Abstract
The purpose of this study was to perform a meta-analysis comparing the effectiveness and safety of anticoagulation to antiplatelet therapy for the prevention of thromboembolic events in patients with atrial fibrillation (AF).
MEDLINE, Cochrane, EMBASE, and Google Scholar databases were searched for studies published through May 31, 2014. Randomized controlled trials comparing anticoagulants (warfarin) and antiplatelet therapy in patients with AF were included. The primary outcomes were the rates of stroke and systemic embolism. Secondary outcomes included the rates of hemorrhage/major bleeding and death. Pooled odds ratios (ORs) and 95% confidence intervals (CIs) were calculated.
Nine reports of 8 trials that enrolled 4363 patients (2169 patients received anticoagulation and 2194 antiplatelet therapy) were included. All of the studies compared adjusted-dose warfarin or with aspirin, and the majority of the patients were >70 years of age. Anticoagulants were titrated to an international normalized ratio (INR) of 2.0 to 4.5, and aspirin was administered at a dosage of 75 to 325 mg/d. Death occurred in 206 participants treated with an anticoagulant and 229 participants treated with antiplatelet therapy. There was no significant difference in the overall stroke rate between the groups (OR = 0.667, 95% CI 0.426–1.045, P = 0.08); however, patients with nonrheumatic AF (NRAF) treated with an anticoagulant had a lower risk of stroke (OR = 0.557, 95% CI 0.411–0.753, P < 0.001). Anticoagulants were associated with a lower risk of embolism (OR = 0.616, 95% CI = 0.392–0.966, P = 0.04), and this finding persisted in patients with NRAF (OR = 0.581, 95% CI 0.359–0.941, P = 0.03). No significant difference in the rate of hemorrhage/major bleeding was noted (OR = 1.497, 95% CI 0.730–3.070, P = 0.27), and this finding persisted on subgroup analysis.
Anticoagulants appear to be more effective than aspirin in preventing embolisms in patients with AF, as the risk of bleeding is not increased.
INTRODUCTION
Ischemic heart disease is now the leading cause of global mortality, accounting for 1.4 million deaths in developed countries and 5.7 million deaths in developing regions annually.1 Atrial fibrillation (AF) is the most common cardiac arrhythmia, and the global burden of AF is increasing with an estimated 33.5 million individuals worldwide affected by the condition in 2010.2 The age-adjusted prevalence rates in men and women have increased from 569.5 and 359.9/100,000 persons, respectively, in 1990 to 592.2 and 373.1, respectively, in 2010 with mortality increasing by 2-fold over that time period.2 Age is a major risk factor for AF, and the likelihood of being diagnosed with AF after age 55 increases by approximately 2-fold over 10 years.2,3 Other risk factors for AF include obesity, cardiovascular complications, and a history of smoking and alcohol use.4
The American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines categorize AF on the basis of cause.5 AF that is not attributable to heart valve defects is considered nonrheumatic AF (NRAF), whereas secondary AF is attributable to other conditions, such as pulmonary or cardiac disease. The occurrence of AF in a patient <60 years with no evidence of cardiac or pulmonary dysfunction has historically been diagnosed as lone AF.5
AF is associated with thromboembolic events, including stroke, and a seminal analysis by the Framingham Heart Study showed that the risk of stroke in the presence of AF increases significantly with age.6 To prevent embolism and stroke, patients with AF are typically treated with an anticoagulant and/or antiplatelet therapy. Warfarin, one of the most prescribed anticoagulants, has been tested in both fixed and adjusted doses.7 In recent years, alternative anticoagulants such as factor X and thrombin inhibitors have also been approved for use in patients with AF.8 Antiplatelet therapies including aspirin and clopidogrel are currently prescribed both alone and in combination with an anticoagulant.5
Anticoagulants are thought to be more effective than antiplatelet agents (mainly aspirin) at reducing stroke, as well as systemic embolism risk in patients with AF.9,10 However, hemorrhage and bleeding have been linked to the use of both.5 Therefore, achieving an optimal balance between the risk of stroke and bleeding is crucial for the individual management of AF. Data generated by trials comparing a placebo with an anticoagulant or an antiplatelet agent may not address this issue. To remedy this problem, several randomized trials have compared the effects of treatment with an anticoagulant with those of an antiplatelet therapy; however, recent meta-analyses of these trials are lacking. The importance of this topic warrants an update to the existing literature; therefore, the objective of the present study was to conduct a meta-analysis of randomized trials comparing the safety and efficacy of anticoagulant and antiplatelet therapies for patients with AF. We focused our analysis on those studies comparing adjusted-dose anticoagulants with antiplatelet therapy.
METHODS
Search Strategy
The methods used in this review adhere to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. MEDLINE, Cochrane, EMBASE, and Google Scholar databases were searched using combinations of the following terms: anticoagulants, antiplatelet, AF, warfarin, aspirin, stroke, and systemic embolism. The search was performed for studies published through May 31, 2014. The reference lists of relevant studies were hand searched to identify other studies that met the inclusion criteria. After the preliminary search results were obtained, duplicate citations were eliminated. The remaining citations were screened by a 2-step process to identify the final studies that would be included in the meta-analysis. In the first step, the title and abstract of each article were examined, and citations not meeting the inclusion criteria were discarded. In the second step, we obtained full-text copies of the remaining citations, and these were examined to determine which met all of the inclusion criteria. Studies were identified by the search strategy by 2 independent reviewers. If any uncertainties existed regarding eligibility, a third reviewer was consulted. Ethical approval of this study was waived, as meta-analyses do not involve patients.
Selection of Studies
Criteria for inclusion in the meta-analysis were randomized controlled trial, diagnosis was AF, interventions involved anticoagulants (warfarin) and antiplatelet therapy, anticoagulants and antiplatelet therapy were administered alone and not combined with the other treatments, and outcomes of anticoagulants and antiplatelet therapy were compared. Exclusion criteria were as follows: the intervention was for secondary prevention, and not primary prevention of stroke or thromboembolic events; outcomes of interest were not reported; the study was nonrandomized. Non-English and non-Chinese publications, letters, case reports, comments, and editorials were also excluded.
Data Extraction
Data were extracted from eligible studies by 2 reviewers. Any disagreements between the 2 reviewers were resolved by consulting a third reviewer. The following information/data were extracted from studies that met the eligibility criteria: the name of the first author, year of publication, study design, number of participants in each treatment group, mean age and gender of participants in each group, diagnostic criteria, drug and dosage for each study group, and data regarding the outcome measures listed below.
Outcome Measures
The primary outcomes were the rates of stroke. The secondary outcomes were the rates of systemic embolism and hemorrhage/major bleeding. Stroke (ischemic or hemorrhagic) was defined as acute onset of a focal neurological deficit of presumed vascular origin lasting for 24 hours or more. The events included minor, nondisabling, disabling, or fatal strokes. Systemic arterial embolism was defined as thromboembolic complications in the extremities, kidneys, mesenteric arteries, lungs, spleen, retina, or grafts there were verified using imaging studies, surgery, or autopsy. Systemic arterial embolism did not include myocardial infarction. Major hemorrhage was defined as an intracranial hemorrhage (including hemorrhagic stroke) or extracranial bleeding that was fatal or required a transfusion, surgery, or hospital admission. Hemorrhagic stroke was included as stroke and also as major hemorrhage.
Statistical Analysis
The differences in the rates of hemorrhage/major bleeding, stroke, and embolism were compared between participants receiving either anticoagulant or antiplatelet therapy. Odds ratios (ORs) with 95% confidence intervals (95% CIs) were calculated for binary outcomes, and were compared between treatments. A separate subgroup analysis was performed to determine the effects of treatments on patients with NRAF. In this meta-analysis, the OR indicates the risk of events (ie, stroke, embolism, and bleeding) of anticoagulants relative to antiplatelet treatment (Riskanticoagulant/Riskantiplatelet). Thus, an OR > 1 indicates more events with anticoagulants and an OR < 1 indicates less events with anticoagulants. For example, an OR > 1 indicates a greater risk of a stroke with anticoagulants relative to antiplatelet therapy, and an OR < 1 indicates a lower risk of stroke with anticoagulants relative to antiplatelet therapy.
A χ2-based test of homogeneity was performed by using Cochran Q statistic and I2. I2 illustrates the percentage of the total variability in effect estimates among trials that is due to heterogeneity rather than to chance. Random-effects models were used if heterogeneity was detected (I2 > 50%). Otherwise, fixed-effects models were used. Pooled ORs were calculated, and a 2-sided P value <0.05 was considered statistically significant. Sensitivity analysis was performed using the leave-one-out approach, and publication bias was assessed by constructing a funnel plot for the rate of stroke and by Egger test. The absence of publication bias is indicated by the data points forming a symmetric, funnel-shaped distribution and by a 1-tailed significance level of P > 0.05 in Egger test.
All analyses were performed with Comprehensive Meta-Analysis statistical software, version 2.0 (Biostat, Englewood, NJ).
Quality Assessment
Quality of the included studies was assessed using the ‘Risk of Bias’ tool in Review Manager 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) and by constructing a funnel plot. Recommendations for judging risk of bias are provided in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions.11
RESULTS
Study Selection
A flow diagram of study selection is shown in Figure 1. A total of 288 articles were identified in the initial search. Of these, 24 (8.33%) underwent full-text review and 15 were excluded; 11 studies did not report an intervention of interest,12–22 3 did not study patients of interest,23–25 and 1 did not report an outcome of interest.26 Thus, 9 articles met the inclusion criteria and were included in the analysis.7,27–34 Two of the articles report findings of the Stroke Prevention in AF II study.31,32 However, because each article presented unique data, both were included in the meta-analysis. (Thus, the analysis included data of 8 studies and 9 articles.)
Figure 1.
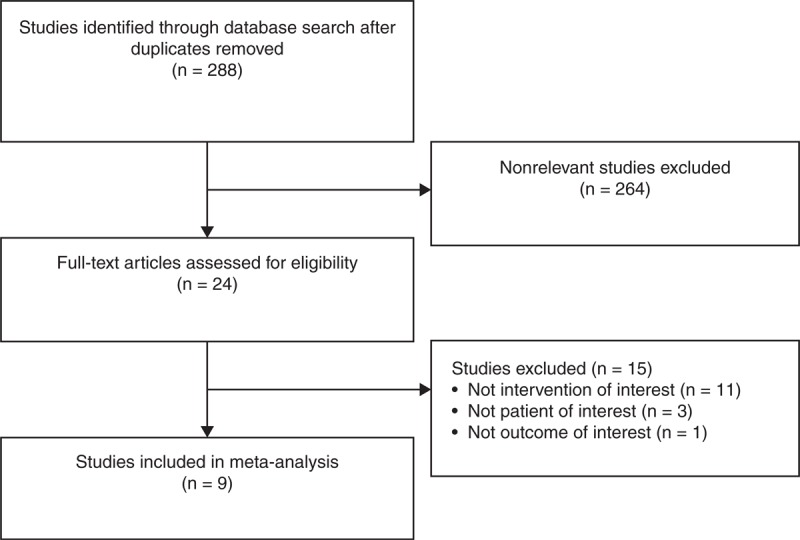
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram for study selection.
Study Characteristics
Characteristics of the 8 trials are summarized in Tables 1 and 2. With the exception of the studies by Lavitola et al27 and Hu et al,34 participants in the studies were >70 years of age, and the ages of the participants were generally similar between the treatment arms. The number of participants in the anticoagulant treatment arms ranged from 36 to 555 (n = 2169), whereas the number in the antiplatelet treatment arms ranged from 39 to 545 (n = 2194). Warfarin was used in all of the studies except for that of Hellemons et al30 that used coumarin, and in all studies the antiplatelet treatment was aspirin. The doses of anticoagulant were titrated to an international normalized ratio (INR) of 2.0 to 4.5, and aspirin was administered at a dosage of 75 to 325 mg/d.
Table 1.
Baseline Characteristics of Trials Included in the Meta-Analysis
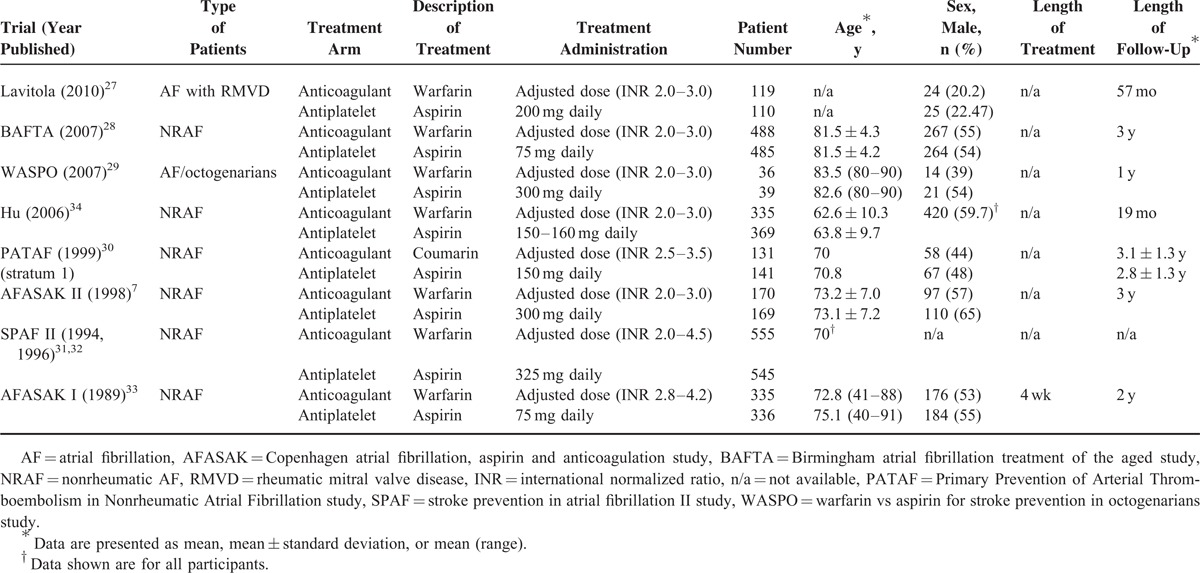
Table 2.
Clinical Events of Patients Treated With an Anticoagulant or Aspirin
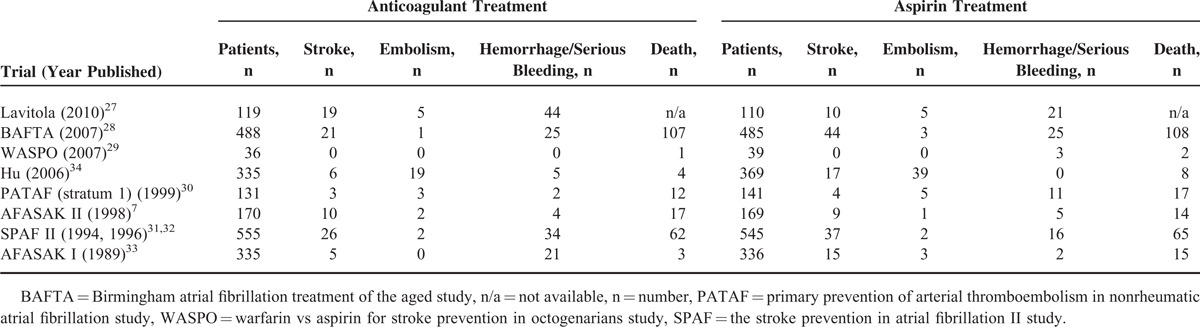
Quality Assessment
Results of the quality assessment of the 8 trials are shown in Figure 2. Only 2 trials6,19 were unbiased in 7 of 7 categories, whereas several had a high risk of performance or detection bias.
Figure 2.
Quality assessment of each included study. (A) Risk of bias summary. (B) Risk of bias graph. AFASAK = the Copenhagen atrial fibrillation, aspirin and anticoagulation study, BAFTA = Birmingham atrial fibrillation treatment of the aged study, PATAF = primary prevention of arterial thromboembolism in nonrheumatic atrial ibrillation study, SPAF = stroke prevention in atrial fibrillation II study, WASPO = warfarin vs aspirin for stroke prevention in octogenarians study.
Outcomes
Stroke
In the 8 trials, 90 patients receiving an anticoagulant and 136 receiving aspirin experienced a stroke. Since the Warfarin vs Aspirin for Stroke Prevention in Octogenarians (WASPO) study reported a stroke rate of 0% for both groups, only 7 studies were included in the analysis. A random-effects analysis was applied because there was evidence of heterogeneity among the studies (Q statistic = 12.885, I2 = 53.43%, P = 0.04). Subgroup analysis of patients with NRAF used a fixed-effects model because no evidence of heterogeneity was noted (Q statistic = 5.212, I2 = 4.08%, P = 0.39). In the overall analysis, there was no significant difference in the stroke rate between the groups (OR = 0.667, 95% CI 0.426–1.045, P = 0.08) (Figure 3A). In contrast, subgroup analysis revealed that patients with NRAF who were treated with an anticoagulant had a lower risk of stroke (OR = 0.557, 95% CI 0.411–0.753, P < 0.001).
Figure 3.
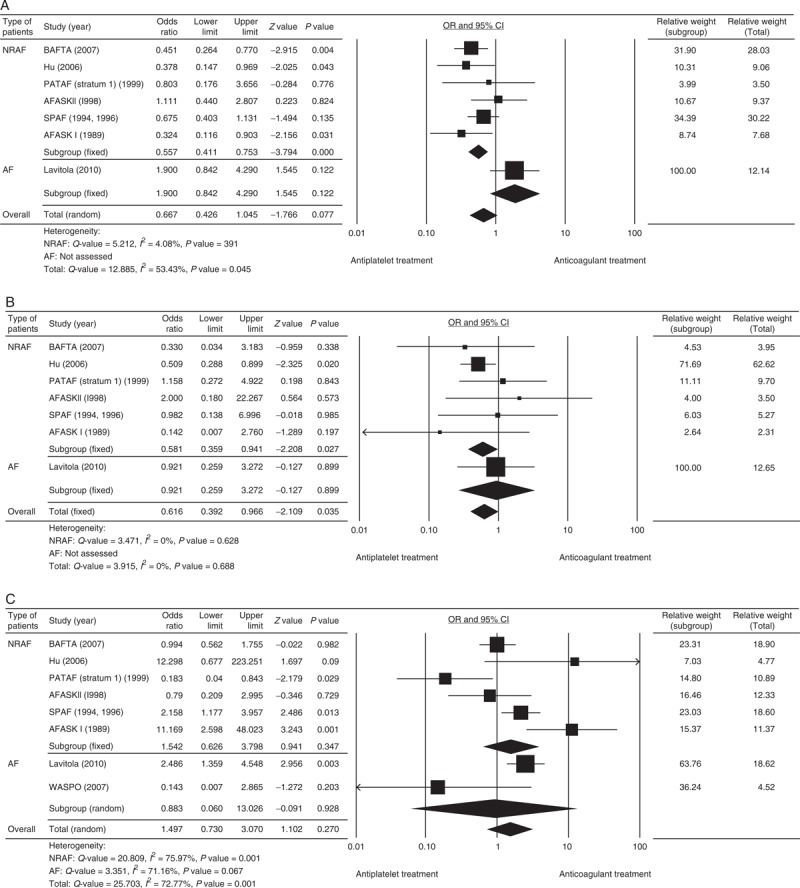
A forest plot comparing the rates of stroke (A), systemic embolism (B), and hemorrhage/major bleeding (C) for participants receiving treatment with an anticoagulant or antiplatelet therapy. AF = atrial fibrillation, AFASK = Copenhagen atrial fibrillation, aspirin and anticoagulation study, BAFTA = Birmingham atrial fibrillation treatment of the aged study, CI = confidence interval, Lower limit = lower bound of the 95% CI, NRAF = nonrheumatic AF, OR = odds ratio, PATAF = primary prevention of arterial thromboembolism in nonrheumatic atrial fibrillation study, SPAF = stroke prevention in atrial fibrillation II study, Upper limit = upper bound of the 95% CI.
Systemic Embolism
In the 8 trials, 32 patients receiving an anticoagulant and 58 receiving aspirin experienced an embolism. Since the WASPO study reported a rate of 0% for both groups, only 7 studies were included in the analysis. A fixed-effects analysis was applied because there was no evidence of heterogeneity (all studies: Q statistic = 3.915, I2 = 0.0%, P = 0.69; studies of NRAF patients: Q statistic = 3.471, I2 = 0.0%, P = 0.63). For all studies, treatment with anticoagulants was associated with a lower risk of embolism (OR = 0.616, 95% CI = 0.392–0.966, P = 0.04) (Figure 3B). Subgroup analysis showed that in patients with NRAF, anticoagulants were associated with a lower risk of embolism (OR = 0.581, 95% CI 0.359–0.941, P = 0.03).
Hemorrhage/Major Bleeding
In the 8 trials, 135 patients receiving an anticoagulant and 83 receiving aspirin experienced a hemorrhage or major bleeding. A random-effects analysis was applied because of heterogeneity among the studies (all studies: Q statistic = 25.703, I2 = 72.77%, P = 0.001; studies of NRAF patients: Q statistic = 20.809, I2 = 7 5.97%, P = 0.001; studies of patients with AF: Q statistic = 3.351, I2 = 71.16%, P = 0.07). No significant difference in the rate of hemorrhage/major bleeding was noted when all 8 studies were analyzed (OR = 1.497, 95% CI 0.730–3.070, P = 0.27), for patients with NRAF (OR = 1.542, 95% CI 0.626–3.798, P = 0.35), or for patients with AF (OR = 0.883, 95% CI 0.060–13.026, P = 0.93) (Figure 3C).
Sensitivity Analysis
Results of the sensitivity analysis using the leave-one-out approach are shown in Figure 4. The results showed that the direction and magnitude of the combined estimates did not change markedly with the exclusion of individual studies indicating the meta-analysis has good reliability.
Figure 4.
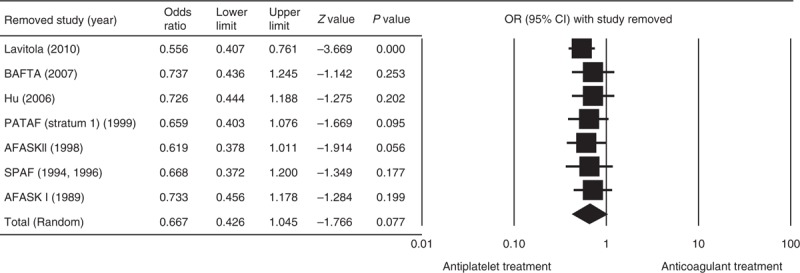
Sensitivity analysis showing the influence of each study on the pooled estimate for the rate of stroke using the leave-one-out approach. CI = confidence interval, Lower limit = lower bound of the 95% CI, OR = odds ratio, Upper limit = upper bound of the 95% CI.
Publication Bias
Results of the assessment of publication bias are shown in Figure 5. The individual data points formed a symmetrical, funnel-shaped distribution indicating the absence of publication bias. Egger test confirmed no publication bias (t = 0.32, 1-tailed P = 0.38).
Figure 5.
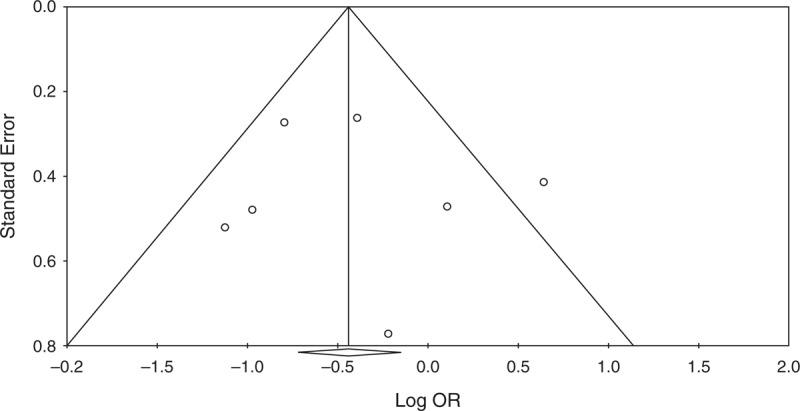
A funnel plot of the rates of stroke of the included studies. OR = odds ratio.
DISCUSSION
In this meta-analysis, we compared the efficacy and safety of anticoagulant treatment with aspirin antiplatelet therapy in patients with AF. A total of 8 studies with approximately 4300 patients were included in the analysis. By including recently published trials, this analysis provides a crucial update to the field. The results suggest that anticoagulants are more effective than aspirin in preventing embolisms in patients with AF. Although overall the risk of stroke was similar between treatments, in patients with NRAF anticoagulants were associated with a lower risk of stroke. Importantly, the overall and subgroup analyses showed that there was no difference in bleeding events between patients treated with anticoagulants and aspirin.
AF is the most common sustained cardiac arrhythmia and an independent risk factor for stroke; in patients with AF the risk of stroke is 2 to 17 times that of the general population.2,4,5 Despite its increasing prevalence, the pathophysiological mechanisms leading to AT are only recently being described. The majority of cases of AF are associated with heart disease including coronary artery disease, congestive heart failure, valvular heart disease, and hypertension.35 Other conditions associated with AF include hyperthyroidism, excessive alcohol consumption, obesity, and sleep apnea.35 Pathophysiological mechanisms thought to be responsible for AF include abnormalities of intracellular calcium signaling36 and atrial remodeling.35,37 Age-related changes including vascular stiffening and cardiac remodeling are thought to be responsible for the association of AF with aging, and approximately 25% of strokes in persons >80 years of age are due to AF.3 Genetic factors are being increasing recognized as having a role in the development of AF,35 as is the role of microRNAs, small noncoding RNAs that are important regulators of gene expression.38 Polymorphisms in glycoprotein IIb/IIIa, which participates in clotting by binding to fibrinogen and von Willebrand factor, have been shown to increase the risk of stroke.39
Despite the fact that adjusted-dose anticoagulants are difficult to use and many patients do not maintain a therapeutic INR, current guidelines recommend that most patients with AF receive anticoagulation.5 Our results confirm the validity of this recommendation only for patients with NRAF, because they indicate that the use of an anticoagulant may reduce the risk of stroke and embolism whereas producing no greater risk of hemorrhage or bleeding. Moreover, they suggest that treatment with an anticoagulant may be more suitable than antiplatelet therapy for patients with nonvalvular AF and a CHA2DS2-VASc score of 1, for whom current guidelines recommend either an anticoagulant or antiplatelet therapy.5
Other meta-analyses have compared the safety and efficacy of anticoagulants with those of antiplatelet therapies.9,10,40–42 Saxena and Koudstaal9 focused on secondary prevention and included only 2 studies. Three meta-analyses10,40,42 concluded that anticoagulants were associated with a lower risk of stroke as compared with antiplatelet therapy. Two studies40,41 concluded that anticoagulants were superior to antiplatelet therapy for preventing a systemic embolism. Two studies that reported data on major bleeding or hemorrhage10,41 did not find substantial evidence for increased risk of these events with the use of anticoagulants compared with antiplatelet therapy.
Several reasons may account for the observed differences between these studies and our own regarding the superior ability of anticoagulants to prevent stroke in NRAF patients. First, different studies were included in the analyses. Segal et al10 only included the Copenhagen Atrial Fibrillation, Aspirin and Anticoagulation study (AFASAK) I and II and the Stroke Prevention in Atrial Fibrillation II (SPAF II) studies, all of which enrolled patients with NRAF. Therefore, their findings agree with our own subgroup analysis. Seven of 8 studies included in our analysis (the Birmingham Atrial Fibrillation Treatment of the Aged study (BAFTA), Primary Prevention of Arterial Thromboembolism in Nonrheumatic Atrial Fibrillation, AFASAK I and II, Chinese Antithrombotic Therapy in Atrial Fibrillation Study, WASPO, and SPAF II) were also included in the analysis by Hart et al.42 However, their analysis included the EAFT study,43 which assessed secondary prevention in patients with NRAF (N = 455), but not that of Lavitola et al,27 which enrolled patients with rheumatic mitral valve disease (RMVD) (N = 229). Aguilar et al40 included the Atrial Fibrillation Clopidogrel Trial With Irbesartan for Prevention of Vascular Events (ACTIVE W) study, which used clopidogrel (N = 6706) in their analysis, but they did not include the BAFTA study (N = 973). In addition, Segal et al10 and Hart et al42 used the subgroup data from the SPAF II trial for patients older or <75 years, whereas we did not.
It should also be noted that patients with nonvalvular AF and valvular AF are different populations and have a different risk for thromboembolism.5 In the study by Lavitola et al27 of patients with RMVD, there were 15 embolic events in patients receiving aspirin and 24 in patients receiving warfarin; however, 21 of the patients receiving warfarin had an INR < 2.0 and only 3 had an INR from 2.0 to 2.2 at the time of the event. When the current meta-analysis is performed with exclusion of the Lavitola et al study, the results (OR = 0.556, 95% CI 0.407–0.761, P < 0.001) are almost identical to that of subgroup analysis for NRAF (OR = 0.557, 95% CI 0.411–0.753, P < 0.001).
There are a number of limitations of this meta-analysis that need to be considered when interpreting the results. The trials included in this analysis, as well as prior meta-analyses, may not have taken into account differences in the time-in-therapeutic-range of the INR. This feature of warfarin use has been shown to vary significantly among the sites of the ACTIVE W trial.44 The definition of stroke may have varied between studies. For example, Hart et al42 included intracranial hemorrhage in the primary outcome of “all strokes,” whereas we defined stroke as the acute onset of a focal neurological deficit of presumed vascular origin lasting for 24 hours or more. The number of studies included in the current analysis was relatively small, and the earliest study was performed in 1989 and the latest in 2010, and various treatment regimens were used over this 2-decade period. This highlights the need for additional high-quality studies to address this issue. Patient characteristics of the included studies were not homogeneous, and all but 2 studies enrolled patients >70 years of age, and thus, the results may not be applicable to younger age groups. Most of the included studies reported data that was analyzed on an intent-to-treat basis, and thus, the pooled effect estimates may have been underestimated.
The only antiplatelet that was studied was aspirin, and newer antiplatelet drugs are available and their effectiveness compared with anticoagulation has yet to be determined. Lastly, several of the studies included in the analysis were found to have a high risk of performance or detection bias.
CONCLUSIONS
The results of this meta-analysis suggest that anticoagulants are more effective than aspirin in preventing embolisms in patients with AF, and though the overall risk of stroke was similar between treatments, and in patients with NRAF anticoagulants were associated with a lower risk of stroke. No difference in bleeding events was found between patients treated with anticoagulants and aspirin. These results support the use of anticoagulation over aspirin to prevent thromboembolic events in patients with AF and illustrate that future trials should strive to enroll well-defined patient populations to allow a definitive analysis of how anticoagulants and antiplatelet therapies perform in different groups of patients.
Footnotes
Abbreviations: AF = atrial fibrillation, CI = confidence interval, INR = international normalized ratio, NRAF = nonrheumatic AF, OR = odds ratio, RMVD = rheumatic mitral valve disease.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Santulli G. Epidemiology of cardiovascular disease in the 21st century: updated numbers and updated facts. J Cardiovasc Dis 2013; 1:1–2. [Google Scholar]
- 2.Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 2014; 129:837–847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lubitz SA, Bauer KA, Benjamin EJ, et al. Stroke prevention in atrial fibrillation in older adults: existing knowledge gaps and areas for innovation: a summary of an American Federation for Aging research seminar. J Am Geriatr Soc 2013; 61:1798–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ball J, Carrington MJ, McMurray JJ, et al. Atrial fibrillation: profile and burden of an evolving epidemic in the 21st century. Int J Cardiol 2013; 167:1807–1824. [DOI] [PubMed] [Google Scholar]
- 5.January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation 2014; 130:2071–2104. [DOI] [PubMed] [Google Scholar]
- 6.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke 1991; 22:983–988. [DOI] [PubMed] [Google Scholar]
- 7.Gullov AL, Koefoed BG, Petersen P, et al. Fixed minidose warfarin and aspirin alone and in combination vs adjusted-dose warfarin for stroke prevention in atrial fibrillation: Second Copenhagen Atrial Fibrillation, Aspirin, and Anticoagulation Study. Arch Intern Med 1998; 158:1513–1521. [DOI] [PubMed] [Google Scholar]
- 8.Soff GA. A new generation of oral direct anticoagulants. Arterioscler Thromb Vasc Biol 2012; 32:569–574. [DOI] [PubMed] [Google Scholar]
- 9.Saxena R, Koudstaal P. Anticoagulants versus antiplatelet therapy for preventing stroke in patients with nonrheumatic atrial fibrillation and a history of stroke or transient ischemic attack. Cochrane Database Syst Rev 2004; 4:CD000187. [DOI] [PubMed] [Google Scholar]
- 10.Segal JB, McNamara RL, Miller MR, et al. Prevention of thromboembolism in atrial fibrillation. A meta-analysis of trials of anticoagulants and antiplatelet drugs. J Gen Intern Med 2000; 15:56–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1. 0 [updated March 2011]. Chichester, West Sussex, UK: The Cochrane Collaboration; 2011. [Google Scholar]
- 12.Connolly S, Pogue J, Hart R, et al. ACTIVE Writing Group of the ACTIVE Investigators. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial. Lancet 2006; 367:1903–1912. [DOI] [PubMed] [Google Scholar]
- 13.Brandes A, Overgaard M, Plauborg L, et al. Guideline adherence of antithrombotic treatment initiated by general practitioners in patients with nonvalvular atrial fibrillation: a Danish survey. Clin Cardiol 2013; 36:427–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flaker GC, Eikelboom JW, Shestakovska O, et al. Bleeding during treatment with aspirin versus apixaban in patients with atrial fibrillation unsuitable for warfarin: the apixaban versus acetylsalicylic acid to prevent stroke in atrial fibrillation patients who have failed or are unsuitable for vitamin K antagonist treatment (AVERROES) trial. Stroke 2012; 43:3291–3297. [DOI] [PubMed] [Google Scholar]
- 15.Flaker GC, Gruber M, Connolly SJ, et al. SPORTIF Investigators. Risks and benefits of combining aspirin with anticoagulant therapy in patients with atrial fibrillation: an exploratory analysis of stroke prevention using an oral thrombin inhibitor in atrial fibrillation (SPORTIF) trials. Am Heart J 2006; 152:967–973. [DOI] [PubMed] [Google Scholar]
- 16.Formiga F, Ferrer A, Mimbrera D, et al. Grupo de Estudio Octabaix. High rate of anticoagulation therapy in oldest old subjects with atrial fibrillation: the Octabaix study. J Am Med Dir Assoc 2012; 13:8–10. [DOI] [PubMed] [Google Scholar]
- 17.Ghaswalla PK, Harpe SE, Slattum PW. Warfarin use in nursing home residents: results from the 2004 national nursing home survey. Am J Geriatr Pharmacother 2012; 10:25–36.e2. [DOI] [PubMed] [Google Scholar]
- 18.Granger CB, Alexander JH, McMurray JJ, et al. ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med 2011; 365:981–992. [DOI] [PubMed] [Google Scholar]
- 19.Hart RG, Pearce LA, Asinger RW, et al. Warfarin in atrial fibrillation patients with moderate chronic kidney disease. Clin J Am Soc Nephrol 2011; 6:2599–2604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kirchhof P, Ammentorp B, Darius H, et al. Management of atrial fibrillation in seven European countries after the publication of the 2010 ESC Guidelines on atrial fibrillation: primary results of the PREvention oF thromboemolic events—European Registry in Atrial Fibrillation (PREFER in AF). Europace 2014; 16:6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morocutti C, Amabile G, Fattapposta F, et al. Indobufen versus warfarin in the secondary prevention of major vascular events in nonrheumatic atrial fibrillation. SIFA (Studio Italiano Fibrillazione Atriale) Investigators. Stroke 1997; 28:1015–1021. [DOI] [PubMed] [Google Scholar]
- 22.Bertomeu-González V, Cordero A, Mazón P, et al. Investigators of the CARDIOTENS2 study. Anticoagulation prescription in atrial fibrillation. Expert Opin Pharmacother 2011; 12:1473–1479. [DOI] [PubMed] [Google Scholar]
- 23.Halkes PH, van Gijn J, Kappelle LJ, et al. ESPRIT Study Group. Medium intensity oral anticoagulants versus aspirin after cerebral ischaemia of arterial origin (ESPRIT): a randomised controlled trial. Lancet Neurol 2007; 6:115–124. [DOI] [PubMed] [Google Scholar]
- 24.Mohr JP, Thompson JL, Lazar RM, et al. Warfarin–Aspirin Recurrent Stroke Study Group. A comparison of warfarin and aspirin for the prevention of recurrent ischemic stroke. N Engl J Med 2001; 345:1444–1451. [DOI] [PubMed] [Google Scholar]
- 25.Colli A, Mestres CA, Castella M, et al. Comparing warfarin to aspirin (WoA) after aortic valve replacement with the St. Jude Medical Epic heart valve bioprosthesis: results of the WoA Epic pilot trial. J Heart Valve Dis 2007; 16:667–671. [PubMed] [Google Scholar]
- 26.Lip GY, Rasmussen LH, Olsson SB, et al. Oral direct thrombin inhibitor AZD0837 for the prevention of stroke and systemic embolism in patients with non-valvular atrial fibrillation: a Phase II study of AZD0837 in patients who are appropriate for but unable or unwilling to take vitamin K antagonist therapy. Thromb Res 2011; 127:91–99. [DOI] [PubMed] [Google Scholar]
- 27.Lavitola Pde L, Sampaio RO, Oliveira WA, et al. Warfarin or aspirin in embolism prevention in patients with mitral valvulopathy and atrial fibrillation. Arq Bras Cardiol 2010; 95:749–755. [DOI] [PubMed] [Google Scholar]
- 28.Mant J, Hobbs FD, Fletcher K, et al. Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial. Lancet 2007; 370:493–503. [DOI] [PubMed] [Google Scholar]
- 29.Rash A, Downes T, Portner R, et al. A randomised controlled trial of warfarin versus aspirin for stroke prevention in octogenarians with atrial fibrillation (WASPO). Age Ageing 2007; 36:151–156. [DOI] [PubMed] [Google Scholar]
- 30.Hellemons BS, Langenberg M, Lodder J, et al. Primary prevention of arterial thromboembolism in non-rheumatic atrial fibrillation in primary care: randomised controlled trial comparing two intensities of coumarin with aspirin. BMJ 1999; 319:958–964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Warfarin versus aspirin for prevention of thromboembolism in atrial fibrillation: Stroke Prevention in Atrial Fibrillation II Study. Lancet 1994; 343:687–691. [PubMed] [Google Scholar]
- 32.Bleeding during antithrombotic therapy in patients with atrial fibrillation. The Stroke Prevention in Atrial Fibrillation Investigators. Arch Intern Med 1996; 156:409–416. [PubMed] [Google Scholar]
- 33.Petersen P, Boysen G, Godtfredsen J, et al. Placebo-controlled, randomised trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study. Lancet 1989; 1:175–179. [DOI] [PubMed] [Google Scholar]
- 34.Hu DY, Zhang HP, Sun YH, et al. The randomized study of efficiency and safety of antithrombotic therapy in nonvalvular atrial fibrillation: warfarin compared with aspirin [article in Chinese]. Zhonghua Xin Xue Guan Bing Za Zhi 2006; 34:295–298. [PubMed] [Google Scholar]
- 35.Wakili R, Voigt N, Kääb S, et al. Recent advances in the molecular pathophysiology of atrial fibrillation. J Clin Invest 2011; 121:2955–2968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xie W, Santulli G, Guo X, et al. Imaging atrial arrhythmic intracellular calcium in intact heart. J Mol Cell Cardiol 2013; 64:120–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Santulli G, D’ascia SL, D’ascia C. Development of atrial fibrillation in recipients of cardiac resynchronization therapy: the role of atrial reverse remodelling. Can J Cardiol 2012; 28:245.e17. [DOI] [PubMed] [Google Scholar]
- 38.Santulli G, Iaccarino G, De Luca N, et al. Atrial fibrillation and microRNAs. Front Physiol 2014; 5:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lanni F, Santulli G, Izzo R, et al. The Pl(A1/A2) polymorphism of glycoprotein IIIa and cerebrovascular events in hypertension: increased risk of ischemic stroke in high-risk patients. J Hypertens 2007; 25:551–556. [DOI] [PubMed] [Google Scholar]
- 40.Aguilar MI, Hart R, Pearce LA. Oral anticoagulants versus antiplatelet therapy for preventing stroke in patients with non-valvular atrial fibrillation and no history of stroke or transient ischemic attacks. Cochrane Database Syst Rev 2007; 3:CD006186. [DOI] [PubMed] [Google Scholar]
- 41.Andersen LV, Vestergaard P, Deichgraeber P, et al. Warfarin for the prevention of systemic embolism in patients with non-valvular atrial fibrillation: a meta-analysis. Heart 2008; 94:1607–1613. [DOI] [PubMed] [Google Scholar]
- 42.Hart RG, Pearce LA, Aguilar MI. Adjusted-dose warfarin versus aspirin for preventing stroke in patients with atrial fibrillation. Ann Intern Med 2007; 147:590–592. [DOI] [PubMed] [Google Scholar]
- 43.Secondary prevention in non-rheumatic atrial fibrillation after transient ischaemic attack or minor stroke. EAFT (European Atrial Fibrillation Trial) Study Group. Lancet 1993; 342:1255–1262. [PubMed] [Google Scholar]
- 44.Connolly SJ, Pogue J, Eikelboom J, et al. Benefit of oral anticoagulant over antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centers and countries as measured by time in therapeutic range. Circulation 2008; 118:2029–2037. [DOI] [PubMed] [Google Scholar]


