Abstract
Epidemiologic studies investigating the differences in respiratory outcomes between asthma–chronic obstructive pulmonary disease overlap syndrome (ACOS) and chronic obstructive pulmonary disease (COPD) in an Asian population are lacking.
We conducted a population-based cohort study to compare the incidence of acute respiratory events between ACOS and COPD cohorts in Taiwan. This study investigated the incidence of acute respiratory events, namely, pneumonia, acute exacerbation, acute respiratory failure, and cardiopulmonary arrest, in 8571 patients with physician-diagnosed ACOS between 2000 and 2007 from the Longitudinal Health Insurance Database. The comparison cohort comprised 17,088 COPD patients, frequency-matched according to age, sex, and the index-year. The duration of follow-up was measured for each patient from the index date to 5 years thereafter. We used univariable and multivariable Poisson regression models to analyze the risk of acute respiratory events by including the variables of sex, age, and comorbidity.
The overall prevalence of ACOS was approximately 17.4% in patients with COPD. The prevalence of ACOS increased with age. During the 5-year follow-up, a greater incidence of acute respiratory events was observed in the ACOS cohort than in the COPD cohort (11.5 and 4.62, per 100 person-years, respectively) with an adjusted incidence rate ratio (IRR) of 1.72 (95% confidence interval [CI] = 1.63–1.81). Compared with the COPD cohort, the ACOS patients had a 1.13-fold adjusted IRR of pneumonia (95% CI = 1.07–1.20) and a 2.58-fold adjusted IRR of acute exacerbation (95% CI = 2.43–2.74). Clinicians should be aware of frequent exacerbation of ACOS and prescribe appropriate treatment.
INTRODUCTION
Asthma and chronic obstructive pulmonary disease (COPD) are highly prevalent chronic illnesses in the general population.1 These 2 obstructive airway diseases are characterized by chronic inflammation involving the entire respiratory tract. Airflow obstruction is usually intermittent and reversible in asthma, but is progressive and largely irreversible in COPD.
A considerable proportion of adult patients aged >40 years who present with symptoms of chronic airway disease have features of both asthma and COPD.2 The term asthma–COPD overlap syndrome (ACOS) was proposed for the clinical phenotype characterized by the overlap of asthma and COPD.3,4 Patients with ACOS are usually smokers with asthma or nonsmokers with long-standing asthma that progresses to COPD. Concurrent doctor-diagnosed asthma and COPD have been reported in between 15% and 20% of patients.5–7 The prevalence of ACOS increases with age, with an estimated prevalence of <10% in patients <50 years and >50% in patients aged ≥80 years.6
The presence of histamine airway hyperresponsiveness in patients with COPD has been associated with an increase in exacerbations and overall mortality.8 Recent Western studies have reported that patients with ACOS had a diminished health-related quality of life and a greater risk of exacerbation and hospitalization than those with COPD did in the United States and 5 major Latin American cities.9,10 However, epidemiologic studies investigating the respiratory outcomes of the different phenotypes of chronic airway obstruction in an Asian population are lacking. Therefore, we conducted a population-based cohort study to compare the incidence of acute respiratory events between ACOS and COPD cohorts in Taiwan.
METHODS
Data Source
The National Health Insurance (NHI) program is a single-payer universal insurance program that originated in 1995. This program provides medical coverage to >99% of the population and has contracts with 97% of hospitals and clinics in Taiwan.11 The National Health Research Institutes established the National Health Insurance Research Database (NHIRD), which contains annual registration files and original claims data for reimbursement. The present study was based on data obtained from the Longitudinal Health Insurance Database 2000 (LHID2000), which is a subset of the NHIRD. The LHID2000 contains 1 million insurants data randomly sampled from the original NHIRD and includes all inpatient claims, ambulatory care claims, and prescriptions for each insurant from 1996 to 2011. Each insurant's diagnosis codes are classified using the International Classification of Disease Diagnoses, Ninth Revision of Clinical Modification (ICD-9-CM). The longitudinal medical history for all insurants is obtained by linking the files through the encoded personal identification number, which secures personal confidentiality and prevents ethical violations regarding the use of claims data. Previous studies have described the high accuracy and validity of ICD-9-CM diagnoses in the NHIRD.12–14 This study was exempted from full review by the Institutional Research Ethics Committee of China Medical University, Taichung, Taiwan (CMU-REC-101–012).
Sampled Patients
Figure 1 shows the process of selecting participants for study cohorts. We identified patients diagnosed with COPD (ICD-9-CM Codes 491, 492, and 496) from claims data for 2000 to 2007. Patients with COPD aged ≥20 with concurrent physician-diagnosed asthma (ICD-9-CM Code 493) were selected for the ACOS cohort. The asthma diagnosis date was defined as the index date. The comparison cohort was randomly selected from the rest of the COPD patients without a diagnosis of asthma. For each patient in the ACOS cohort, 2 controls were randomly selected and frequency matched according to age (every 5 years), sex, and the year of the index date. All patients in both the cohorts were followed up for 5 years following the date on which they were included in the cohort. In total, 8571 patients were included in the ACOS cohort, and 17,088 patients were included in the COPD cohort.
FIGURE 1.
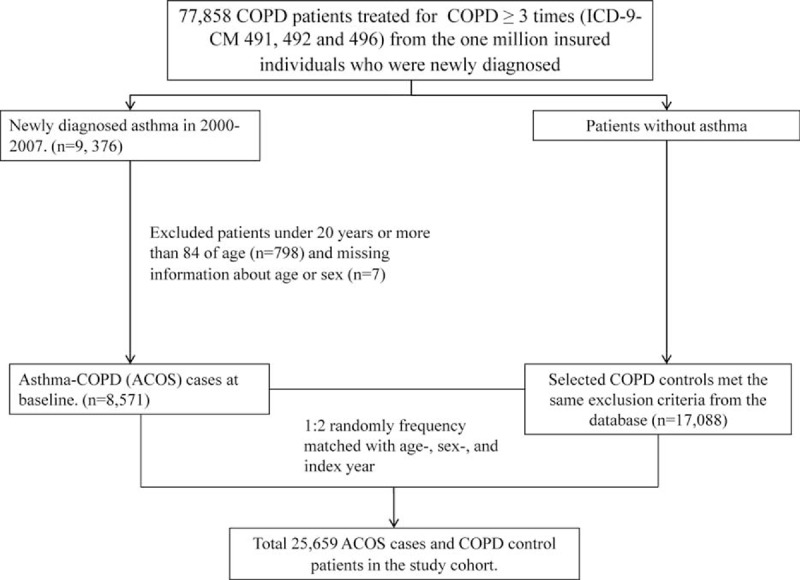
Process of selecting participants for study cohorts.
Outcome
The duration of follow-up (person-years) was measured for each patient from the index date to 5 years thereafter or until the patient was censored because of death or withdrawal from the insurance system. The primary outcome of this study was determined according to the number of acute respiratory events, namely, pneumonia (ICD-9-CM Codes 480–486), acute exacerbation (ICD-9-CM Codes 491, 492, and 496), acute respiratory failure (ICD-9-CM Code 518.81), and cardiopulmonary arrest (ICD-9-CM Codes 799.1, 798, and 427.5). These data were based on emergency room and hospitalization records from the index date to 5 years thereafter.
Comorbidities and Medications
The examined baseline comorbidities were malignancy (ICD-9-CM Codes 140–208), autoimmune disease (ICD-9-CM Codes 710.0, 710.1, 710.2, 710.3, and 714), stroke (ICD-9-CM Codes 430–438), diabetes (ICD-9-CM Code 250), and heart failure (ICD-9-CM Code 428), and the examined medications were inhaled short-acting β-agonists (SABAs), inhaled short-acting muscarinic antagonists (SAMAs), a combination of inhaled SABAs and SAMAs, inhaled long-acting β-agonists (LABAs), inhaled long-acting muscarinic antagonists (LAMAs), and a combination of inhaled corticosteroids (ICSs) and LABAs or ICSs and LAMAs.
Statistical Analysis
First, we calculated the prevalence of concurrent physician-diagnosed asthma in patients with COPD from 2000 to 2007. The demographic distribution, comorbidities, and medications were compared between the ACOS and COPD cohorts and examined using the t test or χ2 test, as appropriate. Follow-up time (in person-years) was used to estimate incidence density rates. The incidence rate ratio (IRR) of the ACOS cohort to the COPD cohort and 95% confidence interval (CI) were estimated using Poisson regression. The multivariable Poisson regression models were adjusted for age, sex, comorbidity, and medication. Data management and statistical analyses were performed using SAS Version 9.3 (SAS Institute Inc., Cary, NC); P < 0.05 indicated statistical significance.
RESULTS
The prevalence of concurrent diagnoses of COPD and asthma increased slightly from 16.3% in 2000 to 17.8% in 2007. The overall prevalence of ACOS was approximately 17.4% in patients with COPD. The prevalence of ACOS increased with age (9.2% in patients <50, 17.1% in patients 50–64, 21.7% in patients 65–79, and 21.7% in patients ≥80 years of age) (data not shown).
Comparison of Baseline Characteristics Between COPD and ACOS Cohorts
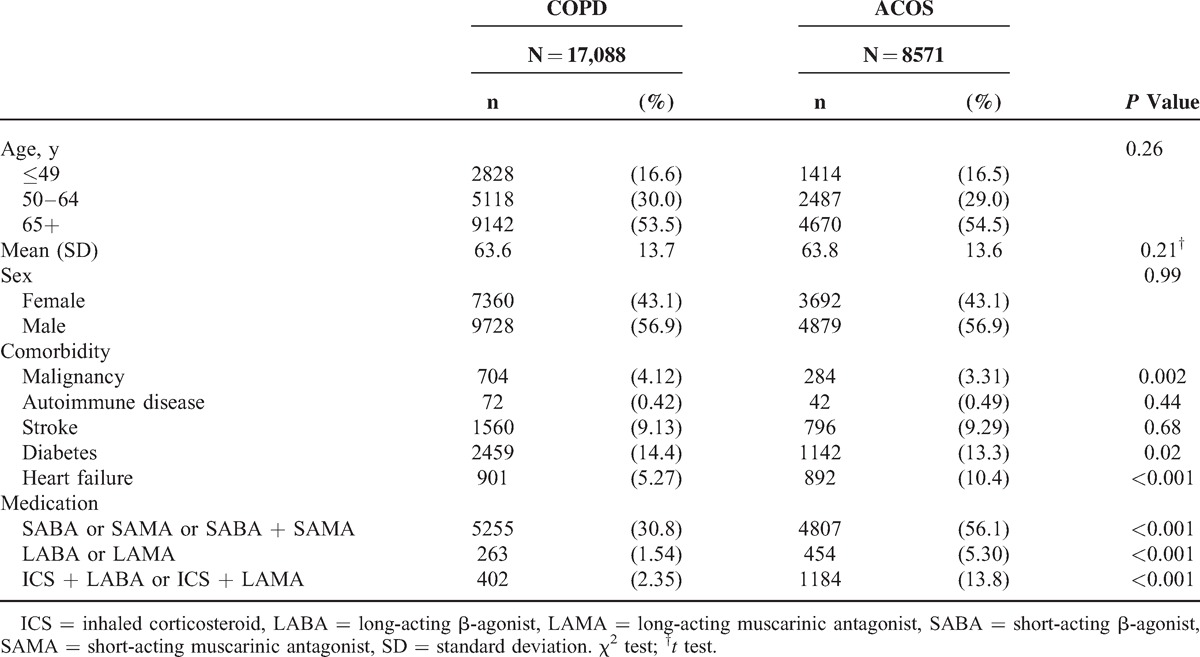
The baseline characteristics, comorbidities, and medications of the patients in both cohorts are presented in Table 1. The patients in both cohorts were predominantly men aged ≥65 years. The mean ages of the patients in the ACOS and COPD cohorts were 63.8 (±13.6) and 63.6 (±13.7) years, respectively. Compared to patients with COPD, patients with ACOS exhibited a higher prevalence of heart failure and inhaled medication use. By contrast, the patients with COPD exhibited a greater prevalence of malignancy and diabetes than did the ACOS patients (4.12% vs 3.31%, P = 0.002 and 14.4% vs 13.3%, P = 0.02).
TABLE 1.
Comparison of Baseline Characteristics Between ACOS and COPD Patients
Comparison of Acute Respiratory Events Between COPD and ACOS Cohorts
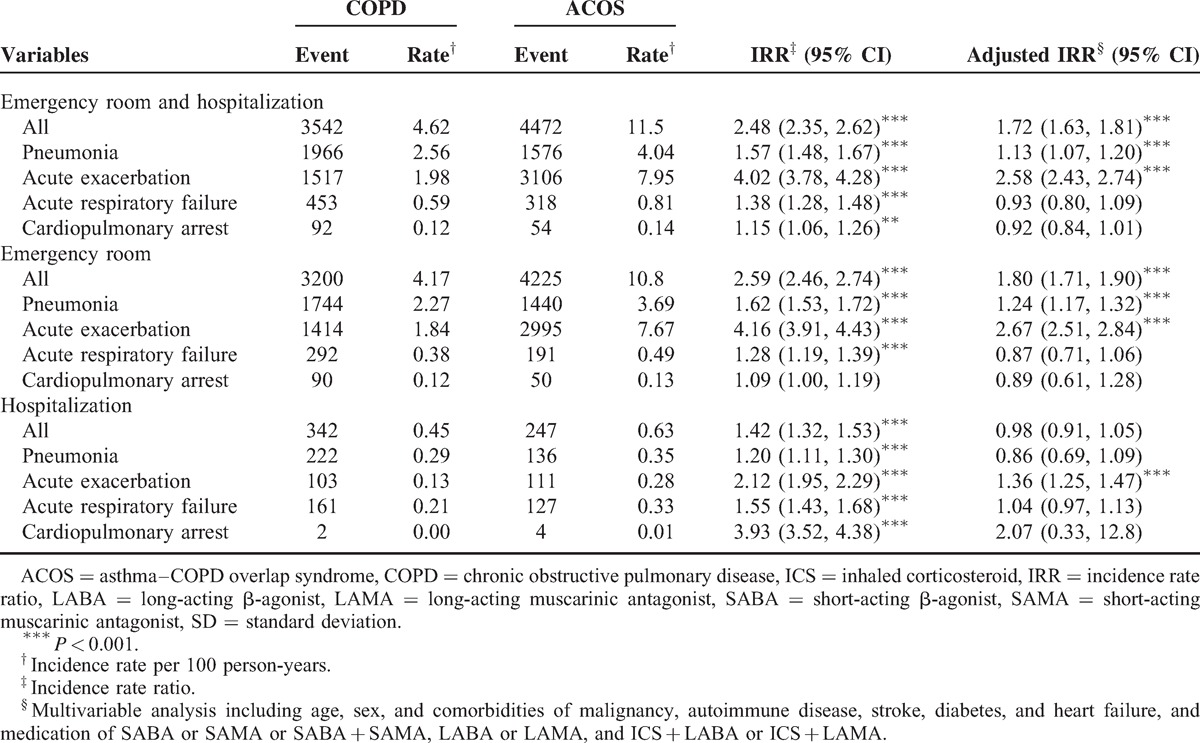
During the 5-year follow-up, a greater incidence of acute respiratory events was observed in the ACOS cohort than in the COPD cohort (11.5 and 4.62, per 100 person-years, respectively), with an adjusted IRR of 1.72 (95% CI = 1.63–1.81) (Table 2). The patients with ACOS had a higher incidence of pneumonia (4.04 vs 2.56 per 100 person-years) and acute exacerbation (7.95 vs 1.98 per 100 person-years) than the patients in the COPD cohort did, with adjusted IRRs of 1.13 (95% CI = 1.07–1.20) and 2.58 (95% CI = 2.43–2.74), respectively. Further analysis of emergency room records revealed a greater incidence of pneumonia and acute exacerbation in the patients with ACOS than in the patients with COPD. The patients with ACOS also exhibited a greater risk of hospitalization for acute exacerbation compared with the COPD cohort, and the adjusted IRR was 1.36 (95% CI = 1.25–1.47). The risk of respiratory failure and cardiopulmonary arrest in the patients with ACOS did not significantly increase compared with that in patients with only COPD.
TABLE 2.
Comparisons of Acute Respiratory Events Between ACOS and COPD Cohorts
Comparisons of Acute Respiratory Events Between ACOS and COPD Cohorts Stratified According to Age, Sex, and Comorbidity
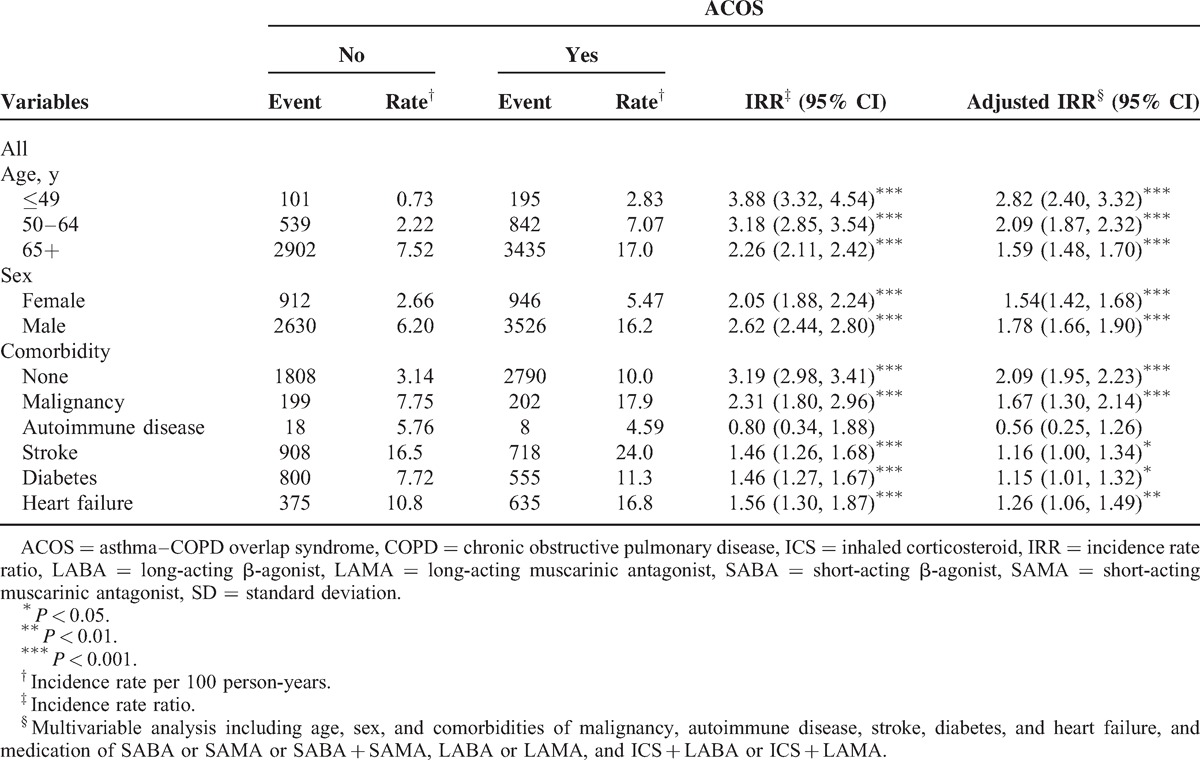
The incidence of acute respiratory events increased with age in the ACOS and COPD cohorts. The ACOS cohort had a greater incidence of acute respiratory events than the COPD cohort did in all age groups (2.83 vs 0.73 per 100 person-years for patients <50 years, 7.07 vs 2.22 per 100 person-years for patients aged 50–64 years, and 17.0 vs 7.52 per 100 person-years for patients >64 years). Men had a greater incidence of acute respiratory events than women did in the ACOS (16.2 vs 5.47 per 100 person-years) and COPD (6.2 vs 2.66 per 100 person-years) cohorts. The incidence of acute respiratory events in the ACOS cohort was greater than that in the COPD cohort for both the sexes. However, compared with the COPD cohort, the ACOS cohort exhibited greater risks of acute respiratory events irrespective of age and sex. The patients with ACOS exhibited a substantially greater risk of acute respiratory events than the patients with COPD did when the patients did not have any comorbid disorders (adjusted IRR = 2.09, 95% CI = 1.95–2.23). The ACOS patients also exhibited greater risks of acute respiratory events than the COPD patients when the patients had comorbidities, except for autoimmune diseases (Table 3).
TABLE 3.
Comparisons of Acute Respiratory Events Between ACOS and COPD Cohorts Stratified by Sex, Age, and Comorbidity
DISCUSSION
This study is the first to investigate the prevalence of ACOS and compare the incidence of acute respiratory events between ACOS and COPD cohorts in an Asian population. Our population-based cohort study showed that approximately 17.4% of patients with COPD had concurrent physician-diagnosed asthma between 2000 and 2007 and the prevalence increased with age. Hardin et al9 performed a cross-sectional COPDGene study and found that 13% of COPD patients had a self-reported history of physician-diagnosed asthma.15 Tálamo et al16 found that 23% of COPD patients had self-reported medically diagnosed asthma in 5 Latin American cities.17 Menezes et al10 reported that 1.8% of the PLATINO population was classified into the ACOS group. The difference in ACOS prevalence between this study and the Western studies can be attributed to the use of medical reimbursement records of physician-diagnosed diseases in our study and worldwide variation in the prevalence of asthma.18,19
This study showed that the patients with ACOS had more episodes of acute respiratory events compared with the patients with only COPD (11.5 vs 4.62 per 100 person-years). After we adjusted for confounders, the patients with ACOS exhibited an overall 1.72-fold greater risk of acute respiratory events than patients with only COPD. Further analysis of acute respiratory events revealed that the ACOS patients had a 1.13-fold greater risk of pneumonia and a 2.58-fold greater risk of acute exacerbation compared with patients in the COPD cohort. Our findings are consistent with those of the COPDGene study, which also showed a greater risk of frequent exacerbation in ACOS patients than in COPD patients.9 Studies have demonstrated that patients with ACOS have poorer pulmonary function, a poorer general health status, and more respiratory symptoms, which may lead to more incidences of acute exacerbation and hospitalization.10,20,21 The findings indicate a considerable difference in respiratory outcome among the clinical phenotypes of COPD. COPD is a heterogeneous disease with a wide range of clinical phenotypes, and not all patients respond to all drugs available for treatment.22 Although the new Global Initiative for Chronic Obstructive Lung Disease updates have addressed the concept of clinical phenotypes of COPD, they do not elaborate an appropriate therapy for ACOS. ACOS is associated with an enhanced response to ICSs because of the predominance of eosinophilic bronchial inflammation.23,24 Clinicians should be aware of frequent exacerbation of ACOS and can prescribe ICSs and LABAs regardless of the severity of airflow obstruction.25
Compared with the COPD cohort, the ACOS cohort exhibited greater risks of acute respiratory events in all age groups for both women and men. For the patients without comorbidities, the risks of acute respiratory events were greater in the patients with ACOS than the patients with only COPD. For the patients with any comorbidity except autoimmune disease, the ACOS patients still had greater risks of acute respiratory events than patients with only COPD. These results are robust because several multivariable model analyses were performed to assess the difference in the risk of acute respiratory events between the ACOS and COPD cohorts. Therefore, clinicians can treat COPD patients according to clinical phenotype to implement personalized therapy regimens.26,27 Patients with an ACOS phenotype may show an enhanced response to inhaled corticosteroids, and infrequent exacerbators can receive only bronchodilators.25
The strength of this cohort longitudinal study is the use of medical reimbursement records of physician-diagnosed diseases in the NHIRD rather than patient-reported diagnoses and outcomes. Because NHI is universal and mandatory in Taiwan, this study obtained detailed information on medication for each study patient. Moreover, each NHI beneficiary is assigned a unique personal identification number. Therefore, every patient can be traced in the NHIRD records throughout the follow-up period.
However, several limitations must be considered when interpreting these findings. The NHIRD does not provide detailed information related to the symptoms of the patients, such as the results of a breathless assessment, pulmonary function test, and laboratory examination. Thus, this study could not use symptoms, breathlessness, and spirometric results to classify the COPD groups in accordance with the Global Initiative for COPD.28
In conclusion, this study determined that patients with ACOS had an increased risk of acute respiratory events, including pneumonia and acute exacerbation, compared with patients with only COPD in an Asian population. Clinicians should be aware of this epiphenomena and treat COPD patients according to clinical phenotype.
Footnotes
Abbreviations: ACOS = asthma–COPD overlap syndrome, CI = confidence interval, COPD = chronic obstructive pulmonary disease, ICD-9-CM = International Classification of Disease Diagnoses, Ninth Revision of Clinical Modification, IRR = incidence rate ratio, NHIRD = National Health Insurance Research Database.
All authors have contributed significantly, and they all are in agreement with the content of the manuscript. Conception/Design: W-SC, C-HK; Collection and/or assembly of data: all authors; Data analysis and interpretation: all authors; Manuscript writing: all authors; and Final approval of manuscript: all authors. C-HK is the guarantor of this article, taking responsibility for the integrity of the work as a whole, from inception to publication.
This study is supported in part by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center of Excellence (MOHW104-TDU-B-212-113002); China Medical University Hospital, Academia Sinica Taiwan Biobank, Stroke Biosignature Project (BM104010092); NRPB Stroke Clinical Trial Consortium (MOST 103-2325-B-039 -006); Tseng-Lien Lin Foundation, Taichung, Taiwan; Taiwan Brain Disease Foundation, Taipei, Taiwan; Katsuzo and Kiyo Aoshima Memorial Funds, Japan; and Health and Welfare Surcharge of Tobacco Products, China Medical University Hospital Cancer Research Center of Excellence (MOHW104-TDU-B-212-124-002, Taiwan). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding was received for this study.
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.de Marco R, Pesce G, Marcon A, et al. The coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle-aged and elderly people from the general population. PloS One 2013; 8:e62985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakawah MO, Hawkins C, Barbandi F. Asthma, chronic obstructive pulmonary disease (COPD), and the overlap syndrome. J Am Board Fam Med 2013; 26:470–477. [DOI] [PubMed] [Google Scholar]
- 3.Soler-Cataluña JJ, Cosío B, Izquierdo JL, et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch Bronconeumol 2012; 48:331–337. [DOI] [PubMed] [Google Scholar]
- 4.Louie S, Zeki AA, Schivo M, et al. The asthma-chronic obstructive pulmonary disease overlap syndrome: pharmacotherapeutic considerations. Expert Rev Clin Pharmacol 2013; 6:197–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McDonald VM, Simpson JL, Higgins I, et al. Multidimensional assessment of older people with asthma and COPD: clinical management and health status. Age Ageing 2011; 40:42–49. [DOI] [PubMed] [Google Scholar]
- 6.Soriano JB, Davis KJ, Coleman B, et al. The proportional Venn diagram of obstructive lung disease: two approximations from the United States and the United Kingdom. Chest 2003; 124:474–481. [DOI] [PubMed] [Google Scholar]
- 7.Diagnosis of Diseases of Chronic Airflow Limitation: Asthma COPD Asthma-COPD Overlap Syndrome. Global Initiative for Asthma (GINA) and Global Initiative for Chronic Obstructive Lung Disease (GOLD); 2014. www.ginasthma.org Accessed November 20, 2014. [Google Scholar]
- 8.Hospers JJ, Postma DS, Rijcken B, et al. Histamine airway hyper-responsiveness and mortality from chronic obstructive pulmonary disease: a cohort study. Lancet 2000; 356:1313–1317. [DOI] [PubMed] [Google Scholar]
- 9.Hardin M, Silverman EK, Barr RG, et al. COPDGene Investigators. The clinical features of the overlap between COPD and asthma. Respir Res 2011; 12:127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Menezes AM, Montes de Oca M, Pérez-Padilla R, et al. PLATINO Team. Increased risk of exacerbation and hospitalization in subjects with an overlap phenotype: COPD-asthma. Chest 2014; 145:297–304. [DOI] [PubMed] [Google Scholar]
- 11.Universal Health Coverage in Taiwan. National Health Insurance Administration, Ministry of Health and Welfare; 2014. http://www.nhi.gov.tw/english/index.aspx Accessed November 10, 2014. [Google Scholar]
- 12.Shen TC, Chung WS, Lin CL, et al. Does chronic obstructive pulmonary disease with or without type 2 diabetes mellitus influence the risk of lung cancer? Result from a population-based cohort study. PloS One 2014; 9:e98290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chung WS, Lin CL, Chen YF, et al. Increased stroke risk among adult asthmatic patients. Eur J Clin Invest 2014; 44:1025–1033. [DOI] [PubMed] [Google Scholar]
- 14.Chung WS, Lin CL, Ho FM, et al. Asthma increases pulmonary thromboembolism risk: a nationwide population cohort study. Eur Respir J 2014; 43:801–807. [DOI] [PubMed] [Google Scholar]
- 15.Regan EA, Hokanson JE, Murphy JR, et al. Genetic epidemiology of COPD (COPDGene) study design. COPD 2010; 7:32–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tálamo C, de Oca MM, Halbert R, et al. PLATINO Team. Diagnostic labeling of COPD in five Latin American cities. Chest 2007; 131:60–67. [DOI] [PubMed] [Google Scholar]
- 17.Menezes AM, Victora CG, Perez-Padilla R. The Platino project: methodology of a multicenter prevalence survey of chronic obstructive pulmonary disease in major Latin American cities. BMC Med Res Methodol 2004; 4:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lai CK, Beasley R, Crane J, et al. Global variation in the prevalence and severity of asthma symptoms: phase three of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax 2009; 64:476–483. [DOI] [PubMed] [Google Scholar]
- 19.Patel SP, Jarvelin MR, Little MP. Systematic review of worldwide variations of the prevalence of wheezing symptoms in children. Environ Health 2008; 7:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mannino DM, Gagnon RC, Petty TL, et al. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med 2000; 160:1683–1689. [DOI] [PubMed] [Google Scholar]
- 21.Kauppi P, Kupiainen H, Lindqvist A, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma 2011; 48:279–285. [DOI] [PubMed] [Google Scholar]
- 22.Gold DL, Dawson M, Yang H, et al. Clinical trial simulation to assist in COPD trial planning and design with a biomarker-based diagnostic: when to pull the trigger? COPD 2014; 11:226–235. [DOI] [PubMed] [Google Scholar]
- 23.Papi A, Romagnoli M, Baraldo S, et al. Partial reversibility of airflow limitation and increased exhaled NO and sputum eosinophilia in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2000; 162:1773–1777. [DOI] [PubMed] [Google Scholar]
- 24.Siva R, Green RH, Brightling CE, et al. Eosinophilic airway inflammation and exacerbations of COPD: a randomised controlled trial. Eur Respir J 2007; 29:906–913. [DOI] [PubMed] [Google Scholar]
- 25.Miravitlles M, Soler-Cataluna JJ, Calle M, et al. Treatment of COPD by clinical phenotypes: putting old evidence into clinical practice. Eur Respir J 2013; 41:1252–1256. [DOI] [PubMed] [Google Scholar]
- 26.Miravitlles M, Calle M, Soler-Cataluna JJ. Clinical phenotypes of COPD: identification, definition and implications for guidelines. Arch Bronconeumol 2012; 48:86–98. [DOI] [PubMed] [Google Scholar]
- 27.Miravitlles M, Soler-Cataluña JJ, Calle M, et al. A new approach to grading and treating COPD based on clinical phenotypes: summary of the Spanish COPD guidelines (GesEPOC). Prim Care Respir J 2013; 22:117–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Decramer M, Vestbo J, Bourbeau J, et al. Global Strategy for the Diagnosis, Management, and Prevention for Chronic Obstructive Pulmonary Disease; 2014. Accessed November 5, 2014. [Google Scholar]


