Abstract
The purpose of this review was to evaluate the efficacy and safety of qigong for hypertension.
A systematic literature search was performed in 7 databases from their respective inceptions until April 2014, including the Cochrane Library, EMBASE, PubMed, Chinese Scientific Journal Database, Chinese Biomedical Literature Database, Wanfang database, and Chinese National Knowledge Infrastructure. Randomized controlled trials of qigong as either monotherapy or adjunctive therapy with antihypertensive drugs versus no intervention, exercise, or antihypertensive drugs for hypertension were identified. The risk of bias was assessed using the tool described in Cochrane Handbook for Systematic Review of Interventions, version 5.1.0.
Twenty trials containing 2349 hypertensive patients were included in the meta-analysis. The risk of bias was generally high. Compared with no intervention, qigong significantly reduced systolic blood pressure (SBP) (weighted mean difference [WMD] = −17.40 mm Hg, 95% confidence interval [CI] −21.06 to −13.74, P < 0.00001) and diastolic blood pressure (DBP) (WMD = −10.15 mm Hg, 95% CI −13.99 to −6.30, P < 0.00001). Qigong was inferior to exercise in decreasing SBP (WMD = 6.51 mm Hg, 95% CI 2.81 to 10.21, P = 0.0006), but no significant difference between the effects of qigong and exercise on DBP (WMD = 0.67 mm Hg, 95% CI −1.39 to 2.73, P = 0.52) was identified. Compared with antihypertensive drugs, qigong produced a clinically meaningful but not statistically significant reduction in SBP (WMD = −7.91 mm Hg, 95% CI −16.81 to 1.00, P = 0.08), but appeared to be more effective in lowering DBP (WMD = −6.08 mm Hg, 95% CI −9.58 to −2.58, P = 0.0007). Qigong plus antihypertensive drugs significantly lowered both SBP (WMD = −11.99 mm Hg, 95% CI −15.59 to −8.39, P < 0.00001) and DBP (WMD = −5.28 mm Hg, 95% CI, −8.13 to −2.42, P = 0.0003) compared with antihypertensive drugs alone. No serious adverse events were reported.
The meta-analysis suggests that qigong is an effective therapy for hypertension. However, more rigorously designed randomized controlled trials with long-term follow-up focusing on hard clinical outcomes are required to confirm the results.
INTRODUCTION
Hypertension is a common condition in the general population that remains one of the most important risk factors for cardiovascular disease and stroke worldwide. For patients not currently undergoing treatment with antihypertensive agents, hypertension is typically characterized by systolic blood pressure (SBP) ≥ 140 mm Hg and/or diastolic blood pressure (DBP) ≥ 90 mm Hg on at least 2 separate intervals (after a 4-week washout period).1 Blood pressure (BP) control in hypertensive patients is an effective intervention for reducing hypertension-associated cardiovascular and renal complications. Achieving BP control in hypertensive patients often requires multiple medications and trial-and-error switching of drug classes.2 Hundreds of compounds representing multiple drug classes were developed nearly 50 years ago. The guidelines on hypertension released by the Eighth Joint National Committee (JNC 8) reflect an evidence-based approach in recommending a therapeutic regimen that includes a healthy diet, weight control, regular exercise, and appropriate initial and supplemental antihypertensive therapy.3 There has been a revival of interest in complementary and alternative medicine (CAM) approaches for lowering BP 4–6 in part because control rates for hypertension remain dismal despite the vast armamentarium of antihypertensive agents available to clinicians.3 In some cases, hypertensive patients can benefit from drug therapy optimization and combination therapy. In some patients, however, adequate BP control cannot be achieved by these approaches.7 Another major impetus for current clinical trials using CAM as a therapeutic strategy is the many adverse effects of long-term conventional antihypertensive drugs.8 Therefore, some traditional therapies, including qigong,9 tai chi,10 acupuncture,11 moxibustion,12 yoga,13 massage,14 dietary supplements,15 and herbal products,16,17 are increasingly favored by hypertensive patients with the hope of lowering BP and relieving hypertension-related symptoms with fewer adverse effects.
Qigong is an ancient Chinese healing art that dates back 7000 years.18 The word “qigong” involves 2 theories: “qi,” the vital energy of the body, and “gong,” the training or cultivation of qi.19 The practice of qigong aims to cultivate energy via systematic training exercises, including the coordination of different breathing patterns, rhythmic movements, and meditation, in contrast to conventional exercise.20 Due to its significant promotion of human health and ease of learning, qigong is appropriate for nearly anyone of any age or physical condition. Qigong has its underpinnings in traditional Chinese medicine (TCM) and philosophy. One possible explanation for the beneficial effects of qigong exercise is increased healthy flow of qi, blood, and fluid throughout the body by repetitive movements to relieve pathological stagnation and regulate the function of meridians and visceral organs. Qigong is practiced by 5% of China's 1.3 billion people to improve health, explore the latent ability of humans, prevent disease, and prolong life in the context of a wide range of conditions, including hypertension,21,22 heart failure,23 coronary heart disease,24 cardiac rehabilitation,25 cancer,26 diabetes,27 metabolic syndrome,28 chronic obstructive pulmonary disease,29 movement disorders,30 chronic pain,31 fatigue,32 stress,33 anxiety,34 depression,35 and immune function36 and to enhance the quality of life (QOL) of patients with other chronic diseases.37
There is increasing evidence that qigong can benefit hypertensive patients, and clinical studies and systematic reviews of the efficacy of qigong as a useful lifestyle intervention for hypertension are ongoing. Qigong has been reported to decrease BP smoothly and moderately, recover the circadian rhythm of BP, improve QOL, slow the progression of severe complications, and reduce mortality.9,21,22,38–40 Until now, positive evidence of BP reduction by qigong has been summarized in 2 systematic reviews published in English based on the poor quality of the primary data.21,22 However, due to different study designs, 4 main databases in Chinese were not included in the retrieval randomized controlled trials (RCTs); thus, these 2 systematic reviews are subject to insufficient literature retrieval.41 For health practitioners, the appropriateness of recommending qigong as an effective therapy for hypertension remains unclear. This study aims to minimize bias and provide more-reliable findings by using explicit and systematic methods. To determine whether qigong safely benefits hypertensive patients, we performed a systematic review and meta-analysis of RCTs of qigong for hypertension.
METHODS
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Ethical approval was not necessary for this review study.
ELIGIBILITY CRITERIA
Types of Studies
Only RCTs evaluating the effects of qigong on hypertension were considered. Animal experiments were not included.
Types of Participants
Participants of any sex, age, and ethnic origin were clinically diagnosed as hypertensive in any stage according to at least 1 of the current or past guidelines or definitions of hypertension. Trials that declared patients with hypertension but without detailed information about the diagnostic criteria were also considered.
Types of Interventions
Eligible RCTs of qigong practiced alone or in combination with antihypertensive drugs versus no intervention, exercise, or antihypertensive drugs for hypertension were identified without restriction of blinding, publication status, or language. We excluded trials if interventions in the qigong or control groups contained other nonconventional therapies, including herbal medicine, acupuncture, moxibustion, cupping, and massage; studies reported only laboratory values rather than BP outcomes; or studies were case reports, case series, and duplicated publications reporting the same group of participants.
Types of Outcome Measures
All trials used categorical or continuous BP as the outcome measure. The efficacy of qigong on categorical BP was evaluated using 3 graded criteria, as authoritatively recommended by the China Food and Drug Administration (available at http://www.sda.gov.cn) and the China National Committee on Screening, and Prevention of Coronary Heart Disease and High Blood Pressure of 1974.22,42 The evaluation criteria were as follows: “significant improvement” (DBP decreased by 10 mm Hg reaching the normal range or DBP not yet returned to normal but reduced by 20 mm Hg or more), “improvement” (DBP decreased by <10 mm Hg but reaching the normal range, DBP decreased by 10 to 19 mm Hg but not reaching the normal range, or SBP decreased by 30 mm Hg or more), and “no improvement” (not reaching the above standards). To permit the overall synthesis of these enumeration data, we grouped these data dichotomously, “significant improvement” and “improvement” as “effective” and “no improvement” as “ineffective.”
Search Strategy
A systematic search was conducted in the following 7 online electronic databases from their inception until April 17, 2014: Cochrane Library (1996–2014), EMBASE (1980–2014), PubMed (1959–2014), Chinese Scientific Journal Database (1989–2014), Chinese Biomedical Literature Database (1978–2014), Wanfang database (1985–2014), and Chinese National Knowledge Infrastructure (1979–2014). We also reviewed the reference lists of retrieved articles. The websites of the Chinese Clinical Trial Registry (http://www.chictr.org/) and the international clinical trial registry of the US National Institutes of Health (http://clinicaltrials.gov/) were also searched to identify unpublished clinical trials. The following keywords were used to search the databases: (“hypertension” OR “high blood pressure” OR “blood pressure”) AND (“qigong” OR “qi gong” OR “chi gong” OR “chi kung”) AND (“clinical trial” OR “randomized controlled trial” OR “randomised controlled trial”).
Study Selection
Two reviewers independently identified the potential literature and selected studies in a standardized manner. Then, the titles and abstracts of the references were screened for potentially relevant RCTs. The full texts of eligible articles were retrieved for further identification according to the specified selection criteria. Disagreements were resolved by consultation or consensus with a third reviewer.
Data Extraction
Two reviewers independently extracted the following data: general information: authors, title, publication data, and literature source; characteristics of the included trials and patients: randomization, allocation concealment, blinding, intention-to-treat analysis, dropouts or withdrawals, sample size, age, sex, diagnosis standard, interventions of each group, and duration of treatment; outcomes: BP data at the baseline and after treatment; length and frequency of follow-up; and adverse events (AEs). Missing information was obtained from the original authors whenever possible.
Quality Assessment
Two reviewers independently assessed the risk of bias in each included trial using Cochrane Collaboration's tool from the Cochrane Handbook for Systematic Review of Interventions, version 5.1.0.43 The following 7 aspects were evaluated: random sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), and other bias (from Chapter 8: assessing risk of bias in included studies). Each item was categorized as low/high/unclear risk of bias. Then, the trials were categorized into 3 levels: low risk of bias (all items were at low risk of bias), high risk of bias (at least 1 item was at high risk for bias), and unclear risk of bias (at least 1 item was at unclear risk of bias).
Data Synthesis
The Review Manager software (RevMan, version 5.1; The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, 2011) was used for data synthesis and analysis. Both dichotomous and continuous outcomes were extracted from the primary trials without any conversion. Dichotomous data were presented as risk ratio and continuous outcomes as weighted mean difference (WMD), both with a 95% confidence interval (CI). A meta-analysis was performed if the outcomes were similar in clinical characteristics. Heterogeneity between trials was recognized as significant when I2 > 50% or P < 0.1. The fixed-effects model was used to analyze data with low heterogeneity (heterogeneity test, P ≥ 0.10), whereas the random-effects model was applied if heterogeneity was significant (heterogeneity test, P < 0.10). Subgroup analysis was conducted according to the types of comparisons. Publication bias was assessed by funnel plot analysis if the group included >10 trials.43
RESULTS
Study Identification
We identified 593 articles on qigong for hypertension from electronic and manual searches. By reading the titles and abstracts, we excluded 235 duplicates of the articles that were included in different databases and 303 articles that were clearly review articles, experts’ commentaries, case reports, case series, or other nonclinical studies. A total of 55 full-text articles were retrieved for further assessment, of which 35 were excluded for the following reasons: participants did not meet the inclusion criteria (n = 23); duplication (n = 5); no control group (n = 3); intervention included other medical therapies, such as acupuncture, moxibustion, massage, and external application (n = 3); and no data for extraction (n = 1). Ultimately, 20 studies were included in this review.44–63 All trials were conducted in 2 countries (China, n = 18; South Korea, n = 2) and were published between 1982 and 2013 in 2 languages (Chinese, n = 17; English, n = 3). The flow diagram of the search and identification process is presented in Figure 1.
FIGURE 1.

Flow diagram of study selection and identification.
Study Characteristics
A total of 2349 hypertensive patients were analyzed. All studies adopted qigong as either monotherapy or adjunctive therapy to antihypertensive drugs in the treatment group. Two trials 47,53 had a 3-group study design: 1 trial included qigong, jogging, and antihypertensive drugs groups,47 whereas the other included qigong plus antihypertensive drugs (QPADs), qigong, and antihypertensive drugs groups.53
Internal qigong (neiqi) and external qigong (waiqi) are distinguished by who is practicing qigong. That is, internal qigong (neiqi) is practiced by hypertensive patients themselves for beneficial health effects, whereas external qigong (waiqi) is performed by a trained practitioner other than the patient to direct the qi energy to the patient. In our review, all trials used internal qigong as the interventions in the treatment group. Interventions included qigong practiced alone44–52 and combined with antihypertensive drugs.53–63 The controls included wait-list control,44,45 conventional exercises,46 jogging,47 no exercise (maintenance of original lifestyle),48 oryzanol,49 or antihypertensive drugs.50–63 Patients in the treatment group received the same type and dosage of antihypertensive drugs under the same standard used for the control group. All studies were single-centered and parallel-designed.
The 20 included trials specified 3 diagnostic criteria of hypertension. Among these trials, 3 used the National Committee on Screening, and Prevention of Coronary Heart Disease and High Blood Pressure in China—1974,47,52,62 3 trials used the National Committee on Prevention and Treatment of Cardiovascular Disease in China—1979,53,54,60 2 trials used the World Health Organization-International Society of Hypertension guidelines for the management of hypertension guidelines for the management of hypertension—1978,51,63 and 12 trials included patients with hypertension without detailed information about diagnostic criteria.44–46,48–50,55–59,61
The total treatment duration ranged from 8 weeks to 12 months. Clinical efficacy on BP was observed in all studies, with no difference in the baseline BP data. Two different methods were used to evaluate the clinical efficacy on BP: 13 trials used BP data,44–48,50–56,63 whereas the other 7 trials used the 3-grade evaluation criteria.49,57–62 AEs were reported in only 1 trial,46 whereas no other studies mentioned them. The detailed study characteristics are summarized in Table 1 .
TABLE 1.
Basic Characteristics of the Included Studies

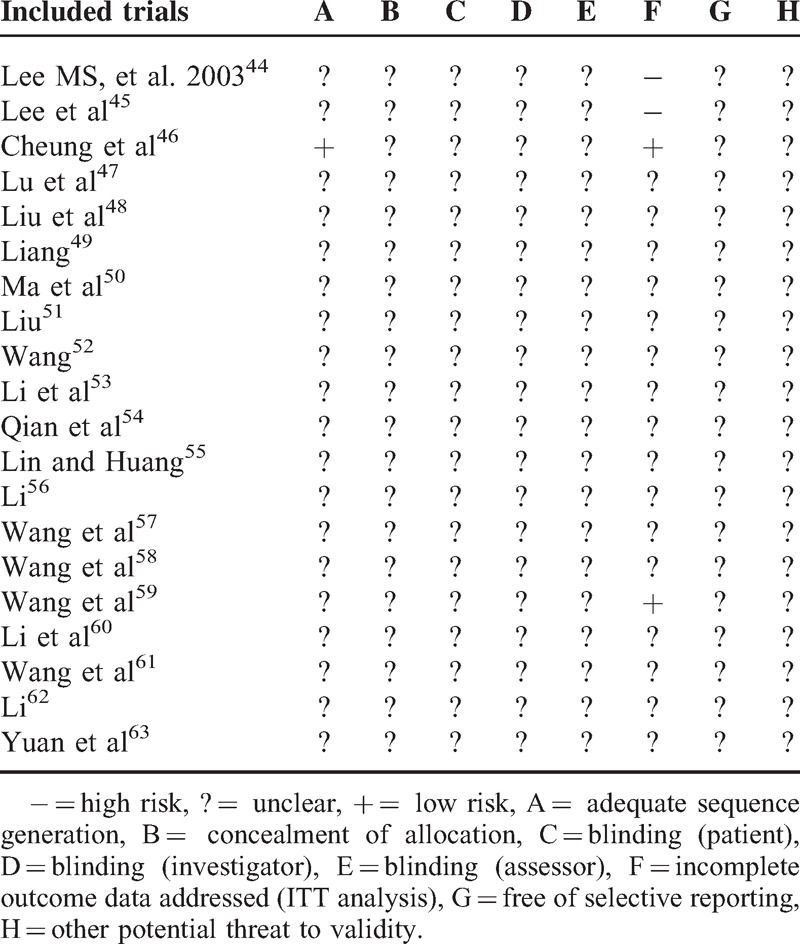
Study Quality
We assessed the risk of bias of the included studies based on the information extracted from the methods section. According to the Cochrane Collaboration tool, most of the included trials were evaluated as high risk of bias. The methodological quality of most of the trials was generally “poor.” Only 1 study described the method for random sequence generation.46 No trials described allocation concealment, blinding of participants, or outcome assessment. Detailed information about dropouts and withdrawals were reported in 4 trials.44–46,59 Only 1 trial described a pretrial estimation of sample size.46 We also attempted to contact authors by telephone, fax, and email for further information, but no responses were received. The details of the risk of bias of each trial are presented in Table 2.
TABLE 1 (Continued).
Basic Characteristics of the Included Studies

TABLE 2.
Methodological Quality of the Included Studies Based on the Cochrane Handbook
Efficacy Assessment
All studies focused on the effect of qigong on hypertensive patients. A subgroup analysis was conducted among 4 different types of comparisons, including qigong versus no intervention,44,45,48,49 qigong versus exercise,46,47 qigong versus antihypertensive drugs,47,50–53 and QPADs versus antihypertensive drugs.53–63
Qigong Versus No Intervention
Interventions in the control groups of 4 trials included wait-list control,44,45 no exercise (maintenance of original lifestyle),48 and oryzanol.49 Because none of the interventions had an effect on BP, we grouped them into a “no-intervention” category for further analysis. There were 111 patients in the qigong group and 79 in the no-intervention group.
Three trials used BP data to measure the clinical efficacy of qigong compared with no intervention.44,45,48 An overall synthesis of BP data was performed. Meta-analysis revealed a significant lowering effect of qigong on SBP (WMD = −17.40 mm Hg, 95% CI −21.06 to −13.74, P < 0.00001) with no significant heterogeneity (χ2 = 2.98, P = 0.22, I2 = 33%) (Figure 2A). Qigong significantly lowered the level of DBP (WMD = −10.15 mm Hg, 95% CI −13.99 to −6.30, P < 0.00001) with high heterogeneity (χ2 = 5.18, P = 0.08, I2 = 61%) compared with no intervention (Figure 2B).
FIGURE 2.
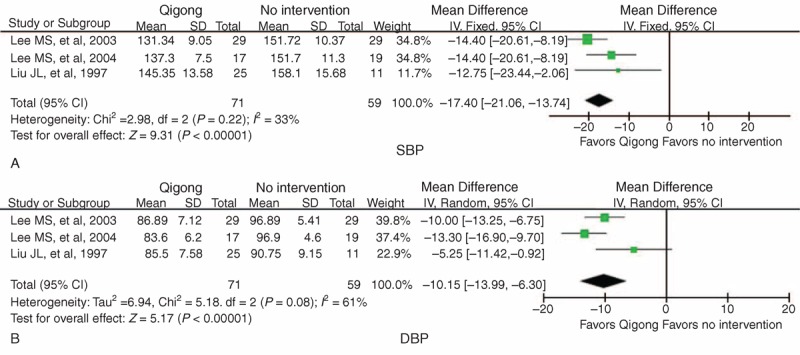
Forest plot of the comparison of qigong versus no intervention for the outcome of BP: (A) SBP and (B) DBP. BP = blood pressure, CI = confidence interval, DBP = diastolic blood pressure, SBP = systolic blood pressure.
One trial conducted by Liang49 used the 3-grade evaluation criteria to assess the effect of qigong on hypertension. A total of 60 hypertensive patients were randomized into a treatment group (n = 40) and control group (n = 20). The participants in the control group received oryzanol therapy, whereas the patients in the treatment group received qigong plus oryzanol therapy. After 3 months, the qigong plus oryzanol group had significantly lower BP in general than the oryzanol group (95% vs 35%, P < 0.01).
Qigong Versus Exercise
Because interventions in the control groups of 2 trials included conventional exercise46 and jogging,47 subgroup analysis of qigong versus exercise was performed. There were 86 patients in the qigong group and 83 in the exercise group. All studies reported BP data at baseline and after intervention. The meta-analysis indicated that SBP was significantly higher in the qigong group compared the exercise group after treatment (WMD = 6.51 mm Hg, 95% CI 2.81 to 10.21, P = 0.0006) with no significant heterogeneity (χ2 = 0.32, P = 0.57, I2 = 0%) (Figure 3A). There was no statistical significance in DBP between the qigong group and exercise group (WMD = 0.67 mm Hg, 95% CI −1.39 to 2.73, P = 0.52) with no significant heterogeneity (χ2 = 0.14, P = 0.71, I2 = 0%) (Figure 3B).
FIGURE 3.

Forest plot of the comparison of qigong versus exercise for the outcome of BP: (A) SBP and (B) DBP. BP = blood pressure, CI = confidence interval, DBP = diastolic blood pressure, SBP = systolic blood pressure.
Qigong Versus Antihypertensive Drugs
Five studies evaluated the effect of qigong on BP compared with antihypertensive drugs.47,50–53 There were 318 patients in the qigong group and 177 in the antihypertensive drug group.
One trial conducted by Wang52 evaluated the effect of qigong on BP compared with antihypertensive drugs in 4 different age groups. The trial demonstrated a significant lowering effect of qigong on SBP and DBP. However, we could not use these data for further meta-analysis.
A change in BP data was also reported in 4 other trials,47,50,51,53 and subgroup analysis was performed. The meta-analysis did not reveal a significant lowering effect on SBP in the qigong group compared with the antihypertensive drug group (WMD = −7.91 mm Hg, 95% CI −16.81 to 1.00, P = 0.08) with high heterogeneity (χ2 = 17.09, P = 0.0007, I2 = 82%) (Figure 4A). Qigong significantly reduced DBP (WMD = −6.08 mm Hg, 95% CI −9.58 to −2.58, P = 0.0007) with high heterogeneity (χ2 = 11.02, P = 0.01, I2 = 73%) compared with antihypertensive drugs (Figure 4B).
FIGURE 4.
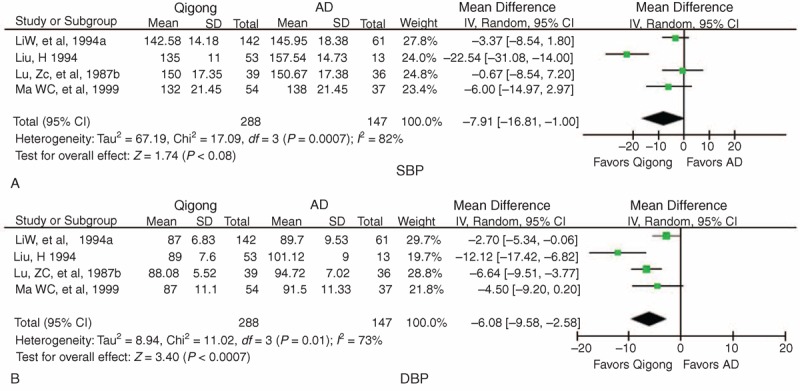
Forest plot of the comparison of qigong versus AD for the outcome of BP: (A) SBP and (B) DBP. AD = antihypertensive drugs, BP = blood pressure, CI = confidence interval, DBP = diastolic blood pressure, SBP = systolic blood pressure.
QPADs Versus Antihypertensive Drugs
Eleven trials compared QPADs (combination therapy group) with antihypertensive drugs (single-therapy group) for the treatment of hypertension.53–63 There were 960 patients in the combination therapy group and 599 in the single-therapy group.
Five trials used BP data to evaluate the effect of combination therapy compared with single therapy,53–56,63 and subgroup analysis was performed. The pooled analysis of 5 trials indicated that compared with the single-therapy group, SBP was significantly lower in the combination therapy group (WMD = −11.99 mm Hg, 95% CI −15.59 to −8.39, P < 0.00001) with significant heterogeneity (χ2 = 8.97, P = 0.06, I2 = 55%) (Figure 5A). A significant lowering effect on DBP was observed in the combination therapy group (WMD = −5.28 mm Hg, 95% CI −8.13 to −2.42, P = 0.0003), with significant heterogeneity (χ2 = 19.39, P = 0.0007, I2 = 79%) compared with the single-therapy group (Figure 5B).
FIGURE 5.

Forest plot of the comparison of QPAD versus AD for the outcome of BP: (A) SBP, (B) DBP, and (C) BP. AD = antihypertensive drugs, BP = blood pressure, CI = confidence interval, DBP = diastolic blood pressure, QPAD = qigong plus antihypertensive drugs, SBP = systolic blood pressure.
Six trials used the 3-grade criteria to assess the effect of combination therapy on BP in general.57–62 A meta-analysis revealed a significant BP-lowering effect in the combination therapy group (risk ratio = 1.33, 95% CI 1.23 to 1.43, P < 0.00001) with no significant heterogeneity (χ2 = 1.43, P = 0.92, I2 = 0%) compared with the single-therapy group (Figure 5C).
Adverse Events
Among the 20 included trials, only 1 (5%, 1/20) mentioned AEs.46 In that trial, a woman in the qigong group experienced vestibular neuronitis; however, this symptom was not related to the practice of qigong. Although AEs were not rigorously monitored and reported in the other 19 trials (95%, 19/20), most of the original authors declared that qigong was a relatively safe approach for various conditions, including hypertension. No severe AEs were reported.
Publication Bias
Because the number of included trials in each subgroup was <10, funnel plots could not be applied to detect potential publication bias.
DISCUSSION
Summary of Evidence
CAM, including TCM, is increasing in popularity among the general population in Western countries.64–67 Hypertensive patients have joined this global trend 68,69 and often seek complementary therapies to conventional antihypertensive treatment without their physicians’ knowledge.70 Previous reports have estimated that CAM therapies are used by 29% to 69.5% of hypertensive patients.71–73 Among the most common forms of CAM therapies, qigong is one of the easiest and most accessible modes worldwide.74,75 In China, qigong has been practiced for its health-enhancing qualities for thousands of years. Qigong was also recently confirmed to improve aspects of the psychosocial, physical, and physiological domains in hypertensive patients. These benefits include relieving tinnitus,76 improving fatigue,77,78 alleviating depression,79 reducing stress and anxiety,34 and enhancing QOL,80 specifically targeting older adults.81,82 However, the selection of such therapies should be based on scientific studies and evidence-based medicine rather than patient preference.83
Regarding the role of qigong in the treatment of hypertension, we aimed to provide a systematic review and meta-analysis of both the English and Chinese literature to address the efficacy and safety of qigong in the treatment of hypertension. Although qigong is mainly practiced and researched in China, only a few Chinese databases were searched in the 2 previous systematic reviews,21,22 potentially excluding relevant studies and inducing selection bias.41 A prominent characteristic of this review was the extensive, unbiased literature search in various Chinese databases, which included much information about qigong that is not available in the English literatures. Although 12 and 9 trials were included in Lee et al's study21 in 2007 and Guo et al's study22 in 2008, respectively, the current review includes additional recently published clinical trials, potentially providing more convincing evidence to support the use of qigong for hypertension. This is the most comprehensive assessment of qigong for hypertension and provides new evidence for clinical professionals.
The overall results of the 20 included randomized trials with 2349 hypertensive patients suggest that qigong is superior to no intervention in lowering SBP (decreased by 17.40 mm Hg) and DBP (decreased by 10.15 mm Hg). Qigong is inferior to exercise in decreasing SBP (increased by 6.51 mm Hg), but no significant difference between qigong and exercise was observed for DBP (increased by 0.67 mm Hg). Qigong resulted in a clinically meaningful but not statistically significant reduction in SBP (decreased by 7.91 mm Hg) but appeared to be more effective in lowering DBP (decreased by 6.08 mm Hg) compared with antihypertensive drugs. As an adjunctive therapy to antihypertensive drugs, qigong significantly lowered SBP (decreased by 11.99 mm Hg) and DBP (decreased by 5.28 mm Hg) compared with antihypertensive drugs alone.
Previous studies conducted by Lewington et al84 suggested that each increase of 20 mm Hg in SBP or 10 mm Hg in DBP doubles the risk of cardiovascular and stroke events in individuals ages 40 to 69 years with a BP > 115/75 mm Hg. However, antihypertensive treatment substantially reduces this cardiovascular risk. In this review, one of the critical issues was the effectiveness of qigong in lowering BP. The BP-lowering effect of qigong was evaluated in 4 subgroups according to different comparisons. The first finding was evidence about the efficacy of qigong compared with the no-intervention control. Our meta-analysis suggested that qigong has beneficial effects for lowering both SBP and DBP compared with no intervention. This result is consistent with previously published meta-analyses,21,22 indicating that regular qigong practice may have positive effects for hypertensive patients.
Another valuable finding of this review was the comparison between qigong and exercise. Guidelines for the management of hypertension recommend exercise as the frontline strategy for key preventive lifestyle modification to reduce the risk of hypertension and to manage high BP.1,6,85 Hypertensive patients are advised to perform 30 to 60 minutes of moderate-to-vigorous–intensity aerobic exercise 4 to 7 days per week in addition to the activities of daily living. Numerous observational epidemiological studies, clinical trials, and meta-analyses have been conducted to summarize the growing numbers of trials addressing the effects of exercise on BP.86–89 These studies have demonstrated that acute and chronic aerobic exercise can contribute to reducing resting and ambulatory BP in hypertensive patients. In this review, a meta-analysis of 2 trials reporting adequate data revealed that exercise is superior to qigong in lowering SBP, and a relatively small but not significant lowering effect was observed for DBP, indicating that regular physical exercise maybe more effective than qigong in the management of hypertension. Similar results were observed in a previously published systematic review.22 However, due to the small sample size, short-term duration, and limited trials, the current conclusions should be treated with caution. In addition, previous national surveys in the United States have revealed that exercise is practiced by only 26% of hypertension patients and that patients >75 years of age are least likely to participate.90 In China, qigong is widely practiced by middle-aged and elderly people, some of whom are intolerant of moderate-to-vigorous–intensity aerobic exercise. Therefore, qigong may be more suitable for elderly patients as a gentle alternative to intense physical activities, particularly static qigong, which has low physical demands, although further evidence is needed.91,92
The third interesting finding of this review was the comparison between qigong and antihypertensive drugs. There is robust evidence from RCTs that a BP reduction of 10 mm Hg systolic or 5 mm Hg diastolic by antihypertensive drugs contributes to a 22% reduction in coronary heart disease events (17%–27%) and a 41% (33%–48%) reduction in stroke.93 Could qigong be used as an alternative therapy to antihypertensive drugs for hypertension? In our review, compared with antihypertensive drugs, qigong had a clinically meaningful but nonsignificant effect on lowering SBP but was effective in lowering DBP. Therefore, qigong may be a valuable lifestyle intervention in maintaining a desirable BP. However, due to the limited number of included trials and significant clinical heterogeneity in this subgroup, additional evidence is needed to confirm these conclusions.
TCM is often used in addition to baseline treatment with effective Western medicines to enhance the hypotensive effect and reduce the toxicity of conventional treatment. That is, patients in the control groups received conventional Western medicine therapy alone, whereas patients in the treatment group received a combination of TCM and Western medicine therapy. This design is also known as an add-on design, which is quite popular for TCM studies of various diseases and conditions.94–99 Is adjunctive qigong therapy more effective than antihypertensive drugs alone in lowering BP? The fourth finding was the evaluation of the effect of the combination of qigong and antihypertensive drugs on BP. Our data suggest that QPADs significantly decrease both SBP and DBP more than antihypertensive drugs alone. A similar positive effect on BP was also reported in other nonpharmacological add-on studies for hypertension.10,12,14 These results suggest that QPAD therapy may be an optimal therapeutic regimen for hypertensive patients who are insensitive to pharmacological treatment alone, particularly when compliance with antihypertensive drug treatment is poor. Considering the potential BP reduction effect of qigong as a monotherapy or adjunctive therapy, its practice could reduce the global burden of disease due to high BP either economically or clinically.
A recent review by Lawes et al100 suggested that approximately 54% of stroke and 47% of ischemic heart disease worldwide are attributable to high BP. Previous studies have also demonstrated that physical activity reduces cardiovascular mortality by 16% to 67%.101 Could qigong contribute to the reduction of cardiovascular events and regular exercise? We estimated the effect of qigong in preventing the incidence of all causes of mortality and progression to severe complications. Only 1 trial assessed these outcomes with a 30-year follow-up, and further evidence is required.59 A total of 242 hypertensive patients were randomized into a QPADs group (n = 122) and an antihypertensive drugs group (n = 120) for 12 months. At the end of follow-up, a significant beneficial effect on total mortality was observed in the QPADs group (25.41% vs 47.50%, P < 0.001), particularly mortality caused by serious hypertensive complications (18.85% vs 39.16%, P < 0.01). Although positive effects of qigong on cardiovascular morbidity and mortality were reported by only 1 trial (5%, 1/20) with long-term follow-up, reporting was inadequate in the other 19 trials (95%, 19/20), demonstrating that the long-term effect of qigong could be evaluated with RCTs and that well-designed studies with a low risk of bias generate more-valid clinical evidence.
In addition, it should be noted that doctor training and expertise are important factors contributing to the positive effects of qigong for hypertensive patients. More recent studies have suggested that the choice of treatment by doctors is influenced by their training and clinical experience.102 Doctors with further elective training in TCM used more individualized TCM therapies. Thus, studies conducted in China are likely completed by qigong experts with better training and experience. Is there any difference in reporting the participation of experienced physicians? In this review, 2 RCTs that were preformed in South Korea all declared the use of qigong experts.44,45 Another trial that was published in English also stated that qigong was taught by an instructor with expertise in guolin qigong.46 Thus, all trials conducted outside China and published in English gave full consideration to this issue, and no difference in doctor training or expertise was identified.
LIMITATIONS
The apparent reported positive findings should be interpreted conservatively due to the low methodological quality and significant heterogeneity of the included trials. There are 5 limitations to this review. First, methodological issues are a common concern in CAM clinical trials.103 The results reported in this article are similar to those of previous systematic reviews,21,22 which also addressed concerns regarding the high risk of bias in the primary studies. In this review, most of the trials were of poor methodological quality. Inadequate reporting of the study design, allocation sequence, allocation concealment, blinding, intention-to-treat analysis, and dropouts was identified in the majority of trials. Randomization is necessary to avoid selection bias. However, only 1 trial reported the method of random sequence generation.46 In addition, no trial described allocation concealment, suggesting that some declared RCTs may not be true RCTs. Blinding is an essential method for preventing research outcomes from being influenced by either performance bias or detection bias. In this review, because it is difficult to blind patients to treatment, only the blinding of the outcome assessor was considered according to the Cochrane risk of bias criteria. However, no trials reported this blinding. The lack of information on dropouts and withdrawals was also problematic. Only 4 trials provided information on dropout rates and withdrawals.44–46,59 Moreover, a lack of follow-up might lead to difficulty in accounting for the long-term effect of qigong. Only 1 study described a pretrial estimation of the sample size.46 Therefore, whether the sample sizes met the basic requirements of clinical research in the other trials is unknown.
Second, the heterogeneity in this analysis merits further attention. The significant clinical heterogeneity reflected in variations in methodological quality, participants, interventions, and antihypertensive drugs might weaken the reliability of the data. Thus, it was not possible to perform a pooling analysis of the trials.
Third, potential publication bias is another major concern that would limit the generalizability of the findings. The large number of duplicate publications was also a matter of concern in this review. Notably, the Shanghai Institute of Hypertension in China has completed numerous studies including >2000 patients in the past 60 years, although few of these studies are represented in the literature. After checking the original data, only 4 of 25 published articles were included.57–59,61 Although great effort was made to avoid language bias and location bias during data retrieval, almost all trials identified after comprehensive searches were conducted in China and published in Chinese with positive results favoring qigong treatment. A systematic review by Vickers et al104 reported that some countries, including China, publish a high proportion of positive results and found publication bias to be a possible explanation. Therefore, we cannot completely rule out potential publication bias.
Fourth, although most studies claimed that antihypertensive drugs were used to achieve the best control of BP, whether these prescriptions met clinical standards was unclear due to insufficient reporting. In addition, the use of 3-grade evaluation criteria to evaluate the overall effect on BP limits the global acceptability and generalizability of these findings.
Furthermore, there was little detailed information about AEs. Appropriate qigong exercise may induce a series of normal physiological and psychological reactions in participants; however, inappropriate training might lead to physical and mental disorders.105–107 Qigong as evaluated in this review generally seemed safe and well tolerated by hypertensive patients. However, the safety of its use could not be confirmed because only 1 study mentioned the safety of interventions. Investigators may have underestimated possible AEs in these trials. Therefore, it is difficult to draw definite conclusions about the safety of qigong.
CONCLUSIONS
Whether qigong is beneficial for hypertensive patients is an important question. Based on the available literature in English and Chinese, the results of this meta-analysis suggest that qigong is an effective therapy for hypertension. Qigong is superior to no intervention and antihypertensive drugs but inferior to exercise in lowering BP; qigong as an adjunctive therapy to antihypertensive drugs significantly lowers BP and could be recommended as a complementary approach for hypertensive patients. However, due to the poor methodological quality of the included studies, further rigorously designed RCTs with long-term follow-up focusing on hard clinical outcomes are required to confirm the results and to provide a high level of evidence, particularly to support qigong as an alternative to regular exercise for elderly patients. If well-designed RCTs with a high quality of methodology confirm that qigong is beneficial, it could be recommended as an evidence-based complementary and alternative therapy for the treatment of hypertension worldwide. On the contrary, negative results would challenge the rational basis and clinical evidence supporting qigong. We hope that this systematic review paves the way for evidence-based research on qigong for hypertension.
Footnotes
Abbreviations: AE = adverse event, BP = blood pressure, CAM = complementary and alternative medicine, CI = confidence interval, DBP = diastolic blood pressure, QOL = quality of life, RCT = randomized controlled trial, SBP = systolic blood pressure, TCM = traditional Chinese medicine, WMD = weighted mean difference.
The study was financially supported by the National Natural Science Foundation Project of China (No. 81403375).
XX conceived the idea, contributed to study design and interpreted the data. WP, LX, and ZY conducted the literature searches and evaluated the methodological quality. XX made the analysis, having full access to all of the data in this study and taking responsibility for the integrity and accuracy of the data analysis. He also drafted the article, which was reviewed and commented by WP, LX, and ZY.
The authors have no conflicts of interest to disclose.
References
- 1.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34:2159–2219. [DOI] [PubMed] [Google Scholar]
- 2.Staessen JA, Wang JG, Bianchi G, et al. Essential hypertension. Lancet 2003; 361:1629–1641. [DOI] [PubMed] [Google Scholar]
- 3.James PA, Oparil S, Carter BL, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults report from the panel members appointed to the Eighth Joint National Committee (JNC 8). J Am Med Assoc 2014; 311:507–520. [DOI] [PubMed] [Google Scholar]
- 4.Brook RD, Appel LJ, Rubenfire M, et al. Beyond medications and diet: alternative approaches to lowering blood pressure. Hypertension 2013; 61:1360–1383. [DOI] [PubMed] [Google Scholar]
- 5.Wang J, Xiong XJ. Evidence-based Chinese medicine for hypertension. Evid Based Complement Alternat Med 2013; 2013:e978398.1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vogel JH, Bolling SF, Costello RB, et al. Integrating complementary medicine into cardiovascular medicine. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents (Writing Committee to Develop an Expert Consensus Document on Complementary and Integrative Medicine). J Am Coll Cardiol 2005; 46:184–221. [DOI] [PubMed] [Google Scholar]
- 7.Guo F, He D, Zhang W, et al. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. J Am Coll Cardiol 2012; 60:599–606. [DOI] [PubMed] [Google Scholar]
- 8.Moser M, Setaro JF. Clinical practice: resistant or difficult-to-control hypertension. N Engl J Med 2006; 355:385–392. [DOI] [PubMed] [Google Scholar]
- 9.Mayer M. Qigong and hypertension: a critique of research. J Altern Complement Med 1999; 5:371–382. [DOI] [PubMed] [Google Scholar]
- 10.Wang J, Feng B, Yang XC, et al. Tai Chi for essential hypertension. Evid Based Complement Alternat Med 2013; 2013:e215254.1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flachskampf FA, Gallasch J, Gefeller O, et al. Randomized trial of acupuncture to lower blood pressure. Circulation 2007; 115:3121–3129. [DOI] [PubMed] [Google Scholar]
- 12.Xiong XJ, Liu W, Yang XC, et al. Moxibustion for essential hypertension. Complement Ther Med 2014; 22:187–195. [DOI] [PubMed] [Google Scholar]
- 13.Blom K, Baker B, How M, et al. Hypertension analysis of stress reduction using mindfulness meditation and yoga: results from the harmony randomized controlled trial. Am J Hypertens 2014; 27:122–129. [DOI] [PubMed] [Google Scholar]
- 14.Xiong XJ, Li SJ, Zhang YQ. Massage therapy for essential hypertension: a systematic review. J Hum Hypertens 2014; doi: 10.1038/jhh. 2014.52. [DOI] [PubMed] [Google Scholar]
- 15.Li JJ, Lu ZL, Kou WR, et al. Impact of xuezhikang on coronary events in hypertensive patients with previous myocardial infarction from the China Coronary Secondary Prevention Study (CCSPS). Ann Med 2010; 42:231–240. [DOI] [PubMed] [Google Scholar]
- 16.Tachjian A, Maria V, Jahangir A. Use of herbal products and potential interactions in patients with cardiovascular diseases. J Am Coll Cardiol 2010; 55:515–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiong XJ, Yang XC, Liu YM, et al. Chinese herbal formulas for treating hypertension in traditional Chinese medicine: perspective of modern science. Hypertens Res 2013; 36:570–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Koh TC. Qigong: Chinese breathing exercise. Am J Chinese Med 1982; 10:86–91. [DOI] [PubMed] [Google Scholar]
- 19.Sancier KM. Therapeutic benefits of qigong exercises in combination with drugs. J Altern Complement Med 1999; 5:383–389. [DOI] [PubMed] [Google Scholar]
- 20.Lee MS, Hong SS, Lim HJ, et al. Retrospective survey on therapeutic efficacy of qigong in Korea. Am J Chinese Med 2003; 31:809–815. [DOI] [PubMed] [Google Scholar]
- 21.Lee MS, Pittler MH, Guo R, et al. Qigong for hypertension: a systematic review of randomized clinical trials. J Hypertens 2007; 25:1525–1532. [DOI] [PubMed] [Google Scholar]
- 22.Guo X, Zhou B, Nishimura T, et al. Clinical effect of qigong practice on essential hypertension: a meta-analysis of randomized controlled trials. J Altern Complement Med 2008; 14:27–37. [DOI] [PubMed] [Google Scholar]
- 23.Barrow DE, Bedford A, Ives G, et al. An evaluation of the effects of Tai Chi Chuan and Chi Kung training in patients with symptomatic heart failure: a randomised controlled pilot study. Postgrad Med J 2007; 83:717–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang CX, Xu DH, Cai MD, et al. Qigong for the treatment of hypertension complicated with coronary heart disease. Shanghai J Tradit Chin Med 1985; 19:46–49. [Google Scholar]
- 25.Chan CL, Wang CW, Ho RT, et al. A systematic review of the effectiveness of qigong exercise in cardiac rehabilitation. Am J Chin Med 2012; 40:255–267. [DOI] [PubMed] [Google Scholar]
- 26.Chen Z, Meng Z, Milbury K, et al. Qigong improves quality of life in women undergoing radiotherapy for breast cancer: results of a randomized controlled trial. Cancer 2013; 119:1690–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sun GC, Lovejoy JC, Gillham S, et al. Effects of qigong on glucose control in type 2 diabetes. Diabetes Care 2010; 33:e8.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu X, Miller YD, Burton NW, et al. A preliminary study of the effects of Tai Chi and Qigong medical exercise on indicators of metabolic syndrome, glycaemic control, health-related quality of life, and psychological health in adults with elevated blood glucose. Br J Sports Med 2010; 44:704–709. [DOI] [PubMed] [Google Scholar]
- 29.Chan AW, Lee A, Lee DT, et al. The sustaining effects of Tai chi Qigong on physiological health for COPD patients: a randomized controlled trial. Complement Ther Med 2013; 21:585–594. [DOI] [PubMed] [Google Scholar]
- 30.Lee MS, Ernst E. Qigong for movement disorders: a systematic review. Movement Disord 2009; 24:301–303. [DOI] [PubMed] [Google Scholar]
- 31.Lee MS, Pittler MH, Ernst E. Internal qigong for pain conditions: a systematic review. J Pain 2009; 10:1121–1127. [DOI] [PubMed] [Google Scholar]
- 32.Wu CY, Han HM, Huang MC, et al. Effect of qigong training on fatigue in haemodialysis patients: a non-randomized controlled trial. Complement Ther Med 2014; 22:244–250. [DOI] [PubMed] [Google Scholar]
- 33.Wang CW, Chan CH, Ho RT, et al. Managing stress and anxiety through qigong exercise in healthy adults: a systematic review and meta-analysis of randomized controlled trials. BMC Complement Altern Med 2014; 14:e8.1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang CW, Chan CL, Ho RT, et al. The effect of qigong on depressive and anxiety symptoms: a systematic review and meta-analysis of randomized controlled trials. Evid Based Complement Alternat Med 2013; 2013:e716094.1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsang HW, Cheung L, Lak DC. Qigong as a psychosocial intervention for depressed elderly with chronic physical illnesses. Int J Geriatr Psychiatry 2002; 17:1146–1154. [DOI] [PubMed] [Google Scholar]
- 36.Wang CW, Ng SM, Ho RT, et al. The effect of qigong exercise on immunity and infections: a systematic review of controlled trials. Am J Chin Med 2012; 40:1143–1156. [DOI] [PubMed] [Google Scholar]
- 37.Ng BH, Tsang HW. Psychophysiological outcomes of health qigong for chronic conditions: a systematic review. Psychophysiology 2009; 46:257–269. [DOI] [PubMed] [Google Scholar]
- 38.Freeman SR, Hanik SA, Littlejohn ML, et al. Sit, breath, smile: effects of single and weekly seated qigong on blood pressure and quality of life in long-term care. Complement Ther Clin Pract 2014; 20:48–53. [DOI] [PubMed] [Google Scholar]
- 39.Ospina MB, Bond K, Karkhaneh M, et al. Clinical trials of meditation practices in health care: characteristics and quality. J Altern Complement Med 2008; 14:1199–1213. [DOI] [PubMed] [Google Scholar]
- 40.Birdee GS, Wayne PM, Davis RB, et al. T’ai Chi and qigong for health: patterns of use in the United States. J Altern Complement Med 2009; 15:969–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wu XY, Tang JL, Mao C, et al. Systematic reviews and meta-analyses of traditional Chinese medicine must search Chinese databases to reduce language bias. Evid Based Complement Alternat Med 2013; 2013:e812179.1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xiong XJ, Liu W, Yang XC, et al. Ginkgo biloba extract for essential hypertension: a systemic review. Phytomedicine 2014; 21:1131–1136. [DOI] [PubMed] [Google Scholar]
- 43.Higgins JPT, Green S. Cochrane Reviewers’ Handbook 5.1.0 [updated March 2011], Review Manager (RevMan) [Computer program]. Version 5.1.0 www.cochrane-handbook.org. [Google Scholar]
- 44.Lee MS, Lee MS, Choi ES, et al. Effects of qigong on blood pressure, blood pressure determinants and ventilatory function in middle-aged patients with essential hypertension. Am J Chinese Med 2003; 31:489–497. [DOI] [PubMed] [Google Scholar]
- 45.Lee MS, Lim HJ, Lee MS, et al. Impact of qigong exercise on self-efficacy and other cognitive perceptual variables in patients with essential hypertension. J Altern Complement Med 2004; 10:675–680. [DOI] [PubMed] [Google Scholar]
- 46.Cheung BMY, Lo JLF, Fong DYT, et al. Randomised controlled trial of qigong in the treatment of mild essential hypertension. J Hum Hypertens 2005; 19:697–704. [DOI] [PubMed] [Google Scholar]
- 47.Lu ZC, Yu HP, Liu JW, et al. Comparative study on the therapeutic effects of a breathing exercise (qigong), jogging and drug therapy on essential hypertension. Chin J Integr Tradit West Med 1987; 7:462–464.452. [PubMed] [Google Scholar]
- 48.Liu JL, Yao SF, Zhou SF. Qigong exercise on atrial natriuretic peptides in hypertensive patients. Chin J Rehab Med 1997; 12:28–29. [Google Scholar]
- 49.Liang P. Effect of qigong on 40 cases senile hypertension. Chin Qigong 1997; 13:7. [Google Scholar]
- 50.Ma WC, Wang ZM, Wei JL. Qigong exercise on essential hypertension. Shanxi Sport Sci Technol 1999; 19:37–39. [Google Scholar]
- 51.Liu H. Effect of qigong on 53 cases of hypertensive patients. Chin Qigong 1994; 10:28–29. [Google Scholar]
- 52.Wang L. Therapeutic effect of qigong on hypertension and its complicated cardiovascular and cerebrovascular diseases. Chin Qigong 1991; 7:20–22. [Google Scholar]
- 53.Li W, Pi DR, Xing ZH, et al. Clinical study of qigong on hypertension. Tradit Chin Med Res 1994; 7:23–24. [Google Scholar]
- 54.Qian YC, Wang CX, Xu DH, et al. Discussion on the relationship between osteoporosis and kidney deficiency: effect of qigong on 40 cases of patients with hypertension in postmenopausal women. Shanghai J Tradit Chin Med 1996; 30:24–26. [Google Scholar]
- 55.Lin H, Huang SJ. Role of wuqinxi qigong in promoting rehabilitation in elderly patients with hypertension. Chin J Geriatr 2013; 33:1465–1467. [Google Scholar]
- 56.Li JP. Effect of qigong on plasma norepinephrine and serotonin in patients with essential hypertension. Chin J Sports Med 1993; 12:152–156. [Google Scholar]
- 57.Wang CX, Xu DH, Qian YC, et al. Effect of qigong on improving cardiac function of the hypertensive patients complicated with coronary heart disease. J Geriatr 1988; 8:83–88.128. [Google Scholar]
- 58.Wang CX, You CY, Zhao GS, et al. The efficacy of qigong (breathing exercise) and antihypertensive drug treatment in 426 hypertensive patients and the change of plasma dopamine-β-hydroxylase activity. Chin J Integr Tradit West Med 1982; 2: 195:218–219. [PubMed] [Google Scholar]
- 59.Wang CX, Xu DH, Qian YC, et al. Effect of qigong on the prevention of hypertensive cerebral apoplexy and its mechanism. Chin J Geriatr 1994; 14:90–92. [Google Scholar]
- 60.Li W, Pi DR, Xing ZH, et al. Effect of qigong on 150 cases hypertensive patients and microcirculation, blood rheology changes. Chin Qigong 1990; 6:22–24. [Google Scholar]
- 61.Wang CX, Xu DH, Qian YC, et al. Study on the effect of qigong on 100 cases senile hypertension and its mechanism. Chin Qigong 1989; 5:13–14. [Google Scholar]
- 62.Li HY. Effect of medical qigong combined with antihypertensive drugs on 40 cases of hypertensive patients. Chin J Integr Tradit West Med 1990; 10:608. [Google Scholar]
- 63.Yuan SX, Wang ZB, Zhu YL, et al. Effect of qigong on blood pressure and vaso-active substances in hypertension due to chronic nephritis. Acta Univ Tradit Med Pharmacol Shanghai 1996; 10:62–65. [Google Scholar]
- 64.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. J Am Med Assoc 1998; 280:1569–1575. [DOI] [PubMed] [Google Scholar]
- 65.Ernst E. The role of complementary and alternative medicine. Br Med J 2000; 321:1133–1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu X, Wu WY, Jiang BH, et al. Pharmacological tools for the development of traditional Chinese medicine. Trends Pharmacol Sci 2013; 34:620–628. [DOI] [PubMed] [Google Scholar]
- 67.Wang J, Xiong XJ. Current situation and perspectives of clinical study in integrative medicine in China. Evid Based Complement Alternat Med 2012; 2012:e268542.1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mansoor GA. Herbs and alternative therapies in the hypertension clinic. Am J Hypertens 2001; 14:971–975. [DOI] [PubMed] [Google Scholar]
- 69.Vora CK, Mansoor GA. Herbs and alternative therapies: relevance to hypertension and cardiovascular diseases. Curr Hypertens Rep 2005; 7:275–280. [DOI] [PubMed] [Google Scholar]
- 70.Ernst E. Complementary/alternative medicine for hypertension: a mini-review. Wien Med Wochenschr 2005; 123:386–391. [DOI] [PubMed] [Google Scholar]
- 71.Bell RA, Suerken CK, Grzywacz JG, et al. CAM use among older adults age 65 or older with hypertension in the United States: general use and disease treatment. J Altern Complement Med 2006; 12:903–909. [DOI] [PubMed] [Google Scholar]
- 72.Osamor PE, Owumi BE. Complementary and alternative medicine in the management of hypertension in an urban Nigerian community. BMC Complement Altern Med 2010; 10:e36.1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nuwaha F, Musinguzi G. Use of alternative medicine for hypertension in Buikwe and Mukono districts of Uganda: a cross sectional study. BMC Complement Altern Med 2013; 13:e301.1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lee MS, Hong SS, Lim HJ, et al. Retrospective survey on therapeutic efficacy of qigong in Korea. Am J Chin Med 2003; 31:809–815. [DOI] [PubMed] [Google Scholar]
- 75.Shinnick P. Qigong: where did it come from? where does it fit in science? what are the advances? J Altern Complement Med 2006; 12:351–353. [DOI] [PubMed] [Google Scholar]
- 76.Biesinger E, Kipman U, Schätz S, et al. Qigong for the treatment of tinnitus: a prospective randomized controlled study. J Psychosom Res 2010; 69:299–304. [DOI] [PubMed] [Google Scholar]
- 77.Chan JS, Ho RT, Wang CW, et al. Effects of qigong exercise on fatigue, anxiety, and depressive symptoms of patients with chronic fatigue syndrome-like illness: a randomized controlled trial. Evid Based Complement Alternat Med 2013; 2013:e485341.1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shin YI, Lee MS. Qi therapy (external qigong) for chronic fatigue syndrome: case studies. Am J Chin Med 2005; 33:139–141. [DOI] [PubMed] [Google Scholar]
- 79.Oh B, Choi SM, Inamori A, et al. Effects of qigong on depression: a systemic review. Evid Based Complement Alternat Med 2013; 2013:e134737.1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ho TJ, Christiani DC, Ma TC, et al. Effect of qigong on quality of life: a cross-sectional population-based comparison study in Taiwan. BMC Public Health 2011; 11:e546.1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tsang HW, Lee JL, Au DW, et al. Developing and testing the effectiveness of a novel health qigong for frail elders in Hong Kong: a preliminary study. Evid Based Complement Alternat Med 2013; 2013:e827392.1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Rogers CE, Larkey LK, Keller C. A review of clinical trials of tai chi and qigong in older adults. West J Nurs Res 2009; 31:245–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lee MS, Oh B, Ernst E. Qigong for healthcare: an overview of systematic reviews. J R Soc Med Sh Rep 2011; 2:e7.1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lewington S, Clarke R, Qizilbash N, et al. Prospective studies collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 85.Aronow WS, Fleg JL, Pepine CJ, et al. ACCF/AHA 2011 expert consensus document on hypertension in the elderly: a report of the American college of cardiology foundation task force on clinical expert consensus documents. Circulation 2011; 123:2434–2506. [DOI] [PubMed] [Google Scholar]
- 86.Cornelissen VA, Buys R, Smart NA. Endurance exercise beneficially affects ambulatory blood pressure: a systematic review and meta-analysis. J Hypertens 2013; 31:639–648. [DOI] [PubMed] [Google Scholar]
- 87.Johnson BT, MacDonald HV, Bruneau ML, Jr, et al. Methodological quality of meta-analyses on the blood pressure response to exercise: a review. J Hypertens 2014; 32:706–723. [DOI] [PubMed] [Google Scholar]
- 88.García-Hermoso A, Saavedra JM, Escalante Y. Effects of exercise on resting blood pressure in obese children: a meta-analysis of randomized controlled trials. Obes Rev 2013; 14:919–928. [DOI] [PubMed] [Google Scholar]
- 89.Whelton SP, Chin A, Xin X, et al. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med 2002; 136:493–503. [DOI] [PubMed] [Google Scholar]
- 90.Mellen PB, Palla SL, Goff DC, Jr, et al. Prevalence of nutrition and exercise counseling for patients with hypertension: United States, 1999 to 2000. J Gen Intern Med 2004; 19:917–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tang KC. Qigong therapy: its effectiveness and regulation. Am J Chin Med 1994; 22:235–242. [DOI] [PubMed] [Google Scholar]
- 92.Sancier KM. Medical applications of qigong. Altern Ther Health Med 1996; 2:40–46. [PubMed] [Google Scholar]
- 93.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. Br Med J 2009; 338:1245–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mao C, Chung VC, Yuan JQ, et al. Evaluation of the add-on effect of Chinese patent medicine for patients with stable or unstable angina: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2013; 2013:e673193.1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chang C. Is integrative medicine the next new frontier in medicine? Clin Rev Allergy Immunol 2013; 44:205–207. [DOI] [PubMed] [Google Scholar]
- 96.Wang J, Feng B, Yang XC, et al. Tianma gouteng yin as adjunctive treatment for essential hypertension: a systematic review of randomized controlled trials. Evid Based Complement Alternat Med 2013; 2013:e706125.1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tsang IK. Establishing the efficacy of traditional Chinese medicine. Nat Clin Pract Rheumatol 2007; 3:60–61. [DOI] [PubMed] [Google Scholar]
- 98.Bell IR, Caspi O, Schwartz GE, et al. Integrative medicine and systemic outcomes research: issues in the emergence of a new model for primary health care. Arch Intern Med 2002; 162:133–140. [DOI] [PubMed] [Google Scholar]
- 99.Wong R, Sagar CM, Sagar SM. Integration of Chinese medicine into supportive cancer care: a modern role for an ancient tradition. Cancer Treat Rev 2001; 27:235–246. [DOI] [PubMed] [Google Scholar]
- 100.Lawes CM, Hoorn SV, Rodgers A. for the International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371:1513–1518. [DOI] [PubMed] [Google Scholar]
- 101.Rossi A, Dikareva A, Bacon SL, et al. The impact of physical activity on mortality in patients with high blood pressure: a systematic review. J Hypertens 2012; 30:1277–1288. [DOI] [PubMed] [Google Scholar]
- 102.Harmsworth K, Lewith GT. Attitudes to traditional Chinese medicine amongst western trained doctors in the People's Republic of China. Soc Sci Med 2001; 52:149–153. [DOI] [PubMed] [Google Scholar]
- 103.Kinsel JF, Straus SE. Complementary and alternative therapeutics: rigorous research is needed to support claims. Annu Rev Pharmacol Toxicol 2003; 43:463–484. [DOI] [PubMed] [Google Scholar]
- 104.Vickers A, Goyal N, Harland R, et al. Do certain countries produce only positive results? A systematic review of controlled trials. Control Clin Trials 1998; 19:159–166. [DOI] [PubMed] [Google Scholar]
- 105.Lee S. Chinese hypnosis can cause qigong induced mental disorders. Br Med J 2000; 320:803. [PMC free article] [PubMed] [Google Scholar]
- 106.Ng BY. Qigong-induced mental disorders: a review. Aust N Z J Psychiatry 1999; 33:197–206. [DOI] [PubMed] [Google Scholar]
- 107.Xu SH. Psychophysiological reactions associated with qigong therapy. Chin Med J (Engl) 1994; 107:230–233. [PubMed] [Google Scholar]


