Abstract
Dietary patterns are a risk factor for metabolic syndrome (MetS). The prevalence of MetS has increased in Korea, and this condition has become a public health issue. Therefore, the present cross-sectional study aimed to identify the associations between dietary patterns and the risk of MetS among Korean women.
The data of 5189 participants were analyzed to determine dietary intake and lifestyle. A principal components analysis was employed to determine participant dietary patterns with regard to 106 food items. MetS was diagnosed using the National Cholesterol Education Program, Adult Treatment Panel III. Logistic regression analyses were applied to evaluate the associations between dietary pattern quintiles and MetS and to generate odds ratios (ORs) and 95% confidence intervals (CIs) after adjusting for potential confounders.
Three dietary patterns were identified: “traditional,” “western,” and “prudent.” The “prudent” dietary pattern consisted of a high intake of fruits and fruit products as well as nuts, dairy, and a low consumption of grains; this pattern was negatively associated with the risk of MetS. The highest quintile of the “prudent” dietary pattern was significantly less likely to develop MetS (OR: 0.5, 95% CI: 0.36–0.68, P for trend <0.001) compared with the lowest quintile. This pattern was also negatively associated with all of the MetS diagnostic criteria: abdominal obesity (OR: 0.52, 95% CI: 0.41–0.65), blood pressure (OR: 0.72, 95% CI: 0.59–0.87), triglycerides (OR: 0.67, 95% CI: 0.52–0.85), fasting glucose (OR: 0.64, 95% CI: 0.43–0.95), and high-density lipoprotein cholesterol (OR: 0.53, 95% CI: 0.42–0.68). However, the “traditional” and “western” dietary patterns were not associated with the risk of MetS.
The “prudent” dietary pattern was negatively associated with the risk of developing MetS among Korean women.
INTRODUCTION
Dietary patterns and nutritional intake influence the development and progress of diseases such as metabolic syndrome (MetS).1–3 MetS is a typical degenerative disorder characterized by the combination of abdominal obesity, dyslipidemia, hypertension, and insulin resistance.4 MetS is therefore associated with an increased risk for cardiovascular disease and diabetes mellitus as well as with general morbidity and mortality.5
The increasing prevalence of MetS is especially evident in Asia.3,6 According to the Chinese National Nutrition and Health Survey, the prevalence of MetS was 13.8% in 2002.7 However, this prevalence increased to 27.4% in 2010, although that was at a regional level.8 A rapid increase in the incidence of MetS from 24.9% to 37% was observed from 1998 to 2012 in Korea, causing MetS to become a public health issue.9,10 Although multiple risk factors (eg, metabolic and genetic components) must be considered to account for this emerging health problem,11,12 the increasing prevalence of MetS might stem from changes in dietary patterns and nutritional intake.1 Over the past several decades, dietary patterns and levels of nutritional intake have changed with the development of food industries and westernization. Trends toward the increased consumption of red meat, fat, and sodium and the insufficient intake of vegetables and fruits13 have occurred, and these trends might be associated with the increased prevalence of MetS.
The traditional Korean diet is likely protective against MetS because it consists of a large portion of vegetables and is lower in fat than the western diet.14,15 Recent studies are not consistent with this notion, however, noting that the traditional dietary pattern did not significantly lower the prevalence of MetS; rather, it increased the risk.16–18 In addition, noble dietary patterns that consist of a variety of food items have been recently observed, and their association with MetS has been investigated.16,18,19 These findings suggest that the association between dietary patterns and MetS in Korea remains unclear, and additional studies are needed to clarify this area of research. Therefore, the present study aimed to determine the association between dietary patterns and the risk of MetS among Korean women.
METHODS
Study Subjects
This research was designed as a cross-sectional study. A total of 5931 female participants were recruited from a health screening examination (a benefit program of the National Health Insurance) at the National Cancer Center in the Republic of Korea between September 2007 and December 2014. All of the participants volunteered for the study and agreed to provide data for the survey questions, including their medical histories, clinical test results, and dietary habits. Participants whose medical records were not available (n = 659) or who reported implausible energy intakes (<500 or ≥4000 kcal, n = 83) were excluded from this study. However, no one was excluded because of other medical issues, including diabetes, stroke, coronary disease, or cancer. The remaining 5189 participants were aged between 31 and 70, and their data were analyzed (Figure 1). The institutional review board provided ethical approval before the commencement of the research (No. NCCNCS-07-077), and all of the participants provided informed consent before participating in the study.
FIGURE 1.
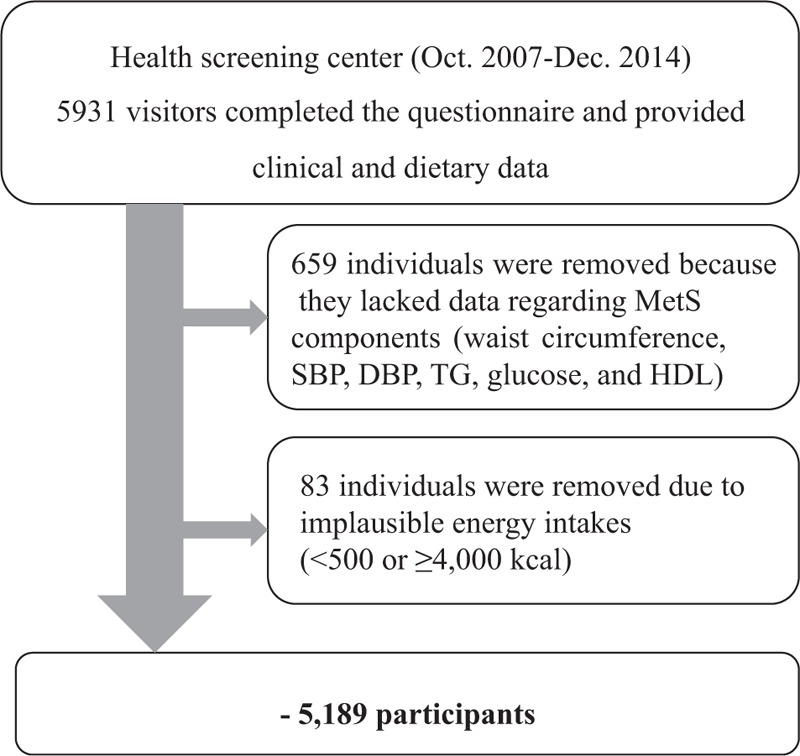
Flow chart of the participant selection process. DBP = diastolic blood pressure, HDL = high-density lipoprotein, SBP = systolic blood pressure, TG = triglyceride.
Data Collection
The participants completed a self-administered questionnaire designed to evaluate each participant's demographics (eg, age, education, household income, and marital status), lifestyle (eg, cigarette smoking, alcohol consumption, and regular physical activity), medical history and diet on the day of the examination. A validated food frequency questionnaire (FFQ) was applied to determine dietary intake. The FFQ classifies 106 food items into 37 groups based on their nutrient profiles and culinary uses. To examine the average consumption of each food item over the last year, 3 portion sizes (eg, small, medium, and large) and 9 degrees of frequency (eg, never or rarely, once a month, 2 or 3 times a month, once or twice a week, 3 or 4 times a week, 5 or 6 times a week, once a day, twice a day, and 3 times a day) were presented. Height and weight of each subject were determined using the InBody 370 (Biospace, Seoul, Korea). Body mass index (BMI) was computed as weight (kg) divided by the square of the height (m). Waist circumference was measured at the umbilical level using a measuring tape (Tech-Med model 4414; Moore Medical Corp., New Britain, CT). Blood pressure was measured using an automatic blood pressure monitor (FT-200S, Jawon Medical, Kyungsan, Korea). Blood samples for biochemical analyses were collected from participants by venipuncture following 8 hours of fasting. Levels for triglyceride (TG) and high-density lipoprotein (HDL) cholesterol (Kyowa Medex, Tokyo, Japan), and fasting glucose (Denka Seiken, Tokyo, Japan) were determined using a Chemistry Analyzer (TBA-200FR, Toshiba, Tokyo, Japan).
Metabolic Syndrome Diagnosis
MetS, with the exception of abdominal obesity, was defined using the National Cholesterol Education Program Adult Treatment Panel III.20 Waist circumference was determined using Asian guidelines.21 The participants were diagnosed with MetS if they had 3 or more of the following risk conditions: waist circumference of ≥80 cm; systolic blood pressure (SBP) of ≥130 mm Hg and a diastolic blood pressure (DBP) of ≥85 mm Hg; TG count of ≥150 mg/dL; fasting blood glucose level of ≥110 mg/dL or medicine therapy for glucose level; and HDL cholesterol level of <50 mg/dL.
Analyses of Dietary Patterns and Nutritional Intakes
To extract the participants’ dietary patterns, a principal components analysis (PCA; PROC FACTOR) was conducted. The analyzed factors were adjusted using a varimax rotation to improve data interpretability. The eigenvalues, scree plot, and interpretability were taken into account to determine the number of retained factors with regard to dietary patterns. The factor score for individual dietary patterns was grouped by quintiles for further analysis. In addition, to understand the characteristics of the identified dietary patterns, analyses for nutritional intake based on the dietary patterns were performed using CAN-PRO 4.0 (Computer Aided Nutritional Analysis Program, The Korean Nutrition Society, Seoul, Korea). Vitamins B1, B2, B6, C, E, and folate as well as sodium, potassium, iron, calcium, and fiber intakes were particular concerns, as were energy, carbohydrates, proteins, and lipids because previous studies have shown that these nutrients are associated with MetS risk, and they benefit human health.3,22
Statistical Analyses
Student t tests and Chi-square tests were performed to compare continuous and categorical variables, respectively. Binominal logistic regression models with a log scale for each dietary pattern score were used to estimate the odds ratios (ORs) and 95% confidence intervals (CIs) across quintiles. The trend tests for the association between each of the dietary patterns and MetS and the comparison of nutritional intakes across quintiles were examined using a general linear model adjusted for confounding factors. All statistical analyses were performed using SAS version 9.3 (SAS Institute, Inc., Cary, NC). All reported P-values were associated with 2-tailed hypotheses with 95% CIs.
RESULTS
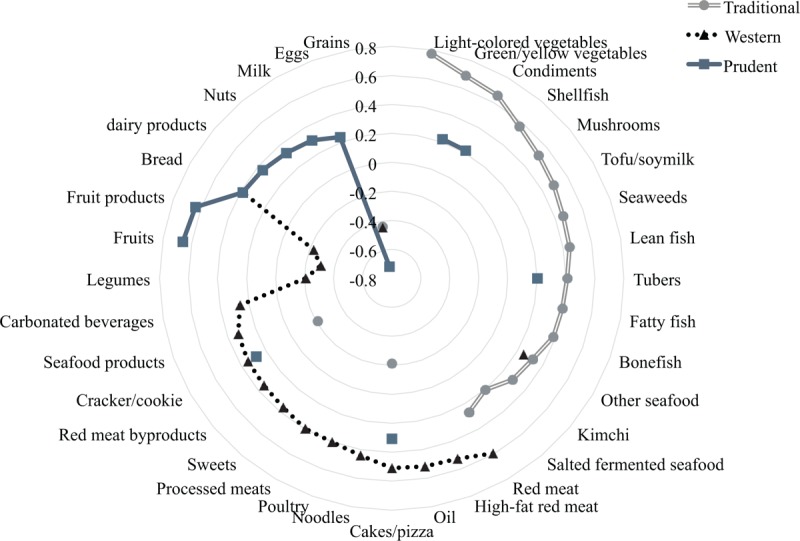
Table 1 provides the general participant characteristics by MetS phenotype. The prevalence of MetS was 11.4% in the study population. The participants with MetS were older and had higher BMIs than the control subjects (P < 0.001). Significant differences were also observed between the MetS phenotypes with regard to socioeconomic variables. The patients with MetS were less likely to be married (P < 0.01) or educated (P < 0.001), and they had less income (P < 0.001) than the healthy controls. The ratio of nondrinkers in MetS subjects was higher than controls (P < 0.001). However, participants without MetS were more engaged in regular physical activity (P = 0.02). These variables might be associated with the incidence of MetS; thus, they were considered as potential confounders in subsequent analyses. All biochemical indices for MetS significantly differed between the absence and presence of MetS (all P < .001).
TABLE 1.
General Characteristics of Study Population and Comparison for Subjects With and Without Metabolic Syndrome
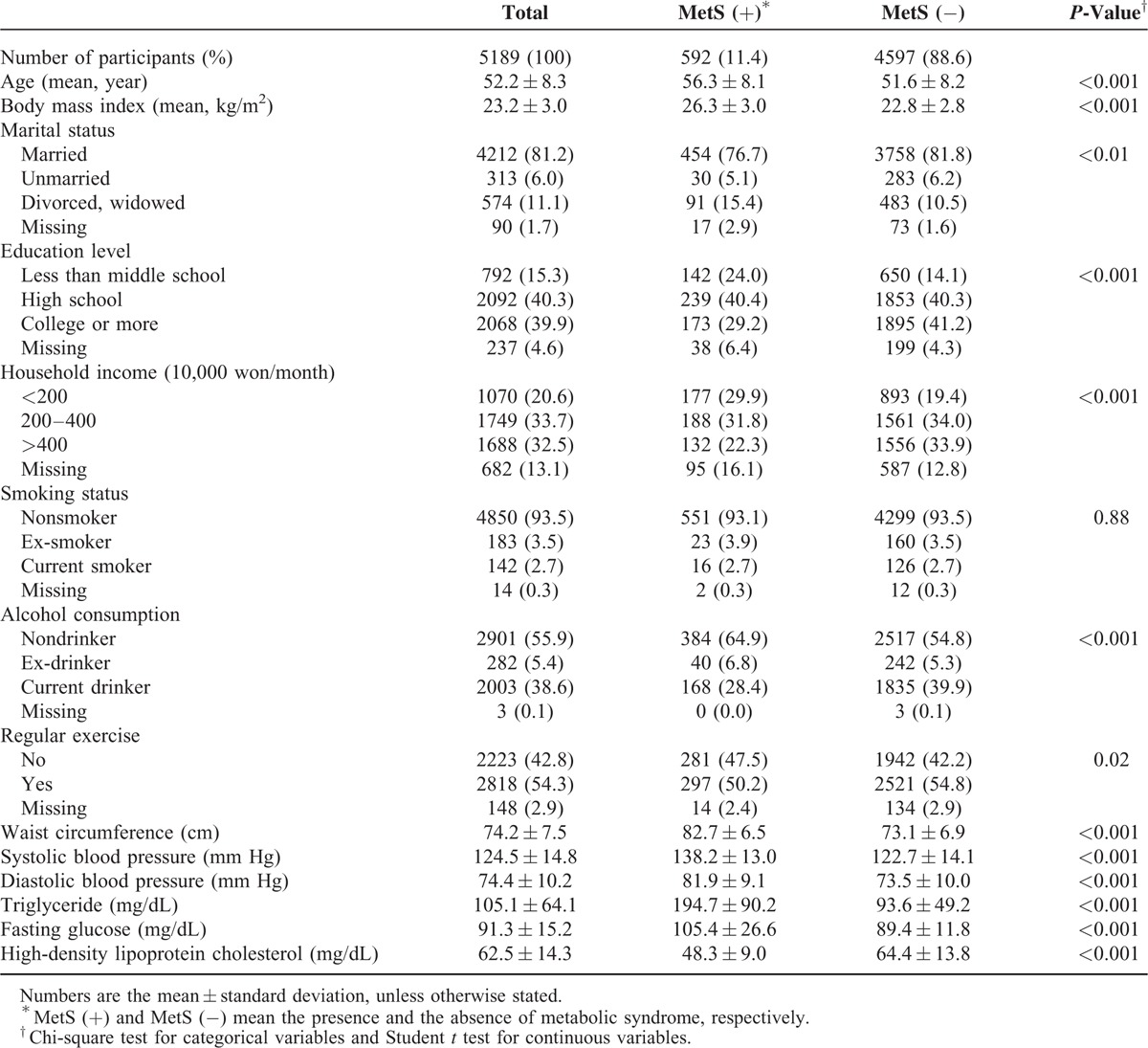
The dietary patterns and factor loadings derived from the PCA are presented in Figure 2. Three dietary patterns were identified that explained 24.7% of the total variance. The “traditional” dietary pattern was characterized by a high intake of traditional food items regularly consumed in Korea, such as vegetables, condiments, shellfish, mushrooms, seaweed, fish, tubers, and kimchi. The “western” dietary pattern was characterized by high intake of general foods found in western diets, such as red meat, oil, cake/pizza, noodles, poultry, processed meats, bread, and sweets and by low intake of grain. The “prudent” dietary pattern was characterized by low consumption of grains and by high intake of fruits and fruit products as well as bread, dairy products, nuts, cake/pizza, and milk.
FIGURE 2.
Factor loading diagram for the 3 major dietary patterns identified using a factor analysis. Factor loadings of <|0.20| were not listed for simplicity; the traditional, western, and prudent dietary patterns explained 11.5%, 7.8%, and 5.4% of the variance, respectively.
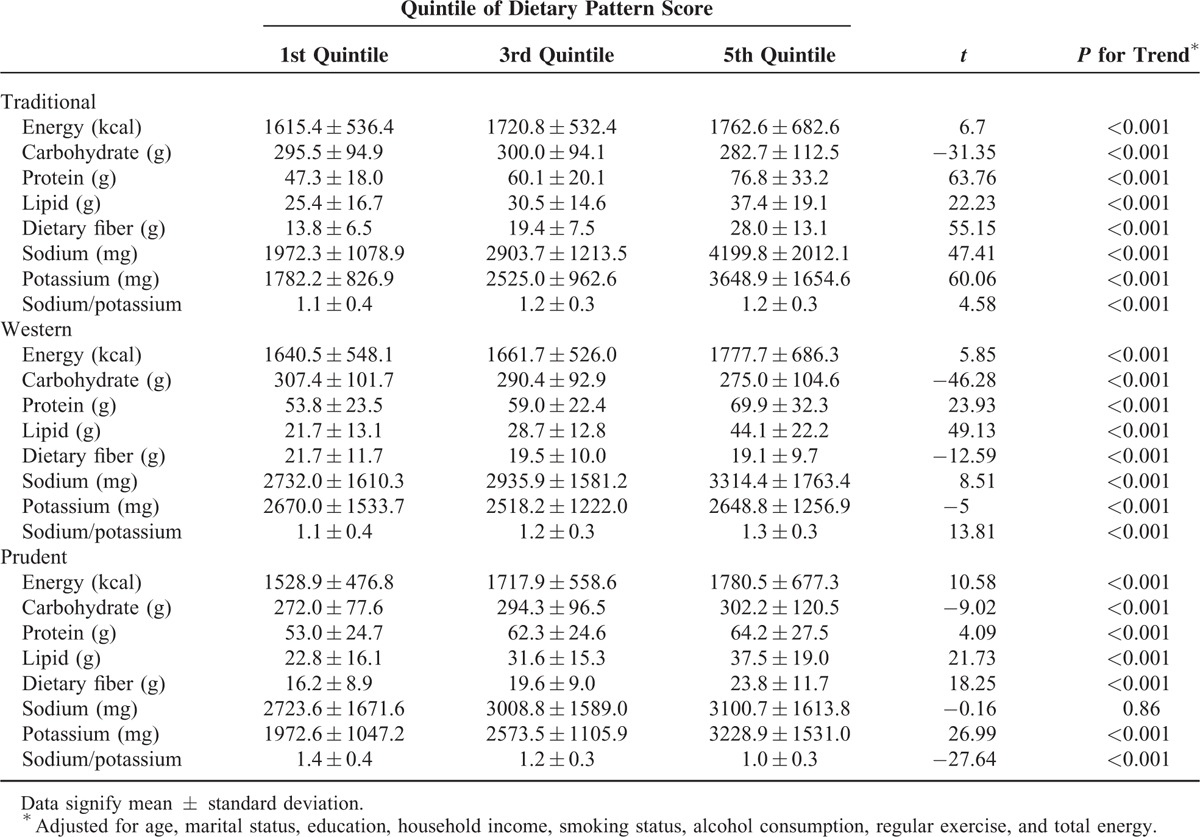
Table 2 shows the nutritional intakes of the participants according to quintiles of the factor scores for each dietary pattern. After controlling for potential confounders, the dietary levels of the examined vitamins, calcium, and iron were increased with factor scores in the “traditional” and “prudent” dietary patterns (data not shown). However, the average intakes of dietary sodium and potassium showed differential trends with regard to the factor scores depending on the dietary patterns. In the “prudent” dietary pattern, dietary sodium levels did not increase with factor scores (P = 0.86), whereas potassium was positively associated with the factor scores, resulting in decreased dietary sodium-to-potassium ratios across the quintiles (1.4 and 1.0 for the lowest and highest quintiles, respectively, P < 0.001). However, the ratios were elevated for both the “traditional” and “western” dietary patterns (P < 0.001). In the “western” dietary pattern, vitamin C, folate, fiber, and potassium intakes were negatively associated with the factor scores (P < 0.001). Carbohydrate intake decreased with the factor scores for all dietary patterns (P < 0.001).
TABLE 2.
Nutrient Intake of the Study Participants According to the Quintile of Factor Scores for Each Dietary Pattern
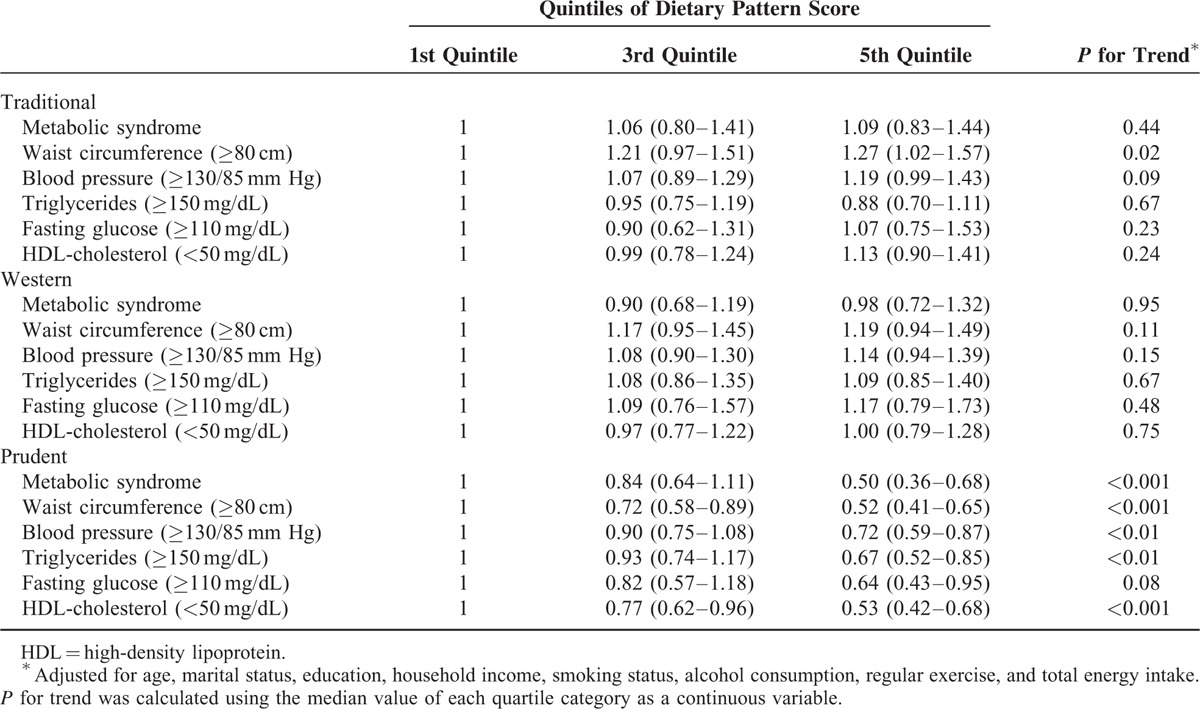
Logistic regression analyses adjusting for potential confounders clearly showed that the dietary patterns were associated with the risk for MetS (Table 3). The highest quintile of the “prudent” dietary pattern was significantly associated with a reduced risk for of developing MetS (OR: 0.5, 95% CI: 0.36–0.68, P for trend <0.001) compared with the lowest quintile. This positive effect of the highest quintile of the “prudent” dietary pattern was also evident with regard to all of the diagnostic criteria for MetS (OR: 0.52, 95% CI: 0.41–0.65 for waist circumference; OR: 0.72, 95% CI: 0.59–0.87 for blood pressure; OR: 0.67, 95% CI: 0.52–0.85 for TG; OR: 0.64, 95% CI: 0.43–0.95 for fasting glucose; and OR: 0.53, 95% CI: 0.42–0.68 for HDL cholesterol). However, the “traditional” and “western” dietary patterns were not associated with the risk of developing MetS. A high intake of the “traditional” dietary pattern was only associated with an increased risk of abdominal obesity (OR: 1.27, 95% CI: 1.02–1.57).
TABLE 3.
Odds Ratios and 95% Confidence Intervals for Metabolic Syndrome and Its Components According to Quintiles of Dietary Pattern Score
DISCUSSION
Dietary pattern is a risk factor for MetS. This cross-sectional study examined various dietary patterns and their associations with MetS risk among Korean women. Three dietary patterns were identified. The “prudent” dietary pattern was negatively associated with the risk for MetS, whereas the “traditional” and “western” dietary patterns did not show any significant association with MetS.
The foods identified in the “prudent” dietary pattern (eg, fruits, dairy products, nuts, bread, and milk) might not be typical of either the traditional Korean or western diets. Since the 1970s, an increasing prevalence of typical features of the western diet (eg, reduced intakes of vegetables and grains but high intakes of fat, sugar, and red meat) has been observed in Korea.13 However, a noble dietary pattern including a high intake of fruits and dairy products with low sugar consumption was also identified beginning in the late 1990s.13,23 The prevalence of this new dietary pattern doubled between 1998–1999 and 2009–2010, whereas that of the western dietary pattern declined over the same period.13 These recent changes in dietary patterns might reflect the public's concern for improved well-being. The association between degenerative chronic diseases and the western diet has been well studied.24 The western diet is known to be associated with elevated incidence of colorectal cancer,25 atherosclerosis,26 hypertension,27 and MetS.28,29 Compared to the western diet, the traditional Korean diet is highlighted as it consists of a variety of vegetables and is low in fat. However, problems with the traditional Korean diet, including high sodium and carbohydrate intakes, have also been reported.16,18 National campaigns and information from the mass media with respect to maintaining a healthy diet may increase individuals’ awareness of the issues with the western and Korean traditional diets as well as about the benefits of foods associated with the “prudent” dietary pattern. Thus, the prevalence of the “prudent” dietary pattern might increase; the present study showed that it achieved its primary goal of maintaining health and reducing disease risk. The “prudent” dietary pattern was significantly associated with a reduced risk for MetS. The protective effect of a high intake of the “prudent” dietary pattern was also evident with regard to each MetS criterion: abdominal obesity, hypertension, dyslipidemia, and fasting glucose level.
The protective effect of the foods in the “prudent” dietary pattern has been suggested previously. Diets high in fruits, vegetables, dairy, and nuts are negatively associated with the risk of MetS.30,31 According to the “Dietary Approaches to Stop Hypertension (DASH)” trial, diets rich in fruits and fruit products as well as in vegetables, low-fat dairy, and nuts reduced DBP and SBP compared with a control diet by an average of 5.5 and 3.0 mm Hg, respectively.32 Adherence to the DASH diet for 8 weeks also decreased weight, BMI, serum TG, and very-low-density lipoprotein cholesterol levels, whereas increased concentrations of plasma total antioxidant capacity and total glutathione were detected.33 The precise mechanisms for the positive effects of these foods remain unclear.22 However, the high consumption of fiber, vitamins, and minerals might lower the risk for high blood pressure and MetS. In addition, antioxidants and other undefined functional compounds may be involved in these mechanisms. The reduced intake of grains might also contribute to the protective effect of the “prudent” dietary pattern. Dietary carbohydrates possess differential effects on the risk of MetS depending on their source and type, and refined grains (including white rice) elevated the risk of MetS among Korean women compared with other carbohydrate sources.34 In line with this research, reduced-grain carbohydrates in the “prudent” dietary pattern might decrease the risk for MetS.
The findings regarding dietary sodium and potassium as well as their decreased ratio support the beneficial effects of “prudent” dietary pattern against MetS. A high sodium intake has long been considered to be associated with increasing SBP and DBP as well as hypertension via the stiffening of the endothelial wall, a perturbation in resistance of the arteries and nitric oxide-releasing mechanisms.35,36 Studies have also shown that a high sodium intake is associated with increased insulin resistance37 and waist circumference in women38; furthermore, reduced dietary sodium improves lipid profiles.39 A low intake of potassium is also a risk factor for elevated blood pressure and hypertension given contrasting effects of potassium and sodium in cellular mechanisms.40 Therefore, reducing sodium, increasing potassium intake, or both are nutritional approaches recommended in preventing hypertension, cardiovascular disease, and MetS.
A growing number of studies suggest that the sodium-to-potassium ratio is strongly associated with blood pressure and cardiovascular disease mortality. A larger such ratio is associated with the risk of hypertension, and this effect is more significant than that of each nutrient alone.41–43 Fruits and fruit products as well as nuts and dairy products (except for cheese), which largely comprise the “prudent” dietary pattern, have a low sodium-to-potassium ratio.44 Furthermore, fruits and their products as well as nuts, dairy products, and milk are generally consumed without condiments (sources of added sodium) in Korean cuisine. Therefore, the decreased sodium-to-potassium ratio caused by the high intake of these foods might also contribute the positive effects of the “prudent” dietary pattern.
In the present study, neither the “traditional” nor the “western” dietary pattern was associated with MetS. As mentioned above, traditional Korean and western diets are generally accepted as having contrasting effects on the risk for MetS: The traditional diet might be protective, but the western diet might increase the risk for MetS.28,29 However, recent studies have reported that neither dietary pattern showed associations with regard to MetS prevalence,16,45 and the risk of the western diet was evident only among males.1,24 Gender-specific effects, differential factor loadings, or both might have led to this discrepancy. In addition, because nutrients are consumed in combination and are highly interrelated, the interactions among nutrients might counter or modify the effect of the foods in the dietary patterns. For instance, the high consumption of condiments from the “traditional” dietary pattern increases sodium intake and the sodium-to-potassium ratio, thereby nullifying the benefits of the traditional pattern. This effect might lead to the lack of an association between that dietary pattern and MetS and show a negative effect with regard to abdominal obesity. Additional studies are required to verify this complex relationship in greater detail.
This study found an interesting association between dietary patterns and MetS risk among Korean women; however, certain limitations exist. Because this study was cross-sectional, temporality, and ambiguous causality between dietary intake and health status may exist. In addition, the participants volunteered for the health screening examination, which shows that these participants had concerns for a healthier lifestyle, which might have led to a lower prevalence of MetS in the present research compared with previous studies. Lastly, the 3 dietary patterns identified using PCA may not account for all dietary patterns in Korean because they explained approximately 24.7% of the total variation. Therefore, the associations identified in the present study should be interpreted with caution.
In summary, the present study identified 3 dietary patterns: “traditional,” “western,” and “prudent.” The “prudent” dietary pattern is characterized by high consumption of fruits, fruit products, dairy products, and nuts as well as low intake of grains; this pattern was negatively associated with the likelihood of having MetS among Korean women. However, the “traditional” and “western” dietary patterns did not significantly influence on the likelihood of developing MetS.
Acknowledgment
A research grant from the National Cancer Center, Republic of Korea (Ref. No. 1510040) supported this work.
Footnotes
Abbreviations: BMI = body mass index, CI = confidence interval, DASH = Dietary Approaches to Stop Hypertension, DBP = diastolic blood pressure, FFQ = food frequency questionnaire, HDL = high-density lipoprotein, MetS = metabolic syndrome, OR = odds ratio, PCA = principal components analysis, SBP = systolic blood pressure, TG = triglyceride.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Woo HD, Shin A, Kim J. Dietary patterns of Korean adults and the prevalence of metabolic syndrome: a cross-sectional study. PLoS One 2014; 9:e111593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pimenta AM, Toledo E, Rodriguez-Diez MC, et al. Dietary indexes, food patterns and incidence of metabolic syndrome in a Mediterranean cohort: the SUN project. Clin Nutr 2015; 34:508–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bian S, Gao Y, Zhang M, et al. Dietary nutrient intake and metabolic syndrome risk in Chinese adults: a case-control study. Nutr J 2013; 12:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hanley AJ, Karter AJ, Williams K, et al. Prediction of type 2 diabetes mellitus with alternative definitions of the metabolic syndrome: the Insulin Resistance Atherosclerosis Study. Circulation 2005; 112:3713–3721. [DOI] [PubMed] [Google Scholar]
- 5.Wang J, Ruotsalainen S, Moilanen L, et al. The metabolic syndrome predicts cardiovascular mortality: a 13-year follow-up study in elderly non-diabetic Finns. Eur Heart J 2007; 28:857–864. [DOI] [PubMed] [Google Scholar]
- 6.Ramachandran A, Snehalatha C, Shetty AS, et al. Trends in prevalence of diabetes in Asian countries. World J Diabetes 2012; 3:110–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hu SS, Kong LZ, Gao RL, et al. Outline of the report on cardiovascular disease in China, 2010. Biomed Environ Sci 2012; 25:251–256. [DOI] [PubMed] [Google Scholar]
- 8.Song QB, Zhao Y, Liu YQ, et al. Sex difference in the prevalence of metabolic syndrome and cardiovascular-related risk factors in urban adults from 33 communities of China: the CHPSNE study. Diab Vasc Dis Res 2015; 12:189–198. [DOI] [PubMed] [Google Scholar]
- 9.Lim S, Shin H, Song JH, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998–2007. Diabetes Care 2011; 34:1323–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Won KB, Chang HJ, Niinuma H, et al. Inverse association between central obesity and arterial stiffness in Korean subjects with metabolic syndrome: a cross-sectional cohort study. Diabetol Metab Syndr 2015; 7:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jeong SW, Chung M, Park SJ, et al. Genome-wide association study of metabolic syndrome in Koreans. Genomics Inform 2014; 12:187–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Litvinova L, Atochin DN, Fattakhov N, et al. Nitric oxide and mitochondria in metabolic syndrome. Front Physiol 2015; 6:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim H, Kim SY, Wang Y, et al. Preservation of a traditional Korean dietary pattern and emergence of a fruit and dairy dietary pattern among adults in South Korea: secular transitions in dietary patterns of a prospective study from 1998 to 2010. Nutr Res 2014; 34:760–770. [DOI] [PubMed] [Google Scholar]
- 14.Lee KW, Cho MS. The traditional Korean dietary pattern is associated with decreased risk of metabolic syndrome: findings from the Korean National Health and Nutrition Examination Survey, 1998–2009. J Med Food 2014; 17:43–56. [DOI] [PubMed] [Google Scholar]
- 15.Kim J, Jo I. Grains, vegetables, and fish dietary pattern is inversely associated with the risk of metabolic syndrome in South Korean adults. J Am Diet Assoc 2011; 111:1141–1149. [DOI] [PubMed] [Google Scholar]
- 16.Cho YA, Kim J, Cho ER, et al. Dietary patterns and the prevalence of metabolic syndrome in Korean women. Nutr Metab Cardiovasc Dis 2011; 21:893–900. [DOI] [PubMed] [Google Scholar]
- 17.Song Y, Joung H. A traditional Korean dietary pattern and metabolic syndrome abnormalities. Nutr Metab Cardiovasc Dis 2012; 22:456–462. [DOI] [PubMed] [Google Scholar]
- 18.Hong S, Song Y, Lee KH, et al. A fruit and dairy dietary pattern is associated with a reduced risk of metabolic syndrome. Metabolism 2012; 61:883–890. [DOI] [PubMed] [Google Scholar]
- 19.Min C, Noh H, Kang YS, et al. Breakfast patterns are associated with metabolic syndrome in Korean adults. Nutr Res Pract 2012; 6:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Third Report of the National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106:3143–3421. [PubMed] [Google Scholar]
- 21.World Health Organization West Pacific Region. The Asia-Pacific Perspective: redefining obesity and its treatment. Int Obes Task Force 2000; 15–21. [Google Scholar]
- 22.Kim MK, Kim K, Shin MH, et al. The relationship of dietary sodium, potassium, fruits, and vegetables intake with blood pressure among Korean adults aged 40 and older. Nutr Res Pract 2014; 8:453–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shin S, Sung J, Joung H. A fruit, milk and whole grain dietary pattern is positively associated with bone mineral density in Korean healthy adults. Eur J Clin Nutr 2015; 69:442–448. [DOI] [PubMed] [Google Scholar]
- 24.Park JE, Jung H, Lee JE. Dietary pattern and hypertension in Korean adults. Public Health Nutr 2014; 17:597–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yusof AS, Isa ZM, Shah SA. Dietary patterns and risk of colorectal cancer: a systematic review of cohort studies. Asian Pac J Cancer Prev 2012; 13:4713–4717. [DOI] [PubMed] [Google Scholar]
- 26.Steffen LM, Folsom AR, Cushman M, et al. Greater fish, fruit, and vegetable intakes are related to lower incidence of venous thromboembolism: the Longitudinal Investigation of Thromboembolism Etiology. Circulation 2007; 115:188–195. [DOI] [PubMed] [Google Scholar]
- 27.Steffen LM, Kroenke CH, Yu X, et al. Associations of plant food, dairy product, and meat intakes with 15-y incidence of elevated blood pressure in young black and white adults: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J ClinNutr 2005; 82:1169–1177. [DOI] [PubMed] [Google Scholar]
- 28.Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation 2008; 117:754–761. [DOI] [PubMed] [Google Scholar]
- 29.Panagiotakos DB, Pitsavos C, Skoumas Y, et al. The association between food patterns and the metabolic syndrome using principal components analysis: the ATTICA Study. J Am Diet Assoc 2007; 107:979–987.quiz 997. [DOI] [PubMed] [Google Scholar]
- 30.Park S, Ham JO, Lee BK. Effects of total vitamin A, vitamin C, and fruit intake on risk for metabolic syndrome in Korean women and men. Nutrition 2015; 31:111–118. [DOI] [PubMed] [Google Scholar]
- 31.Steffen LM, Van Horn L, Daviglus ML, et al. A modified Mediterranean diet score is associated with a lower risk of incident metabolic syndrome over 25 years among young adults: the CARDIA (Coronary Artery Risk Development in Young Adults) study. Br J Nutr 2014; 112:1654–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997; 336:1117–1124. [DOI] [PubMed] [Google Scholar]
- 33.Asemi Z, Samimi M, Tabassi Z, et al. Effects of DASH diet on lipid profiles and biomarkers of oxidative stress in overweight and obese women with polycystic ovary syndrome: a randomized clinical trial. Nutrition 2014; 30:1287–1293. [DOI] [PubMed] [Google Scholar]
- 34.Song S, Lee JE, Song WO, et al. Carbohydrate intake and refined-grain consumption are associated with metabolic syndrome in the Korean adult population. J Acad Nutr Diet 2014; 114:54–62. [DOI] [PubMed] [Google Scholar]
- 35.Bussemaker E, Hillebrand U, Hausberg M, et al. Pathogenesis of hypertension: interactions among sodium, potassium, and aldosterone. Am J Kidney Dis 2010; 55:1111–1120. [DOI] [PubMed] [Google Scholar]
- 36.Adrogue HJ, Madias NE. Shared primacy of sodium and potassium on cardiovascular risk. Am J Kidney Dis 2009; 54:598–601. [DOI] [PubMed] [Google Scholar]
- 37.Baudrand R, Campino C, Carvajal CA, et al. High sodium intake is associated with increased glucocorticoid production, insulin resistance and metabolic syndrome. Clin Endocrinol (Oxf) 2014; 80:677–684. [DOI] [PubMed] [Google Scholar]
- 38.Yi SS, Firestone MJ, Beasley JM. Independent associations of sodium intake with measures of body size and predictive body fatness. Obesity (Silver Spring) 2015; 23:20–23. [DOI] [PubMed] [Google Scholar]
- 39.Graudal NA, Hubeck-Graudal T, Jurgens G. Effects of low sodium diet versus high sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride. Cochrane Database Syst Rev 2011; CD004022. [DOI] [PubMed] [Google Scholar]
- 40.Zhang Z, Cogswell ME, Gillespie C, et al. Association between usual sodium and potassium intake and blood pressure and hypertension among U.S. adults: NHANES. PLoS One 2013; 8:e75289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cook NR, Obarzanek E, Cutler JA, et al. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow-up study. Arch Intern Med 2009; 169:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yang Q, Liu T, Kuklina EV, et al. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 2011; 171:1183–1191. [DOI] [PubMed] [Google Scholar]
- 43.Aaron KJ, Sanders PW. Role of dietary salt and potassium intake in cardiovascular health and disease: a review of the evidence. Mayo Clin Proc 2013; 88:987–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Meneton P, Lafay L, Tard A, et al. Dietary sources and correlates of sodium and potassium intakes in the French general population. Eur J Clin Nutr 2009; 63:1169–1175. [DOI] [PubMed] [Google Scholar]
- 45.Shin HJ, Cho E, Lee HJ, et al. Instant noodle intake and dietary patterns are associated with distinct cardiometabolic risk factors in Korea. J Nutr 2014; 144:1247–1255. [DOI] [PubMed] [Google Scholar]


