Abstract
The elderly population has significantly increased in China. However, data regarding renal histopathology in this population is lacking. The present study retrospectively analyzed renal disease spectrum of 430 elderly patients who had received renal biopsy at Peking University First Hospital between January 2003 and December 2012.
Among 6049 patients receiving renal biopsies during the same period, 430 (7.10%) were elderly (≥65 years). The ratio of male (263 patients) to female (167 patients) was 1.57:1, with an age of 70.29 ± 3.99 (range 65–82) years at the time of biopsy. The most common indication for renal biopsy was nephrotic syndrome (59.53%), followed by acute kidney injury (AKI, 19.53%) and chronic glomerulonephritis (CGN, 16.05%). The most common renal histopathology in primary glomerular disease was idiopathic membranous nephropathy (iMN, 61.02%), followed by IgA nephropathy (18.22%), minimal change disease (MCD, 9.32%) and focal segmental glomerulosclerosis (6.78%). ANCA-associated vasculitis (AAV, 43.95%) was the leading secondary glomerular disease, followed by HBV-related glomerulonephritis (HBV-GN, 24.2%), and amyloidosis (14.01%). In patients with nephrotic syndrome, iMN (50%) was the leading cause, followed by HBV-GN (16.02%), MCD (7.81%), and amyloidosis (7.81%). In patients with iMN, 89.5% presented as nephrotic syndrome, 8.39% as CGN. In patients with AKI, the leading cause was AAV (48.12%), followed by acute interstitial nephritis (20.48%) and acute tubular necrosis (8.43%).
In conclusion, in elderly Chinese patients, the most common renal histopathology pattern was iMN in patients with nephrotic syndrome, and AAV in patients with AKI.
INTRODUCTION
The trend of proportion in global elderly population is steadily increasing; especially in low- and middle-income countries.1 The elderly population (those aged 65 and over) in China is growing, with 102 million, or over one-fifth of the world elderly population in 2005. The percentage of elderly in China is predicted to triple from 8% to 24% by 2050, to a total number of 322 million.2
As life expectancy increases, more elderly patients are surviving longer with acute and chronic diseases.3 The range of renal diseases in the elderly patients differs from that in younger ones.4 As the advanced age is no longer a contraindication for renal biopsy, renal replacement therapy, immunosuppressive therapy, and even renal transplantation,3,5 the frequency of renal biopsy in elderly will increase. It is important to recognize the spectrum of kidney diseases in the elderly in order to understand the etiology as well as factors of disease progression to end stage renal disease (ESRD).
Several studies have focused on renal histopathology in elderly patients.6–10 Studies by Davison and Verde11,12 found that the most common indication for renal biopsy in elderly patients was nephritic syndrome and the most common primary glomerular disease (PGD) was idiopathic membranous nephropathy (iMN). A recent study from United States3 showed that acute kidney injury (AKI) was the leading indication for renal biopsy in very elderly patients (over 85 years). The most frequent cause of nephrotic-range proteinuria in the elderly was iMN in several studies,11–13 although one study indicated minimal change disease (MCD).14 For those with AKI, some studies suggested acute tubular necrosis (ATN) was the main cause,15,16 while others demonstrated that the crescentic glomerulonephritis (CreGN) was the leading cause.11,13 However, to the best of our knowledge, there was little data about the spectrum of kidney disease in the elderly in China.
The aim of this study is to investigate the renal histopathology spectrum of native renal biopsies in elderly patients (≥65 years) from one of the largest clinic nephrology centers in China.
PATIENTS AND METHODS
Patients
This retrospective study included all patients aged 65 years and over with native renal biopsy at Peking University First Hospital during a 10-years period from January 2003 to December 2012. During this period, a total of 6272 native renal biopsies were performed. Indications for renal biopsy were as follows: nephrotic syndrome or nephrotic range proteinuria, acute nephritic syndrome (ANS), rapidly progressive glomerulonephritis (RPGN) syndrome, chronic nephritic syndrome, asymptomatic hematuria with proteinuria, and AKI without confirmed diagnosis. The indication of renal biopsy remained unchanged during the whole observation period. Incomplete records (n = 16), inadequate biopsies (less than 10 glomeruli in the specimen for light microscopy when there were no typical findings in immunofluorescence or electron microscopy or absence of a glomerulus in immunofluorescence (n = 46), biopsies from transplant kidneys and nephrectomies (n = 16), age less than 14 years (n = 45) and repeat biopsies (n = 100) were excluded. Then, 6049 (96.44%) qualified cases were enrolled in this study. Data included demographic data, clinical and renal histopathological diagnosis. In these 6049 qualified cases, 430 (7.10%) were elderly patients.
Although different criteria for elderly (≥60 years11,15,17 vs. ≥65 years13,18) have been applied in previous publications in defining the cut-off for being elderly. In this study, individuals aged 65 years or above were considered elderly. Demographic and clinical records of each patient at the time of renal biopsy were collected.
The research was in compliance with the Declaration of Helsinki and was approved by the ethics committee of our hospital. Written informed consent was obtained from each participant.
Clinical Presentation
The main clinical syndromes observed in patients at the time of the renal biopsy were reported as our previous study: nephrotic syndrome (NS) was defined as proteinuria >3.5 g/day and hypoalbuminemia (serum albumin <30 g/L), without AKI, with or without hematuria. Chronic glomerulonephritis (CGN) was defined as proteinuria (1–3.5 g/day) and/or hematuria that persisted for at least 3 months. ANS was defined as hematuria, RBC casts and proteinuria (<3.5 g/day), which persisted less than 3 months. Asymptomatic urinary abnormality (AUA) was defined as proteinuria (<1.0 g/day) and hematuria found by routine check-up, without edema, hypertension or renal dysfunction.
Acute kidney injury was defined according to Moutzouris study3: if the indication recorded by the nephrologist was AKI, acute renal failure, acute on chronic renal failure (A on C), rapidly progressive glomerulonephritis, or if the clinical picture illustrated by the patients’ clinical data made a deterioration of renal function unlikely to be explained by chronic kidney injury (ie, absence of anemia, absence of small kidneys on renal-ultrasound, or improvement of renal function over time). If no definite indication was provided by the referring physician, AKI was presumed if serum creatinine doubled in patients with prior normal renal function, if serum creatinine increased by 50% within 3 months in patients with chronic kidney injury, and if serum creatinine was 2 mg/dl in patients with unknown baseline renal function. Patients in the AKI category could also present with or without proteinuria and/or hematuria.
Renal Histopathology
All specimens obtained from percutaneous renal biopsy were stained and analyzed in light microscopy (LM) and immunofluorescence (for IgG, IgA, IgM,C3, C4, C1q, and fibrinogen) by two pathologists. For LM, paraffin sections were routinely stained with periodic-acid Schiff, hematoxylin–eosin and periodic acid-silver methenamine, stained with Congo red when renal amyloidosis was considered according to the pathological features. Electron microscopy (EM) was performed on 418 biopsy specimens (97.2%) to confirm the light microscopic changes.
Furthermore, renal histopathological diagnosis was divided into four main categories: PGD, secondary glomerular disease (SGD), tubulointerstitial nephropathy (TIN), and (4) others.
PGD has been classified into nine entities19: IgA nephropathy (IgAN), non-IgA mesangial proliferative glomerulonephritis (MsPGN), iMN, MCD, FSGS, endocapillary proliferative glomerulonephritis (EnPGN), CreGN, membrane proliferative glomerulonephritis (MPGN) and the others; the last category includes rare diseases such as fibrillary glomerulonephritis, immunotactoid glomerulopathy, fibronectin glomerulopathy, and collagen III glomerulopathy.
SGD was classified as reported by Okpechi et al16 those involving systemic diseases such as lupus nephritis (LN) and cryoglobulinaemic GN, those related to infections, for example, HIV-related pathologies, endocarditis, hepatitis B and C, tuberculosis and others, diseases involving metabolic, hereditary and rare glomerular diseases and these included diabetic nephropathy (DN), amyloidosis, light chain deposition disease, Goodpasture disease, hereditary renal diseases such as Alport nephritis, Fabry disease, thin basement membrane disease, and other rare renal diseases, and diseases that affected the vessels included benign and malignant nephroangiosclerosis, pre-eclampsia, systemic vasculitis, systemic sclerosis, antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) and hemolytic uremic syndrome/thrombotic thrombocytopenic purpura.
Diseases classified as TIN included acute interstitial nephritis (AIN), chronic interstitial nephritis (CIN) and ATN.
Statistical Analysis
The data were entered into a personal computer and stored on a standard Microsoft Excel database. Analysis was carried out with the SPSS statistical package version 11.0 (SPSS Inc, Chicago, IL). The percentages or as mean ± standard deviation (SD) were used to describe categorical and continuous variables. Differences of qualitative data were compared using the chi-square test/Fisher exact test. The student t test was used to compare continuous variables. A P-value <0.05 was considered as significant.
RESULTS
Demographic Data of Elderly Patients with Renal Histopathology
Six thousand forty-nine qualified renal biopsies were identified, and 430 (7.10%) patients were elderly patients (≥65 years). The ratio of male (263 patients) to female (167 patients) was 1.57:1, with an age of 70.29 ± 3.99 (range 65–82) years at the time of biopsy.
The total number of elderly patients receiving renal biopsy increased yearly (Figure 1). The number of biopsies was increased from 13 male and 7 female in 2003 to 53 male and 36 female in 2012, respectively. The patients receiving renal biopsy were male predominant from 2003 to 2012.
FIGURE 1.
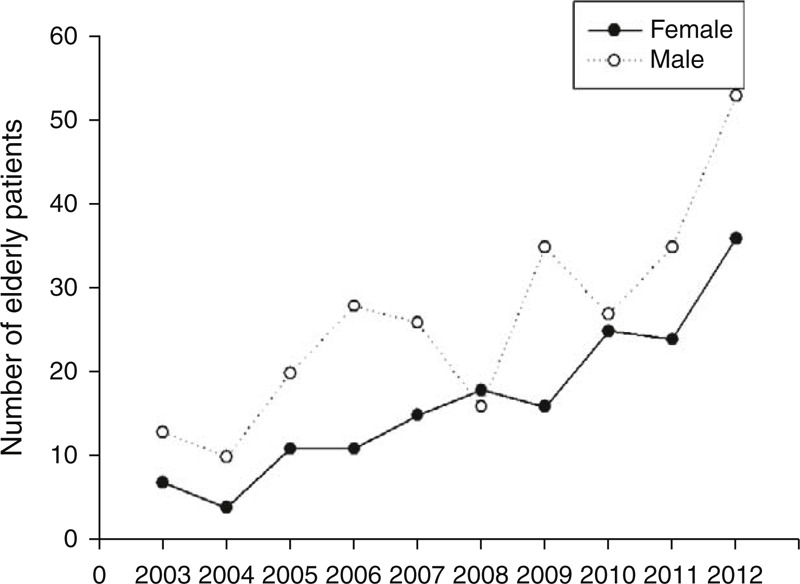
The number of elderly patients with renal biopsy distributed by year and gender. Open dots indicate male, dark dots indicate female.
Indications of Renal Biopsy and Category of Kidney Disease for the Elderly Patients
Indications for biopsy were shown in Figure 2A. The most frequent indication for renal biopsy in the elderly was nephrotic syndrome, accounting for more than half of the patients (n = 256, 59.53%), followed by AKI (n = 84, 19.53%), CGN (n = 69, 16.05%), and ANS (n = 17, 3.95%). AUA (n = 4, 0.94%) was the least common indication for renal biopsy of elderly patients.
FIGURE 2.
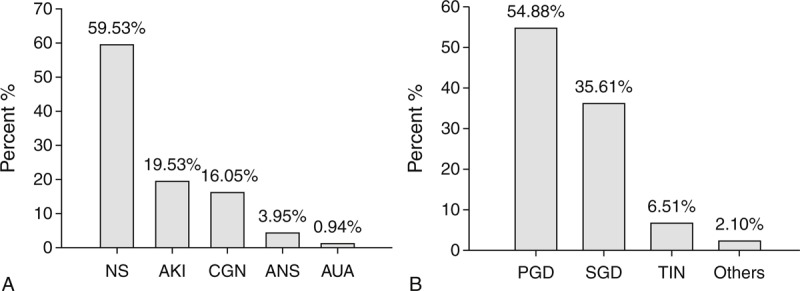
The indication for renal biopsy in the elderly (A) and the distribution of renal diseases categories in the elderly (B) Abbreviations: AKI: acute kidney injury; ANS: acute nephritic syndrome; AUA: asymptomatic urinary abnormality; CGN: chronic glomerulonephritis; NS: nephrotic syndrome; PGD: primary glomerular disease; SGD: secondary glomerular disease; TIN: tubulo-interstitial nephropathy.
The distribution of the four categories of kidney diseases in the elderly was shown in Figure 2B. PGDs occurred more frequently (n = 236, 54.88%) than SGDs (n = 157, 35.61%), TIN (n = 28, 6.51%), and others (n = 9, 2.10%).
Distribution of Histopathological Patterns of Elderly Patients with PGD
PGD was the most common category of kidney disease in the elderly. The distribution of histopathological patterns of PGDs in the elderly patients was shown in Figure 3A. IMN was the most common type, accounting for 61.02% (n = 144) of patients with PGDs, followed by IgAN (n = 43, 18.22%), MCD (n = 22, 9.32%), FSGS (n = 16, 6.78%), MsPGN (n = 4, 1.69%), CreGN (n = 3, 1.27%), MPGN (n = 3, 1.27%), and EnPGN (n = 1, 0.42%), respectively.
FIGURE 3.
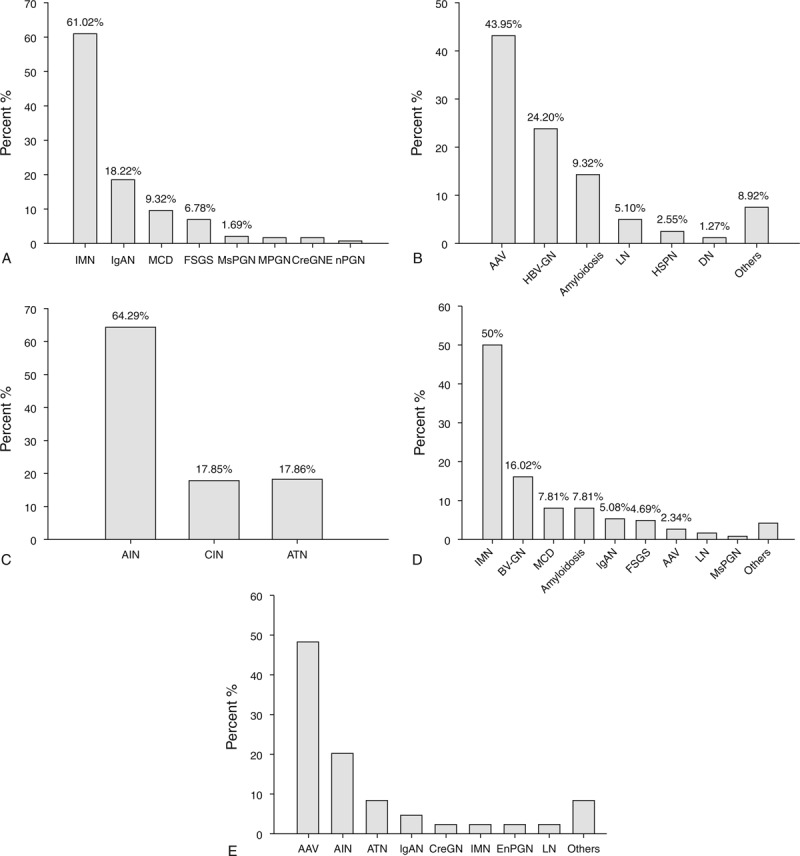
The frequency of histopathological patterns in the categories of PGD (A), SGD (B), TIN (C), nephrotic syndrome (D), and AKI (E). Abbreviations: AAV: ANCA-associated vasculitis; AIN: acute interstitial nephritis; ATN: acute tubular necrosis; CIN: chronic interstitial nephritis; CreGN: crescentic glomerulonephritis; DN: diabetic nephropathy; EnPGN: endocapillary proliferative glomerulonephritis; FSGS: focal segmental glomerulosclerosis; HBV-GN: HBV-related glomerulonephritis; HSPN: Henoch-Schonlein purpura nephritis; IgAN: IgA nephropathy; iMN: idiopathic membranous nephropathy; LN: lupus nephritis; MCD: minimal change disease; MPGN: membrane proliferative glomerulonephritis; MsPGN: non-IgA mesangioproliferative glomerulonephritis.
Distribution of Histopathological Patterns of Elderly Patients with SGD
For patients with SGD, the leading cause in the elderly was AAV, accounting for 43.95% (n = 69), followed by HBV-GN and amyloidosis, accounting for 24.20% (n = 38) and 14.01% (n = 22), respectively. The frequencies of lupus nephritis and Henoch-Schonlein purpura nephritis were 5.10% (n = 8) and 2.55% (n = 4), respectively. Only 2 cases of diabetic nephropathy were observed (1.27%) (Figure 3B).
Distribution of Histopathological Patterns of Elderly Patients with TIN
As shown in Figure 3C, the most common histopathological pattern of TIN was the AIN, accounting for more than half of the patients (n = 18, 64.29%). ATN and CIN were equally frequent and identified in 17.85% (n = 5) of the cases, respectively.
Distribution of Renal Histopathology Pattern in Different Indications of Renal Biopsy
Nephrotic syndrome was the most frequent indication of renal biopsy in the elderly. As shown in Figure 3D, in patients biopsied for nephrotic syndrome, iMN was the leading histopathology pattern (n = 128, 50%), followed by HBV-GN (n = 41, 16.02%), MCD (n = 20, 7.81%), and amyloidosis (n = 20, 7.81%). These four diseases made up almost 80% of all biopsies presenting as the nephrotic syndrome.
AKI was the second frequent indication for renal biopsy in the elderly. As shown in Figure 3E, the leading histopathology pattern was AAV (n = 40, 47.62%), followed by AIN (n = 17, 20.24%) and ATN (n = 7, 8.33%).
Clinical and Pathological Correlation in Patients with Common Renal Diseases
The clinical presentation before renal biopsy was further analyzed for the elderly patients with iMN and AAV (shown in Figure 4A). For patients with iMN, 89.5% (n = 128) of them presented as nephrotic syndrome, 8.39% (n = 12) presented as CGN and only 1.4% (n = 2) with AKI. For patients with AAV, 60.6% (n = 40) of patients presented as AKI, 27.27% (n = 18) presented as CGN and 9.09% (n = 6) with nephrotic syndrome.
FIGURE 4.
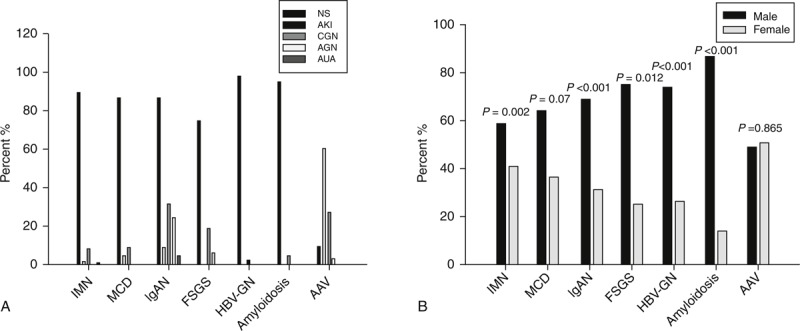
The clinicopathologic correlates (A) and gender distribution (B) of the common kidney diseases in the elderly. Abbreviations: AAV: ANCA-associated vasculitis; FSGS: focal segmental glomerulosclerosis; HBV-GN: HBV-related glomerulonephritis; IgAN: IgA nephropathy; iMN: idiopathic membranous nephropathy; MCD: minimal change disease.
Gender Distribution of Patients with Different Histopathologies
It was male predominant in elderly patients who underwent renal biopsy. As shown in Figure 4B, male predominance was demonstrated in patients with IMN (P = 0.002), IgAN (P < 0.001), FSGS (P = 0.012), HBV-GN (P < 0.001), and renal amyloidosis (P < 0.001).
DISCUSSION
To the best of our knowledge, there is little data about the distribution pattern of biopsy-proven kidney diseases in the elderly from China. In the current study, we analyzed the clinical and pathological data of 6049 cases receiving renal biopsies from 2003 to 2012 in one of the largest renal centers in China, in which the elderly constituted more than one fifteenth. In this large Chinese cohort, we found that nephrotic syndrome and AKI were the most common indication for performing the renal biopsy in the elderly in China; iMN was the leading cause in patients with nephrotic syndrome and AAV was the leading cause of AKI; the most common pathology pattern in PGDs was iMN and in SGDs was AAV. We report a relatively large number of elderly patients from a single center in China and the results have a great clinical significance in practice.
There were some characteristics of renal histopathology spectrum in Chinese elderly, as compared with reports from other countries16 (see Table 1). In our series, male is predominant, especially in those with iMN, IgAN, and HBV-GN. These results were partially in line with some other studies,11,20,21 while other studies reported that there is a slight female predominance or almost equal number of male and female patients in the very elderly patients (over 80 years old).6,14 The reason for the gender differences in the two groups may be largely attributed to their greater life expectancy in very elderly women.
TABLE 1.
Renal Histopathology Spectrum in the Elderly from Various Published Studies

Our previous study reported that IgAN was the most common form of glomerulonephritis in adult Chinese with PGDs.19 However, in the elderly patients with PGDs, iMN was the most common pathological diagnosis, which accounted for 61.02% of patients, followed by IgAN and MCD. These were consistent with some other studies.3,11–15,17
Diabetic nephropathy is the leading cause of the SGD and ESRD in western countries.32 However, the frequency of diabetic nephropathy was only 1.27% of SGDs in our study, which was quite different from that of the western countries. The major reason for this discrepancy may be explained by the indication of renal biopsy for patients with diabetic nephropathy. We usually do not perform a renal biopsy for patients with diabetic nephropathy except for those with a suspected combined glomerular disease or those with another glomerular disease on the background of diabetic mellitus.32 The second reason might be due to the lower prevalence, compared with western countries, of diabetic nephropathy in Chinese patients with ESRD, although significantly increasing recently.19 In our study, the most common cause of SGDs in the elderly was AAV, followed by HBV-GN and amyloidosis. AAV represented 43.95% of patients with SGDs; this indicated that autoimmune renal disease is still a major cause of SGDs in Chinese elderly. In our previous studies, we demonstrated that Chinese patients with AAV were mainly myeloperoxidase-ANCA associated microscopic polyangiitis, which mainly affects elderly.22 The second common renal pathology pattern was HBV-GN, which reflects the consequence of HBV infection in Chinese population in the past, and this indicates that chronic infection-induced renal disease is still a challenge for Chinese nephrologists.
In combination of primary and SGDs, nephrotic syndrome (with an overall frequency of 59.53%) was the most common indication for renal biopsy in the elderly patients in our study. IMN was the most common renal histopathology pattern, followed by HBV-GN and amyloidosis. In the literature, most studies in the elderly patients (age over 65 years) showed that iMN was the most common histopathological diagnosis, followed by amyloidosis and MCD.8,11,20,23–26 The reasons for this difference may be due to racial and regional disparities. On the other hand, several studies reported relatively high frequencies of FSGS in nephrotic patients over 65 years old,25,27 while FSGS (6.78%) was only the fourth common histological pattern in our patients with nephrotic syndrome. This may be also explained by racial difference, and our previous study in adults demonstrated a lower prevalence of FSGS in Chinese patients with PGDs.19
The elderly are more vulnerable to AKI because of the changes in kidney function and anatomy with age, and other factors which function as renal stressors (eg, surgery, nephrotoxins). AKI in the elderly can also occur more often in the setting of dehydration, hypotension, renal-toxic medication usage, post-surgery, infections, contrast medium exposure, atheroembolic disease, and obstructive uropathy.28 Thus, it is important to identify possible etiology of AKI early in the elderly by any means including renal biopsy. In addition to nephrotic syndrome (59.53%), AKI was the second most frequent indication for biopsy in the elderly in our study accounting for 19.53% of all biopsies performed. This was in accordance with most other studies.6,7,20,27,29,30 However, a recent study suggests that AKI is the first indication for renal biopsy in elderly patients over 80 years.3 These differences may be due to the discrepancies of ages in these two studies.
In our study, the most common diagnosis in patients with AKI was AAV, followed with AIN and ATN. These were in accordance with other studies which reported the high frequency of AAV both in elderly patients over 60 years and 80 years old.6,14,20,30,31 AAV is very frequent in the elderly population, which is four times greater than that in the adult.32 In our study, we found a higher percentage (47.62%) of AAV in patients with AKI than that was observed in other studies.6,9 This might explain the higher prevalence of AAV in elderly patients with AKI. Tubulointerstitial injury might be partly due to drug-induced tubule-interstitial nephritis. Various medications, including non-steroidal anti-inflammatory drugs, antibiotics, chemotherapeutic medicine and herbs, are still the predominant causes of drug-induced tubule-interstitial nephritis.33 The usage of herbs is popular in China, which may explain partly the high frequency of AIN in elderly patients with AKI in our study. Our findings highlight the importance of early renal biopsy in settings on the clinical etiology of AKI in elderly patients.
There are various clinical manifestations of elderly kidney diseases, especially in nephritic syndrome and AKI. There are some limitations to diagnosis, treat and judge prognosis of the elderly kidney diseases by clinical manifestations and laboratory findings alone. Nair et al14 reported that in 40% of patients who underwent renal biopsy, the diagnosed renal condition was potentially amenable to targeted intervention. It is necessary to perform renal biopsy in nephritic syndrome and AKI, especially in elderly patients. The therapeutic schedule should be determined by the histopathology after renal biopsy. Of note, even in patients where the biopsy diagnosis does not directly modify the decision-making of treatment, the biopsy offers prognostic information and can also eliminate potentially harmful empiric therapies. Bearing in mind that performing renal biopsies in elderly patients is not associated with increased risk for complications,14,34 we believe that renal biopsy in elderly patients is a valuable diagnostic option that offers the appropriate indications and a clinical setting that maximizes the potential benefit.
Our study has several limitations. Firstly, the retrospective design restricts the amount of data that can be gathered from the medical records of patients included. Secondly, selection bias might exist since the referral patients in this study were not from the population screened for proteinuria or microscopic hematuria. Therefore, our results need to be confirmed in larger prospective cohort studies. Finally, this is an observational study with no evidence to understand the influence factor(s) for the disease spectrum. So the spectrum information should be explained with caution of bias.
In summary, nephrotic syndrome is the leading indication of renal biopsy in Chinese elderly. IMN and AAV are the most common histopathology patterns in patients with primary and SGDs, respectively. IMN is the leading cause of nephrotic syndrome and AAV is the leading cause of AKI.
Footnotes
Abbreviations: AAV = ANCAassociated vasculitis, AIN = acute interstitial nephritis, AKI = acute kidney injury, ANS = acute nephritic syndrome, ATN = acute tubular necrosis, AUA = asymptomatic urinary abnormality, CGN = chronic glomerulonephritis, CIN = chronic interstitial nephritis, CreGN = crescentic glomerulonephritis, DN = diabetic nephropathy, EnPGN = endocapillary proliferative glomerulonephritis, FSGS = focal segmental glomerulosclerosis, HBV-GN = HBVrelated glomerulonephritis, HSPN = henoch-Schonlein purpura nephritis, IgAN = IgA nephropathy, iMN = idiopathic membranous nephropathy, LN = lupus nephritis, MCD = minimal change disease, MPGN = membrane proliferative glomerulonephritis, MsPGN = non-IgAmesangioproliferative glomerulonephritis, NS = nephrotic syndrome, PGD = primary glomerular disease, SGD = secondary glomerular disease, TIN = tubulo-interstitial nephropathy.
All the authors declared no competing interests.
This work was supported by a grant of Chinese 973 project (No. 2012CB517702) and a grant from Natural Science Fund of China to the Innovation Research Group (81321064).
REFERENCES
- 1.Azarpira N, Ramzi M, Aghdaie M, et al. Interleukin-10 gene polymorphism in bone marrow transplant recipients. Exp Clin Transplant 2008; 6:74. [PubMed] [Google Scholar]
- 2.Przepiorka D, Weisdorf D, Martin P, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant 1995; 15:825. [PubMed] [Google Scholar]
- 3.Moutzouris D-A, Herlitz L, Appel GB, et al. Renal biopsy in the very elderly. Clin J Am Soc Nephrol 2009; 4:1073–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kohli HS, Jairam A, Bhat A, et al. Safety of kidney biopsy in elderly: a prospective study. Int Urol Nephrol 2006; 38:815–820. [DOI] [PubMed] [Google Scholar]
- 5.Heldal K, Hartmann A, Grootendorst DC, et al. Benefit of kidney transplantation beyond 70 years of age. Nephrol Dial Transplant 2010; 25:1680–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haas M, Spargo BH, Wit E-JC, Meehan SM. Etiologies and outcome of acute renal insufficiency in older adults: a renal biopsy study of 259 cases. Am J Kidney Dis 2000; 35:433–447. [DOI] [PubMed] [Google Scholar]
- 7.Ferro G, Dattolo P, Nigrelli S, et al. Clinical pathological correlates of renal biopsy in elderly patients. Clin Nephrol 2006; 65:243–247. [DOI] [PubMed] [Google Scholar]
- 8.Vendemia F, Gesualdo L, Schena FP, D’Amico G. Epidemiology of primary glomerulonephritis in the elderly. Report from the Italian Registry of Renal Biopsy. J Nephrol 2000; 14:340–352. [PubMed] [Google Scholar]
- 9.Shin J, Pyo H, Kwon Y, et al. Renal biopsy in elderly patients: clinicopathological correlation in 117 Korean patients. Clin Nephrol 2001; 56:19–26. [PubMed] [Google Scholar]
- 10.Davison AM, Johnston PA. Idiopathic glomerulonephritis in the elderly. Contrib Nephrol 1993; 105:38. [DOI] [PubMed] [Google Scholar]
- 11.Davison AM, Johnston P. Glomerulonephritis in the elderly. Nephrol Dial Transplant 1996; 11 suppl 9:34–37. [DOI] [PubMed] [Google Scholar]
- 12.Verde E, Quiroga B, Rivera F, López-Gómez JM. Renal biopsy in very elderly patients: data from the Spanish Registry of Glomerulonephritis. Am J Nephrol 2012; 35:230–237. [DOI] [PubMed] [Google Scholar]
- 13.Brown CM, Scheven L, O’Kelly P, et al. Renal histology in the elderly: indications and outcomes. J Nephrol 2012; 25:240. [DOI] [PubMed] [Google Scholar]
- 14.Nair R, Bell JM, Walker PD. Renal biopsy in patients aged 80 years and older. Am J Kidney Dis 2004; 44:618–626. [PubMed] [Google Scholar]
- 15.de Oliveira C, Costa R, Vieira NO, et al. Renal diseases in the elderly underwent to percutaneous biopsy of native kidneys. J Bras Nefrol 2010; 32:379–385. [PubMed] [Google Scholar]
- 16.Okpechi IG, Ayodele OE, Rayner BL, Swanepoel CR. Kidney disease in elderly South Africans. Clin Nephrol 2013; 79:269–278. [DOI] [PubMed] [Google Scholar]
- 17.Prakash J, Singh A, Saxena R. Glomerular diseases in the elderly in India. Int Urol Nephrol 2003; 35:283–288. [DOI] [PubMed] [Google Scholar]
- 18.Pinçon E, Rioux-Leclercq N, Frouget T, et al. Renal biopsies after 70 years of age: a retrospective longitudinal study from 2000 to 2007 on 150 patients in Western France. Arch Gerontol Geriatr 2010; 51:e120–e124. [DOI] [PubMed] [Google Scholar]
- 19.Zhou FD, Zhao MH, Zou WZ, et al. The changing spectrum of primary glomerular diseases within 15 years: a survey of 3331 patients in a single Chinese centre. Nephrol Dial Transplant 2009; 24:870–876. [DOI] [PubMed] [Google Scholar]
- 20.Rivera F, Lopez-Gomez JM, Perez-Garcia R. Clinicopathologic correlations of renal pathology in Spain. Kidney Int 2004; 66:898–904. [DOI] [PubMed] [Google Scholar]
- 21.Schena F. Survey of the Italian Registry of Renal Biopsies. Frequency of the renal diseases for 7 consecutive years. The Italian Group of Renal Immunopathology. Nephrol Dial Transplant 1997; 12:418–426. [DOI] [PubMed] [Google Scholar]
- 22.Chen M, Yu F, Zhang Y, Zhao MH. Antineutrophil cytoplasmic autoantibody-associated vasculitis in older patients. Medicine (Baltimore) 2008; 87:203–209. [DOI] [PubMed] [Google Scholar]
- 23.Modesto-Segonds A, Ah-Soune M, Durand D, Suc J. Renal biopsy in the elderly. Am J Nephrol 1993; 13:27–34. [DOI] [PubMed] [Google Scholar]
- 24.Cameron JS. Nephrotic syndrome in the elderly. Semin Nephrol 1996; 16:319–329. [PubMed] [Google Scholar]
- 25.Komatsuda A, Nakamoto Y, Imai H, et al. Kidney diseases among the elderly—a clinicopathological analysis of 247 elderly patients. Int Med (Tokyo, Japan) 1993; 32:377–381. [DOI] [PubMed] [Google Scholar]
- 26.Glassock RJ. Glomerular Disease in the Elderly Population. Nephrology and Geriatrics Integrated. Berlin Heidelberg: Springer; 2000. [Google Scholar]
- 27.Rychlík I, Jančová E, Tesař V, et al. The Czech registry of renal biopsies. Occurrence of renal diseases in the years. Nephrol Dial Transplant 2004; 19:3040–3049. [DOI] [PubMed] [Google Scholar]
- 28.Levison S. Renal disease in the elderly: the role of the renal biopsy. Am J Kidney Dis 1990; 16:300–306. [DOI] [PubMed] [Google Scholar]
- 29.Covic A, Schiller A, Volovat C, et al. Epidemiology of renal disease in Romania: a 10 year review of two regional renal biopsy databases. Nephrol Dial Transplant 2006; 21:419–424. [DOI] [PubMed] [Google Scholar]
- 30.Uezono S, Hara S, Sato Y, et al. Renal biopsy in elderly patients: a clinicopathological analysis. Ren Fail 2006; 28:549–555. [DOI] [PubMed] [Google Scholar]
- 31.López-Gómez JM, Rivera F. Renal biopsy findings in acute renal failure in the cohort of patients in the Spanish Registry of Glomerulonephritis. Clin J Am Soc Nephrol 2008; 3:674–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cattran DC. Glomerulonephritis in the Elderly. Nephrology and Urology in the Aged Patient. Berlin Heidelberg: Springer; 1993. [Google Scholar]
- 33.Shi Y, Su T, Qu L, et al. Evaluation of urinary biomarkers for the prognosis of drug-associated chronic tubulointerstitial nephritis. Am J Med Sci 2013; 346:283–288. [DOI] [PubMed] [Google Scholar]
- 34.Parrish AE. Complications of percutaneous renal biopsy: a review of 37 years’ experience. Clin Nephrol 1992; 38:135–141. [PubMed] [Google Scholar]


