Abstract
Issues regarding healthcare disparity continue to increase in connection with access to quality care for acute myocardial infarction (AMI), even though the case-fatality rate (CFR) continues to decrease.
We explored regional variation in AMI CFRs and examined whether the variation was due to disparities in access to quality medical services for AMI patients.
A dataset was constructed from the Korea National Health Insurance Claims Database to conduct a retrospective cohort study of 95,616 patients who were admitted to a hospital in Korea from 2003 to 2007 with AMI. Each patient was followed in the claims database for information about treatment after admission or death.
The procedure rate decreased as the region went “down” from Seoul to the county level, whereas the AMI CFR increased as the county level as a function of proximity to the county level (30-day AMI CFRs: Seoul, 16.4%; metropolitan areas, 16.2%, cities; 18.8%, counties, 39.4%). Even after adjusting for covariates, an identical regional variation in the odds of patients receiving treatment services and dying was identified. After adjusting for invasive and medical management variables in addition to earlier covariates, the death risk in the counties remained statistically significantly higher than in Seoul; however, the degree of the difference decreased greatly and the significant differences in metropolitan areas and cities disappeared.
Policy interventions are needed to increase access to quality AMI care in county-level local areas because regional differences in the AMI CFR are likely caused by differences in the performance of medical and invasive management among the regions of Korea. Additionally, a public education program to increase the awareness of early symptoms and the necessity of visiting the hospital early should be established as the first priority to improve the outcome of AMI patents, especially in county-level local areas.
INTRODUCTION
It is known that death and disability from acute myocardial infarction (AMI) can be decreased if quality medical services and appropriate interventions are applied rapidly, even though the onset of AMI is also associated with a relatively high case-fatality rate (CFR). In this context, Korea, the USA, and several European countries have added AMI to the list of targets to be monitored and assessed at the national level.1–4
In Korea, the prevalence of cardiocerebrovascular disease has increased recently due to the ageing of the population, the Westernization of diets, and the continuing evolution of diagnostic technologies. Related socio-economic costs are also soaring. Indeed, the incidence of AMI has increased ∼10% per year and socio-economic costs due to cardiocerebrovascular disease (∼4200 billion Korean won/year) are close to those of associated with cancer (∼5500 billion Korean won/year), more than enough to be a major burden to Korean society.4–6 Although the incidence of AMI has been increasing annually, the CFR has decreased markedly since 2000 (16.0% in 2000 → 11.4% in 2007).4 Many countries have reported similar trends.7,8 These declines in the CFR of AMI have been reported to be caused by advances in invasive treatments and medical management, such as thrombolytic therapy, and patients visiting hospitals earlier.4,9–11
However, issues regarding healthcare disparity continue to increase in connection with access to quality AMI care despite the continued decrease in the CFR.12 In this context, studies of regional variation in the AMI CFR and the causes thereof have been reported.13–15
Additionally, limited access to quality healthcare in the rural areas of Korea constitutes an important challenge, because healthcare resources are concentrated in Seoul. It has been reported that 40% of medical institutions that can provide specialized AMI care services are concentrated in Seoul, and the disproportionate differences in the medical infrastructure available in Seoul versus in local areas is the focus of growing concern.5 This regional variation in the medical infrastructure may have a direct effect on death rates due to differences in the appropriate and timely administration of medical procedures or medication. Thus, we need additional empirical evidence regarding the relationship between regional variations in the quality of treatment and health outcomes to improve the quality of care on a national basis.
This study explored regional variations in AMI CFRs and examined whether such variations may be associated with disparities among geographical regions in access to quality medical services for patients with AMI. This study included all AMI patients in Korea identified in claims database of the Korea National Health Insurance (NHI) program.
METHODS
Data Source and Study Population
Study data were collected from the Korea National Health Insurance (KNHI) Claims Database of the Health Insurance Review and Assessment Service (HIRA) for the period from 2003 to 2007. This database contains all claims data provided by the National Health Insurance (NHI) program and the Medical Aid program. The NHI program of Korea covers about 96% to 97% of the population as a compulsory social insurance scheme. The remaining 3% to 4% is protected under the Medical Aid program as public assistance for healthcare for the poor.16,17
The National Health Insurance Corporation (NHIC) is the sole healthcare insurer in Korea, established by statute and responsible for operating the KNHI program; HIRA is in charge of reviewing healthcare providers’ claims and the Ministry of Health and Welfare (MOHW) supervises the program as a whole. Its main sources of funding are contributions from the insured and government subsidies.16,18 Korea's healthcare delivery system and claims data have been described in detail in previous reports.18–20
This retrospective cohort study of new AMI patients admitted to a hospital was conducted to examine whether regional variations in AMI fatality rates may be due to disparities in access to quality medical services. In total, 97,718 patients were first diagnosed with AMI (code “I21” of the International Classification of Disease, 10th revision; ICD-10) as their primary condition from 2003 to 2007; 296 of these patients were admitted to a clinic and were excluded. Additionally, 1806 patients who were transferred to other hospitals were excluded. Finally, 95,616 patients were selected for analysis. The time of each patient's initial diagnosis was confirmed by the lack of a medical claim for AMI (ICD–10 I21) as a primary or secondary disease from December 1994, the year in which the computerized billing system was initiated, to 2002.4,19 Each patient was followed in the claims database for information about treatment after admission or death.19
This study was approved by the Institutional Review Boards of the Health Insurance Review and Assessment Service.
Study Variables
Dependent Variable: CFR
The primary outcome variables were the 1- and 30-day CFRs, defined as the proportion of AMI patients who died on the day of admission or within 30 days of follow-up after admission against the number of diagnosed cases of the disease.16,19
Independent Variable: Region (Seoul, Metropolitan Area, City, County)
The primary independent variable was region of admission. In this study, Korea's geographical location was classified into 4 regions: Seoul, as a special city, metropolitan areas, cities, and counties. The administrative divisions of Korea include 1 special city (Seoul), 6 metropolitan cities, and 9 provinces. Each province is subdivided into cities and counties. Each city has a population of at least 150,000. Each county has a population of less than 150,000.21
Covariates
Covariates consisted of demographic (age, sex, insurance type), severity, medical management, and invasive management variables. Severity variables included the presence or absence of coexisting conditions, including diabetes, hypertension, chronic obstructive pulmonary disease (COPD), chronic liver disease, chronic renal disease, cerebrovascular disease, anemia, and cancer, and the presence or absence of complications. Complications were subdivided into mechanical and arrhythmic complications. Mechanical complications, primarily referring to left ventricular dysfunction, included congestive heart failure, left heart failure, cardiomegaly, acquired cardiac septal defects, and cardiogenic shock. Arrhythmic complications (ie, electrical instability) included cardiac dysrhythmias, atrioventricular blocks, and other conduction disorders.16,19,22 We assumed the presence or absence of complications based on whether the admission claim for each case included specific diseases, because we could not identify the onset of complications due to lack of information.
To assess whether regional differences in the CFRs of AMI inpatients were associated with differences in the rates of invasive or medical management, we investigated the procedures performed within 30 days after admission.19 Medical management variables included aspirin, thrombolytic drugs (tissue plasminogen activator (t-PA), urokinase, streptokinase, limaprost, and tenecteplase), β-blockers, and cholesterol-lowering drugs (statins, fibrates). Invasive management variables were coronary angiography (CAG), cardiac catheterization, percutaneous coronary intervention (PCI), and coronary artery bypass graft (CABG).9,19,22 These medical or invasive management variables were the principal variables that affected the CFR of AMI patients.9,19,22
Statistical Analysis
We performed χ2 tests and analyses of variance (ANOVA) to evaluate differences in demographic characteristics and severity among AMI patients admitted in the 4 region types. Differences in the rates of performing medical or invasive management and in the AMI CFRs by region were evaluated using a multiple logistic regression model. To compare the performance rates, we adjusted for age, sex, insurance type (National Health Insurance, Medical Aid), presence or absence of coexisting conditions, and presence or absence of complications. Additionally, for the CFRs, medical or invasive management variables were added to the covariates.
RESULTS
Characteristics of the Patients
Of the 95,616 AMI patients, the largest numbers were treated in cities (n = 38,909; 40.7%), followed by 34.8% in metropolitan areas (n = 33,270), 20.5% in Seoul (n = 19,612), and 4.0% in counties (n = 3825).
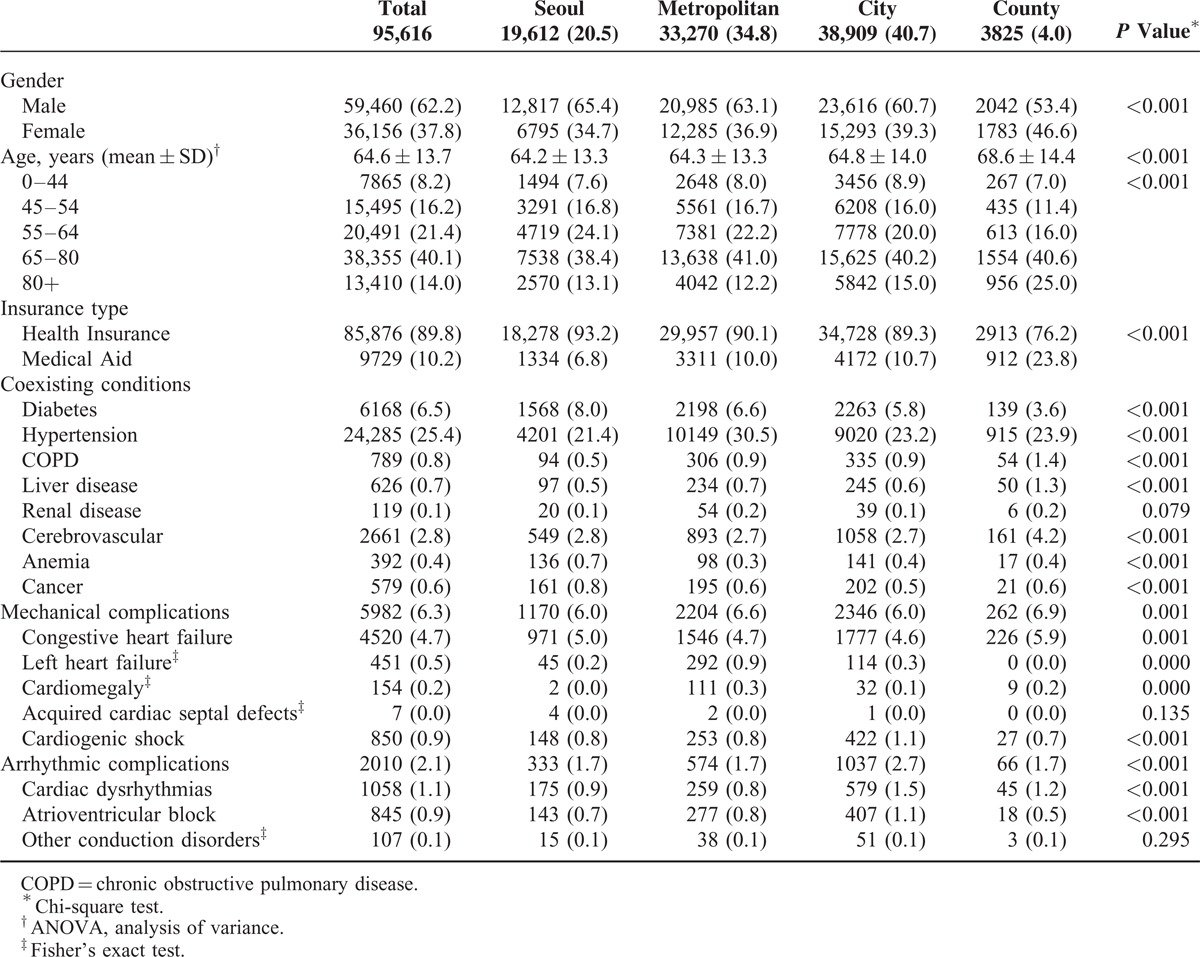
In terms of the study population's characteristics by region, counties showed higher proportions of females, seniors aged 80 or older, and Medical Aid beneficiaries, compared with other regions (Table 1). Seoul and metropolitan areas had higher proportions of patients with diabetes, hypertension, anemia, and cancer, whereas counties had higher proportions of patients with COPD, liver disease, and cerebrovascular disease as coexisting conditions versus other regions. Whereas mechanical complications were more frequent in the patients from counties, arrhythmic complications were more common in those in cities (Table 1).
TABLE 1.
Characteristics of Study Subjects by Region
Invasive and Medical Management
The rate of performing invasive management was 59.6% for CAG, 11.7% for cardiac catheterization, 48.0% for PCI, and 2.2% for CABG (Table 2). The rates varied among regions; the rate decreased as the region went “down” from Seoul to the counties. In particular, the rates in counties (CAG: 21.1%, cardiac catheterization: 5.8%, PCI: 17.0%, CABG: 0.3%) were considerably lower than those in other regions. Even after adjusting for sex, age, insurance type, coexisting conditions, and complications, the odds of patients receiving invasive management was lower in counties than in other regions (total invasive management: Seoul, odds ratio (OR) = 8.46, 95% confidence interval (CI) = 7.79–9.12; metropolitan areas, OR = 6.87, 95% CI = 6.35–7.44; cities, OR = 4.87, 95% CI = 4.50–5.26; vs. counties, OR = 1.0). Comparisons according to type of invasive management (CAG, cardiac catheterization, PCI, and CABG) showed similar results.
TABLE 2.
ORs of Receiving Invasive and Medical Management in Admitted AMI Patients by Region
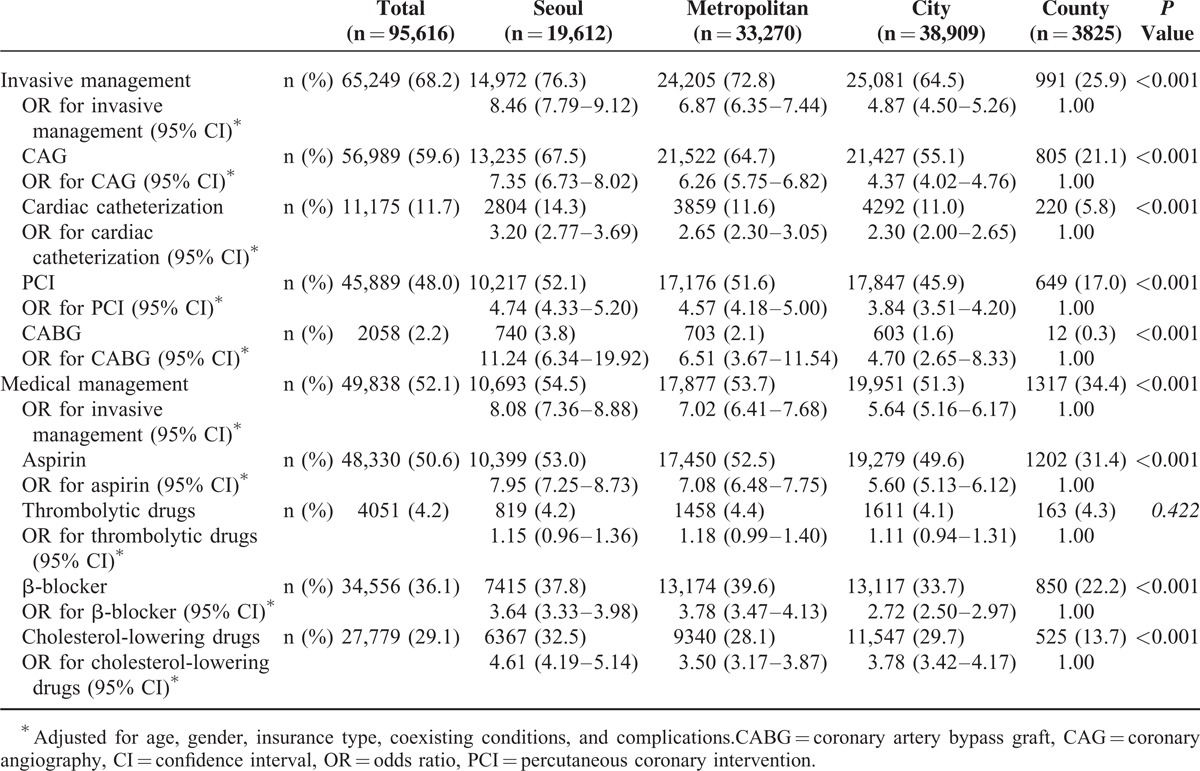
A similar trend was evident in the rates of performing medical management; the rates were lower in counties (aspirin: 31.4%, thrombolytic drugs: 4.3%, β-blockers: 22.2%, cholesterol-lowering drugs: 13.7%) than in other regions (Table 2). The odds of patients receiving medical management after adjusting for the same covariates as invasive management were lower in counties than in other regions (total medical management: Seoul, OR = 8.08, 95% CI = 7.36–8.88; metropolitan areas, OR = 7.02, 95% CI = 6.41–7.68; cities, OR = 5.64, 95% CI = 5.16–6.17; vs. counties, OR = 1.0).
Case-Fatality Rate
Of the total 95,616 AMI patients, 9814 (10.3%) died on the day of admission and 17,458 (18.3%) died within 30 days after admission (Table 3). The AMI CFRs on the day of admission and within 30 days thereafter in Seoul and metropolitan areas were lower than the mean level of all regions, whereas both rates in cities and counties were higher. In particular, in the counties, the AMI CFR reached 25.0% on the day of admission and 39.4% within 30 days thereafter. Even after adjusting for patient demographic characteristics and severity, the odds of death were higher in patients in regions other than Seoul: metropolitan areas (on the day of admission: OR = 1.18, 95% = CI 1.10–1.25; within 30 days of admission: OR = 1.07, 95% CI = 1.02–1.12), cities (on the day of admission: OR = 1.37, 95% CI = 1.29–1.46; within 30 days of admission: OR = 1.17, 95% CI = 1.11–1.22), and counties (on the day of admission: OR = 3.76, 95% CI = 3.43–4.13; within 30 days of admission: OR = 3.09, 95% CI = 2.85–3.45).
TABLE 3.
ORs of Death on the Day of Admission and Within 30 Days After Admission by Region
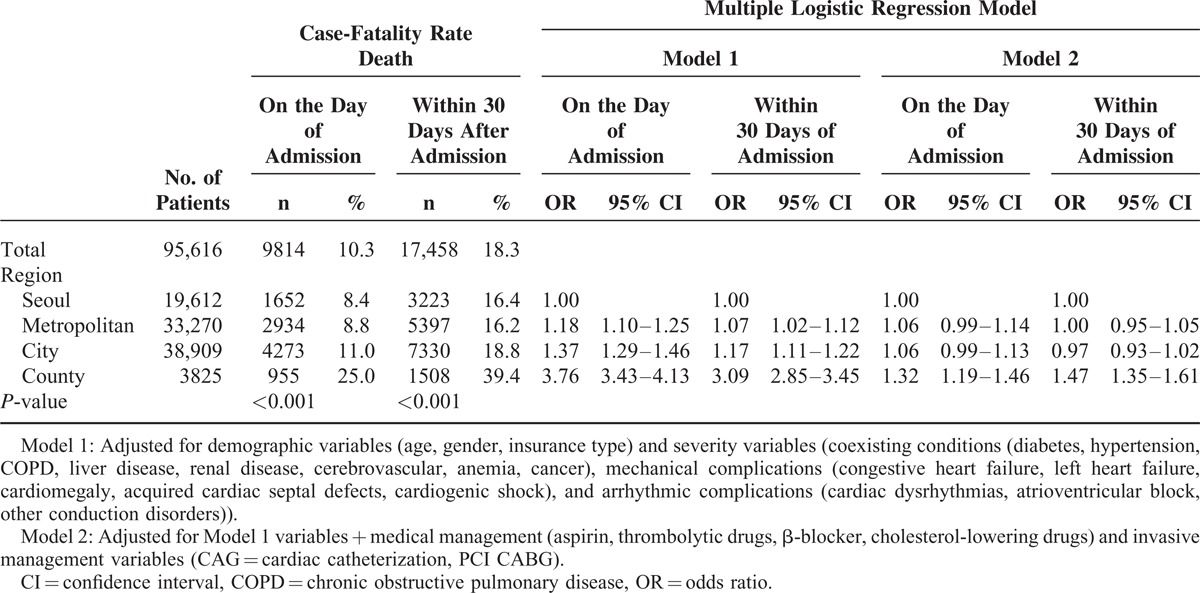
After adjusting for invasive and medical management variables in addition to the earlier covariates, the difference between Seoul and the counties was reduced. The odds of death for AMI patients in counties (on the day of admission: OR = 1.32, 95% = CI 1.19–1.46; within 30 days of admission: OR = 1.47, 95% CI = 1.35–1.61) remained statistically significantly higher than in Seoul, but the extent of the difference decreased greatly, and the significance of differences between metropolitan areas (on the day of admission: OR = 1.06, 95% = CI 0.99–1.14; within 30 days of admission: OR = 1.00, 95% CI = 0.95–1.05) and cities disappeared (on the day of admission: OR = 1.06, 95% = CI 0.99–1.13; within 30 days of admission: OR = 0.97, 95% CI = 0.93–1.02).
DISCUSSION
The Organization for Economic Cooperation and Development (OECD) reported that Korea ranked among the highest in the quality of care for AMI; noted that it seemed to follow clinical guidelines and best practices better than other OECD countries when considering good performance in process indicators, such as the administration of aspirin upon arrival at the hospital and appropriate prescriptions at the time of discharge; and showed huge increases in the volume and capacity for invasive management measures such as PCI or CABG in recent years.23 However, ∼40% of the hospitals providing healthcare services specialized for AMI are concentrated in Seoul, and the disparity between Seoul and the rest of the country in terms of healthcare system infrastructure continues to be alarming.5
Consequently, experts have suggested the existence of large regional variations in the volume and quality of care for AMI, which could lead to variation in the risk of mortality among the regions.5,23,24 Indeed, in this study, we identified significant differences among regions in terms of the CFR. Specifically, the CFR for AMI patients in Seoul was 16.4%, whereas the rate for counties was 39.4%, almost 2.4-fold higher than in Seoul (Table 3).
The sources of this variation may be explained in 2 ways: differences in patient clinical characteristics in terms of severity, and/or differences among the regions in the quality of care due to disparities in healthcare facilities and professionals specializing in AMI.15,19
This study found differences in the AMI patient clinical characteristics and the intensity of the medical interventions provided by region. Compared with other regions, counties had higher proportions of patients aged 80 years or older (counties: 25.0% vs. other regions: 13.6%; P < 0.001), females (counties: 46.6% vs. other regions: 37.4%; P < 0.001), and Medical Aid beneficiaries (counties: 23.8% vs. other regions: 9.6%; P < 0.001), who have been reported to have higher AMI mortality risks.4,25–27 Additionally, counties had higher proportions of patients with coexisting conditions, such as cerebrovascular disease (counties: 4.2% vs. other regions: 2.7%; P < 0.001) and mechanical complications (counties: 6.9% vs. other regions: 6.2%; P = 0.001) than other regions (Table 1). However, differences in the CFRs among the regions remained even after adjusting for patient demographic characteristics and severity (Table 3). Thus, these remaining differences may be due to causes other than patient clinical characteristics.
This study examined regional variations in the intensity of medical and invasive management (Table 2). Revascularization has been reported to improve the short- and long-term survival rates by decreasing the degree of myocardial necrosis and preventing hemodynamic malfunction of the ventricles.28–31 Previous studies have reported that administering aspirin promptly after a suspected AMI can reduce the risk of death and have effects that are apparent for 10 years;32–33 indeed, early β-blocker therapy in AMI patients can also reduce the case-fatality and morbidity risks.34 The American Heart Association (AHA) recommended measuring cholesterol within 24 hours of admission in a patient with AMI and reported that administering cholesterol-lowering drugs at the onset of symptoms lowered the case-fatality risk.35 In this study, the rate of performance of both invasive cardiac procedures (CAG, cardiac catheterization, PCI, CABG) and medical management (administration of aspirin, thrombolytic drugs, and cholesterol-lowering drugs) in AMI patients decreased compared with that in Seoul in metropolitan areas, cities, and counties (in that order). These differences persisted after adjusting for patient demographic characteristics and severity (Table 2). This caused us to suspect that regional variation in the AMI CFR was due to differences in the frequency of performance of those cardiac interventions among regions. To examine this, we explored regional variation in the AMI CFR after adjusting for invasive and medical management in addition to the earlier covariates. The odds of death for AMI-admitted patients in counties remained significantly higher versus in Seoul; however, the extent of the difference decreased greatly, and there were no longer significant differences among Seoul, metropolitan areas, and cities (Table 3).
To summarize, the regional variation in the AMI CFR in Korea is likely caused by differences in the frequency of the performance of medical and invasive procedures rather than being due to differences in patient characteristics and disease severity. Moreover, the difference in providing cardiac procedures seems to be, at least in part, explained by the concentration of large hospitals in Seoul and the major metropolitan areas.
In Korea, healthcare institutions are classified into 3 groups according to the number of beds they contain: “clinics” have fewer than 30 beds, “hospitals” have 30 to 99 beds, and “general hospitals” have more than 99 beds. The MOHW also differentiates “tertiary hospitals” from “general hospital” applicants on the basis of whether they meet the standards for teaching hospitals and fulfill other criteria.17,20
Of the total 44 tertiary hospitals in Korea, 17 (38.6%) are located in Seoul. Furthermore, 66.7% of AMI patients admitted in Seoul used the tertiary hospitals in Seoul, but 61.0% of county patients were hospitalized in hospitals. Thus the disparity in access to quality AMI care among the regions is difficult to ignore.
In local areas, the average fulfillment rate for critical conditions of emergency healthcare institutions (facilities, equipment, manpower) was 46.0%, lower than the national average of 58.4%.36 That is, the regional imbalance in healthcare institutions providing appropriate and prompt care for cardiovascular diseases can be thought of as the major source of the significant difference in performance of AMI treatment between urban and rural areas.23
This study had several limitations. First, we identified only whether specific cardiac procedures were implemented; we did not measure the quality of care. To reduce the CFR, it is important to assess whether the procedure was performed, but the appropriateness of the procedure performed and the quality of care are also important.15,37 The fact that the CFRs in the counties compared with Seoul remained higher after adjusting for both patient clinical characteristics and performance of invasive and medical management indicates that there is room for improvement in terms of controlling differences in quality of AMI care among regions. In this regard, further studies are needed.
Second, in this study, we did not consider the specific type of AMI. To designate type (STEMI vs. NSTEMI), it is necessary to have ICD-10 diagnosis codes consisting of at least 4 digits. However, 10.7% of the total study populations (n = 10,200) had claims with only a 3-digit code, “I21.” One possible explanation for using the 3-digit code is that the type of AMI may not have been determined at the time of diagnosis. Also, medical institutions may simply have omitted the 4th digit because use of the 3-digit code is accepted for provider reimbursement in the KNHI. Despite this coding issue, the multiple logistic regression results obtained after additional adjustment for AMI type (STEMI, ICD-10 codes I21.0, I21.1, I21.2, and I21.3, 23.0%; NSTEMI, ICD-10 code I21.4, 4.2%; unspecified, ICD-10 code I21.9, 62.1%) and exclusion of the 10,200 patients with an ICD-10 diagnosis of 121 reflected the same trend as shown in Table 3 (data not provided).16,19
Third, we did not consider distance to the healthcare facility as one of the sources of regional variations in AMI CFRs. Even if all other conditions were identical, differences in the transport time to the medical institution may have contributed to the observed regional variations. In other words, the higher AMI CFRs in counties than in Seoul may have been caused by lack of appropriate invasive or medical management or by lack of the timely administration of these services due to longer transport times. It is important to consider the time elapsed and the distance travelled before admission to a medical institution as possible contributors to regional variations in AMI CFRs in future research.
Finally, the data used this study are probably characterized by a hierarchical structure in which patients are nested in hospitals and hospitals are nested in regions. That is, patients from the same hospital may have been more closely related than were those in different hospitals. Future studies should employ a multi-level analysis to examine regional variations and their sources after controlling for the bias of this hierarchical structure.
In conclusion, we confirmed regional variations in the AMI CFRs. This is likely to have been caused by the differing frequencies of the performance of medical and invasive procedures among regions. Regional differences in the AMI CFR could be caused by differences in specialized facilities and manpower or by differences in time from the onset of AMI to arrival in hospital among regions. Benefit from revascularization is directly associated with the time taken for the restoration of perfusion to the part that has suffered ischemia; thus reducing this time as much as possible would result in the optimal outcome.31,38,39 In Korea, the proportion of patients receiving primary revascularization within 90 min of hospital arrival has been reported to be 97.7%; however, the door-to-hospital arrival time from onset of AMI was 156 min, on average.24,40 This could explain why patient outcomes, such as overall survival, hospital discharge rate, and 1-year survival rate, have not improved markedly even though the frequency of cardiac procedures provided since hospital arrival is higher than that in other OECD countries.5,23,24
Generally, given that the ageing population is increasing rapidly and access to hospitals is relatively low in rural areas versus major urban areas, a public education program to make patients aware of early symptoms and to immediately make an emergency medical call or visit a hospital early should be established as the first priority to improve the outcomes of AMI patients who reside in counties (primary prevention). Next, we need to design emergency medical center extensions and activate a cooperative network to provide appropriate AMI care within all regions (secondary prevention). In connection with the preceding preventative steps, establishing a patient registration system and designing a systematic treatment process to provide continuous rehabilitation care will also contribute substantially to improving AMI patient outcomes (tertiary prevention).
ACKNOWLEDGMENTS
The authors thank the Health Insurance Review & Assessment Service (HIRA) of Korea. This study was conducted using data from the Korean National Health Insurance Claims Database of HIRA.
Footnotes
Abbreviations: AMI = acute myocardial infarction, CABG = coronary artery bypass graft, CAG = coronary angiography, CFR = case-fatality rate, CI = confidence interval, COPD = chronic obstructive pulmonary disease, ICD-10 = the International Classification of Disease, 10th revision, NSTEMI = non-ST elevation myocardial infarction, OECD = Organization for Economic Cooperation and Development, OR = odds ratio, PCI = percutaneous coronary intervention, STEMI = ST-segment elevation myocardial infarction, t-PA = tissue plasminogen activator.
The authors have no funding and conflicts of interest to disclose.
REFERENCES
- 1.Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, et al. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation 1994; 90:583–612. [DOI] [PubMed] [Google Scholar]
- 2.Fortmann SP, Haskell WL, Williams PT, et al. Community surveillance of cardiovascular diseases in the Stanford Five-City Project. Methods and initial experience. Am J Epidemiol 1986; 123:656–669. [DOI] [PubMed] [Google Scholar]
- 3.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined: a consensus document of the Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 2000; 36:959–969. [DOI] [PubMed] [Google Scholar]
- 4.Hong JS, Kang HC, Lee SH, Kim J. Long-term trend in the incidence of acute myocardial infarction in Korea: 1997–2007. Korean Circ J 2009; 39:467–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee DH, Seo JM, Choi JH, et al. Early experience of Busan–Ulsan regional cardiocerebrovascular center project in the treatment of ST elevation myocardial infarction. Korean J Med 2013; 85:275–284.[Korean]. [Google Scholar]
- 6.Korean Ministry of Health and Welfare. The Third National Health Promotion Plan (Health Plan 2020) [Internet]. Seoul (KR): Korean Ministry of Health and Welfare, 2011. Available from: http://www.mw.go.kr/front_new/index.jsp. [Korean]. [Google Scholar]
- 7.Lundblad D, Holmgren L, Jansson JH, et al. Gender differences in trends of acute myocardial infarction events: the Northern Sweden MONICA study 1985–2004. BMC Cardiovasc Disord 2008; 8:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wellenius GA, Mittleman MA. Disparities in myocardial infarction case fatality rates among the elderly: the 20-year Medicare experience. Am Heart J 2008; 156:483–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stukel TA, Lucas FL, Wennberg DE. Long-term outcomes of regional variations in intensity of invasive vs medical management of Medicare Patients with acute myocardial infarction. JAMA 2005; 293:1329–1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosén M, Alfredsson L, Hammar N, et al. Attack rate, mortality and case fatality for acute myocardial infarction in Sweden during 1987–95. Results from the national AMI register in Sweden. J Intern Med 2000; 248:159–164. [DOI] [PubMed] [Google Scholar]
- 11.Liew R, Sulfi S, Ranjadayalan K, et al. Declining case fatality rates for acute myocardial infarction in South Asian and white patients in the past 15 years. Heart. 2006; 92:1030–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macinko JA, Starfield B. Annotated bibliography on equity in health, 1980–2001. Int J Equity Health 2002; 1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krumholz HM, Chen J, Rathore SS, et al. Regional variation in the treatment and outcomes of myocardial infarction: investigating New England's advantage. Am Heart J 2003; 146:242–249. [DOI] [PubMed] [Google Scholar]
- 14.O’Connor GT, Quinton HB, Traven ND, et al. Geographic variation in the treatment of acute myocardial infarction: the Cooperative Cardiovascular Project. JAMA 1999; 281:627–633. [DOI] [PubMed] [Google Scholar]
- 15.Ko DT, Krumholz HM, Wang Y, et al. Regional differences in process of care and outcomes for older acute myocardial infarction patients in the United States and Ontario, Canada. Circulation 2007; 115:196–203. [DOI] [PubMed] [Google Scholar]
- 16.Hong JS, Kang HC. Seasonal variation in case fatality rate in Korean patients with acute myocardial infarction using the 1997–2006 Korean National Health Insurance Claims Database. Acta Cardiol 2014; 69:513–521. [DOI] [PubMed] [Google Scholar]
- 17.National Health Insurance Corporation National Health Insurance Program of Korea. Seoul: Health Care Delivery System; 2007. [Google Scholar]
- 18.Kang HC, Hong JS. Do differences in profiling criteria bias performance measurements? Economic profiling of medical clinics under the Korea National Health Insurance program: an observational study using claims data. BMC Health Serv Res 2011; 11:189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hong JS, Kang HC, Lee SH. Comparison of case-fatality rates for acute myocardial infarction in weekday vs. weekend admissions in South Korea. Circ J 2010; 74:496–502. [DOI] [PubMed] [Google Scholar]
- 20.Kang HC, Hong JS, Park HJ. Development of peer-group-classification criteria for the comparison of cost efficiency among general hospitals under the Korean NHI program. Health Serv Res 2012; 47:1719–1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wikipedia, the free encyclopedia. South Korea. Available at: <http://en.wikipedia.org/wiki/South_Korea#Administrative_divisions>; 2014 Accessed 28.04.14. [Google Scholar]
- 22.Kostis WJ, Demissie K, Marcella SW, et al. Myocardial Infarction Data Acquisition System (MIDAS 10) Study Group. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med 2007; 356:1099–1109. [DOI] [PubMed] [Google Scholar]
- 23.Organization for Economic Cooperation and Development (OECD), Health Care Quality Review. Korea, Paris: Organization for Economic Cooperation and Development; 2012. [Google Scholar]
- 24.Jeong JO. Regional Cardiocerebrovascular Center Project in the treatment of acute myocardial infarction. Korean J Med 2013; 85:272–4.[Korean]. [Google Scholar]
- 25.Paul SD, O’Gara PT, Mahjoub ZA, et al. Geriatric patients with acute myocardial infarction: cardiac risk factors profiles, presentation, thrombolysis, coronary interventions, and prognosis. Am Heart J 1995; 131:710–715. [DOI] [PubMed] [Google Scholar]
- 26.Maynard C, Litwin PE, Martin JS, Weaver WD. Gender differences in the treatment and outcome of acute myocardial infarction. Arch Intern Med 1992; 152:972–976. [PubMed] [Google Scholar]
- 27.Fiebach NH, Viscoli CM, Horwitz RI. Differences between women and men in survival after myocardial infarction. Biology and methodology. JAMA 1990; 263:1092–1096. [PubMed] [Google Scholar]
- 28.Babaev A, Frederick PD, Pasta DJ, et al. Trends in management and outcomes of patients with acute myocardial infarction complicated by cardiogenic shock. JAMA 2005; 294:448–454. [DOI] [PubMed] [Google Scholar]
- 29.Fox KA, Poole-Wilson P, Clayton TC, et al. 5-Year outcome of an interventional strategy in non-ST-elevation acute coronary syndrome: the British Heart Foundation RITA 3 randomised trial. Lancet 2005; 366:914–920. [DOI] [PubMed] [Google Scholar]
- 30.Smith SC, Jr, Dove JT, Jacobs AK, et al. ACC/AHA guidelines for percutaneous coronary intervention (revision of the 1993 PTCA guidelines)-executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee to revise the 1993 guidelines for percutaneous transluminal coronary angioplasty) endorsed by the Society for Cardiac Angiography and Interventions. Circulation 2001; 103:3019–3041. [DOI] [PubMed] [Google Scholar]
- 31.Kim JA, Jeong JO, Ahn KT, et al. Causative factors for time delays in patients with acute st-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Korean J Med 2010; 78:586–594.[Korean]. [Google Scholar]
- 32.Meade TW, Brennan PJ, Wilkes HC, Zuhrie SR. Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. The Medical Research Council's General Practice Research, Framework. Lancet 1998; 351:233–241. [PubMed] [Google Scholar]
- 33.Baigent C, Collins R, Appleby P, et al. ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. The ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. BMJ 1998; 316:1337–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Goldstein S. Beta-blockers in hypertensive and coronary heart disease. Arch Intern Med 1996; 156:1267–1276. [PubMed] [Google Scholar]
- 35.Luepker RV, Apple FS, Christenson RH, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on Epidemiology and Prevention; AHA Statistics Committee; World Heart Federation Council on Epidemiology and Prevention; the European Society of Cardiology Working Group on Epidemiology and Prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation 2003; 108:2543–2549. [DOI] [PubMed] [Google Scholar]
- 36.Korean Ministry of Health and Welfare. Emergency Medical Facility Evaluation Report. 2011; Seoul: Korean Ministry of Health and Welfare, [Korean]. [Google Scholar]
- 37.Chan PS, Patel MR, Klein LW, et al. Appropriateness of percutaneous coronary intervention. JAMA 2011; 306:53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Steg PG, Bonnefoy E, Chabaud S, et al. Impact of time to treatment on mortality after prehospital fibrinolysis or primary angioplasty: data from the CAPTIM randomized clinical trial. Circulation 2003; 108:2851–2856. [DOI] [PubMed] [Google Scholar]
- 39.Mehta RH, Sadiq I, Goldberg RJ, et al. Effectiveness of primary percutaneous coronary intervention compared with that of thrombolytic therapy in elderly patients with acute myocardial infarction. Am Heart J 2004; 147:253–259. [DOI] [PubMed] [Google Scholar]
- 40.Health Insurance Review & Assessment Service. Acute Myocardial Infarction Quality Assessment Data 2008-2011. Seoul, Korean Health Insurance Review & Assessment Service, 2012. [Korean]. [Google Scholar]


