Supplemental Digital Content is available in the text
Abstract
In this study, we tried to find a safe as well as fast effective treatment for sedation and analgesia for intrathecal injection in childhood leukemia patients, relieving treatment difficulties and pain, increasing the success rate of single intrathecal injection.
The patients were divided into the experimental group (fentanyl combined with etomidate) and the control group (lidocaine only) randomly. The experimental group was given fentanyl 1 to 2 μg/kg intravenously first, then etomidate 0.1 to 0.3 mg/kg intravenously after the pipe washed. The patients younger than 1.5 years or who did not achieve satisfied sedative and analgesic situation received an additional time of etomidate (0.1–0.3 mg/kg). The patients were given oxygen at the rate of 4–5 L/min during the whole operation, and the finger pulse oximeter was used simultaneously to detect the changes in heart rate (HR) and blood oxygen saturation (SpO2). The doctors who performed the procedures assessed the quality of sedation and analgesia.
In the experimental group, the patients’ HR increased slightly after given fentanyl combined with etomidate. The patients’ SpO2 was stable. Most patients achieved a good sedative and analgesic state within 1 to 2 minutes, and no case of respiration depression or cardiac arrhythmias occurred during the whole operation. The wake-up time was 55.42 ± 20.62 min. In the control group, the patients were not very cooperative during the intrathecal injection, which made the procedures very difficult.
During intrathecal injection, pain obviously reduced and the success rate of single lumbar puncture increased. It is safe and effective to apply fentanyl combined with etomidate for sedation and analgesia.
INTRODUCTION
Owing to the progress of chemotherapy for leukemia in the last 10 years, the prognosis of acute lymphocytic leukemia (ALL) and acute myelocytic leukemia (AML) has improved significantly. However, because of the existence of the blood-brain barrier, it is hard for chemotherapeutics to pass the meninges to kill leukemia cells in the central nervous system, meaning that central nervous system leukemia (CNS-L) easily occurs. So, an essential part of acute leukemia treatment is central nervous system (CNS) prophylaxis, mostly performed by intrathecal chemotherapy. Intrathecal injection by lumbar puncture is an important way for children with leukemia to get intrathecal drug prevention and treatment of meningeal leukemia.
About 20 times of the lumbar puncture need to be done during the entire treatment. Although lumbar puncture is highly safe, this procedure may cause a lot of pain and suffering for the patients and even their parents. At the same time, multiple attempts in one procedure, failures, injury, and delays in treatment of cerebral leukemia may occur in later chemotherapy because of the pain.1–3 Furthermore, the patients’ experience of their first lumbar puncture may directly affect their acceptance of the following treatment.
Therefore, an easily applicable method to relieve the patients’ pain for intrathecal injection is urgently needed. There have been several studies about fentanyl combined with etomidate for sedation and analgesia4–7; this method was safe and effective. However, there were few studies about sedation and analgesia in children. This study will explore the effects of sedation and analgesia with fentanyl and etomidate for intrathecal injection in childhood leukemia patients.
METHODS
Patients
Fifty person-times who received fentanyl combined with etomidate and 52 person-times who received lidocaine only in the intrathecal injection among hospitalized children aged 1 to 14 years with leukemia were collected from March 1, 2013 to May 31, 2014. The patients’ parents provided informed consent before the procedures. This study was approved by the institutional review board of Kunming Children's Hospital, Kunming, Yunnan, USA.
Conditions for enrollment are as follows:
1 to 14 years of age, diagnosed of leukemia, as well as needed intrathecal injection and lumbar puncture
The parents were notified and they approved the procedures
Without the history of serious hypofunction of the heart, lung, liver, or kidney
No rachiterata or other unsuitable conditions for lumbar puncture
No sedative or analgesic drugs was used before the procedures
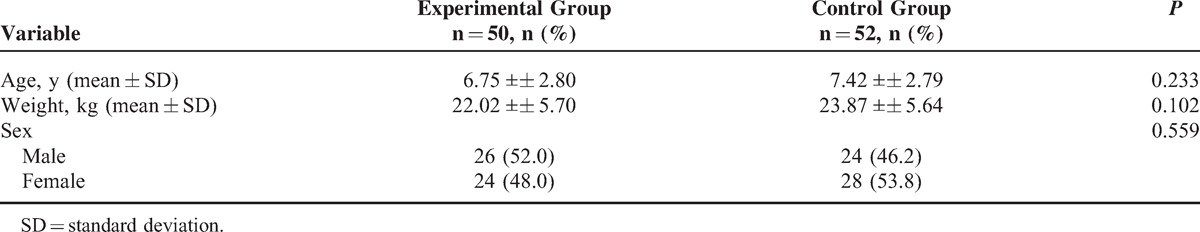
The patients were divided into the experimental group (fentanyl combined with etomidate, 50 times) and the control group (lidocaine only, 52 times) randomly. Analyzed by SPSS independent-samples t test, no significant differences were found in age, weight, or sex (P > 0.05; Table 1).
TABLE 1.
Characteristics of the Patients
Materials prepared included fentanyl, etomidate, lidocaine, epinephrine, intravenous pump, oxygen saturation (SpO2) monitor, electrocardiography monitor, cardiopulmonary resuscitation (CPR) bag, ventilator, and tracheal intubation facilities.
Application Methods
The patients’ blood pressure (BP), heart rate (HR), SpO2, and respiration were monitored the day before the operation as basic values. No food or water was allowed 1 hour before the procedure.
BP, HR, SpO2, and respiration were monitored intra-operation and post-operation.
The experimental group was given fentanyl 1 to 2 μg/kg intravenously before intrathecal injection by nurses, followed by intravenous etomidate 0.1 to 0.3 mg/kg 3 to 5 minutes later. Lumbar puncture and intrathecal injection were performed once the children achieved satisfactory sedation, in which eyebrow reflex disappeared and the muscles were relaxed. Oxygen at the rate of 4 to 5 L/min was given to the patients once they fell asleep. Pulse, respiration, and SpO2 during the whole operation were monitored. An additional etomidate 0.1 to 0.3 mg/kg could be administered until satisfactory sedation was obtained. Etomidate (150–450 μg/kg/h) was also delivered with a pump while the patients fell asleep, until the cerebrospinal fluid was collected. The patients were conveyed back to the wards after they woke up; their circulation and respiration were stable. Etomidate was discontinued in the case of SpO2 <80%. A CPR bag was available for positive pressure ventilation in cases of serious respiration depression.
The control group was given 2% lidocaine 20–40 mg, from the skin to the intervertebral ligaments for local infiltration anesthesia. Lumbar puncture and intrathecal injection were completed after that.
The observation index also included degree of sedation and analgesia, wake-up time (duration between time when the etomidate was discontinued and the time when the patients could response to questions or opened eyes [for child, preschool]). The doctors who performed the procedures assessed the degree of sedation and analgesia.
Effects of Sedation and Analgesia
Significantly Effective
The patients fell asleep and the procedures could be completed successfully; the monitoring indices, for example, respiration, pulse, and BP, were stable; the patients did not feel pain (face, legs, activity, cry, consolability [FLACC] score 0) and were cooperative during the procedures (Ramsay Sedation Score 4 or greater).8
Effective
The patients did not fall asleep, but the procedures could be completed; the monitoring indices, for example, respiration, pulse, and BP, were stable; the patients felt pain (FLACC score 1–3) and were not very cooperative during the procedures (Ramsay Sedation Score 2 or 3).8
Ineffective
The procedures could not be completed; the patients felt pain (FLACC score 4 or greater) and were not cooperative during the procedures (Ramsay Sedation Score 1).8
Statistical Analysis
The statistical analysis was performed by SPSSInc.,233SouthWackerDrive,11thFloor,Chicago,IL60606-6412.Patent number:7,023,453. software version 17.0, by the methods of Wilcoxon rank sum test, χ2, Fisher exact test, and analysis of variance, with an alpha level of 0.05. These data were expressed by X¯ ± S.
RESULTS
Effects of Sedation and Analgesia
In the experimental group, the total effective rate was 100%, and significantly effective rate was 64.00%, 36.00% for effective; whereas the total effective rate was 76.92% and ineffective rate was 23.08% in the control group. The curative effects in the experimental group were better than that in the control group significantly (Table 2, P < 0.05 by the Wilcoxon rank sum test).
TABLE 2.
Response and Sedation Quality Evaluation Scores
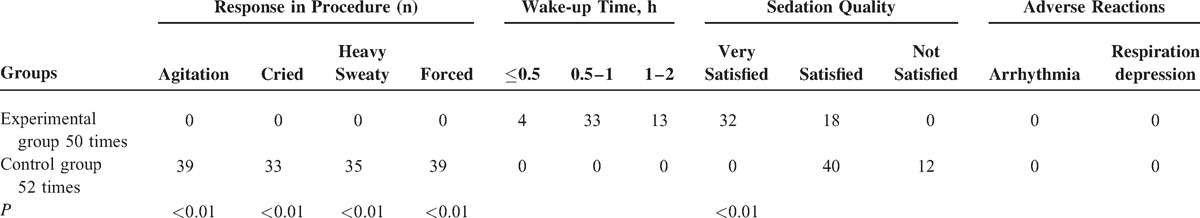
In the experimental group, 18 patients did not achieve satisfied sedation and analgesia after given fentanyl combined with etomidate. However, after given an additional etomidate (0.1–0.3 mg/kg), they all achieved satisfied situation. No additional etomidate was needed for other children. Most children waked up in 30 minutes to 1 hour. No case of respiration depression or cardiac arrhythmias occurred during the whole operation. The coordination situation of the experimental group was significantly better than that of the control group (P < 0.01 by χ2 and Fisher exact test). The experimental group (fentanyl combined with etomidate group) did not demonstrate restlessness or crying, whereas these behaviors were observed in 75% of the control group (Table 2).
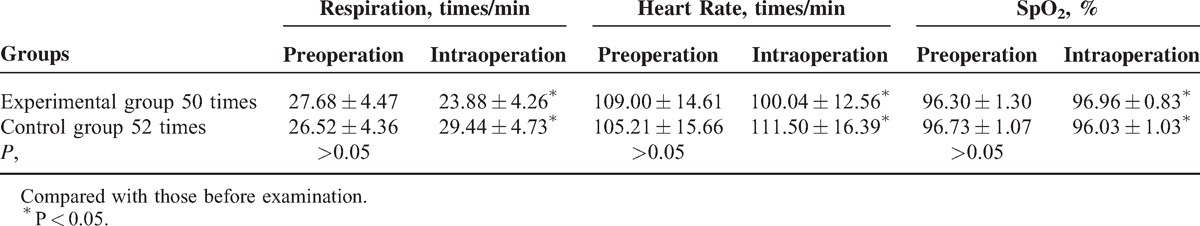
There were no significant differences between the two groups, in respiration, HR, or SpO2 before the procedure. The respiration, HR, and SpO2 changed significantly for both groups in pre-operation and intra-operation. For the experimental group, respiration and HR decreased mildly, and SpO2 increased slightly. Nevertheless, the situation is reversed in control group. However, there was no clinical significance for these changes (Table 3).
TABLE 3.
Changes in Respiration, Heart Rate, and SpO2 (X¯ ± S)
Drug Dosage and Wake-up Time
Drug dosage in the experimental group is as follows: fentanyl dosage (33.03 ± 8.55) μg, etomidate dosage (7.82 ± 1.59) mg, recovery time (50.92 ± 11.11) min (Table 4).
TABLE 4.
Drug Dosage and Wake-up Time (X¯ ± S)
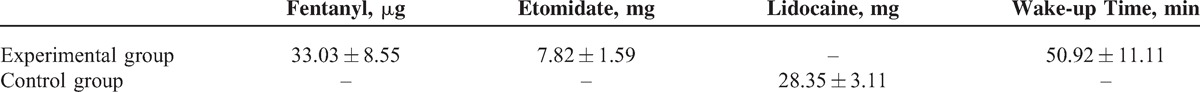
Drug dosage in the control group is as follows: 2% lidocaine dosage (28.35 ± 3.11) mg (Table 4) http://links.lww.com/MD/A139.
DISCUSSION
Various types of sedation and analgesia technique have been used during intrathecal injection procedures, such as local anesthesia (lidocaine, tetracaine hydrochloride mucilage) and general sedation (diazepam, chloral hydrate, midazolam, procaine, propofol, sevoflurane, fentanyl, and sufentanil, etc). The main problem of intravenous medication is respiration depression, whereas the local anesthesia in lumbar punctures may not work because the patients have not achieved satisfied sedation. So a safe, effective, and painless method to solve these problems is urgently needed. The fentanyl combined with etomidate achieved effective sedation and analgesia in the intrathecal injection procedures in childhood leukemia patients. No severe side effects such as respiration depression or cardiac arrhythmias were observed.
Etomidate is a short-acting intravenous anesthetic agent used for the induction of general anesthesia and for sedation for short procedures such as intrathecal injection. It is used as an anesthetic agent for its rapid action, easy dosing profile, low risk in cardiovascular, and limited suppression of ventilation. Meanwhile, it can also decrease intracranial pressure and maintain a normal arterial pressure, which may protect the function of brain. A research showed that in those patients with sepsis, one dose of the medication does not appear to affect the risk of death.9 Accordingly, etomidate could be used for sedation in childhood. It can pass the blood-brain barrier quickly, producing the phenomenon of temporary amnesia, which reduces the children's anxiety, fear, and nervousness to intrathecal injection. In addition, among general anesthesia induction drugs, etomidate is the only imidazole, and it has the most favorable therapeutic index for single bolus administration.10 The major molecular targets mediating anesthetic effects of etomidate in the central nervous system are specific γ-aminobutyric acid type A receptor subtypes.10
But etomidate does not have analgesic effects, and may even occur myoclonus. However, these adverse reactions could be effectively reduced when etomidate combined with fentanyl was used.11–12 The possible mechanism for analgesia and muscle relaxation in fentanyl may be that the drug selectively inhibited brain inhibitory pathway. By doing that, the release of facilitation neurons did not encounter resistance and enhanced excitability of skeletal muscle.13 Physicians who have experience in airway management and cardiopulmonary resuscitation will be needed when propofol is being used, which has extreme potency and cannot be reversed. Nevertheless, fentanyl does not have this problem, for it can easily be reversed.14 Meanwhile, Meredith et al15 studied propofol alone or propofol and fentanyl with the method of self-control. They found that propofol with fentanyl was associated with fewer adverse events and faster recovery. Fentanyl is opioid receptor agonist. It has a wide margin of safety, and possesses minimum effects on the cardiovascular and respiratory systems.16 So, it is an effective and safe analgesic drug. But there was a study showing that etomidate and fentanyl can independently cause bradycardia and even lead to cardiac asystole.17 So, the vital sign is still needed to be observed carefully during the sedation and analgesia using etomidate and fentanyl.
The children's pain, tension, and fear were significantly reduced by using fentanyl combined with etomidate for sedation and analgesia in intrathecal injection. Using this method increased the success rate of single intrathecal injection, and reduced the incidence of adverse effects as well. It also improved satisfaction of the children's parents by applying this method. This method is safe and effective for sedation; simultaneously, non-narcotic medical professionals can easily grasp the usage and dosage of the medicine.
Some other methods for sedation and analgesia in children have been researched by several studies. Mantadakis et al18 studied fentanyl and midazolam. They showed the combination was effective and safe. Meanwhile, there was a research that studied propofol/alfentanil and propofol/ketamine. They found that propofol/ketamine was safer than propofol/alfentanil because of the lower incidence of side effects.19 In a retrospective review of almost 32 000 people, etomidate, when used for the induction of anesthesia, was associated with a 2.5-fold increase in the risk of dying than those given propofol.20 So, perhaps propofol is more suitable for sedation in childhood leukemia patients. Lee-Jayaram et al21 studied ketamine/midazolam versus etomidate/fentanyl. They found that with its significantly shorter sedation and recovery times, K/M is more effective at reducing observed distress than E/F. Perhaps because of the small sample size, no serious adverse reactions were observed in our hospital since this method was used, such as respiration depression and arrhythmia. According to the latest procedural sedation and analgesia in children,22 supplemental oxygen should be recommended before and during sedation, especially in pediatric patients, owing to their greater susceptibility to hypoxemia. Anesthesiologists and nonanesthesiologists need to work together to achieve a safe and effective sedation and analgesia.23 To easily observe the outcome, some studies suggest that electrosympathicograph24 and electroencephalograph25 can be used in estimating sedation and analgesia. This may make it easier for sedation and analgesia in pediatrics, needing lesser doctors. It is more suitable for some countries that have patients far more than doctors, especially like China. Further study is needed to find a better method for sedation and analgesia reducing the pain brought by intrathecal injection.
Footnotes
Abbreviations: ALL = acute lymphocytic leukemia, AML = acute myelocytic leukemia, BP = blood pressure, CPR = cardiopulmonary resuscitation, EEG = electroencephalographical, ESG = electro-sympathicograph, HR = heart rate, SpO2, oxygen saturation.
Research supported by the Scientific Research Foundation of Yunnan Province, China (#2013EZ246).
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Barbi E, Badina L, Marchetti F, et al. Attitudes of children with leukemia toward repeated deep sedations with propofol. J Pediatr Hematol Oncol 2005; 27:639–643. [DOI] [PubMed] [Google Scholar]
- 2.Nagel K, Willan AR, Lappan J, et al. Pediatric oncology sedation trial (POST): A double-blind randomized study. Pediatr Blood Cancer 2008; 51:634–638. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen M, Vandenbroucke F, Roy JD, et al. Evaluation of the addition of bupivacaine to intrathecal morphine and fentanyl for postoperative pain management in laparascopic liver resection. Reg Anesth Pain Med 2010; 35:261–266. [DOI] [PubMed] [Google Scholar]
- 4.Zhang GH, Sun L. Peri-intubation hemodynamic changes during low dose fentanyl, remifentanil and sufentanil combined with etomidate for anesthetic induction. Chin Med J (Engl) 2009; 122:2330–2334. [PubMed] [Google Scholar]
- 5.Wu J, Yao S, Wu Z, et al. A comparison of anesthetic regimens using etomidate and propofol in patients undergoing first-trimester abortions: double-blind, randomized clinical trial of safety and efficacy. Contraception 2013; 87:55–62. [DOI] [PubMed] [Google Scholar]
- 6.Isitemiz I, Uzman S, Toptaş M, et al. Prevention of etomidate-induced myoclonus: Which is superior: Fentanyl, midazolam, or a combination? A Retrospective comparative study. Med Sci Monit 2014; 20:262–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ko BJ, Oh JN, Lee JH, et al. Comparison of effects of fentanyl and remifentanil on hemodynamic response to endotracheal intubation and myoclonus in elderly patients with etomidate induction. Korean J Anesthesiol 2013; 64:12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xin T, Jingquan L, Yuanping T, et al. Research on analgesia intrathecal injection in acute leukemia among children. Clin Med Engineer 2010; 17:43–45. [Google Scholar]
- 9.Gu WJ, Wang F, Tang L, et al. Single-dose etomidate does not increase mortality in patients with sepsis: a systematic review and meta-analysis of randomized controlled trials and observational studies. Chest 2014. [DOI] [PubMed] [Google Scholar]
- 10.Forman SA. Clinical and molecular pharmacology of etomidate. Anesthesiology 2011; 114:695–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van den Broek WW, Groenland TH, Kusuma A, et al. Double-blind placebo controlled study of the effects of etomidate-alfentanil anesthesia in electroconvulsive therapy. J ECT 2004; 20:107–111. [DOI] [PubMed] [Google Scholar]
- 12.Hueter L, Schwarzkopf K, Simon M, et al. Pretreatment with sufentanil reduces myoclonus after etomidate. Acta Anaesthesiol Scand 2003; 47:482–484. [DOI] [PubMed] [Google Scholar]
- 13.Jian L. The clinical observation of etomidate combined with fentanyl for intravenous anesthesia. Jilin Med J 2013; 34:1688–1689. [Google Scholar]
- 14.Ray NP. Pediatric “sedation” protocols: exchanging old problems for new ones. J Pediatr Hematol Oncol 2008; 30:117–118. [DOI] [PubMed] [Google Scholar]
- 15.Cechvala MM, Christenson D, Eickhoff JC, et al. Sedative preference of families for lumbar punctures in children with acute leukemia: propofol alone or propofol and fentanyl. J Pediatr Hematol Oncol 2008; 30:142–147. [DOI] [PubMed] [Google Scholar]
- 16.Kukanich B, Clark TP. The history and pharmacology of fentanyl: relevance to a novel, long-acting transdermal fentanyl solution newly approved for use in dogs. J Vet Pharmacol Ther 2012; 35 Suppl 2:3–19. [DOI] [PubMed] [Google Scholar]
- 17.Setty S, Kumar AB. Asystole on anesthesia induction in adults: don’t blame the Succinylcholine alone. Minerva Anestesiol 2012; 78:258–259. [PubMed] [Google Scholar]
- 18.Mantadakis E, Katzilakis N, Foundoulaki E, et al. Moderate intravenous sedation with fentanyl and midazolam for invasive procedures in children with acute lymphoblastic leukemia. J Pediatr Oncol Nurs 2009; 26:217–222. [DOI] [PubMed] [Google Scholar]
- 19.Chiaretti A, Ruggiero A, Barone G, et al. Propofol/alfentanil and propofol/ketamine procedural sedation in children with acute lymphoblastic leukaemia: safety, efficacy and their correlation with pain neuromediator expression. Eur J Cancer Care (Engl) 2010; 19:212–220. [DOI] [PubMed] [Google Scholar]
- 20.Komatsu R, You J, Mascha EJ, et al. Anesthetic induction with etomidate, rather than propofol, is associated with increased 30-day mortality and cardiovascular morbidity after noncardiac surgery. Anesth Analg 2013; 117:1329–1337. [DOI] [PubMed] [Google Scholar]
- 21.Lee-Jayaram JJ, Green A, Siembieda J, et al. Ketamine/midazolam versus etomidate/fentanyl procedural sedation for pediatric orthopedic reductions. Pediatr Emerg Care 2010; 26:408–412. [DOI] [PubMed] [Google Scholar]
- 22.Golzari SE, Soleimanpour H, Najafi M. Procedural sedation and analgesia in children. N Engl J Med 2014; 371:90–91. [DOI] [PubMed] [Google Scholar]
- 23.Bartkowska-Śniatkowska A1, Rosada-Kurasińska J, Zielińska M, et al. Procedural sedation and analgesia for gastrointestinal endoscopy in infants and children: how, with what, and by whom? Anaesthesiol Intensive Ther 2014; 46:109–115. [DOI] [PubMed] [Google Scholar]
- 24.Winterhalter M, Münte S, Gerhard M, et al. Prospective study comparing skin impedance with eeg parameters during the induction of anaesthesia with fentanyl and etomidate. Eur J Med Res 2010; 15:47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van der Linde HJ, Van Deuren B, Somers Y, et al. EEG in the FEAB model: Measurement of electroencephalographical burst suppression and seizure liability in safety pharmacology. J Pharmacol Toxicol Methods 2011; 63:96–101. [DOI] [PubMed] [Google Scholar]


