Abstract
A retrospective study.
To summarize and describe the radiographic parameters of adult degenerative scoliosis (ADS) and explore the radiological parameters which are significantly different in sagittal balanced and imbalanced ADS patients.
ADS is the most common type of adult spinal deformity. However, no comprehensive description of radiographic parameters in ADS patients has been made, and few studies have been performed to explore which radiological parameters are significantly different between sagittal balanced and imbalanced ADS patients.
Medical records of ADS patients in our outpatient clinic from January 2012 to January 2014 were reviewed. Demographic data including age and sex, and radiographic data including the coronal Cobb angle, location of apical vertebra/disc, convexity of the curve, degree of apical vertebra rotation, curve segments, thoracic kyphosis (TK), lumbar lordosis (LL), thoracolumbar kyphosis (TL), sacral slope (SS), pelvic tilt (PT), pelvic incidence (PI), sagittal vertical axis (SVA), and PI minus LL (PI − LL) were reviewed to make comprehensive description of radiographic parameters of ADS. Furthermore, patients were divided into 2 groups according to whether the patients’ sagittal plane was balanced: Group A (imbalanced, SVA > 5 cm) and Group B (balanced, SVA ≤ 5 cm). Demographic and radiological parameters were compared between these 2 groups.
A total of 99 patients were included in this study (Group A = 33 and Group B = 66; female = 83 and male = 16; sex ratio = 5:1). The median of age were 67 years (range: 41–92 years). The median of coronal Cobb angle and length of curve was 23 (range: 10–75°) and 5 segments (range: 3–7), respectively. The most common location of apical vertebra was at L2 to L3 (81%) and the median of degree of apical vertebra rotation was 2° (range: 1–3). Our study also showed significant correlations between coronal Cobb angle and curve segments (r = 0.23, P < 0.005) and degree of apical vertebra rotation (r = 0.53, P < 0.005). With regard to the sagittal balance, there were significant differences in age, LL, PT, coronal Cobb angle, degree of apical vertebra rotation, and PI − LL between imbalanced group and balanced group (all P < 0.05); however, no significant difference was observed in gender, TK, TL, SS, and PI.
Our study provided the general radiographic parameters of ADS. Weak or moderate but significant correlations between coronal Cobb angle and curve segments and degree of apical vertebra rotation were observed. Furthermore, age, coronal Cobb angle, LL, PT, and PI − LL were significantly different between sagittal balanced and imbalanced ADS patients.
INTRODUCTION
Adult degenerative scoliosis (ADS), the most common type of adult spinal deformity (ASD), is defined as a spinal deformity in a skeletally mature patient with a Cobb angle greater than 10°, who has no history of scoliosis during childhood and adolescence.1 ADS is typically diagnosed in patients older than 40 years and the incidence of ADS is increasing rapidly due to the social aging problem around the world, which is becoming a significant healthcare concern.1,2 Although the prevalence of ADS is difficult to evaluate precisely, it has been reported to reach 64% to 68% among aged population.2,3
Due to the rapid increase of prevalence of ADS, more and more attention have been paid to this disease, including the researches of etiology,4,5 patients’ demographics,6 clinical and radiological evaluation,7 conservation treatment and surgery.8–10 Only a few studies3,6,11 have been performed to make a description of some patients’ demographics and radiographic parameters. However, few studies have been conducted exclusively to describe the sagittal parameters in ADS patients that have shown substantial correlation with health-related quality of life measures.12 Therefore, detailed information of both coronal and sagittal plane's radiographic parameters is essential for us to make a more profound understanding of ADS.2,13,14
In recent years, the importance of sagittal spinopelvic alignment in spinal deformity is becoming increasingly recognized as it relates to clinical outcomes.15–18 Furthermore, importance of preoperative and postoperative sagittal balance, such as the significant correlation between sagittal balance and health status, has also been paid attention to in ADS patients.12,19 However, unlike adolescent idiopathic scoliosis (AIS),20–22 little information is available on the relative factors influencing sagittal balance in ADS patients, which is correlated with patient symptoms and health status and could be useful for decision-making, surgical planning, and surgical treatment.12,23,24
Therefore, the characteristics and parameters of both coronal and sagittal plane and radiological parameters that are significantly different in sagittal balanced and imbalanced ADS patients are crucial to be explored and discussed. We performed this study to investigate the radiographic parameters of ADS and explore the radiological parameters that are significantly different in sagittal balanced and imbalanced ADS patients.
MATERIALS AND METHODS
Patient Population
A total of 99 ADS patients in our outpatient clinic from January 2012 to January 2014, who met the inclusion and exclusion criteria, were retrospectively reviewed. The inclusion criteria of patients were as follows: patients older than 40 years; patients with coronal Cobb angle greater than 10° on the posteroanterior full-length stand film; patients have no history of scoliosis during young period. Patients without sufficient radiographic parameters or who had gone any spine surgery were also excluded from our study. This study was approved by the Institutional Review Board in Second Military Medical University, and all patients in our study provided written informed consent for the study and surgery.
Data Collection
Demographic data collected were patient age and sex. Radiographic measurements, including coronal Cobb angle, location of the apical vertebra/disc, convexity of the curve, degree of apical vertebra rotation (evaluated by Nash–Moe method), curve segments (from the upper-end vertebra to lower-end vertebra of the Cobb angle), thoracic kyphosis (TK, Cobb angle from the upper endplate of T5 to the lower endplate of T12 on the sagittal full-length film), lumbar lordosis (LL, Cobb angle from the upper endplate of L1 to the lower endplate of S1), thoracolumbar kyphosis (TL, Cobb angle from the upper endplate of T10 to the lower endplate of L2), sacral slope (SS, the angle between the horizontal and the sacral plate), pelvic tilt (PT, the angle between the vertical and the line through the midpoint of the sacral plate to femoral heads axis), pelvic incidence (PI, angle subtended by a perpendicular from the upper endplate of S1 and a line connecting the center of the femoral head to the center of the upper endplate of S1), sagittal vertical axis (SVA, the horizontal offset from the posterosuperior corner of S1 to the vertebral body of C7) and the relationship between PI and LL, expressed as PI − LL (PI minus LL), were measured by 2 individual surgeons, and the mean value was used for analysis. Sagittal imbalance was defined as an imbalance greater than 5 cm.25,26 Patients were divided into 2 groups according to whether patients’ sagittal plane was balanced in lateral full spine standing radiographs: Group A (imbalanced, SVA > 5 cm) and Group B (balanced, SVA ≤ 5 cm). Age, segments number, coronal Cobb angle, apex rotation, TK, TL, LL, SS, PT, PI, and PI − LL were compared between 2 groups.
Statistical Analysis
Statistical analyses were performed using SPSS 17.0 statistics software (SPSS, Inc., Chicago, IL). Descriptive statistics were listed in the form of median and the data involved in the comparison were represented in mean and standard deviation. Categorical variables, such as gender, were compared by Chi-square test. Independent 2-sample t-test was used to compare the differences of other variables between 2 groups. Coronal Cobb angle and its correlation with radiographic parameters were analyzed by correlation coefficient test. The following general categories indicate a quick way of interpreting a calculated r value: 0.0 to 0.2: very weak to negligible correlation; 0.2 to 0.4: weak, low correlation (not very significant); 0.4 to 0.7: moderate correlation; 0.7 to 0.9: strong, high correlation; 0.9 to 1.0: very strong correlation. P < 0.05 was selected as significant level.
RESULTS
Radiographic Parameters of ADS Patients
A total of 99 patients were included in this study. The median age of ADS patients were 67 years (range: 41–92 years) and the sex ratio was 5:1 (female: 63 and male: 16). Convexity of the curve located at right side was found in 54 patients (55%) and others’ convexity of the curve was located at left side (45%). There were 10 patients (10%) classified with a curve type of thoracolumbar curve and 89 (90%) classified with lumbar curve. The median of coronal Cobb angle was 23° (range: 10–75°) and the median of segments number of curve was 5 segments (range: 3–7). Besides, the median of rotation of apical vertebra was 2° (range: 1–3) (shown in Table 1). According to our study, most of the apical vertebra was located at L2 to L3 (n = 80, 81%), as is shown in Figure 1. As shown in Figure 2, 39% patients’ Cobb angle (n = 39) was found in the range of 20–29°, 31 patients (31%) in the range of 10–19°, 13 patients’ Cobb angle (13%) was found in the range of 30–39° and 16 patients’ Cobb angle was larger than 40° (16%). Furthermore, our study also showed significant correlations between coronal Cobb angle and segments number of Cobb angle (r = 0.23, P = 0.025) and degree of apical vertebra rotation (r = 0.53, P < 0.001) (Table 2).
TABLE 1.
General Characteristics and Radiographic Parameters in ADS Patients

FIGURE 1.

The distribution of location of apical vertebra/disc.
FIGURE 2.
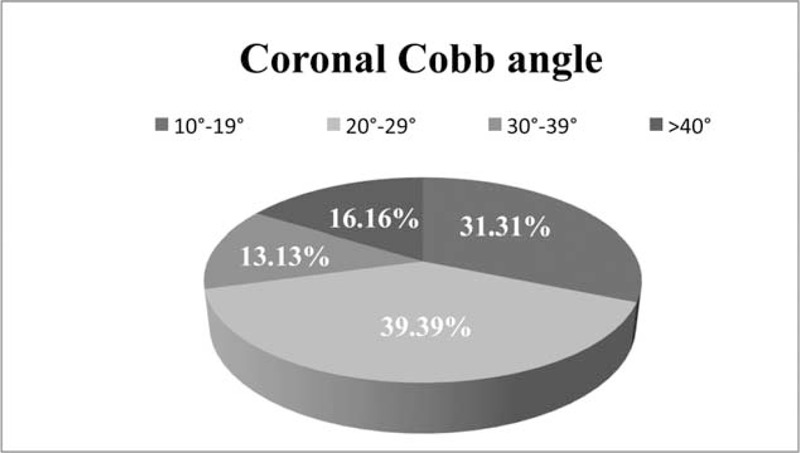
The percentages of coronal Cobb angle.
TABLE 2.
Correlation Between Coronal Cobb Angle and Other Variables

With regard to the sagittal parameters, TK, TL, LL, SS, PT, PI, PI − LL, and SVA ranged from −13° to 64° with a median of TK of 28°, −62° to 23° with a median of TL of −6°, −9° to 77° with a median of LL of 40°, 6° to 63° with a median of SS of 32°, 5° to 43° with a median of PT of 26°, 29° to 90° with a median of PI of 55°, −31° to 64° with a median of PI − LL of 18° and −34 mm to 224 mm with a median of SVA of 30 mm, respectively (Table 1).
Comparison of Parameters Between Sagittal Balanced and Imbalanced Patients
Sagittal plane was observed imbalanced in 33 patients and 66 patients’ sagittal plane was found balanced in lateral full spine stand radiographs (33% vs. 67%; ratio = 1:2). Our results indicated that there were significant differences in age (P = 0.001), LL (P < 0.001), PT (P = 0.031), coronal Cobb angle (P = 0.016), degree of apical vertebra rotation (P = 0.006), and PI − LL (P < 0.001) between Group A and Group B; however, no significant difference was observed in gender, segments, TK, TL, SS, and PI between 2 groups (all P > 0.05), as shown in Table 3.
TABLE 3.
Comparison of Radiographic Parameters Between 2 Groups

DISCUSSION
Radiographic Parameters of ADS Patients
ADS is an increasing healthcare issue due to the global aging problem.27 Recently, Schwab et al27 proposed a new classification of ASD. Coronal curve types and sagittal modifiers, including PI − LL, global alignment and PT that have shown substantial correlation with health-related quality of life were included in their classification and researches suggested that there was excellent inter- and intrarater reliability and interrater agreement for curve type and each modifier, which might be a guideline for the surgical treatment of ASD. However, the classification system involved all the ASD, including adult idiopathic scoliosis and ADS, which might not be used to describe the characteristics of ADS precisely.28,29 Furthermore, although some studies3,6,11 have reported some characteristic parameters of ADS, no large-scaled studies and comprehensive description of ADS have been performed and made, which are essential to our profound understanding and treatment of ADS.
In our study, the median of age of ADS patients were 67 years (range: 41–92 years), and women were more susceptible to suffer from ADS (sex ratio = 5:1), which was consistent with Watanuki et al's study.6 According to our study, most of the apical vertebra was located at L2 to L3, which was consistent with Pritchett and Bortel's study.11 Furthermore, our study also showed significant correlations between coronal Cobb angle and segments of curve (r = 0.23, P = 0.025) and degree of apical vertebra rotation (r = 0.53, P < 0.001), while no significant correlation was observed with age or gender, indicating that more segments involved in lumbar/thoracolumbar curve and more rotation degree of apex might result in larger coronal Cobb angle, which might be related to the biomechanics of the spine.30,31
With regard to the sagittal parameters of our patients, TK, TL, LL, SS, PT, PI, PI − LL, and SVA, which were similar to the results reported in Lafage et al's study19 and Schwab et al's study.27
According to these results, we could conclude that: There was a tendency for female predominance, and the frequency of the disorder increased with age; compared with AIS, the severity of these curves was relatively low, with a median of Cobb angle of 23°, with most in the range 20–29°, and with a median rotation of apex of 2°; most patients were classified with lumbar curve, with a median of segment of 5, and with the apex vertebra most located at L2/L3; coronal Cobb angle were highly correlated with segments and apex rotation; all the sagittal parameters of ADS were listed in our article, which might be useful in understanding of ADS and surgical management that should ideally restore normal sagittal alignment by correcting the deformity.32,33
Comparison of Parameters Between Sagittal Balanced and Imbalanced Patients
Sagittal balance is one of the most important considerations to be taken when evaluating spinal deformity nowadays due to the fact that the sagittal profile of the spine and pelvis largely influences both of the standing balance and clinical outcomes.12,15–19,27,34 Glassman et al12 evaluated the relationships between radiographic parameters and health status and they found that although even mildly positive sagittal balance was somewhat detrimental, severity of symptoms increased in a linear fashion with progressive sagittal imbalance. Lafage et al19 performed a prospective study to investigate the relationship between spinopelvic parameters and patient self-reported outcomes on adult subjects with spinal deformities and their results demonstrated significant T1-SPI (angle between T1-hip axis and vertical) correlation with health related quality of life (HRQOL) measures and outperforms SVA. Besides, PT was shown to play an important role in the sagittal balance as it represented a compensatory mechanism in the chain of correlation of sagittal alignment. Therefore, it is essential to explore the parameters which play a key role in the sagittal balance when making surgical plan.12,23,24 However, to our knowledge, no relevant studies have been conducted to explore which radiological parameters are significantly different between sagittal balanced and imbalanced ADS patients.
We divided the 99 recruited patients into 2 groups according to whether their sagittal plane were balanced in lateral spine radiographs25,26 to explore the different parameters between balanced and imbalanced ADS patients. In our study, we found that nearly 33% of ADS patients suffered from sagittal balance and there were significant differences in age, LL, PT, coronal Cobb angle, degree of apical vertebra rotation, and PI − LL between Group A and Group B; however, no significant difference was observed in gender, TK, TL, SS, and PI between 2 groups. Age, an important and independent factor, was observed older in imbalanced group than balanced group, indicating that older ADS patients were more easily suffered from sagittal imbalance, which should be considered into the surgical management. LL is an important parameter in the evaluation of ADS patients because lumbar hypolordosis is related to the spinopelvic orientation.35 In our study, LL in imbalanced group was less than that in balanced group. PT is also a crucial parameter in assessing ADS because high PT (increased pelvic retroversion) is a compensatory mechanism.19 Our results showed higher PT in imbalanced patients, compared with normal sagittal balance ADS patients (28 vs. 24, P = 0.031). PI − LL is a new parameter proposed by Schwab et al.27 In their opinion, this measure is important because surgical planning for a patient with a small LL relative to the PI, via an osteotomy or osteotomies, should take into account the amount of postoperative LL necessary to achieve a harmonious alignment. Our study showed higher PI − LL in imbalanced group, which represented the imbalance of sagittal plane and harmonious alignment of sagittal plane could be achieved if this parameter was considered in the surgical procedure.27 Besides, our study suggested that coronal radiographic parameters, such as coronal Cobb angle and degree of apical vertebra rotation, were significantly different between these 2 groups, which might be closely related to the etiology of ADS. The mechanism and etiology of ADS is multifactorial and is related to progressive degenerative disc disease, compression fractures, disorders of bone quality, and osteoarthritis that creates an asymmetrical deformity of the spine in the axial, coronal, and sagittal planes,4,36 indicating that both coronal risk factors inducing coronal deformity might play an important role in the sagittal imbalance in ADS patients.
There are some limitations of this study that should be addressed. First, all the patients we recruited in our study came from outpatient clinic of our hospital, which might result in the selection bias and could not represent the general characteristics of ADS in the overall populations. Second, no patients’ clinic outcomes, such as visual analog score (VAS) and Oswestry Disability Index (ODI), were observed in our study, which could not detect the possible relationship between clinic outcomes and radiographic parameters. Besides, our study was a single-center study and there were also some selection in our research. Therefore, large-scaled and multicenter studies should be performed to make a more comprehensive research into the radiographic parameters and explore the possible parameters which play a key role in the sagittal balance in ADS patients.
CONCLUSION
Our study provided the general radiographic parameters of ADS. Weak but significant correlations between coronal Cobb angle and curve segments and degree of apical vertebra rotation were observed. Furthermore, age, coronal Cobb angle, LL, PT, and PI − LL were significantly different between sagittal balanced and imbalanced ADS patients.
Footnotes
Abbreviations: ADS = adult degenerative scoliosis, AIS = adolescent idiopathic scoliosis, ASD = adult spinal deformity, HRQOL = correlation with health related quality of life, LL = lumbar lordosis, ODI = Oswestry Disability Index, PI = pelvic incidence, PI–LL = PI minus LL, PT = pelvic tilt, SS = sacral slope, SVA = sagittal vertical axis, T1-SPI = angle between T1-hip axis and vertical, TK = thoracic kyphosis, TL = thoracolumbar kyphosis, VAS = visual analog score.
C.Y., M.Y., and Y.C. are cofirst authors.
This study was supported by “1255” Project Foundation of Changhai Hospital, Shanghai, China.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Schwab FJ, Smith VA, Biserni M, et al. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine 2002; 27:387–392. [DOI] [PubMed] [Google Scholar]
- 2.Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 2010; 28:E1. [DOI] [PubMed] [Google Scholar]
- 3.Jimbo S, Kobayashi T, Aono K, et al. Epidemiology of degenerative lumbar scoliosis: a community-based cohort study. Spine 2012; 37:1763–1770. [DOI] [PubMed] [Google Scholar]
- 4.Kotwal S, Pumberger M, Hughes A, et al. Degenerative scoliosis: a review. HSS J 2011; 7:257–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu Y, Han S, Zhao H, et al. Comparative analysis of serum proteomes of degenerative scoliosis. J Orthop Res 2011; 29:1896–1903. [DOI] [PubMed] [Google Scholar]
- 6.Watanuki A, Yamada H, Tsutsui S, et al. Radiographic features and risk of curve progression of de-novo degenerative lumbar scoliosis in the elderly: a 15-year follow-up study in a community-based cohort. J Orthop Sci 2012; 17:526–531. [DOI] [PubMed] [Google Scholar]
- 7.Smith JS, Shaffrey CI, Fu KM, et al. Clinical and radiographic evaluation of the adult spinal deformity patient. Neurosurg Clin N Am 2013; 24:143–156. [DOI] [PubMed] [Google Scholar]
- 8.Fu L, Chang MS, Crandall DG, et al. Does obesity affect surgical outcomes in degenerative scoliosis? Spine 2014; 39:2049–2055. [DOI] [PubMed] [Google Scholar]
- 9.Kleinstueck FS, Fekete TF, Jeszenszky D, et al. Adult degenerative scoliosis: comparison of patient-rated outcome after three different surgical treatments. Eur Spine J 2014; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 10.Haque RM, Uddin OM, Ahmed Y, et al. “Push-Through” Rod Passage Technique for the Improvement of Lumbar Lordosis and Sagittal Balance in Minimally Invasive Adult Degenerative Scoliosis Surgery. J Spinal Disord Tech 2014; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 11.Pritchett JW, Bortel DT. Degenerative symptomatic lumbar scoliosis. Spine 1993; 18:700–703. [DOI] [PubMed] [Google Scholar]
- 12.Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 2005; 30:682–688. [DOI] [PubMed] [Google Scholar]
- 13.Cho KJ, Kim YT, Shin SH, et al. Surgical treatment of adult degenerative scoliosis. Asian Spine J 2014; 8:371–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palmisani M, Dema E, Cervellati S. Surgical treatment of adult degenerative scoliosis. Eur Spine J 2013; 22 Suppl. 6:S829–S833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mac-Thiong JM, Labelle H, Charlebois M, et al. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine 2003; 28:1404–1409. [DOI] [PubMed] [Google Scholar]
- 16.Li WS, Li G, Chen ZQ, et al. Sagittal plane analysis of the spine and pelvis in adult idiopathic scoliosis. Chin Med J 2010; 123:2978–2982. [PubMed] [Google Scholar]
- 17.Savage JW, Patel AA. Fixed sagittal plane imbalance. Global Spine J 2014; 4:287–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lazennec JY, Ramare S, Arafati N, et al. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 2000; 9:47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine 2009; 34:E599–E606. [DOI] [PubMed] [Google Scholar]
- 20.Lonner BS, Auerbach JD, Sponseller P, et al. Variations in pelvic and other sagittal spinal parameters as a function of race in adolescent idiopathic scoliosis. Spine 2010; 35:E374–E377. [DOI] [PubMed] [Google Scholar]
- 21.Yong Q, Zhen L, Zezhang Z, et al. Comparison of sagittal spinopelvic alignment in Chinese adolescents with and without idiopathic thoracic scoliosis. Spine 2012; 37:E714–E720. [DOI] [PubMed] [Google Scholar]
- 22.Upasani VV, Tis J, Bastrom T, et al. Analysis of sagittal alignment in thoracic and thoracolumbar curves in adolescent idiopathic scoliosis: how do these two curve types differ? Spine 2007; 32:1355–1359. [DOI] [PubMed] [Google Scholar]
- 23.O'Shaughnessy BA, Ondra SL. Measuring, preserving, and restoring sagittal spinal balance. Neurosurg Clin N Am 2007; 18:347–356. [DOI] [PubMed] [Google Scholar]
- 24.Yagi M, Hosogane N, Okada E, et al. Factors affecting the postoperative progression of thoracic kyphosis in surgically treated adult patients with lumbar degenerative scoliosis. Spine 2014; 39:E521–E528. [DOI] [PubMed] [Google Scholar]
- 25.Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine 2012; 37:1479–1489. [DOI] [PubMed] [Google Scholar]
- 26.Kim HJ, Yagi M, Nyugen J, et al. Combined anterior-posterior surgery is the most important risk factor for developing proximal junctional kyphosis in idiopathic scoliosis. Clin Orthop Relat Res 2012; 470:1633–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schwab F, Ungar B, Blondel B, et al. Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine 2012; 37:1077–1082. [DOI] [PubMed] [Google Scholar]
- 28.Blondel B, Wickman AM, Apazidis A, et al. Selection of fusion levels in adults with spinal deformity: an update. Spine J 2013; 13:464–474. [DOI] [PubMed] [Google Scholar]
- 29.Faldini C, Di Martino A, De Fine M, et al. Current classification systems for adult degenerative scoliosis. Musculoskelet Surg 2013; 97:1–8. [DOI] [PubMed] [Google Scholar]
- 30.Ploumis A, Transfledt EE, Denis F. Degenerative lumbar scoliosis associated with spinal stenosis. Spine J 2007; 7:428–436. [DOI] [PubMed] [Google Scholar]
- 31.Mao ZG, Wu QX, Zhu JM, et al. Surgical treatment for degenerative lumbar scoliosis associated with spinal stenosis. Zhongguo Gu Shang 2008; 21:860–862. [PubMed] [Google Scholar]
- 32.Blondel B, Schwab F, Ungar B, et al. Impact of magnitude and percentage of global sagittal plane correction on health-related quality of life at 2-years follow-up. Neurosurgery 2012; 71:341–348.discussion 8. [DOI] [PubMed] [Google Scholar]
- 33.Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine 2013; 38:E803–E812. [DOI] [PubMed] [Google Scholar]
- 34.Liu H, Li S, Zheng Z, et al. Pelvic retroversion is the key protective mechanism of L4-5 degenerative spondylolisthesis. Eur Spine J 2015; 24:1204–12110. [DOI] [PubMed] [Google Scholar]
- 35.Hong JY, Suh SW, Modi HN, et al. Reliability analysis for radiographic measures of lumbar lordosis in adult scoliosis: a case-control study comparing 6 methods. Eur Spine J 2010; 19:1551–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tempel ZJ, Gandhoke GS, Bonfield CM, et al. Radiographic and clinical outcomes following combined lateral lumbar interbody fusion and posterior segmental stabilization in patients with adult degenerative scoliosis. Neurosurg Focus 2014; 36:E11. [DOI] [PubMed] [Google Scholar]


