Abstract
Patients with chronic kidney disease (CKD) are more at risk for pneumonia than the general population. Patients with pneumonia are usually treated as outpatients. However, previous studies were conducted on the basis of inpatient pneumonia. This method may underestimate the risk of pneumonia in patients with CKD. Therefore, we investigated the risk of pneumonia among CKD patients in both outpatient and inpatient settings.
A total of 15,562 patients with CKD and 62,109 individuals without CKD (matched for age and gender) were taken as subjects in the Longitudinal Health Insurance Database of Taiwan National Insurance from 1996 to 2010. The incidence density rates of inpatient and outpatient pneumonia were calculated. The risk factors associated with pneumonia were analyzed using Cox proportional hazard models with adjustments for confounders.
The incidence density rate of pneumonia was 65.6 per 1000 person-years in patients with CKD and 28.4 per 1000 person-years in individuals without CKD. The incidence density rate of inpatient pneumonia was 43.3 per 1000 person-years in patients with CKD and 16.6 per 1000 person-years in individuals without CKD. CKD was associated with increased risk of pneumonia (adjusted hazard ratio [aHR], 1.97; 95% confidence interval [CI], 1.89–2.05; P < 0.001), outpatient pneumonia (aHR, 1.40; 95% CI, 1.31–1.49), and inpatient pneumonia (aHR, 2.17; 95% CI, 2.07–2.29, P < 0.001). Patients’ comorbidities, including diabetes, cardiovascular disease (CVD), asthma, and chronic obstructive pulmonary disease (COPD), were independently associated with increased risk of pneumonia.
CKD is associated with the increased risk of both outpatient and inpatient pneumonia. This association is independent of comorbid diabetes, CVD, asthma, and COPD.
INTRODUCTION
Pneumonia is one of the most common sources of infectious morbidities in patients with chronic kidney disease (CKD). Pneumonia in patients with CKD is associated with increased hospitalization, cardiovascular events,1,2 and mortality.3,4 The pneumonia-related mortality rate of patients with CKD is 14 to 16-fold higher than that of the general population.4 The risk of inpatient pneumonia and mortality within 30 days is increased with the decline of renal function in patients with CKD.5 However, all previous studies were based on the incidence of inpatient pneumonia. This condition may underestimate the risk of pneumonia because most treatments for pneumonia are provided in outpatient settings. This study thus aims to determine the incidence of both inpatient and outpatient pneumonia in patients with CKD using the National Health Insurance (NHI) data of Taiwan.
MATERIALS AND METHODS
This work is a retrospective cohort study using an encrypted database from the Bureau of National Health Insurance (BNHI). The Institutional Review Board of China Medical waived the need for informed consent. The Longitudinal Health Insurance Database (LHID) of the Taiwan National Health Research Institute (NHRI) was released by BNHI. LHID included all medical records from 1996 to 2010. From these records, one million people were randomly selected. No significant differences were found in the sex and age distributions between LHID and all individuals in the NHRI. The International Classification of Disease Revision, Ninth Clinical Modification (ICD-9-CM) was used for the diagnosis codes. A 1:4 study design was used because an increase in controls did not increase statistical efficiency.6
Study Sample
Patients with CKD were defined as patients with ICD-9-CM code 585 from LHID who are not in the catastrophic illness patient database. The patients included in this database are those with CKD stages 3 to 5 without renal replacement therapy, including hemodialysis, peritoneal dialysis, and kidney transplantation (Figure 1).7 A total of 15,562 patients with CKD and 62,109 patients without CKD (matched for age and sex) were included. Pneumonia was identified using ICD-9-CM codes 481, 482, 485, and 486. Pneumonia-related hospitalization was also recorded. The first episode of pneumonia was recorded for patients who developed more than 1 episode. Patients with pneumonia before CKD diagnosis were excluded because we focused on the primary risk of pneumonia. Time was calculated from the index date of CKD to the date of pneumonia. Comorbidities, including diabetes (ICD-9-CM code 250), hypertension (401–405), cardiovascular disease (CVD) (410–414), asthma (493), and chronic obstructive pulmonary disease (COPD) (491, 492, 494, and 496) were defined as those that have >3 medical visits.
FIGURE 1.
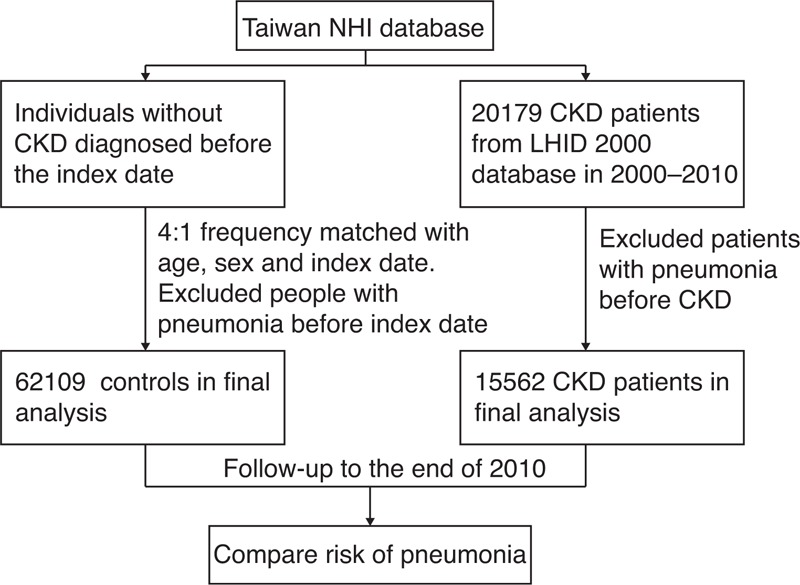
Flowchart of the study design. CKD = chronic kidney disease, LHID = Longitudinal Health Insurance Database, NHI = National Health Insurance.
Statistical Analysis
The distribution of sex, age, and comorbidities for patients with CKD and for control individuals was analyzed using χ2 test for categorical variables or t test for continuous variables. The incidence density was defined as the number of pneumonia cases divided by the total follow-up person-years (expressed as per 1000 person-years). The adjusted hazard ratio (aHR) and the 95% confidence intervals (CIs) of pneumonia risk factors were analyzed using Cox proportional hazard regression models with adjustment for sex, age, hypertension, diabetes, CVD, asthma, and COPD. The statistical significance level was set at a 2-tailed probability value <0.05. All analyses were performed using SAS software version 9.1 (SAS Institute, Cary, NC).
RESULTS
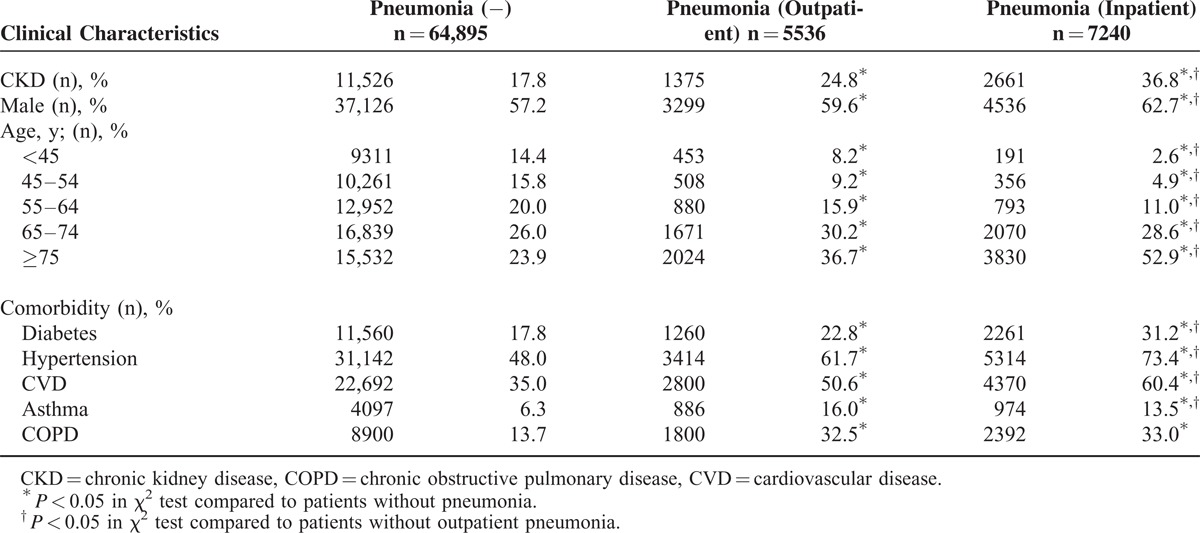
The incidence density rate of pneumonia was 65.6 per 1000 person-years in patients with CKD and 28.4 per 1000 person-years in patients without CKD (Table 1). The incidence density rate was used because the follow-up of patients without CKD was longer than that for patients with CKD. The incidence density rate of inpatient pneumonia was 43.3 per 1000 person-years in patients with CKD and 16.6 per 1000 person-years in patients without CKD. Patients with CKD had a higher rate of diabetes (P < 0.001), hypertension (P < 0.001), CVD (P < 0.001), asthma (P < 0.001), and COPD (P < 0.001) than patients without CKD. Patients who developed pneumonia were older than those without pneumonia and were also more likely to have CKD, diabetes, hypertension, CVD, asthma, and COPD (Table 2). Of 5536 patients with outpatient pneumonia, 1375 (24.8%) had CKD. Of 7240 patients with inpatient pneumonia, 2661 (36.8%) had CKD. The patients with inpatient pneumonia were older than patients with outpatient pneumonia. Patients with inpatient pneumonia were more likely to have diabetes, hypertension, and CVD than patients with outpatient pneumonia. The percentage of patients with asthma was lower in patients with inpatient pneumonia than in patients with outpatient pneumonia. The prevalence of patients with COPD was not significantly different between patients with inpatient pneumonia and those with outpatient pneumonia.
TABLE 1.
Demographic Data of Patients With and Without CKD
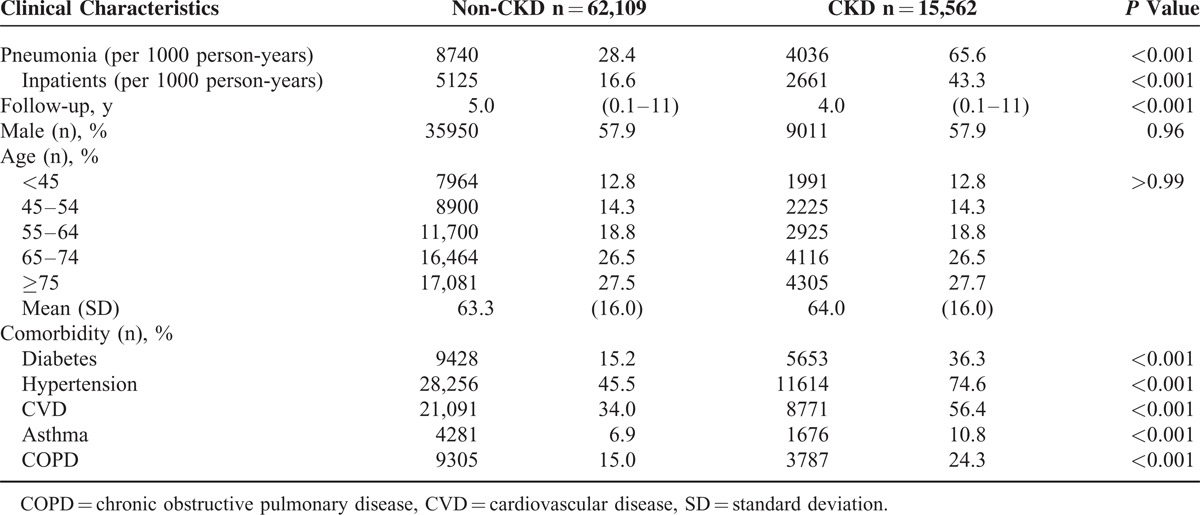
TABLE 2.
Characteristics of Patients With and Without Pneumonia
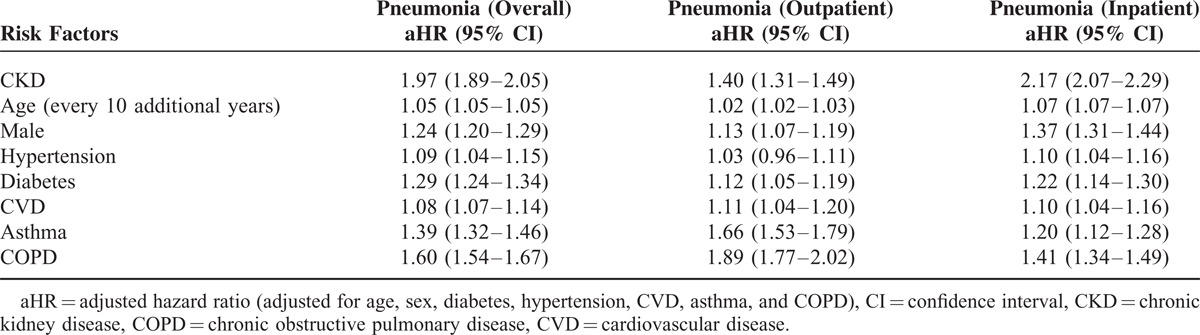
CKD, age, male gender, hypertension, diabetes, CVD, asthma, and COPD were associated with increased risk of pneumonia (Table 3). The aHR values of CKD for any type of pneumonia were 1.97 (95% CI, 1.89–2.05, P < 0.001) and 1.40 (95% CI, 1.31–1.49) for outpatient pneumonia and 2.17 (95% CI, 2.07–2.29) for inpatient pneumonia. Male gender (aHR, 1.13; 95% CI, 1.07–1.19), comorbid diabetes (aHR, 1.12; 95% CI, 1.05–1.19), comorbid CVD (aHR, 1.11; 95% CI, 1.04–1.20), comorbid asthma (aHR, 1.66; 95% CI, 1.56–1.79), and comorbid COPD (aHR, 1.89; 95% CI, 1.77–2.02) were independently associated with the increased pneumonia risk of outpatients. The comorbid hypertension was not associated with the increased pneumonia risk of outpatients but was associated with the increased pneumonia risk of inpatients (aHR, 1.10; 95% CI, 1.04–1.16).
TABLE 3.
Hazard Ratio of Pneumonia Risk Factors
DISCUSSIONS
CKD is associated with the increased risk of both outpatient and inpatient pneumonia. The risk of pneumonia was 1.97-fold higher in patients with CKD, 1.4-fold higher for outpatient pneumonia, and 2.17-fold higher for inpatient pneumonia compared with patients without CKD (Table 3). Patients with CKD have not only an increased risk of pneumonia but also an increased severity of pneumonia (indicated by hospitalization) compared with patients without CKD. The risk of overall pneumonia was higher in patients with CKD than in patients with other comorbidities (COPD, asthma, and diabetes). The risk of inpatient pneumonia was also the highest in patients with CKD. These results suggested that CKD might be an independently important contributor to the increased risk of pneumonia. The incidence of pneumonia in this study was higher than that reported in the previous studies1,2,5,8–11 because outpatient pneumonia was considered in the present work. The increased infection risk in patients with CKD can be explained by uremia-related impairment in monocyte,12 neutrophil phagocytosis,13 T lymphocytes,14 B lymphocytes,15 and increased cytokines.16 The increased risk of inpatient pneumonia in patients with CKD may be related to the comorbidity of patients with CKD because comorbidities are associated with the severity of pneumonia.17,18
The major strength of this study was the sample population size derived from the NHI data of Taiwan. The percentage of inpatient pneumonia was 58.6% in patients without CKD who developed pneumonia and 65.9% in patients with CKD who developed pneumonia. The high hospitalization rate of pneumonia can be attributed to 2 reasons. First, the hospitalization costs in Taiwan are low. Second, most of the hospitalization cost is covered by health insurance, and patients only need to pay 10% of the cost. The high rate of diabetes, hypertension, CVD,3,19,20 asthma, and COPD21,22 in patients with CKD was consistent with the findings of the previous studies.21,22
The limitations of this study are as follows. First, we could not determine the exact stage of CKD on the basis of the ICD-9-CM code 585. This condition may result in the nondifferential misclassification of CKD definition. Patients with CKD stages 1 and 2 and some patients with CKD stage 3 may be included in either patients with CKD or patients without CKD. This nondifferential misclassification may underestimate the contribution of CKD to the risk of pneumonia in the present analyses. Second, we were unable to identify CKD stages 3 to 5 exactly, and we failed to demonstrate the association of increased pneumonia risk with the worsening of CKD stages. Third, pneumonia severity index variables, such as mental status, vital signs, and laboratory data, were unavailable in LHID. Fourth, the pneumonia pathogen was associated with the severity of pneumonia23 but was not recorded in LHID. We failed to determine whether any specific pathogen was related to the pneumonia in patients with CKD.
In conclusion, patients with CKD have an increased risk for inpatient and outpatient pneumonia, especially pneumonia that requires hospitalization. The increased risk of pneumonia in patients with CKD is independent of their comorbidity.
Acknowledgment
The authors would like to thank the National Health Research Institute, Taiwan, for providing the data on insurance claims.
Footnotes
Abbreviations: BNHI = Bureau of National Health Insurance, CKD = chronic kidney disease, COPD = chronic obstructive pulmonary disease, CVD = cardiovascular disease, LHID = Longitudinal Health Insurance Database, NHI = National Health Insurance, NHRI = National Health Research Institute.
This study was supported in part by the Executive Yuan National Science Council (Grant number NSC 98-2621-M-039-001), the Clinical Trial and Research Center of Excellence of the Department of Health (Grant number DOH101-TD-B-111-004), the Taiwan Department of Health Cancer Research Center of Excellence (Grant number DOH101-TD-C-111-005), and the China Medical University Hospital (Grant number 1MS1). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Guo H, Liu J, Collins AJ, et al. Pneumonia in incident dialysis patients—the United States Renal Data System. Nephrol Dial Transplant 2008; 23:680–686. [DOI] [PubMed] [Google Scholar]
- 2.Viasus D, Garcia-Vidal C, Cruzado JM, et al. Epidemiology, clinical features and outcomes of pneumonia in patients with chronic kidney disease. Nephrol Dial Transplant 2011; 26:2899–2906. [DOI] [PubMed] [Google Scholar]
- 3.Collins AJ, Foley RN, Gilbertson DT, et al. The state of chronic kidney disease, ESRD, and morbidity and mortality in the first year of dialysis. Clin J Am Soc Nephrol 2009; 4 Suppl 1:S5–11. [DOI] [PubMed] [Google Scholar]
- 4.Sarnak MJ, Jaber BL. Pulmonary infectious mortality among patients with end-stage renal disease. Chest 2001; 120:1883–1887. [DOI] [PubMed] [Google Scholar]
- 5.James MT, Quan H, Tonelli M, et al. CKD and risk of hospitalization and death with pneumonia. Am J Kidney Dis 2009; 54:24–32. [DOI] [PubMed] [Google Scholar]
- 6.Chung CJ, Huang CY, Tsai HB, et al. Sex differences in the development of malignancies among end-stage renal disease patients: a nationwide population-based follow-up study in Taiwan. PLoS One 2012; 7:e44675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu JH, Lin SY, Hsu CY, et al. The risk for chronic kidney disease in patients with heart diseases: a 7-year follow-up in a cohort study in Taiwan. BMC Nephrol 2012; 13:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agarwal R, Bunaye Z, Bekele DM, et al. Competing risk factor analysis of end-stage renal disease and mortality in chronic kidney disease. Am J Nephrol 2008; 28:569–575. [DOI] [PubMed] [Google Scholar]
- 9.Hwang SJ, Lin MY, Chen HC, et al. Increased risk of mortality in the elderly population with late-stage chronic kidney disease: a cohort study in Taiwan. Nephrol Dial Transplant 2008; 23:3192–3198. [DOI] [PubMed] [Google Scholar]
- 10.Menendez R, Torres A, Zalacain R, et al. Risk factors of treatment failure in community acquired pneumonia: implications for disease outcome. Thorax 2004; 59:960–965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Slinin Y, Foley RN, Collins AJ. Clinical epidemiology of pneumonia in hemodialysis patients: the USRDS waves 1, 3, and 4 study. Kidney Int 2006; 70:1135–1141. [DOI] [PubMed] [Google Scholar]
- 12.Lim WH, Kireta S, Leedham E, et al. Uremia impairs monocyte and monocyte-derived dendritic cell function in hemodialysis patients. Kidney Int 2007; 72:1138–1148. [DOI] [PubMed] [Google Scholar]
- 13.Anding K, Gross P, Rost JM, et al. The influence of uraemia and haemodialysis on neutrophil phagocytosis and antimicrobial killing. Nephrol Dial Transplant 2003; 18:2067–2073. [DOI] [PubMed] [Google Scholar]
- 14.Sester U, Sester M, Hauk M, et al. T-cell activation follows Th1 rather than Th2 pattern in haemodialysis patients. Nephrol Dial Transplant 2000; 15:1217–1223. [DOI] [PubMed] [Google Scholar]
- 15.Fernandez-Fresnedo G, Ramos MA, Gonzalez-Pardo MC, et al. B lymphopenia in uremia is related to an accelerated in vitro apoptosis and dysregulation of Bcl-2. Nephrol Dial Transplant 2000; 15:502–510. [DOI] [PubMed] [Google Scholar]
- 16.Kimmel PL, Phillips TM, Simmens SJ, et al. Immunologic function and survival in hemodialysis patients. Kidney Int 1998; 54:236–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arnold FW, Ramirez JA, McDonald LC, et al. Hospitalization for community-acquired pneumonia: the pneumonia severity index vs clinical judgment. Chest 2003; 124:121–124. [DOI] [PubMed] [Google Scholar]
- 18.Ewig S, Ruiz M, Mensa J, et al. Severe community-acquired pneumonia. Assessment of severity criteria. Am J Respir Crit Care Med 1998; 158:1102–1108. [DOI] [PubMed] [Google Scholar]
- 19.Di Angelantonio E, Chowdhury R, Sarwar N, et al. Chronic kidney disease and risk of major cardiovascular disease and non-vascular mortality: prospective population based cohort study. BMJ 2010; 341:c4986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Palmer SC, Hayen A, Macaskill P, et al. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA 2011; 305:1119–1127. [DOI] [PubMed] [Google Scholar]
- 21.Kent BD, Eltayeb EE, Woodman A, et al. The impact of chronic obstructive pulmonary disease and smoking on mortality and kidney transplantation in end-stage kidney disease. Am J Nephrol 2012; 36:287–295. [DOI] [PubMed] [Google Scholar]
- 22.van Gestel YR, Chonchol M, Hoeks SE, et al. Association between chronic obstructive pulmonary disease and chronic kidney disease in vascular surgery patients. Nephrol Dial Transplant 2009; 24:2763–2767. [DOI] [PubMed] [Google Scholar]
- 23.Ruiz M, Ewig S, Marcos MA, et al. Etiology of community-acquired pneumonia: impact of age, comorbidity, and severity. Am J Respir Crit Care Med 1999; 160:397–405. [DOI] [PubMed] [Google Scholar]


