Abstract
The article presents the most frequent errors made in the ultrasound diagnosis of the urinary system. They usually result from improper technique of ultrasound examination or its erroneous interpretation. Such errors are frequent effects of insufficient experience of the ultrasonographer, inadequate class of the scanner, insufficient knowledge of its operation as well as of wrong preparation of patients, their constitution, severe condition and the lack of cooperation during the examination. The reasons for misinterpretations of ultrasound images of the urinary system may lie in a large polymorphism of the kidney (defects and developmental variants) and may result from improper access to the organ as well as from the presence of artefacts. Errors may also result from the lack of knowledge concerning clinical and laboratory data. Moreover, mistakes in ultrasound diagnosis of the urinary system are frequently related to the lack of knowledge of the management algorithms and diagnostic possibilities of other imaging modalities. The paper lists errors in ultrasound diagnosis of the urinary system divided into: errors resulting from improper technique of examination, artefacts caused by incorrect preparation of patients for the examination or their constitution and errors resulting from misinterpretation of ultrasound images of the kidneys (such as their number, size, fluid spaces, pathological lesions and others), ureters and urinary bladder. Each physician performing kidney or bladder ultrasound examination should possess the knowledge of the most frequent errors and their causes which might help to avoid them.
Keywords: urinary system ultrasound, kidney ultrasound examination, urinary bladder ultrasound examination, errors in ultrasound examination of the urinary system, renal pseudotumors
Abstract
W artykule omówiono najczęściej popełniane błędy w diagnostyce ultrasonograficznej układu moczowego. Zazwyczaj są one efektem nieprawidłowo wykonanego badania ultrasonograficznego lub też jego błędnej interpretacji. Z reguły wynikają z niedostatecznego doświadczenia klinicznego ultrasonografisty, klasy stosowanej aparatury ultrasonograficznej, niedostatecznej znajomości obsługi aparatu ultrasonograficznego, ale także ze złego przygotowania, konstytucji, ciężkiego stanu pacjenta oraz braku jego współpracy w trakcie wykonywania badania. Błędy w interpretacji obrazu ultrasonograficznego układu moczowego mogą mieć swoją przyczynę w dużym polimorfizmie budowy nerek (wady i odmiany rozwojowe), mogą wynikać z niewłaściwego dostępu do badanego narządu, jak również z obecności artefaktów. Błędna interpretacja badania może być także wynikiem nieznajomości danych klinicznych i laboratoryjnych. Ponadto błędy w diagnostyce ultrasonograficznej układu moczowego często wynikają z nieznajomości algorytmów postępowania i możliwości diagnostycznych innych metod obrazowania. Poniżej wymieniono błędy w diagnostyce ultrasonograficznej układu moczowego w podziale na: błędy wynikające z niewłaściwej metody badania, artefakty wynikające z niewłaściwego przygotowania pacjenta do badania lub konstytucji pacjenta oraz błędy wynikające z nieprawidłowej interpretacji obrazu ultrasonograficznego nerek (m.in. ich liczby, wielkości, przestrzeni płynowych, zmian patologicznych, inne), moczowodów i pęcherza moczowego. Każdy lekarz wykonujący badanie ultrasonograficzne nerek i pęcherza moczowego powinien posiadać wiedzę o najczęściej popełnianych błędach, przyczynach ich powstawania, co pozwoli na ich uniknięcie.
Introduction
The reasons for errors made in ultrasound diagnosis of the urinary system are usually of multifactorial nature. Generally, they result from improper technique of ultrasound (US) examination or its erroneous interpretation. Such errors are frequent effects of insufficient experience of the ultrasonographer, inadequate class of the scanner, insufficient knowledge of its operation and of wrong preparation of patients, their constitution and severe condition as well as the lack of cooperation during the examination. The reasons for misinterpretations of ultrasound images of the urinary system may lie in a large polymorphism of the kidney (defects and developmental variants) and may result from improper access to the organ as well as from the presence of artefacts.
Errors may also result from the lack of knowledge concerning clinical and laboratory data. Moreover, mistakes in ultrasound diagnosis of the urinary system are frequently related to the lack of knowledge of the management algorithms and diagnostic possibilities of other imaging modalities.
Below, the authors list errors in ultrasound diagnosis of the urinary system divided into: errors resulting from improper technique of examination, incorrect preparation of patients for the examination or their constitution and errors resulting from misinterpretations of ultrasound images.
Errors resulting from improper technique of examination(1, 2)
Insufficient quality of ultrasound equipment precludes obtaining diagnostic images and thus, involves a risk of failing to visualize pathologies, mistaking artefacts for pathologies and making differential diagnosis impossible to conduct.
Inadequate selection of the transducer, i.e. wrong type of the transducer and frequency, e.g. selecting convex probes with the frequency 2.0–5.0 MHz in examining the urinary system in children (fig. 1 A, B).
Inadequate set up selection for the examination of given organs, e.g. to examine the urinary system, one should choose the abdomen set up and to examine the kidneys, the correct choice is “kidney” set up. Inappropriate gain of the ultrasound beam and other parameters (TGC, brightness of the monitor, penetration, focus). Each time, the image should be optimized and adjusted to the conditions of the examination and constitution of the patient.
Improper lighting in the ultrasound laboratory, i.e. too bright rooms or placing the ultrasound monitor opposite the windows.
Noise which affects concentration of the ultraso nographer.
Excess tiredness of the ultrasonographer which limits logical thinking and affects image interpretation.
Artefacts and distortions caused by electric and electromagnetic devices which affect the operation of the ultrasound scanner (e.g. magnetic resonance, respirators etc.).
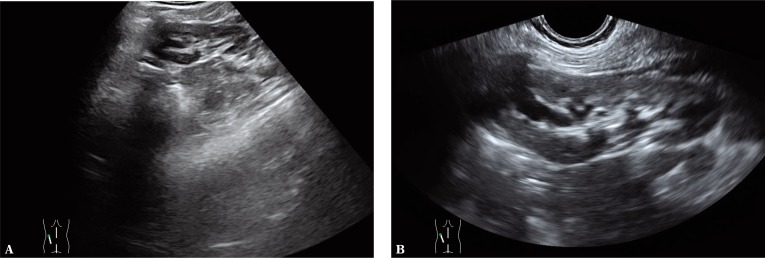
Fig. 1.
Error caused by the selection of the transducer with too low frequency in ultrasound examination of the urinary system in children. A. Examination performed with the use of a convex probe with the frequency of 2.0–6.0 MHz visualizes solely the dilatation of the upper pelvicalyceal system. B. Examination performed with a high-frequency transducer (9.0–12.0 MHz) visualizes the dilatation of the pelvicalyceal system also in the region of the middle and lower calyces and renal pelvis. Examination performed in the prone position
Errors resulting from inadequate preparation of patients for examination or from their constitution
Intestinal gas and contents cause artefacts which conceal the internal organs.
The inability to take and hold breath by the patient may considerably inhibit or preclude kidney visualization, particularly in obese patients.
- Lack of cooperation with the patient:
- children – lack of cooperation, crying, screaming, physical agitation;
- unconscious patients – lack of cooperation in terms of breathing, position and taking the patient's history.
Tenderness and pain in the abdominal cavity – impossibility to apply necessary pressure with the transducer.
Pyknic constitution – high position of the diaphragm may considerably reduce the possibility to visualize the kidneys (an attempt should be made to visualize them by intercostal access); the presence of gas in the intestine frequently produces artefacts that conceal the kidneys.
Patients with dyspnea – impossibility to draw a deep breath and frequently, inability to remain in supine position.
Open wounds in the region of the abdomen, dressings, sutures or catheters – optimal transducer application is impossible.
Empty urinary bladder – impossibility to assess the bladder and other organs of the pelvis minor.
Errors resulting from misinterpretation of ultrasound images
Errors in kidney assessment(3, 4)
Errors concerning the number of kidneys:
- Failure to visualize the kidney in its typical site:
- agenesis/aplasia – sonography does not enable the differentiation between these two pathologies;
- renal ectopia or dystopia;
- hypoplasia or aplasia – the kidney is so small or so altered that its identification is impossible for various reasons (obesity, artefacts produced by intestinal gas, kidney localization etc.).
Duplex kidney with a single ureter or completely duplicated with two ureters. In US examination, the differentiation between these two types is not feasible. The final verification is conducted on the basis of intravenous urography or computed tomography.
- Situations occurring more rarely:
- renal agenesis in neonates – the possibility to mistake enlarged adrenal glands for hypoplastic kidneys;
- tumors of the gastrointestinal tract – e.g. colon carcinoma manifests itself as a, so-called, “pseudokidney,” particularly in patients with unilateral renal agenesis;
- ectopic kidneys – possibility to mistake pelvic kidney for a tumor-like lesion;
- in extreme cases, ectopic ovaries and their “high,” abdominal localization may mimic a hypoplastic kidney;
- renal hypoplasia and dysplasia with concomitant ectopia – a particularly complex anomaly which prohibits the identification of the kidneys and inhibits their assessment;
- Errors in size assessment(5):
- errors resulting from anomalous location, structure and rotation of the kidney; this inhibits the measurement of the longest longitudinal and transverse lengths which should be measured in these planes, e.g. horseshoe kidney;
- errors resulting from the selection of improper plane for the measurements – renal measurements should be conducted after the longest longitudinal and transverse lengths have been obtained; errors may be caused by taking measurements in oblique sections;
- errors resulting from the lack of standardization of measurement sites – failure to obtain reproducible measurements; measurements of the kidneys and dilated pelvicalyceal system ought to be performed each time in the same manner;
- errors resulting from the dynamics of renal conditions, influence of an ongoing treatment as well as degree of hydration and fullness of the pelvicalyceal system, e.g. erroneous interpretation of the pelvicalyceal system filled with urine with maximally filled bladder as hydronephrosis – in such cases, one should assess the kidneys following miction;
- errors resulting from the impossibility to visualize the entire kidneys or overlapping shadows of the ribs and intestinal loops as well as faulty measurements reflecting a part of the kidney, not the entire one.
- Errors in the interpretation of fluid-filled spaces in the kidneys:
- identification of isolated dilatation of the calyceal system/systems in the case of central cysts;
- mistaking central renal cysts for dilatation of the pelvicalyceal system;
- misinterpretation of a cyst localized at the hilum as dilated renal pelvis;
- erroneous differentiation between a central cyst and aneurysm of the renal artery – Doppler mode is used for differential diagnosis;
- erroneous differentiation of the character of a cystic lesion – a complex cyst versus cystic form of renal carcinoma or solid-cystic renal carcinoma;
- erroneous interpretation of the cyst in the upper pole as an adrenal or hepatic cyst in the case of the right kidney and as a cyst in the tail of the pancreas or spleen in the case of the left kidney;
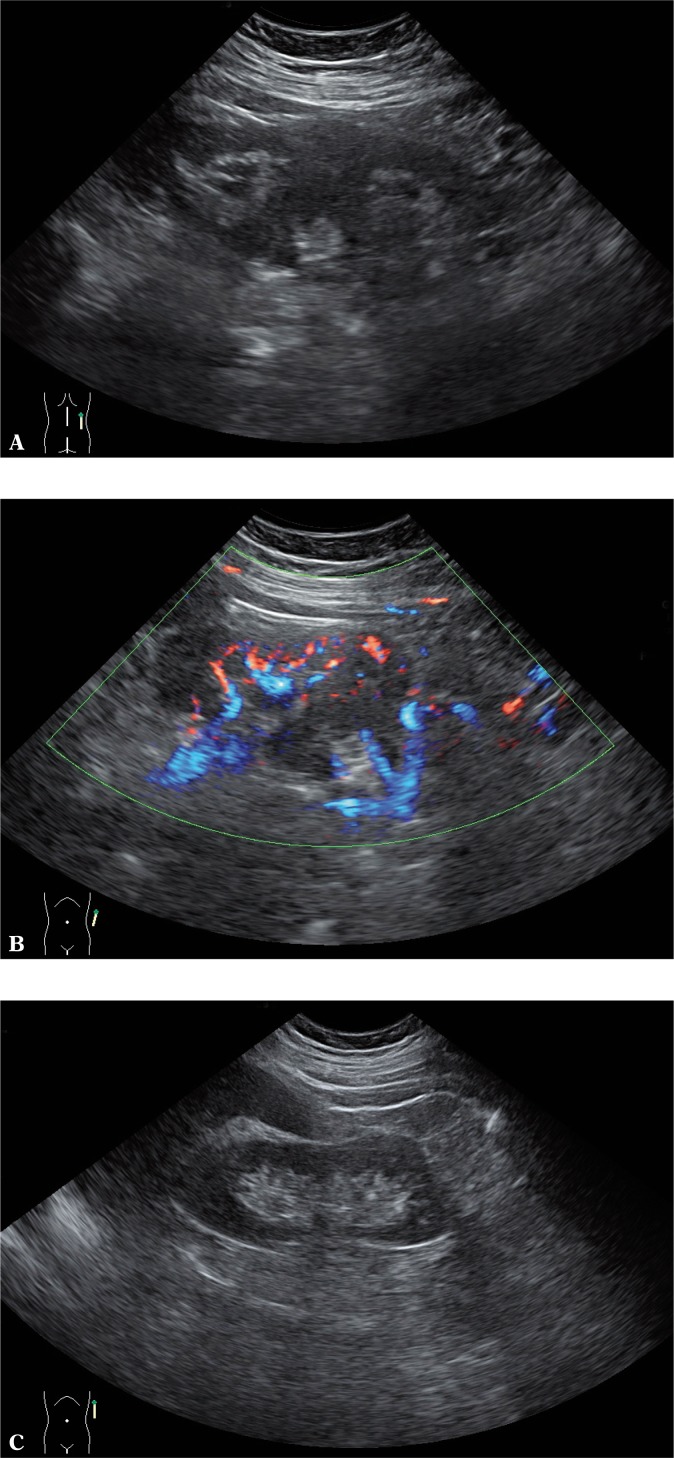
- errors in interpreting a cystic lesion with abscesslike character as a cyst without obtaining clinical information (fig. 3);
- erroneous interpretation of hypoechoic lesions, e.g. renal lymphoma (fig. 4 B), as dilatation of the pelvicalyceal system; differential diagnosis is facilitated by Doppler options.
- Errors resulting from the morphological similarity of pathological lesions to the presentation of the kidney, which is the effect of diverse renal structures depending on the patient's age, developmental defects, individual polymorphism and proliferative changes (tab. 1)(6):
- normal presentation of the kidneys in premature infants and neonates (kidneys of lobar structure with hypoechoic pyramids and hyperechoic cortex) is erroneously interpreted as lesions in the course of pyelonephritis, renal failure or renal cysts;
- renal scar (elements of the connective tissue penetrating into the parenchyma) interpreted as angiomyolipoma or postinflammatory scar;
- inflammatory tumors, postinfarction tumors and other lesions related to vascularity disorders may be erroneously interpreted as neoplastic tumors;
- renal lymphomas, leukemic infiltrations and primary proliferative lesions with echostructure and vascular pattern resembling normal renal parenchyma may be misinterpreted as a normal kidney particularly when they are small and not well-demarcated.
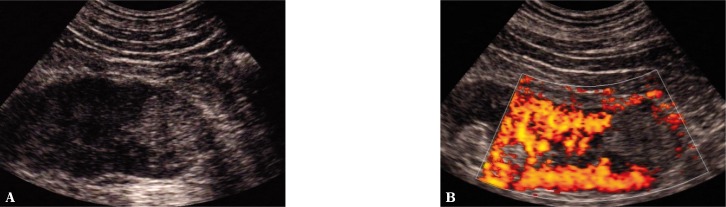
Vascular malformations (e.g. angiomas) may be misinterpreted as renal tumors (fig. 7 A, B).
- Errors resulting from ultrasound physics. The essence of ultrasound imaging is the phenomenon of ultrasound wave reflection. Making use of the reverse piezoelectric effect, the US transducers generate ultrasonic waves which are sent inside the tissues where they are reflected and return to the transducer. Depending on the presentation used by the scanner, these returning echoes are enhanced, appropriately processed and displayed. The size of the returning echo depends on multiple factors, the knowledge of which enables accurate interpretation of ultrasound images. Apart from being reflected, the ultrasonic wave also undergoes refraction, interference, scattering and absorption. In sonography, there are other equally significant factors such as: acoustic impedance of tissues, the shape of reflecting surfaces or elastic properties of tissues(7). Being familiar with all these phenomena and their influence on the displayed ultrasound image is a condition for its accurate interpretation.
- Errors in the assessment of the site after nephrectomy:
- false positive identification of neoplastic relapse caused by stool retention in the bowel loops;
- errors resulting from the presence of gas in the bowels, which precludes reliable assessment of the site after kidney removal.
Fig. 2.
A. Isthmus of the horseshoe kidney mimicking a tumor of the extraperitoneal space. 2D B-mode presentation. B. Examination performed in a different plane enables correct interpretation. 2D B-mode presentation
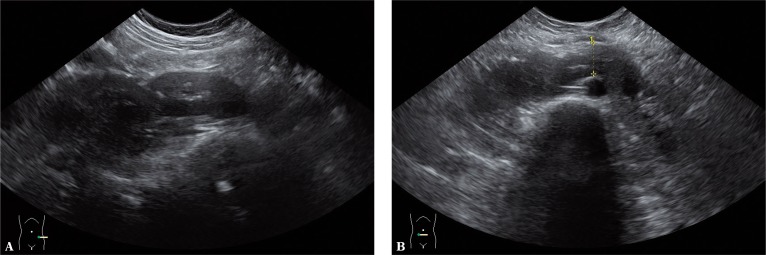
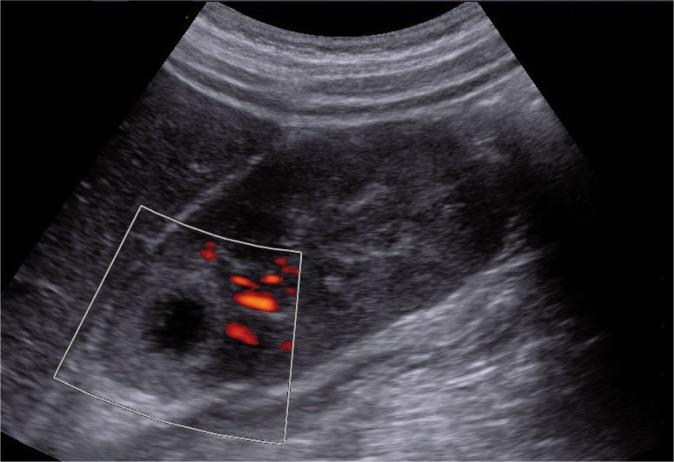
Fig. 3.
Focal lesion in the kidney with low echogenicity (abscess) mimicking a cyst. 2D power Doppler image. Abscesses with “dense” contents may also mimic renal tumors. Being familiar with clinical presentation (apart from certain clinically silent cases, such as considerable immunodeficiency) and application of Doppler options enables the differential diagnosis in these cases
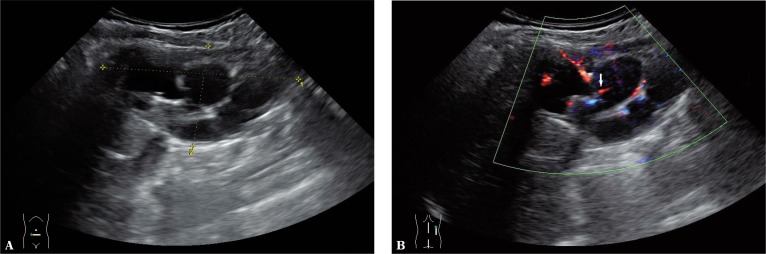
Fig. 4.
A. Hypoechoic regions (lymphoma) mimicking the dilatation of the pelvicalyceal system with concomitant dilatation of the upper pelvicalyceal system. 2D B-mode presentation. B. Doppler examination reveals vessels running into the pathological lesion (arrow). 2D B-mode presentation
Tab. 1.
Pseudotumors in the kidneys
| Developmental |
| Prominent renal pyramids and columns of Bertin |
| Persistent fetal lobulation |
| Dromedary hump of the kidney |
| Splenorenal fusion |
| Infectious |
| Abscess |
| Pyelonephritis |
| Scarred kidney |
| Granulomatous |
| Xanthogranulomatous pyelonephritis |
| Sarcoidosis |
| Malacoplakia |
| Tuberculosis |
| Vascular |
| Foci of extramedullary haematopoiesis |
| Arteriovenous malformation |
| Haematomas of the renal pelvisc |
| Subcapsular haematoma |
| Other |
| Regenerative nodule after reflux |
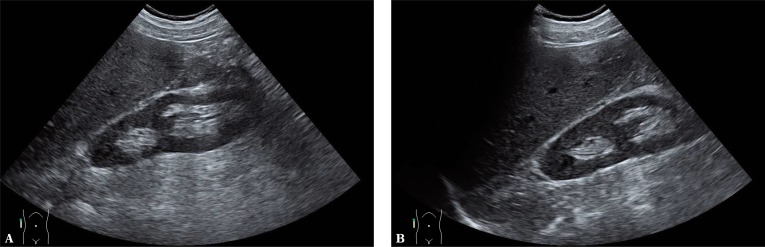
Fig. 5.
A. Dromedary hump of the left kidney mimicking a tumor. 2D B-mode presentation. B. Application of the B-flow mode reveals vascularization that is analogous to the one of the remaining renal parenchyma. C. Impression of the spleen on the left kidney causing renal hump which may be misinterpreted as a renal tumor. 2D B-mode presentation
Fig. 6.
A. Renal column mimicking a tumor. 2D B-mode presentation. B. Examination performed in the correct plane resolves diagnostic doubts. 2D B-mode presentation
Fig. 7.
A. Hyperechoic focal lesion in the kidney (angioma) mimicking a malignant tumor. 2D B-mode presentation. B. Power Doppler examination failed to show the signs of flow in the region of the lesion
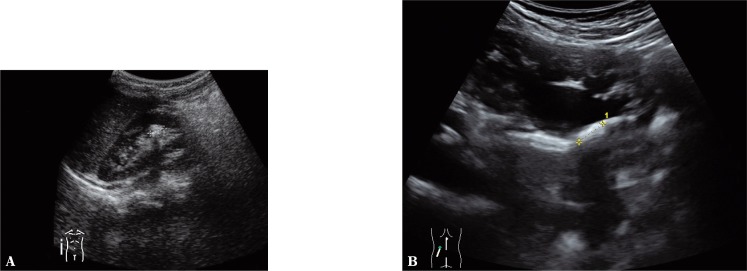
Fig. 8.
A. Hyperechoic region in the kidney (postinflammatory scar) mimicking a stone. 2D B-mode presentation. B. Hyperechoic connective tissue of the renal pelvis produces acoustic shadow and mimics a stone. 2D B-mode presentation
Errors in ureter assessment
Normal ureters are not usually visible on US examination, except for in very slim patients. Usually, it is possible to visualize the upper fragment of the ureter down to the level of the inferior pole of the kidney and perivesical portion of the ureter (intramural and retrovesical parts) provided that the urinary bladder is well filled. The visualization of the entire ureter should raise suspicions of a pathology which inhibits urine draining from the kidney. In normal conditions, the ureter has its peristaltic waves which in a natural way eliminate the possibility to trace the ureter on its entire length. Retroperitoneal fibrosis (Ormond's disease) is a disease entity which is difficult to diagnose on the basis of US examination. One of the characteristic features observed in intravenous urography or in computed tomography (CT) in the urographic phase is the medial shift of the ureters caused by inflammatory process taking place in the retroperitoneal space. The changes in the retroperitoneal space may be visible as iso- or hyperechoic focal lesions. CT and MRI are referential methods.
With respect to the comments above, in US diagnosis of the ureters the following may occur:
Errors resulting from the presence of artefacts generated by the intestinal contents and gas, e.g. mimicking concretions in the ureter.
Erroneous interpretation of the iliac vessels as dilated ureters – Doppler examination helps in differentiation.
Erroneous indication of the level of narrowing or obstruction of the ureter due to its covering by intestinal contents.
Errors resulting from diseases of the tissues adjacent to the ureter, e.g. extraperitoneal fibrosis.
Errors in the assessment of the urinary bladder
- Errors resulting from insufficiently or excessively filled bladder(8, 9):
- when the bladder is not filled sufficiently, its reliable assessment is inhibited and there is a risk of omitting proliferative changes in the wall, diverticula, vesical stones, abnormalities in the structure of the bladder neck and ureteral orifices as well as mistaking the folds of the mucous membrane of the urinary bladder for a neoplastic infiltration;
- the urinary bladder which is filled excessively or insufficiently does not allow for a reliable assessment of retained urine volume and measurement of the wall thickness; assessing the thickness of the bladder wall is a measure of subvesical obstruction and to perform it, the urinary bladder must be filled with at least 250 ml of fluid.
- Errors resulting from the impression of the bladder by the surrounding organs:
- dilated intestinal loops with the empty bladder may mimic a tumor of the bladder;
- the enlarged prostate gland indenting the urinary bladder may be erroneously interpreted as a tumor of the bladder;
- the enlarged uterine body with myomas indenting the urinary bladder may be erroneously interpreted as a tumor of the bladder;
- a tumor of the ovary indenting the urinary bladder may be erroneously interpreted as a tumor of the bladder;
- when the bladder is empty, smooth-walled ovarian cysts, embryonic cysts in the medial line of the prostate and cystic form of seminal vesicle carcinoma may be interpreted as the urinary bladder.
Conflict of interest
Authors do not report any financial or personal links with other persons or organizations, which might affect negatively the content of this publication and/or claim authorship rights to this publication.
References
- 1.American Urological Association (AUA) American Institute of Ultrasound in Medicine (AIUM): AIUM Practice Guideline for the Performance of an Ultrasound Examination in the Practice of Urology; Effective November 5, 2011 – AIUM PRACTICE GUIDELINES – Ultrasound in the Practice of Urology; Available from: www.aium.org. [Google Scholar]
- 2.ACR–AIUM–SPR–SRU Practice Guideline for the Performance of an Ultrasound Examination of the Abdomen and/or Retroperitoneum; Revised 2012 (Resolution 29). Available from: www.acr.org/guidelines. [Google Scholar]
- 3.Wieczorek P. Błędy w diagnostyce usg układu moczowego, stercza, moszny, przestrzeni pozaotrzewnowej. Ultrasonografia. 2005;5(21):29–31. [Google Scholar]
- 4.Wieczorek P. Błędy w diagnostyce usg układu moczowego, stercza, moszny i przestrzeni zaotrzewnowej. In: Jakubowski W, editor. Błędy i pomyłki w diagnostyce ultrasonograficznej. 1st ed. Warszawa – Zamość: Praktyczna Ultrasonografia, Roztoczańska Szkoła Ultrasonografii; 2005. pp. 165–184. [Google Scholar]
- 5.Bhatt S, MacLennan G, Dogra V. Renal pseudotumors. AJR Am J Roentgenol. 2007;188:1380–1387. doi: 10.2214/AJR.06.0920. [DOI] [PubMed] [Google Scholar]
- 6.Larson DB, Meyers ML, O'Hara SM. Reliability of renal length measurements made with ultrasound compared with measurements from helical CT multiplanar reformat images. AJR Am J Roentgenol. 2011;196:W592–W597. doi: 10.2214/AJR.10.5486. [DOI] [PubMed] [Google Scholar]
- 7.Nowicki A. Wstęp do ultrasonografii. Podstawy fizyczne i instrumentacja. Warszawa: Medipage; 2003. [Google Scholar]
- 8.Tyloch J. Przydatność badania ultrasonograficznego do pomiaru pojemności pęcherza moczowego i oceny ilości zalegającego moczu – porównanie dokładności kilkunastu sposobów pomiaru. Ultrasonografia. 2002;2(7):86–91. [Google Scholar]
- 9.Tyloch J. Ocena dokładności własnej metody pomiaru pojemności pęcherza moczowego i zalegania moczu u chorych z asymetrycznym, niekształtnym pęcherzem moczowym. Ultrasonografia. 2002;2(7):97–100. [Google Scholar]