variables. Because removal of missing values from analysis resulted in a loss of information, we used mode theory to replace the missing values for categorical variables, whereas filled means for the continuous variables. We first used the χ2 tests to compare the differences in the process and outcome quality of hypertensive care between the 2 cities. Then binary logistic regression models were constructed to compare indicators between the 2 cities after controlling for all patient characteristics including sex, age, body mass index (BMI), complications, family history, smoking status, alcohol drinking, and exercising habits. To evaluate the association of process indicators with BP control, we developed binary logistic regression models with all patient characteristics (the same as those above), all care process indicators (ie, advice on smoking cessation, alcohol intake reduction, increasing physical activity, low-sodium, regular follow-up, drug treatment), as well as the city (ie Shanghai vs Shenzhen) as covariates. For all tests conducted in the study, a P value of <0.05 was adopted as the statistically significant level. All analyses were performed using SPSS19.0 (international business machines Corporation, New York, USA).
Ethical Approval
Ethical approval was obtained from the Joint Chinese University of Hong Kong and New Territories East Cluster Clinical Research Ethics Committee (Ref. no. clinical research ethics-2010.441).
RESULTS
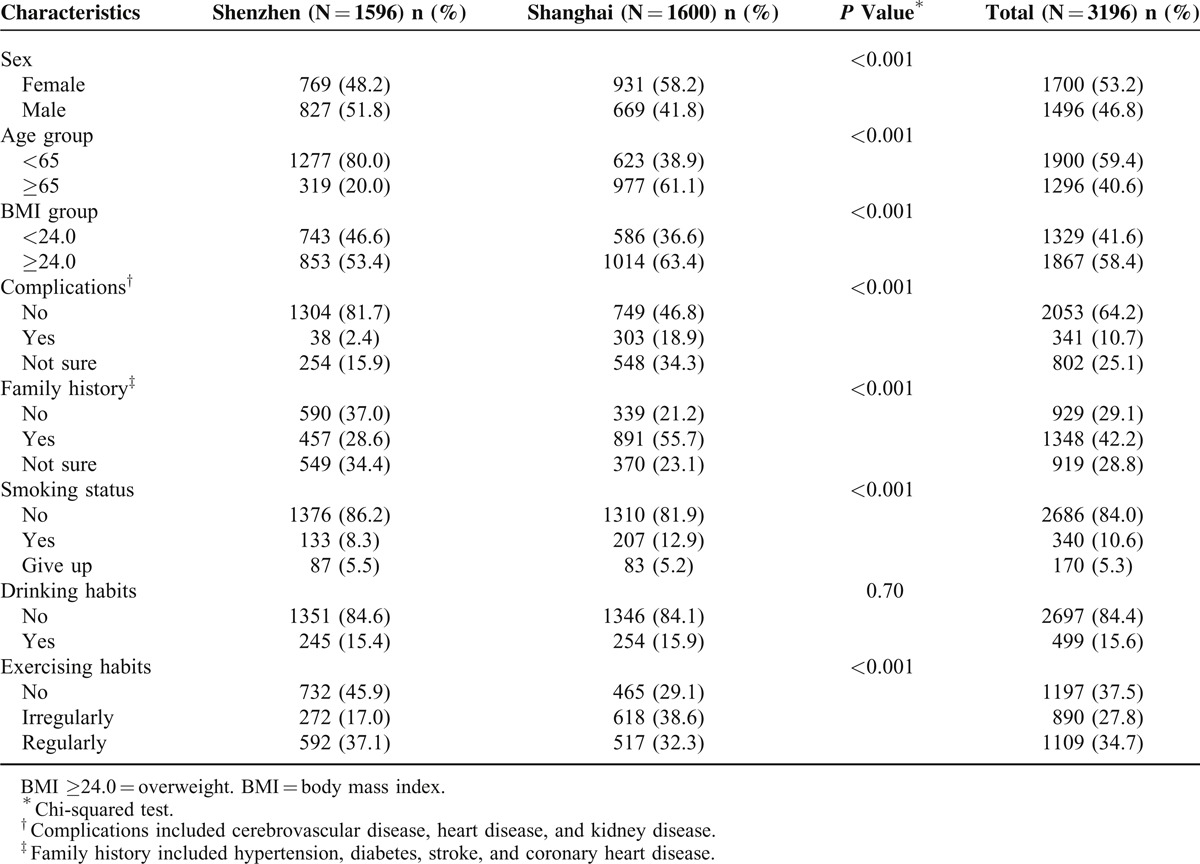
A total of 3196 patients’ records were assessed, with 1596 from Shenzhen and 1600 from Shanghai. A higher proportion was female (53.2%), and the majority was aged 65 years or younger (59.4%). More than half of the patients were overweight (58.4%) and did not have any complications due to hypertension (64.2%). Approximately 42.2% patients had a family history of hypertension and related diseases (namely diabetes, stroke, and coronary heart disease). Most of the patients were nonsmokers (84.0%) and nondrinkers (84.4%). Around one-third (34.7%) did exercise regularly. There was significant heterogeneity between the 2 cities in terms of all patient characteristics except for alcohol drinking habits. (Table 1)
Table 1.
Characteristics of Hypertensive Patients
After adjusting for patient characteristics, patients from Shenzhen were more likely to receive advice on smoking cessation (7.7 vs 33.8%, P < 0.001), increasing physical activity (16.8 vs 52.4%, P < 0.001), low-sodium diet (64.1 vs 72.0%, P < 0.001), and regular follow-up (8.6 vs 37.8%, P < 0.001), whereas less likely to receive drug prescriptions (95.2 vs 74.2%, P < 0.001) when compared with those from Shanghai. The hypertension control rate was not significantly different between the 2 cities (83.2 vs 76.3%) (Table 2). However, when care process indicators (including advice on smoking cessation, alcohol intake reduction, increasing physical activity, low-sodium, regular follow-up, and drug treatment) were also included in the multiple regression models, it was found that the hypertension control rate was higher in Shanghai than in Shenzhen (odds ratio 1.711, 95% CI 1.311–2.235) (Table 3). Subgroup analyses with hypertensive patients being stratified by age (ie, 65-year as the cut-off) showed similar findings (data not shown).
Table 2.
Process and Outcome Quality of Primary Care for Hypertensive Patients by City
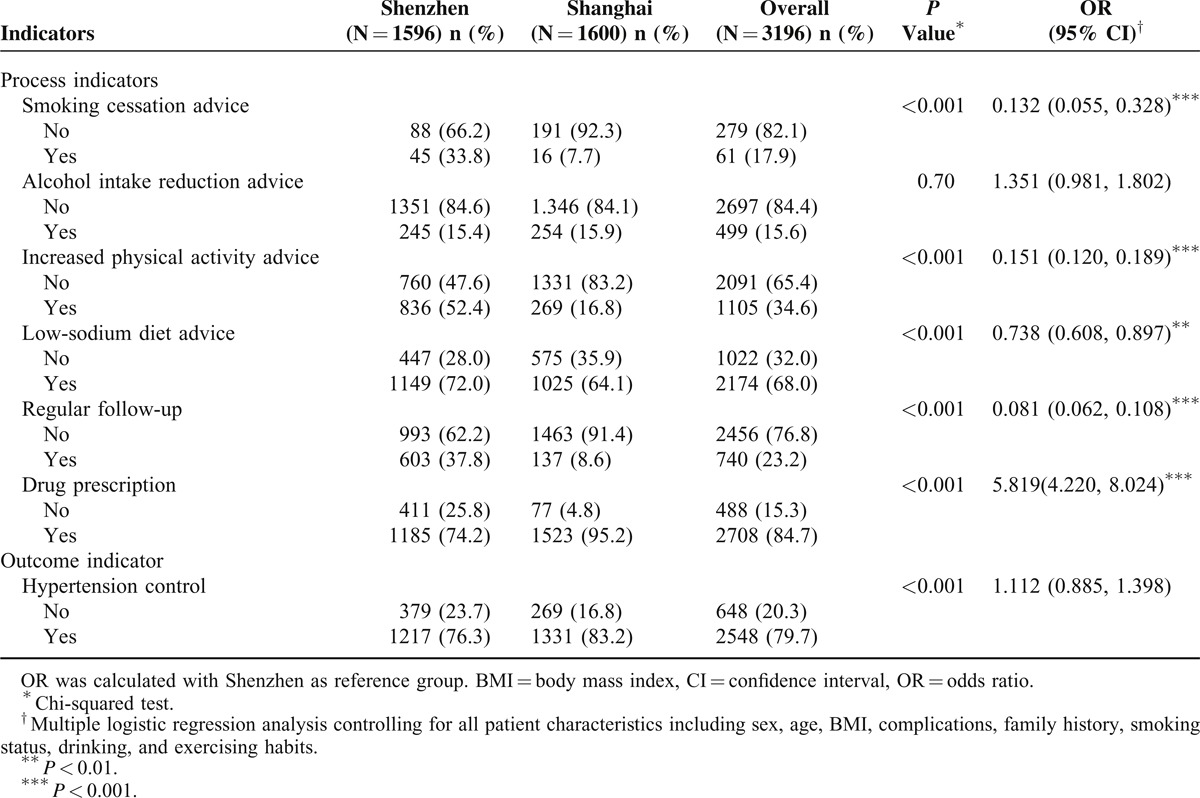
Table 3.
Multiple Logistic Regression Analysis of Factors Associated With BP Control
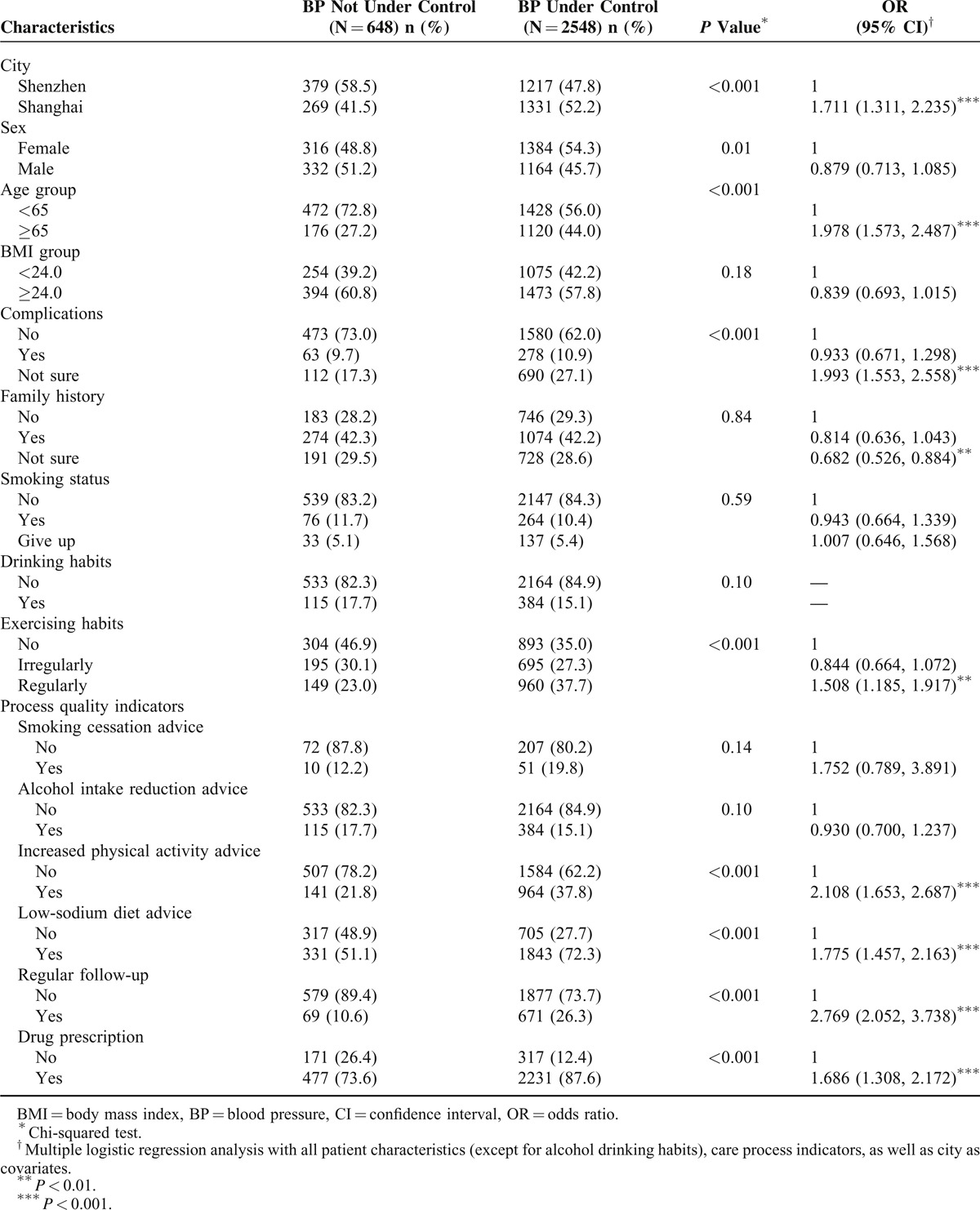
The subjects whose BP was under control were more likely to have received advice on increasing physical activity (21.8 vs 37.8%, P < 0.001), low-sodium diet (51.1 vs 72.3%, P < 0.001), drug prescriptions (73.6 vs 87.6%, P < 0.01), and regular follow-up (10.6 vs 26.3%, P < 0.001) than those whose BP was not under control (Table 3). After adjustments were made for patient characteristics and the study location, these significant differences still remained.
DISCUSSION
Our study found that the proportions of hypertensive patients who received advice on smoking cessation, increasing physical activity, low-sodium diet, and regular follow-up were higher in Shenzhen than in Shanghai. However, the drug treatment rate in Shenzhen was lower than that in Shanghai. The hypertension control rate in Shanghai was higher than that in Shenzhen when care process indicators were controlled in multiple regression models, although separate regression analysis without controlling care process indicators as covariates showed no significant difference between the 2 cities. It was indicated that better performance in the hypertensive care process, as assessed by process quality indicators, was associated with better BP control.
The higher nonpharmacological treatment rate and the more frequent follow-up of hypertensive patients in Shenzhen than that in Shanghai might be due to the heavier workload encountered by doctors in Shanghai than those in Shenzhen. Previous studies have found that lack of consultation time might impair the ability of health care providers to follow guidelines.18 In both cities, CHC doctors are responsible for provision of both medical and public health services. Although there are usually more doctors in CHCs in Shanghai than in Shenzhen, the workload of doctors in Shanghai is usually heavier than that in Shenzhen.19 Consequently, the time spared to each hypertensive patient is limited, and regular services such as smoking cessation advice and counseling on physical activity might be neglected in Shanghai.
Patients received more antihypertensive drugs in Shanghai compared with those in Shenzhen, which is possibly due to the higher availability of these drugs in Shanghai. The Essential Medicines Scheme has been implemented in both cities that CHCs have to prescribe drugs only within the list of essential medicine. The local government can make an adjustment of the list by adding more medicines. We found that >40 types of antihypertensive drugs were available in Shanghai's CHCs, whereas only 8 in Shenzhen's CHCs. This may reflect that Shanghai has more aging population so that the local essential medicine list contains more antihypertensive drugs.
Different health insurance schemes might be another health system factor contributing to the differences in the drug treatment rate between the 2 cities. Previous studies have shown that insurance is associated with improved hypertension treatment and medication adherence.20 In Shanghai, health insurance coverage was almost universal among CHC users, but it was only about 60% in Shenzhen. Furthermore, it was reported that increased copayments were associated with reduced antihypertensive drug treatments and adherence to medications. In Shenzhen, there is reimbursement constraint for those under Medical Insurance Scheme for Migrant employees. The patients covered by this scheme could get a maximum total reimbursement amount of Ren Min Bi 800 per year, which might result in patients seeking health care primarily for acute problems.21
Beliefs about consequences of taking antihypertensive drugs by patients and health care providers might also be 1 possible explanation of this observation. Our study found that patients in Shenzhen were younger and less likely to have complications than those in Shanghai. CHC doctors might perceive that their BP is more manageable through lifestyle modification initiatives when pharmacological therapy is not perceived as a “given.”13 On the other hand, patients are also reluctant or unwilling to commence antihypertensives when their BP is marginal and clinically asymptomatic.22,23 Additionally, in Shenzhen, the reported discrimination by health care providers against migrants might influence acceptability of medicines.24
The higher BP control rate in Shanghai than in Shenzhen might be due to the higher drug treatment rate in Shanghai than that in Shenzhen. Previous studies found that drug treatment rate is better among elderly patients, which usually translate into better control of BP.25 Our study found that about 76% of patients from Shanghai were >60 years old with the rest being older than 45-year. However, in Shenzhen, more than two-thirds of patients were younger than 60 years with about half of them being younger than 44 years. It should be noted that the significant difference in the BP control rate between the 2 cites was eliminated when care process indicators (including advice on smoking cessation, alcohol intake reduction, increasing physical activity, low-sodium, regular follow-up, and drug treatment) were removed from multiple regression models. This suggests that the process of hypertensive care delivery may have a direct impact on BP control. Because the distribution of process indicators was different among the participants from the 2 cities, the estimates of BP control rates differed between multiple regression analysis results with and without controlling these variables.
One interesting finding was that the BP control rate was only about 7% higher in Shanghai than in Shenzhen, whereas drug treatment rate in Shanghai was about 21% higher than that in Shenzhen. This is possibly because the patients in Shenzhen are young; they may have transiently elevated BP at an earlier occasion, which may have spontaneously returned to normal. In addition, they may change to a healthier lifestyle, resulting in the detection of achieved BP target in the absence of drug therapy. On other hand, patients in Shanghai tended to be older and having comorbidities, resulting in difficulties in achieving the target BP level attributed to reasons like poor adherence to drug treatments.
The current literature showed mixed views regarding the relationship between the management pattern of CHCs and hypertension control. A study in 29 cities across China showed that hypertension control rate was similar among the 3 models of CHCs, that is, G-CHCs, H-CHCs, and privately owned CHCs.26 However, the study conducted in Guangdong province pointed out that hypertension control rate was the highest among privately owned CHCs, followed by H-CHCs and then G-CHCs.27 Another study identified that government-funded CHC in Guangdong was more likely to have optimal BP control, whereas privately funded CHC was less likely to achieve BP control, irrespective of whether antihypertensive drugs were prescribed.13 The conflicting findings among different studies regarding the relationship between management pattern of CHCs and BP control might suggest that the performance of CHCs depends more on the process of hypertension management rather than the ownership of providers.
Results showed that the drug treatment rate of registered hypertensive patients was higher than that of hypertensive patients recruited from general population, whereas there were significant gaps between standards of care and medical practice in terms of nonpharmacological treatment and regular follow-up of hypertension. We found that about 85% of hypertensive patients received pharmacotherapy, which is similar to the rate reported by Wong et al13 (75%), whose study was conducted with registered hypertensive patients in the Pearl River Delta region of China.13 Our figure is much higher than that of hypertensive patients recruited from general population, among whom the drug treatment rate is <50%.28–31 In other words, the registered hypertensive patients have access to appropriate pharmacological treatment.30 However, results showed that only about 23% of hypertensive patients received regular follow-ups. The perceived impractical features of the guidelines for management of hypertension may be 1 possible explanation of this finding.32 Our figure is much lower than that reported by Asch et al9 and Saxena et al.33 The possible reason is that the follow-up interval used in our study is shorter than the ones used in other studies. In addition, our study demonstrated that nonpharmacological treatment of hypertension was documented for only a few of hypertensive patients. Shortage of staff 34 and insufficient financial incentives23 might act as barriers to health care providers to follow the guidelines. The observations of our study supported the notion that good hypertension management guidelines often do not translate into their use in practice, although they are available to all CHCs in both cities.35
Findings indicated that hypertension control rate in registered hypertensive patients was higher than that in hypertensive patients recruited from general population, which suggests that management of hypertension at primary care settings achieves better BP control in China. We found that about 80% of hypertensive patients had their BP under control. Our observation is consistent with a study conducted among registered hypertensive patients in 29 cities across China in 2007, which showed that the BP control rate was 74%.26 Our figure is also similar to that reported by a British study, which showed that the BPs of about 69% of registered hypertensive patients were under control.11 However, our figure is much higher than that among hypertensive patients recruited from general population. The 2002 National Hypertension Survey in China showed that 23% patients with hypertension were aware of it, 17% were on treatment, and only 4% had their BP under control.36 Another study used data from the China Health and Retirement Longitudinal Study of Chinese people aged 45 years or older, showed that >40% of the individuals found to have hypertension were unaware that they were hypertensive, more than half were not receiving any form of antihypertensive medication, and <20% were controlling their hypertension well,30 whereas the awareness, treatment, and control rates of hypertension in more developed countries were much higher than that in China. A study by Guo et al37 with a nationally representative sample of the noninstitutionalized US population (National Health and Nutrition Examination Survey) reported that in the study period 2009 to 2010, hypertension awareness and treatment rates were 81% and 74%, whereas control rate was 53%. In Canada, approximately 83% patients with hypertension were aware of it with 80% and 66% being treated and controlled, respectively.38 Given that hypertension can be controlled at low cost, there is no good reason why hypertension in China cannot be managed as well as hypertension in other, more developed countries. Studies have found that the individuals who know they are hypertensive have access to appropriate treatment, and many of the registered individuals who are receiving antihypertensive drugs appear to be under effective control.30 Therefore, our study suggests that the big difference in terms of hypertension control between registered hypertensive patients and general population is the extent of awareness and treatment. As community-based primary care becomes increasingly available and affordable in China,39 the effective management of hypertension largely becomes a case identification problem, as well as a participation problem in China.
Patients with controlled BP received more of the indicated process care than did patients with uncontrolled BP, suggesting a relationship between process and outcome of hypertensive care. Previous studies have also indicated the positive relationship between control of BP and lifestyle modifications, drug prescription, and regular follow-up.9,40 Linking process and outcome are an important goal of quality of care assessment.40 Such linkages imply that the process measures truly capture the quality of care and that as a result, changes in performance may be expected to improve outcomes.41 However, the cross-sectional nature of these studies, including the current one, warrant further investigations to establish the causal inferences between process and outcome of hypertensive care.
Studies have documented the advantages of the use of indicators to provide feedback for quality improvement initiatives and regulation.42 The recent health care reform plan in China reaffirmed the key role of primary care in managing chronic diseases, and consequently a strong primary care is urgently needed.43 Our study may help policymakers to formulate quality improvement programs most likely to improve BP control and avoid adverse outcomes.44 For CHCs in both cities, passive dissemination of hypertension management guidelines rarely induces the expected changes in doctors’ behavior. Policymakers need to engage in active programs to educate and promote changes in doctors’ behavior. Previous studies suggested that assessment of hypertension management might be an effective approach of such a strategy.45 Moreover, doctor's workload should be appropriate for quality hypertensive care provision. The staffing standards of a CHC need to be updated according to the total designed 6 integrated health services delivered by the CHC. Furthermore, drug availability should be enhanced. Studies showed that patient determinants were highly relevant to the pharmacological treatment of hypertension.46 Therefore, we need to determine the types of antihypertensive drugs provided by CHCs not only depending on health professionals’ opinions, but also considering the drug-taking habits of patients, as well as their preferences.
The limitations of this study should be addressed. First, the representativeness of the CHCs might be limited, because only 8 CHCs were chosen as study settings. To make the results more representative, we used random sampling methods to select CHCs. Secondly, caution should be taken when applying the results at city level because only 4 CHCs were selected in each city. Additionally, we did not include hypertensive patients not under the CHC management. Thirdly, the information system did not contain information on insurance, household income, education, and employment status, which are potential confounders influencing service delivery and outcome measures. Thus, no adjustment for these factors is possible. In addition, the lack of information on the duration of hypertension and severity of complications might introduce case-mix bias. Besides, unavailability of the information on the etiology of hypertension (ie, primary or secondary hypertension) made it impossible to perform stratification analysis based on classification of hypertension. Fourth, due to unavailability of the information on whether or not the patients were diabetic, we did not include the target BP for patients with diabetes (<130/80 mm Hg) as suggested by some guidelines.47 This may result in an overestimated BP control rate in both cities especially in Shanghai.
CONCLUSIONS
In conclusion, community-based primary care is shown to be effective in managing hypertension, although primary care facilities (ie, CHCs) are in different management and operation models. Our study suggests that improvements in the process of hypertensive care including physical activity advice, low-sodium diet advice, regular follow-up, and drug prescription may lead to better BP control, whereas care process can be improved through enlarged health insurance coverage, reduced copayments, as well as increased supply of doctors and antihypertensive drugs.
ACKNOWLEDGMENTS
The study was supported by the Research Grants Council of Hong Kong (4002 SPPR 10). The authors would also wish to thank the study participants for their contribution to the research, especially the faculty members and students from the Chinese University of Hong Kong and Shanghai Jiao Tong University for their work in data collection. We are also grateful to the Health Authorities of Shanghai and Shenzhen and their Associations of Primary Care for their coordination assistance. We appreciate the Research Grants Council of Hong Kong for providing funding to conduct the study.
Footnotes
Abbreviations: BMI = body mass index, BP = blood pressure, CHC = community health center, CI = confidence interval, G-CHC = government-managed community health center, H-CHC = hospital-managed community health center.
This work was supported by the Research Grants Council of Hong Kong (grant number 4002 strategic public policy research (SPPR) 10). However, the funding body had no role in research design, data collection, interpretation of the data, and writing or submitting the manuscript.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Jimenez Villa J. Evaluation needs the population perspective. Atencion primaria/Sociedad Espanola de Medicina de Familiay Comunitaria 2007; 39:402–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute for Health and Clinical Excellence. Hypertension: clinical management of primary hypertension in adults. 2011. http://www.nice.org.uk/guidance/CG127. [Google Scholar]
- 3.Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 4.He J, Gu D, Chen J, et al. Premature deaths attributable to blood pressure in China: a prospective cohort study. Lancet 2009; 374:1765–1772. [DOI] [PubMed] [Google Scholar]
- 5.Starfield B. Primary care: balancing health needs, services, and technology. New York: Oxford University Press; 1998. [Google Scholar]
- 6.Beaglehole R, Epping-Jordan J, Patel V, et al. Improving the prevention and management of chronic disease in low-income and middle-income countries: a priority for primary health care. Lancet 2008; 372:940–949. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization, Primary health care—now more than ever. 2008. http://www.who.int/whr/2008/en/. [Google Scholar]
- 8.Liu LS. [2010 Chinese guidelines for the management of hypertension]. Zhonghua Xin Xue Guan Bing Za Zhi 2011; 39:579–615. [PubMed] [Google Scholar]
- 9.Asch SM, Kerr EA, Lapuerta P, et al. A new approach for measuring quality of care for women with hypertension. Arch Intern Med 2001; 161:1329–1335. [DOI] [PubMed] [Google Scholar]
- 10.Crawley D, Ng A, Mainous AG, 3rd, et al. Impact of pay for performance on quality of chronic disease management by social class group in England. J R Soc Med 2009; 102:103–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hammouche S, Holland R, Steel N. Does quality of care for hypertension in primary care vary with postcode area deprivation? An observational study. BMC Health Serv Res 2011; 11:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang Z, Wang X, Chen Z, et al. Hypertension control in community health centers across china: analysis of antihypertensive drug treatment patterns. Am J Hypertens 2014; 27:252–259. [DOI] [PubMed] [Google Scholar]
- 13.Wong MC, Wang HH, Wong SY, et al. Performance comparison among the major healthcare financing systems in six cities of the Pearl River Delta region, Mainland China. PloS One 2012; 7:e46309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 15.Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Circulation 2007; 116:e391–e413. [DOI] [PubMed] [Google Scholar]
- 16.Simpson CR, Hannaford PC, Ritchie LD, et al. Impact of the pay-for-performance contract and the management of hypertension in Scottish primary care: a 6-year population-based repeated cross-sectional study. Br J Gen Pract 2011; 61:e443–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marshall M, Campbell S, Hacker J, et al. Quality indicators for general practice: a practical guide for health professionals and managers. London, UK: Royal Society of Medicine Press; 2002. [Google Scholar]
- 18.Hernandez J, Anderson S. Storied experiences of nurse practitioners managing prehypertension in primary care. J Am Acad Nurse Pract 2012; 24:89–96. [DOI] [PubMed] [Google Scholar]
- 19.Li H, Chung RY, Wei X, et al. Comparison of perceived quality amongst migrant and local patients using primary health care delivered by community health centres in Shenzhen, China. BMC Fam Pract 2014; 15:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bleich SN, Cutler DM, Adams AS, et al. Impact of insurance and supply of health professionals on coverage of treatment for hypertension in Mexico: population based study. BMJ 2007; 335:875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kusuma YS, Gupta SK, Pandav CS. Treatment seeking behaviour in hypertension: factors associated with awareness and medication among socioeconomically disadvantaged migrants in Delhi, India. Coll Antropol 2013; 37:717–722. [PubMed] [Google Scholar]
- 22.Ogedegbe G, Harrison M, Robbins L, et al. Barriers and facilitators of medication adherence in hypertensive African Americans: a qualitative study. Ethn Dis Winter 2004; 14:3–12. [PubMed] [Google Scholar]
- 23.Howes F, Hansen E, Williams D, et al. Barriers to diagnosing and managing hypertension—a qualitative study in Australian general practice. Aust Fam Physician 2010; 39:511–516. [PubMed] [Google Scholar]
- 24.Greer TM. Perceived racial discrimination in clinical encounters among African American hypertensive patients. J Health Care Poor Underserved 2010; 21:251–263. [DOI] [PubMed] [Google Scholar]
- 25.Jenson A, Omar AL, Omar MA, et al. Assessment of hypertension control in a district of Mombasa, Kenya. Glob Public Health 2011; 6:293–306. [DOI] [PubMed] [Google Scholar]
- 26.Wang Y. [Study on characteristics and development tactics of community health service institutions by different holders]. Huazhong Technology University 2008. [Google Scholar]
- 27.Guo H. [A comparison study on three kinds of community health service models in Guangdong province]. Zhongshan University 2010. [Google Scholar]
- 28.Guthrie B, Inkster M, Fahey T. Tackling therapeutic inertia: role of treatment data in quality indicators. BMJ 2007; 335:542–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 30.Feng XL, Pang M, Beard J. Health system strengthening and hypertension awareness, treatment and control: data from the China Health and Retirement Longitudinal Study. Bull World Health Organ 2014; 92:29–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wei X, Zou G, Yin J, et al. Characteristics of high risk people with cardiovascular disease in Chinese rural areas: clinical indictors, disease patterns and drug treatment. PloS One 2013; 8:e54169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cranney M, Warren E, Barton S, et al. Why do GPs not implement evidence-based guidelines? A descriptive study. Fam Pract 2001; 18:359–363. [DOI] [PubMed] [Google Scholar]
- 33.Saxena S, Car J, Eldred D, et al. Practice size, caseload, deprivation and quality of care of patients with coronary heart disease, hypertension and stroke in primary care: national cross-sectional study. BMC Health Serv Res 2007; 7:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Parker WA, Steyn NP, Levitt NS, et al. Health promotion services for patients having non-communicable diseases: feedback from patients and health care providers in Cape Town, South Africa. BMC Public Health 2012; 12:503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Woolf SH, Grol R, Hutchinson A, et al. Clinical guidelines: potential benefits, limitations, and harms of clinical guidelines. BMJ 1999; 318:527–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu Y, Huxley R, Li L, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey. Circulation 2008; 118:2679–2686. [DOI] [PubMed] [Google Scholar]
- 37.Guo F, He D, Zhang W, et al. Trends in prevalence, awareness, management, and control of hypertension among United States adults. J Am Coll Cardiol 2012; 60:599–606. [DOI] [PubMed] [Google Scholar]
- 38.Joffres M, Falaschetti E, Gillespie C, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open 2013; 3:e003423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yip WC, Hsiao WC, Chen W, et al. Early appraisal of China's huge and complex health-care reforms. Lancet 2012; 379:833–842. [DOI] [PubMed] [Google Scholar]
- 40.Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med 1998; 339:1957–1963. [DOI] [PubMed] [Google Scholar]
- 41.Brook RH, McGlynn EA, Cleary PD. Quality of health care. Part 2: Measuring quality of care. N Engl J Med 1996; 335:966–970. [DOI] [PubMed] [Google Scholar]
- 42.Barnsley J, Berta W, Cockerill R, et al. Identifying performance indicators for family practice: assessing levels of consensus. Can Fam Physician 2005; 51:700–701. [PMC free article] [PubMed] [Google Scholar]
- 43.Liu Q, Wang B, Kong Y, et al. China's primary health-care reform. Lancet 2011; 377:2064–2066. [DOI] [PubMed] [Google Scholar]
- 44.Godley P, Nguyen A, Yokoyama K, et al. Improving hypertension care in a large group-model MCO. Am J Health Syst Pharm 2003; 60:554–564. [DOI] [PubMed] [Google Scholar]
- 45.Cassady C, Starfield B, Hurtado M, et al. Measuring consumer experiences with primary care. Pediatrics 2000; 105:998–1003. [PubMed] [Google Scholar]
- 46.Frijling BD, Spies TH, Lobo CM, et al. Blood pressure control in treated hypertensive patients: clinical performance of general practitioners. Br J Gen Pract 2001; 51:9–14. [PMC free article] [PubMed] [Google Scholar]
- 47.American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care 2014; 37 suppl 1:S14–S80. [DOI] [PubMed] [Google Scholar]


