Supplemental Digital Content is available in the text
Abstract
Patients presenting late in the course of kidney disease who require urgent initiation of dialysis have traditionally received temporary vascular catheters followed by hemodialysis. Recent changes in Medicare payment policy for dialysis in the USA incentivized the use of peritoneal dialysis (PD). Consequently, the use of more expeditious PD for late-presenting patients (urgent-start PD) has received new attention. Urgent-start PD has been shown to be safe and effective, and offers a mechanism for increasing PD utilization. However, there has been no assessment of the dialysis-related costs over the first 90 days of care.
The objective of this study was to characterize the costs associated with urgent-start PD, urgent-start hemodialysis (HD), or a dual approach (urgent-start HD followed by urgent-start PD) over the first 90 days of treatment from a provider perspective.
A survey of practitioners from 5 clinics known to use urgent-start PD was conducted to provide inputs for a cost model representing typical patients. Model inputs were obtained from the survey, literature review, and available cost data. Sensitivity analyses were also conducted.
The estimated per patient cost over the first 90 days for urgent-start PD was $16,398. Dialysis access represented 15% of total costs, dialysis services 48%, and initial hospitalization 37%. For urgent-start HD, total per patient costs were $19,352, and dialysis access accounted for 27%, dialysis services 42%, and initial hospitalization 31%. The estimated cost for dual patients was $19,400.
Urgent-start PD may offer a cost saving approach for the initiation of dialysis in eligible patients requiring an urgent-start to dialysis.
INTRODUCTION
Medicare has been the primary payer for dialysis services for patients with end-stage renal disease (ESRD) in the USA since 1973. With the number of patients requiring renal replacement therapy (RRT) growing from approximately 16,000 in 1973 to over 600,000 in 2011, Medicare's spending on RRTs has increased dramatically from $229 million in 1973 to $34 billion in 2011.1,2 To control costs, Medicare's payment policy for dialysis care has evolved from fee-for-service to a composite rate in 1983 and then to an experimental capitation for erythropoietin use in the early 1990s.1
In 2011, the Centers for Medicare & Medicaid (CMS) substantially changed the payment system to a “bundled payment” system. In this new system, the prior composite rate and separately billable intravenous drugs and additional laboratory tests became bundled into one base rate per dialysis treatment regardless of dialysis modality.3 Consequently, peritoneal dialysis (PD), which provides similar clinical outcomes at a lower cost, was incentivized relative to hemodialysis (HD). Studies have confirmed that under the bundled payment system, the operating margin for dialysis providers is higher when providing PD to patients with ESRD compared with HD and consequently the use of PD among the 1st and 2nd-year ESRD patients has grown more rapidly than HD.4–6
However, planning and preparation for dialysis remains suboptimal in the USA. In 2011, 42.1% of ESRD patients failed to see a nephrologist prior to dialysis initiation. Only 26.3% of the patients with advanced kidney disease follow up with a nephrologist more than 1 year prior to dialysis initiation.2 As a result, the majority of patients start dialysis in an unplanned “crash” scenario.
PD has not traditionally been considered for the late-referred, more urgent patient in the “crash” scenario because PD catheter placement was considered an “elective” and non-urgent procedure and by the belief that post-implantation of the PD catheter requires 14 days of healing and maturation before PD therapy could be initiated. PD, which is a home dialysis modality, also requires patient training to allow for safe transition of the therapy to the patient's home. As a result of these barriers, and ease of in-center HD initiation, patients that present late and unplanned almost uniformly receive HD with temporary central venous catheters (CVCs).2,7
A major concern with acute unplanned urgent-start hemodialysis (urgent-start HD) using CVCs is the association with greater mortality in incident patients and high rates of infectious complications.8–11 Consequently, recent quality improvement initiatives have been developed to promote utilization of urgent-start peritoneal dialysis (urgent-start PD) to avoid HD with CVCs in patients who are acceptable candidates for PD.12,13 In this approach, the PD catheter is placed expeditiously and PD therapy is initiated using special precautions to prevent complications.14 Hence, PD therapy is an option even for the late-referred, unplanned patient.
In addition, a recent study conducted by Lobbedez et al15 demonstrated that 83% of eligible patients given a choice of urgent-start HD vs urgent-start PD, chose urgent-start PD, helping reduce the use of CVC. Given the large number of unplanned start patients in the United States, urgent-start PD offers a potentially significant mechanism for increasing the use of PD, which in turn has the potential to cut costs for private payers and Medicare.
Currently, there are no studies addressing the economic implications of urgent-start PD vs. urgent-start HD from a combined (hospital and clinic) provider perspective.5,12,13,16 Additionally, the cost implications for what we term dual patients, those who receive very transient initial urgent-start HD and swiftly transition to urgent-start PD in the first 90 days of unplanned acute dialysis, are not available in the literature. This study provides cost estimates for urgent-start PD, urgent-start HD, and dual patients during the initial 90 days of dialysis.
METHODS
Structured interviews and published reports were used to populate a quantitative model to estimate resource utilization and costs from the combined provider perspective of the first 90 days of urgent-start PD, urgent-start HD, and dual patients. Dual patients are defined as those who receive two HD sessions prior to starting PD as part of their urgent-start care in the first 90 days. The study inputs were not based on analyzing patient level data, but rather on best estimates of resource use and resource costs associated with each modality from the combined providers’ perspective.
Clinical Pathway
A comprehensive clinical pathway was determined to capture steps involved in the urgent initiation of dialysis based on a review of recent relevant published literature and nephrologists’ opinion. This pathway served as the framework for assessing the costs of the first 90 days of urgent-start dialysis treatments (Figure 1).13,17 The framework outlines the current processes associated with the first 90 days of urgent-start PD, urgent-start HD, and dual strategies. The pathway includes initial hospitalization, initial and permanent access procedures, and dialysis (mix of in-center and at home depending on the modality).
FIGURE 1.
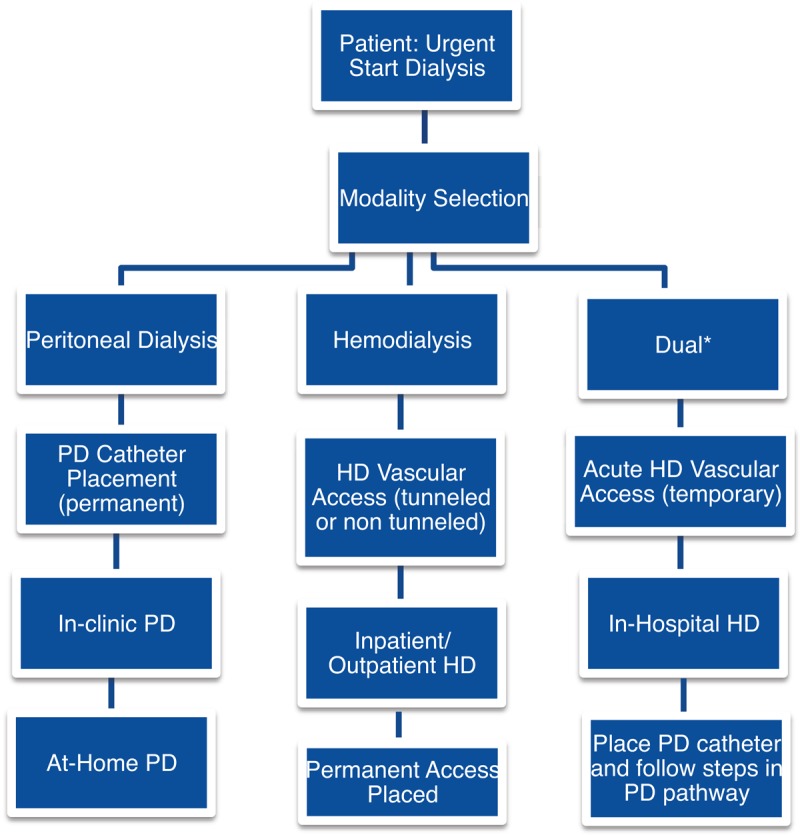
Urgent-Start Dialysis Clinical Pathway, Days 0 to 90. ∗Dual is defined as having urgent HD for 2 sessions followed by Initiation of PD.
Resource Data Collection
Based on the clinical pathway, and focusing on the combined provider perspective, a set of questions for a structured interview was developed and semi-structured interviews with staff from 5 clinics were conducted. The primary purpose of the interviews was to gather detailed information regarding the use of resources, including personnel, supplies, labs, medications, and overhead, during the first 90 days of urgent-start PD, urgent-start HD, and dual patients and to provide estimates regarding the proportions of patients receiving particular access procedures. Days 0 to 14, representing the typical urgent treatment period, were separated from days 15 to 90 in terms of estimating personnel time, laboratory tests, medications, supplies, and procedures.
The chosen sites were known to have experience in urgent-start PD and urgent-start HD. The interviews involved nephrologists and nurses at these clinics. The first two interviews were conducted in-person and used to refine the survey as well as collect initial data. Another three phone and web-based interviews were then conducted. Following the initial collection, the data were collated and examined. Missing values, items that demonstrated substantial variance, and outlier responses were identified and followed up using emails to achieve consensus values for the model. Where consensus among sites was not possible and/or where sites were unwilling or able to provide estimates, most recent literature and expert opinion (coauthors who practice nephrology) were used to best approximate the input in question.
Calculation of Costs
A spreadsheet-based cost-model was developed for a typical patient requiring urgent initiation of dialysis. The resource utilization results were combined with respective estimates of costs to complete the calculations. Costs were grouped into hospital costs, access costs, and dialysis costs. Dialysis costs were further broken into personnel, supplies, laboratory costs, medications, and facility and maintenance. The particular sources for each part of the clinical pathways are delineated below (the Appendices also provide further detail, http://links.lww.com/MD/A107). Sensitivity analyses were conducted to assess the comparative costs of the three modalities with different clinical and economic scenarios. All costs reflect 2013 dollars. When necessary, costs were inflated using an annual rate of 3.2% based on medical consumer price index information for Urban locations from the US Department of Labor between 2011 and 2013.18
Hospital Costs
Hospital costs per day reported by Kaiser Family Foundation across types of hospitals were weighted by counts of types of hospitals available from the American Hospital Association and inflated to 2013 dollars.18–20 A consensus estimate from the survey was a 3-day hospital stay for a typical patient entering into urgent-start HD and urgent-start PD and a 4-day stay for dual patients.
Access Costs
To initiate dialysis, patients require procedures to create an access to the blood for HD or to the abdominal cavity for PD. The blood devices can be temporary catheters or permanent blood vessel procedures and often several procedures are required, such as an initial temporary device to initiate therapy followed by the creation of a more permanent access point. Access costs were estimated using the geometric mean of payments calculated by CMS using Healthcare Common Procedure Coding System (HCPCS) codes and estimated frequencies of known access strategies from the survey (Laparoscopy and Percutaneous for PD catheter placement and temporary vascular catheters in the femoral vein or temporary catheters with or without Dacron cuffs—the catheter types used in common clinical practice for HD).21 The costs of permanent vascular access procedures for HD were based on native vessel arteriovenous fistula (AVF) or placement of an artificial vessel used as a graft (AVG). For urgent-start HD, all patients start dialysis with a temporary catheter and it was assumed that 90% would have permanent access (AVF or AVG) placed in the first 90 days.22 Access costs for dual patients were based on survey results for type of initial HD access followed by the same access costs used for urgent-start PD.
Personnel Costs of Dialysis Services
For personnel costs, US Bureau of Labor Statistics (BLS) data on wages, adjusted to reflect that wages, and benefits tend to reflect 70.1% of all personnel costs, by occupational category (Nurse, Dietician, Social Worker, Financial Coordinator, Clinic Manager, Technician) were used along with detailed time estimates for each occupational category from the surveys.23,24 However, the amount for a Medical Director Fee could not be found at BLS or elsewhere and was estimated based on expert opinion.
Supply Costs of Dialysis Services
Baxter Healthcare Corporation internal estimates based on average sales prices to dialysis clinics were used for the majority of supply costs (eg, PD solution, and integrated automatic PD cassettes for urgent-start PD patients; dialysates, blood sets, and dialyzers for urgent-start HD patients). Fresenius Medical Care catalogues were used for costing the use of dialysis chairs identified in the survey.25 Total supply costs were calculated based on per session costs multiplied by 39 (90 days divided by 7 days/week times 3 sessions/week), and costs of large items such as machines and water treatment systems were converted to average costs per session by annuitizing over an estimated lifetime assuming zero resale value and a 3% real discount rate and then converted to a simple average per session. Hornberger et al4 was used as a reference for the lifetime of durable supplies (eg, water treatment systems). For further detail, see Appendix (http://links.lww.com/MD/A107).
Laboratory Costs of Dialysis Services
Laboratory costs were based on detailed survey results regarding frequency of each type of lab test and corresponding costs by Current Procedure Terminology (CPT) code from the National Fee Analyzer.26
I.V. Medication Costs
CMS Drug Average Sales Price (ASP) from July 13, 2013 was used to estimate drug costs, combined with doses and frequency of use in the first 90 days for each drug (erythropoietin [EPO], iron sucrose, doxercalciferol, calcitriol, recombinant tissue plasminogen activator [r-TPA]) from the survey. However, consensus could not be reached regarding the frequency of use and dose of EPO across the centers and there was wide variance across the centers. Therefore, the dose estimate for EPO was based on 2013 USRDS (United States Renal Data System) Annual Data Report.2,27
Facility and Maintenance Costs
Facility and maintenance costs, deemed to be proprietary by all of the clinics, were taken from the recent study of resource use in PD and HD conducted by Hornberger et al4 combined with time estimates from the survey of 2 weeks in center for PD followed by 2.5 months at home and 3 months in center for HD.
Sensitivity Analyses
Sensitivity analyses were conducted to assess the potential impact on costs of various potential clinical strategies, adverse events, and potential variation in supply costs. These included changing the days of hospitalizations for PD and HD, the type of PD and HD catheter placement and reducing nurse time in PD by 20% to simulate potential efficiencies from improvements in training.9,28,29 Further, the analysis examined the impact of both increasing and decreasing the costs of supplies by 20% and lowering the dose of EPO for PD and HD by 30% to reflect potential changes since the implementation of the CMS prospective payment system in 2011. In addition, published rates, as well as consensus best and worst case scenarios were used to examine the impact of infections as well as infection and non-infection related catheter replacement rates.6,28,30 Cost information for infections were from the Healthcare Cost and Utilization Project.29
RESULTS
The clinics reported seeing a total of 376 incident dialysis patients over a 1-year period, and 218 were unplanned. Among the unplanned patients, 95 were initiated using urgent-start PD, 26 using dual, and 97 with urgent-start HD.
Base Case Costs
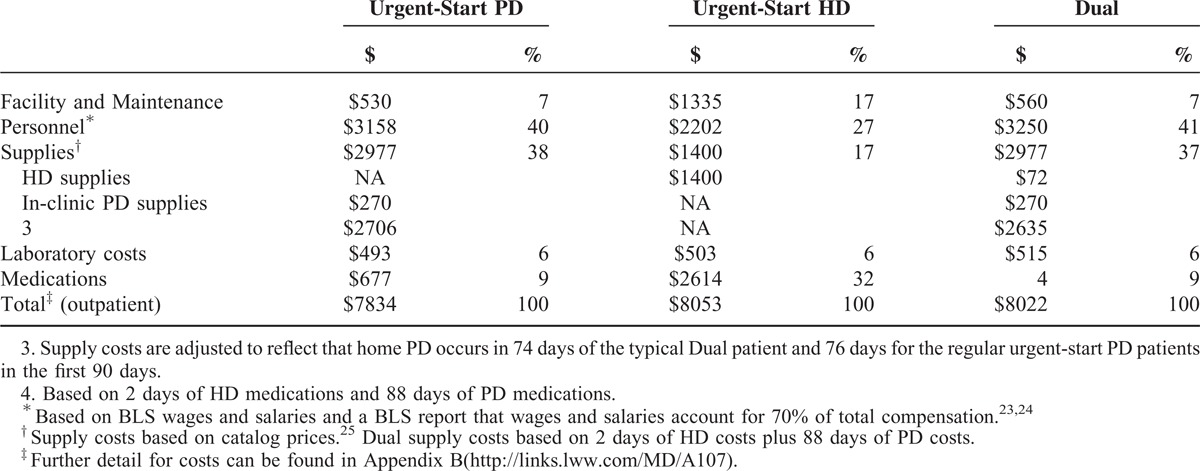
Table 1 shows total estimated costs by category across the modalities from the combined provider perspective. The estimated per patient costs over 90 days for urgent-start PD, urgent-start HD, and dual patients were $16,398, $19,352, and $19,400, respectively. The cost of dialysis services, including facility and maintenance, personnel, supplies, laboratory, and medication-related costs accounted for a substantial portion of costs in all modalities. Compared to urgent-start HD, there were significant savings in costs for urgent-start PD, which arose from differences in the expected costs of dialysis access. Table 2 provides further details for the costs of dialysis services. Overall, the costs of providing dialysis services through urgent-start PD and urgent-start HD were similar for the first 90 days. However, the supply costs and personnel (especially nurse time) are higher for urgent-start PD, while the EPO and facility costs were higher for urgent-start HD vs. urgent-start PD.
TABLE 1.
Costs Across Dialysis Modalities for Days 0 to 90
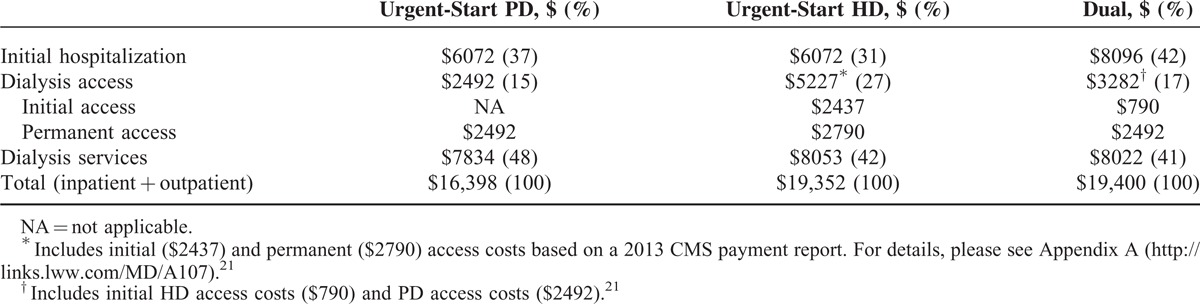
TABLE 2.
Detailed Cost Estimates of Dialysis Services Across Modalities for the First 90 Days
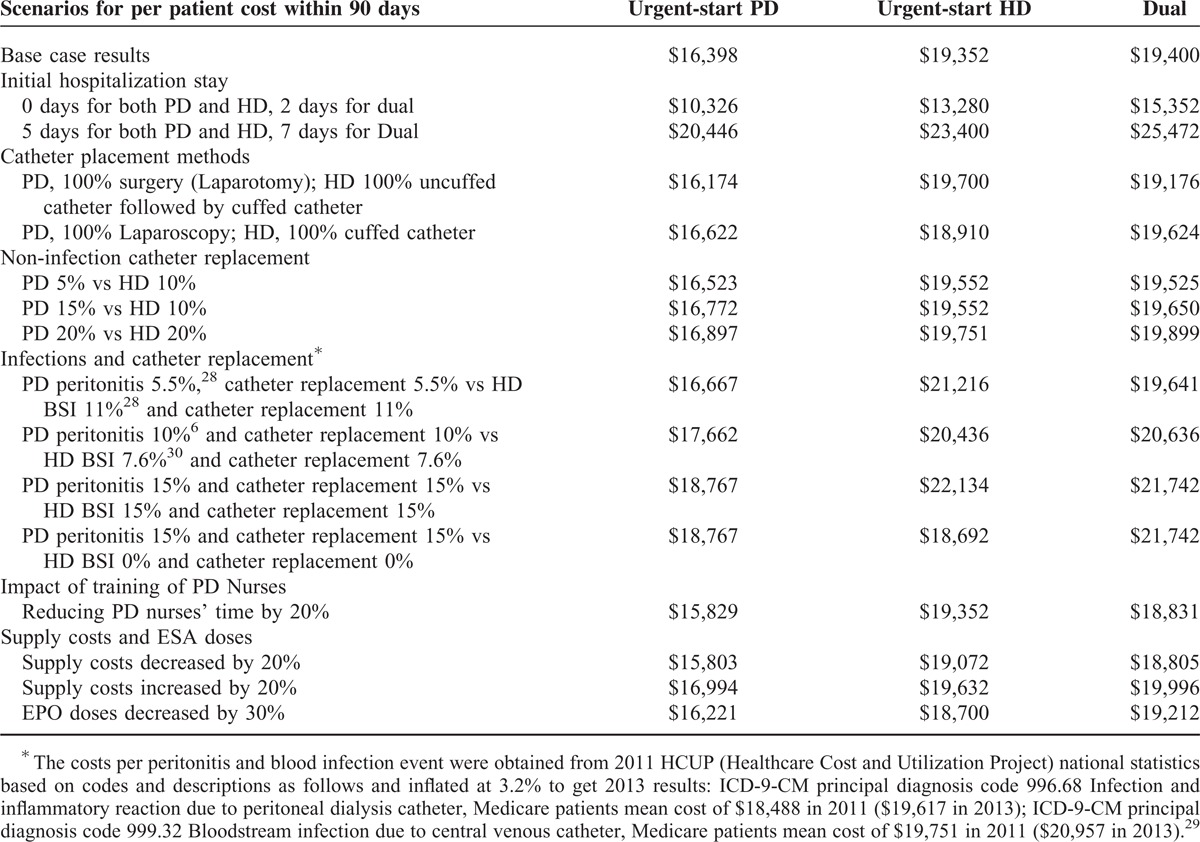
Results From the Sensitivity Analyses
Table 3 shows results from sensitivity analyses on total costs across the 3 modalities. Across the scenarios, the cost of urgent-start PD varies from $10,326 to $20,446, urgent-start HD from $13,280 to $23,400, and dual from $15,352 to $27,496, with lower costs associated with urgent-start PD in all but one scenario. The length of initial hospitalization and the rates of infections had the highest impact on costs. Within scenarios, the savings from urgent-start PD relative to urgent-start HD for a patient up to 90 days of treatment varies from −$75 in the worst case of high PD-associated infections and an idealized scenario of no dialysis associated infections for HD to $4,549 in which case the infection rates and catheter replacement rates for urgent-start PD were half of those for urgent-start HD (5.5% vs 11%).
TABLE 3.
Sensitivity Analyses
DISCUSSION
Dialysis treatments for patients with ESRD continue to impose a substantial financial burden to Medicare and Accountable Care Organizations (ACOs) covering dialysis treatments. In the USA, yearly costs of PD therapy are significantly less than in-center HD, while providing similar clinical outcomes. The most recent USRDS report suggests around $16,000 annual cost savings for patients on PD as compared to HD.2 In an attempt to generate cost savings, the changes in dialysis reimbursement instituted by CMS in 2011, as part of the bundled payment system, provide incentives to increase PD utilization.
Historically, however, initiation of PD, as compared to HD, was considered more labor-intensive, requiring patient training, elective pre-emptive surgery for catheter placement, and time to allow for catheter insertion site healing. Thus, initiation of PD was typically limited to patients presenting in an elective, non-urgent manner. Unfortunately, most patients initiating dialysis in the USA start late in the course of their disease or have unexpected kidney deteriorations requiring dialysis in an urgent manner. As a result, the utilization of PD in the USA has remained low as compared to many other industrialized countries.2
A reintroduced clinical pathway, termed urgent-start PD, has recently received increased attention.12,13,31 For patients presenting late in the course of their kidney disease, urgent-start PD has been shown to be safe and feasible and offers a mechanism for increasing the use of PD without compromising patient outcomes.12,32
While differences in long-term costs between PD and in-center HD are known, this study provides the first economic analyses comparing urgent-start PD, urgent-start HD, and a dual approach over the first 90 days after dialysis initiation.2,4,6,33,34 We find that urgent-start PD, and to a lesser extent the dual strategy, appears to be financially superior compared with urgent-start HD. These findings complement the financial incentives for increased PD utilization under the current bundled payment mechanism.3,12,13
Despite the relatively low use of PD in incident patients in the USA, the clinics participating in the survey reported that more than 50% of patients requiring urgent-start dialysis chose and received urgent-start PD, suggesting there is room for expansion of urgent-start PD. This is consistent with the findings by Lobbedez et al15 who found that among patients eligible for urgent-start PD and were given the choice of HD vs. PD, PD was chosen 83% of the time.
The current analysis provides a framework and a collection of the best available evidence to understand current urgent-start dialysis practices and the associated costs in the first 90 days of treatment. If projected to 1 year, the savings of urgent-start PD could be larger, and overall our findings provide an economic rationale for wider adoption of urgent-start PD programs. On the other hand, it has to be stressed that the survey was done using clinical providers favoring the use of PD and expansion to new centers would generally involve initial increases in start-up cost to initiate urgent-start programs. Further studies are needed to better understand the costs of establishing urgent-start PD capabilities in existing facilities, longer-term outcomes, as well as to examine variation in costs across a broader set of patient populations. For example, costs may be very different if the number of home dialysis patients is small because of inefficiencies related to staffing and infrastructure for urgent-start PD programs.
Limitations
The study is based on 5 clinics across 5 states and may not be generalizable to other settings. The sample size of the clinician interviews was small, and this study may not capture the variability in urgent-start dialysis care and practice across the USA. Nonetheless, the clinician-interview nature of the study helped depict a real-world clinical setting and was the only feasible mechanism for obtaining data of an urgent dialysis clinical pathway at this point. Furthermore, clinical experts were involved in study design, questionnaire development, clinician interviews, and resource utilization parameters assessments during analysis.
There were instances of missing data despite clinician interviews and follow up with each site, often due to the proprietary nature of some cost information. Typically there were existing published sources to provide estimates when direct information was not available. However, expert nephrology opinion by the physician authors was also occasionally required. Also, most of the supply costs for both PD and HD were based on information from Baxter and those would likely vary across suppliers. There are similar limitations to the lab and medication costs where costs may be different across settings and different drugs and/or lab tests may be used in other settings than were used in the 5 clinics surveyed here. Nonetheless, given the robustness of the results in the sensitivity analysis, it is doubtful that any changes related to strategies for filling in missing data in the surveys or to changes in cost sources that were consistent across the modalities would alter the main findings. (See the Appendices for more detailed descriptions of data sources for all the inputs, http://links.lww.com/MD/A107.)
The results are not based on patient level data and as such the survey involved asking clinicians to focus on characterizing a typical patient to be able to obtain precise measures of resource utilization and costs. In a real-world clinical setting for dialysis, it is unlikely that patients would meet all of the inherent assumptions in characterizing a typical patient. Hence, while the interview nature of the study depicts a real life setting, the costs may not reflect average costs overall. For example, the model uses an assumption of 90% of AV grafts or fistula being performed in the first 90 days for urgent-start HD patients. In actuality, this number may be lower which would delay graft costs and lower the costs of urgent-start HD in the first 90 days directly but may also be associated with more catheter complications and associated costs. This is also an example where there was not enough evidence in the literature to conduct a meaningful sensitivity analysis.
Further, in applying the results more generally, it would be important to consider selection bias or channeling bias in that severe patients are likely channeled to urgent HD due to the ability to be on HD within an hour while urgent PD may still require the use of HD temporarily. The findings for dual patients are less subject to selection bias; however, the downstream costs of dual modal patients may be higher than average PD costs. Further there could be implications of urgent-start PD in overall cost estimates beyond 90 days. It is beyond the scope of this model to estimate the magnitude of these potential biases.
CONCLUSION
Initiation of dialysis is a costly medical intervention, especially in patients who present late in the course of their disease or have an unexpected deterioration in underlying kidney function that prevents the more elective transition to dialysis. The study demonstrated that for a typical patient undergoing urgent-start PD, there is likely to be lower costs to hospitals and clinics during the first 90 days of dialysis compared to a patient initiating dialysis with urgent-start HD. The main cost savings come from lower costs associated with peritoneal access establishment. There may also be savings (or expenses) through differences in costs associated with infectious complications, as shown in our sensitivity analysis. The results suggest that urgent-start PD is likely to generate significant cost savings in most clinical presentations if applied to a substantial number of patients. The findings of this research should help inform policy makers to better understand the economic impact of PD vs HD in the acute, unplanned setting. Together with uncompromised clinical outcomes of these programs, urgent-start PD may be a preferable treatment modality for a substantial portion of patients requiring dialysis in the acute, unplanned setting.
Acknowledgments
Baxter Healthcare Corporation provided support for this project. Frank Xiaoqing Liu and Steven Guest are employees of Baxter Healthcare Corporation. Harman Dhatt, Beth Lesher, Xin Gao, and Surrey Walton were paid as consultants by Baxter. The other authors received no funding for this project.
Footnotes
Abbreviations: ACO = Accountable Care Organization, ASP = Average Sales Price, AVF = arteriovenous fistula, AVG = arteriovenous graft, BLS = Bureau of Labor Statistics, CMS = Centers for Medicare & Medicaid, CPT = Current Procedure Terminology, CVC = central venous catheter, EPO = erythropoietin, ESRD = end-stage renal disease, HCPCS = Healthcare Common Procedure Coding System, HCUP = Healthcare Cost and Utilization Project, HD = hemodialysis, ICD-9-CM = International Classification of Diseases, 9th edition, Clinical Modification, PD = peritoneal dialysis, RRT = renal replacement therapy, r-TPA = recombinant tissue plasminogen activator, USA = United States of America, USRDS = United States Renal Data System.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Swaminathan S, Mor V, Mehrotra R, Trivedi A. Medicare's payment strategy for end-stage renal disease now embraces bundled payment and pay-for-performance to cut costs. Health Aff (Millwood) 2012; 31:2051–2058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.U.S. Renal Data System. USRDS 2013 Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States. Bethesda, MD: USRDS; 2013. [Google Scholar]
- 3.Golper TA, Guest S, Glickman JD, et al. Home dialysis in the new USA bundled payment plan: implications and impact. Perit Dial Int 2011; 31:12–16. [DOI] [PubMed] [Google Scholar]
- 4.Hornberger J, Hirth RA. Financial implications of choice of dialysis type of the revised Medicare payment system: an economic analysis. Am J Kidney Dis 2012; 60:280–287. [DOI] [PubMed] [Google Scholar]
- 5.Hirth RA, Turenne MN, Wheeler JR, et al. The initial impact of Medicare's new prospective payment system for kidney dialysis. Am J Kidney Dis 2013; 62:662–669. [DOI] [PubMed] [Google Scholar]
- 6.Liu Y, Zhang L, Lin A, et al. Impact of break-in period on the short-term outcomes of patients started on peritoneal dialysis. Perit Dial Int 2014; 34:49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oliver MJ, Verrelli M, Zacharias JM, et al. Choosing peritoneal dialysis reduces the risk of invasive access interventions. Nephrol Dial Transplant 2012; 27:810–816. [DOI] [PubMed] [Google Scholar]
- 8.Perl J, Wald R, McFarlane P, et al. Hemodialysis vascular access modifies the association between dialysis modality and survival. J Am Soc Nephrol 2011; 22:1113–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ravani P, Gillespie BW, Quinn RR, et al. Temporal risk profile for infectious and noninfectious complications of hemodialysis access. J Am Soc Nephrol 2013; 24:1668–1677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kosa SD, Lok CE. The economics of hemodialysis catheter-related infection prophylaxis. Semin Dial 2013; 26:482–493. [DOI] [PubMed] [Google Scholar]
- 11.Engemann JJ, Friedman JY, Reed SD, et al. Clinical outcomes and costs due to Staphylococcus aureus bacteremia among patients receiving long-term hemodialysis. Infect Control Hosp Epidemiol 2005; 26:534–539. [DOI] [PubMed] [Google Scholar]
- 12.Ghaffari A. Urgent-start peritoneal dialysis: a quality improvement report. Am J Kidney Dis 2012; 59:400–408. [DOI] [PubMed] [Google Scholar]
- 13.Casaretto A, Rosario R, Kotzker WR, et al. Urgent-start peritoneal dialysis: report from a U.S. private nephrology practice. Adv Perit Dial 2012; 28:102–105. [PubMed] [Google Scholar]
- 14.Mahnensmith RL. Urgent-start peritoneal dialysis: what are the problems and their solutions? Semin Dial 2014; 27:291–294. [DOI] [PubMed] [Google Scholar]
- 15.Lobbedez T, Lecouf A, Ficheux M, et al. Is rapid initiation of peritoneal dialysis feasible in unplanned dialysis patients? A single-centre experience. Nephrol Dial Transplant 2008; 23:3290–3294. [DOI] [PubMed] [Google Scholar]
- 16.Chambers JD, Weiner DE, Bliss SK, Neumann PJ. What can we learn from the U.S. expanded end-stage renal disease bundle? Health Policy 2013; 110:164–171. [DOI] [PubMed] [Google Scholar]
- 17.Ghaffari A, Kumar V, Guest S. Infrastructure requirements for an urgent-start peritoneal dialysis program. Perit Dial Int 2013; 33:611–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bureau of Labor Statistics. Medical Care Consumer Price Index All Urban Consumers. US Department of Labor: Available at: http://data.bls.gov/cgi-bin/surveymost Accessed on June 4, 2014. [Google Scholar]
- 19.American Hospital Association. Fast Facts on US Hospitals. Available at: http://www.aha.org/research/rc/stat-studies/fast-facts.shtml Accessed on June 4, 2014. [Google Scholar]
- 20.Henry J Kaiser Family Foundation. Hospital Adjusted Expenses per Inpatient Day by Ownership. Available at: http://kff.org/other/state-indicator/expenses-per-inpatient-day-by-ownership/ Accessed on June 4 2014. [Google Scholar]
- 21.Centers for Medicare Medicaid Services. CY 2013 OPPS Comparison Between Proposed Geometric Mean and Median Based Payments. Available at: http://www.cms.gov/apps/ama/license.asp?file=/ascpayment/downloads/CMS-1589-P-geometric-mean-median-based-payment-compare.zip Accessed on June 4 2014. [Google Scholar]
- 22.Gomes A, Schmidt R, Wish J. Re-envisioning Fistula First in a patient-centered culture. Clin J Am Soc Nephrol 2013; 8:1791–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Department of Labor Bureau of Labor U.S. Statistics. Occupational Employment Statistics. Available at: http://www.bls.gov/oes/home.htm Accessed on June 4, 2014. [Google Scholar]
- 24.Bureau of Labor Statistics. Economic News Release. Available at: http://www.bls.gov/news.release/ecec.nr0.htm Accessed on June 4, 2014. [Google Scholar]
- 25.Fresenius Medical Care. Fresenius Medical Care Ancillary Products Listed by Product Type. Available at: http://www.fmcna.com/fmcna/idcplg?IdcService=GET_FILE&allowInterrupt=1&RevisionSelectionMethod=LatestReleased&Rendition=Primary&dDocName=PDF_100049455 Accessed on June 4, 2014. [Google Scholar]
- 26.Ingenix OptumCoding. National Fee Analyzer. Optuminsight 2013. [Google Scholar]
- 27.Centers for Medicare Medicaid Services. 2013 ASP Drug Pricing Files, July 2013. Available at: http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Part-B-Drugs/McrPartBDrugAvgSalesPrice/2013ASPFiles.html Accessed on June 4, 2014. [Google Scholar]
- 28.Aslam N, Bernardini J, Fried L, et al. Comparison of infectious complications between incident hemodialysis and peritoneal dialysis patients. Clin J Am Soc Nephrol 2006; 1:1226–1233. [DOI] [PubMed] [Google Scholar]
- 29.HCUPnet. Healthcare Cost and Utilization Project (HCUP). 2011; Rockville, MD: Agency for Healthcare Research and Quality, Available at: http://hcupnetahrq.gov/. Accessed on June 4, 2014. [PubMed] [Google Scholar]
- 30.Xue H, Ix JH, Wang W, et al. Hemodialysis access usage patterns in the incident dialysis year and associated catheter-related complications. Am J Kidney Dis 2013; 61:123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arramreddy R, Zheng S, Saxena AB, et al. Urgent-start peritoneal dialysis: a chance for a new beginning. Am J Kidney Dis 2014; 63:390–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koch M, Kohnle M, Trapp R, et al. Comparable outcome of acute unplanned peritoneal dialysis and haemodialysis. Nephrol Dial Transplant 2012; 27:375–380. [DOI] [PubMed] [Google Scholar]
- 33.Just PM, Riella MC, Tschosik EA, et al. Economic evaluations of dialysis treatment modalities. Health Policy 2008; 86:163–180. [DOI] [PubMed] [Google Scholar]
- 34.Liu FX, Quock TP, Burkart J, et al. Economic evaluations of peritoneal dialysis and hemodialysis: 2004–2012. F1000Research 2013, 2:273 (doi:10.12688/f1000research.2-273.v1). Available at: http://f1000research.com/articles/2-273/v1 Accessed on June 4, 2014. [Google Scholar]


