Abstract
Most soft tissue mass lesions of the hand are benign. Ganglia are the commonest lesions encountered, followed by giant cell tumors of the tendon sheath. Malignant tumors are rare. Often a specific diagnosis can be achieved on imaging by considering the location and anatomical relations of the lesion within the hand or wrist, and assessing its morphology. Magnetic resonance imaging is an excellent modality for evaluating soft tissue tumors with its multiplanar capability and ability to characterize tissue. Ultrasound plays a complementary role to MRI. It is often the initial modality used for assessing masses as it is cheap and available, and allows reliable differentiation of cystic from solid lesions, along with a real time assessment of vascularity. This review describes the US appearances of the most frequently encountered soft tissue masses of the wrist and hand, correlating the findings with MRI where appropriate.
Keywords: ultrasound, magnetic resonance imaging, hand, wrist, tumor, mass, ganglion, giant cell tumor, pseudomasses
Abstract
Większość guzów tkanek miękkich ręki ma łagodny charakter. Do najczęstszych należą gangliony oraz guzy olbrzymiokomórkowe pochewki ścięgnistej. Zmiany złośliwe występują rzadko. W wielu przypadkach ustalenie rozpoznania jest możliwe w badaniach obrazowych na podstawie oceny lokalizacji i morfologii zmian oraz stosunków anatomicznych w obrębie ręki. Rezonans magnetyczny jest doskonałą metodą oceny guzów tkanek miękkich dzięki możliwości wielopłaszczyznowego obrazowania oraz określenia charakteru tkanek. Ultrasonografia stanowi uzupełnienie badania techniką rezonansu magnetycznego. Często jest badaniem pierwszego wyboru z uwagi na niższy koszt i większą dostępność w porównaniu z rezonansem magnetycznym. Pozwala na wiarygodne odróżnienie przestrzeni płynowych od zmian litych oraz na ocenę unaczynienia zmian. Niniejszy artykuł przedstawia obrazy ultrasonograficzne najczęstszych zmian guzowatych tkanek miękkich ręki w korelacji z obrazami rezonansu magnetycznego.
Introduction
Most soft tissue mass lesions of the hand (anatomically made up of the wrist, metacarpus, and fingers) have a benign etiology(1, 2). In practice, ganglion cysts are the commonest lesions encountered. Benign solid masses include giant cell tumors of the tendon sheath, lipomas, Dupuytren's contractures, nerve sheath tumors, glomus tumors, hemangioma/vascular malformations and synovial pathology. Malignant tumors such as soft tissue sarcomas are rare.
In many cases a specific diagnosis can be achieved by considering the location and anatomical relations of the lesion within the hand or wrist, its configuration and its morphology(2–5). Plain films and computed tomography (CT) may detect calcification and allow assessment of adjacent bony structures but otherwise do not offer much in the way of soft tissue characterization. Magnetic resonance imaging (MRI) is an excellent technique for evaluating soft tissue masses in the hand and wrist with its multiplanar capability and ability to characterize soft tissue components. Ultrasound (US) plays a complementary role to MRI. It is often the first imaging modality used, as it is readily available and cheap. US is extremely useful in localizing lesions and determining if the lesion is cystic or solid(6, 7). It also allows real time assessment of tumor vascularity. Furthermore US facilitates guided biopsy or aspiration of lesions.
This review describes the US appearances of the most frequently encountered soft tissue masses of the wrist and hand, correlating the findings with MRI where appropriate.
Ultrasound technique
Ideally a high frequency linear array probe (10–20 MHz) should be used to evaluate the superficial structures of the hand and wrist. A small footprint probe or hockey stick probe may be required to access certain areas such as the web space between the fingers. A jelly stand-off may be useful to improve visualization of structures, and increase the sensitivity of Doppler evaluation. Dynamic evaluation using active and passive mobilization of the fingers can help accentuate pathology and determine the nature of lesions. Furthermore, the compressibility of a lesion may allow assessment of its consistency and determine if it is cystic.
The use of extended field of view (EFOV) imaging allows for better image presentation and may improve delineation of the lesion in relation to its surrounding structures.
The use of Doppler ultrasound is integral to the evaluation of soft tissue masses(8). The lack of color flow within a hypoechoic lesion can help confirm the cystic nature of a lesion. The presence of flow within a lesion on the other hand confirms that it is solid. Vascular malformations may show slow vascular filling with compression and release.
The use of microbubble contrast agents can improve detection of low-volume blood flow in smaller vessels, thereby facilitating detection of angiogenetic vessels in inflammatory conditions or tumors(9), however this is not usually required in routine practice.
Ganglion
Ganglia are the most common cause for a palpable mass in the wrist and hand, accounting for up to 60% of cases(2). The typical patient is a young woman but any age group may be affected. The etiology of ganglia is unclear but a history of trauma is present in around 10% of patients. On histology, a ganglion has a thin connective tissue capsule but no true synovial lining. There is usually a close relationship to a joint, tendon sheath or ligament. A synovial cyst, on the other hand, represents a herniation of synovial membrane through the joint capsule and therefore has a true synovial lining and is histologically distinct from ganglia. On imaging it is often impossible to differentiate between these two entities and the terms ganglion, ganglion cyst and synovial cyst are therefore often used interchangeably.
On ultrasound simple ganglia appear as well circumscribed, thin walled, anechoic masses with posterior acoustic enhancement(10). Thin internal septations are often visible, appearing as fine linear internal echoes. They may be unilocular or multilocular, and may have a rounded or lobular appearance. The ganglion/ cyst usually lies adjacent to a joint or tendon sheath. A thin stalk may be visible, and is an important feature to describe, particularly if surgery is contemplated, as this may be the clue to the exact origin of the ganglion. On Doppler interrogation there is no internal flow. Occasionally, vessels are seen within the wall or in the surrounding soft tissues.
In one study most ganglia were found to be complex rather than simple on sonography(10). Complex ganglia are larger than simple ganglia and usually have well-defined margins, thick walls, locules, and acoustic enhancement. A collapsed or decompressed ganglion may be difficult to differentiate from an area of localized synovial thickening.
On MRI ganglia appear as unilocular or multilocular, rounded or lobular fluid signal masses adjacent to a joint or tendon sheath. Small cysts may simulate a small effusion but the diagnosis should be considered if the fluid is localized and is absent or there is a paucity of it in the remainder of the joint. Typically they are of low signal on T1-weighted images and high signal on T2-weighted images, but high proteinaceous content or hemorrhage can result in lesions appearing iso- or hyperintense on T1-weighted images. Following intravenous gadolinium mild enhancement of the capsule or of septae may be seen.
In the wrist and hand ganglia occur in four main areas(11):
Dorsum of the wrist (around 60%). These typically originate from the scapholunate joint or ligament. On imaging a small synovial stalk frequently extends through the fibers of the scapholunate ligament and dissects through overlying structures to lie superficially. If the ganglion lies deep to the extensor tendons it may not be clinically palpable and is considered an “occult ganglion” (fig. 1).
Volar aspect of the wrist (20%). These usually arise from the radioscaphoid, scaphotrapezial, pisiform-triquetral or metacarpotrapezial joint. They often extend around the flexor carpi radialis tendon and lie adjacent to radial artery, sometimes causing displacement of the vessel. Ulnar aspect ganglia are associated with tears in the triangular fibrocartilage complex (figs. 2, 3).
Flexor tendon sheath (10%). These are also referred to as volar retinacular ganglion cysts. Usually they occur at the level of the metacarpophalangeal joint involving the A1 pulley. This type of ganglion penetrates through the pulley and is tethered and therefore does not move with tendon motion (fig. 4).
Dorsal aspect of the distal interphalangeal joint, between the nail and distal interphalangeal joint (10%). Commonly referred to as “mucous cysts” these are usually associated with osteoarthritis. They may be painful and cause nail distortion, and may discharge (fig. 5).
Fig. 1.
Occult dorsal ganglion. Anechoic cyst (arrowhead) intimately related to the scapholunate ligament (arrow), lying deep to the extensor tendons. The scaphoid (S) and lunate (L) are indicated
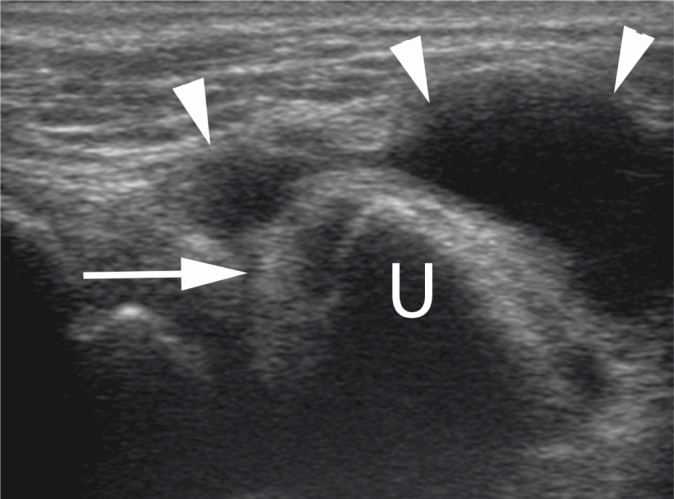
Fig. 2.
Triangular fibrocartilage (TFC) tear with ganglion. Ulnar aspect ganglion (arrowheads) arising from a tear of the TFC (arrow)
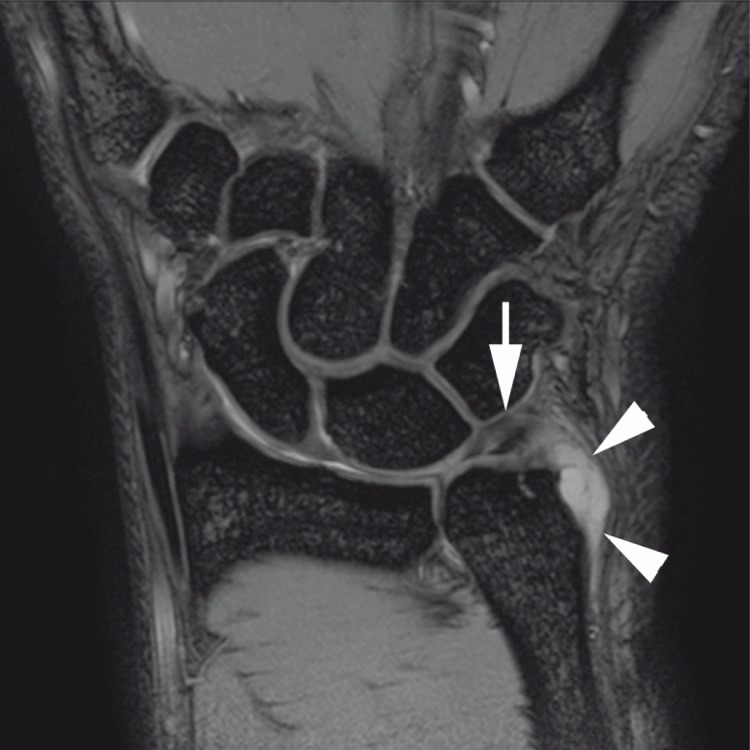
Fig. 3.
Same patient as fig. 2. Coronal gradient echo image demonstrating TFC tear (arrow) with adjacent ganglion (arrowheads)
Fig. 4.
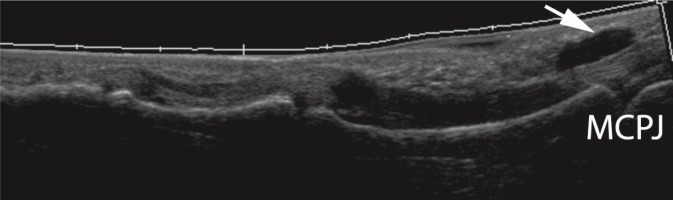
A1 pulley ganglion. Extended field of view image showing volar ganglion related to A1 pulley at the level of the metacarpophalangeal joint (MCPJ)
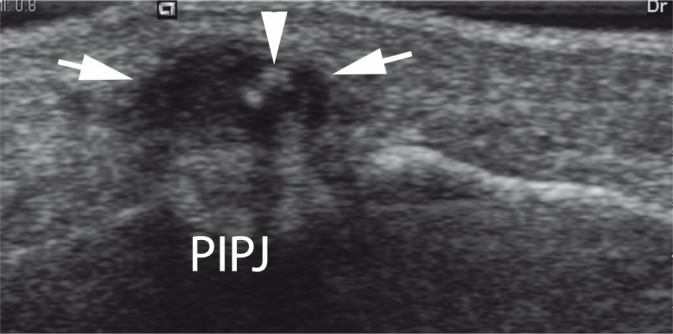
Fig. 5.
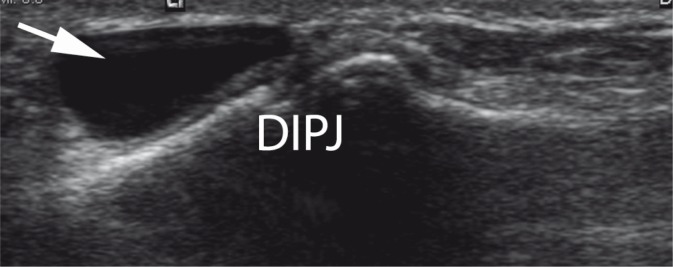
Mucous cyst. Ganglion (arrow) arising from a degenerate distal interphalangeal joint (DIPJ)
Giant cell tumor of the tendon sheath
The first description of pigmented villonodular synovitis (PVNS) was by Chassaignac in 1852, who described a nodular lesion of the synovial membrane that affected the flexor tendons of the fingers(12). The World Health Organization nomenclature describes two forms of PVNS – the giant cell tumor of the tendon sheath (GCTTS), sometimes also referred to as focal PVNS, and diffuse type giant cell tumor for the diffuse intra-articular form of PVNS. Localized disease, whether extra-articular or intra-articular, comprises 77% of cases (with the tenosynovial form being the most common), compared with diffuse intra-articular involvement, which accounts for 23% (a 3.3:1 ratio)(12).
GCTTS is the second commonest mass in the hand and wrist following ganglia. The etiology of GCTTS has been variously attributed to a synovial inflammatory process, recurrent hemorrhage, repetitive trauma or a disorder of lipid metabolism(12). However, consistent cytogenetic abnormalities and its potential for autonomous growth and malignant transformation suggest that the disease should be considered a neoplastic process. There is a slight female predominance. These lesions usually affect the volar aspect of the first three digits(13), much less commonly affecting the wrist.
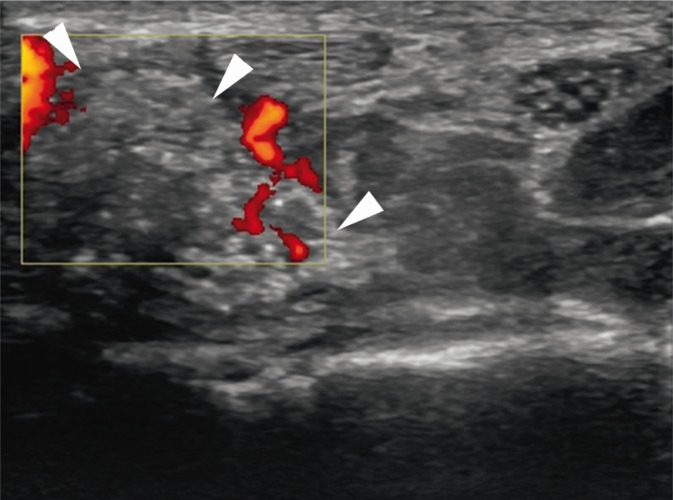
On ultrasound GCTTS appears as a hypoechoic mass, which is often lobulated, with well-demarcated margins(13). Its intimate relation to a tendon sheath or joint capsule, and its creeping extension along the length of the tendon, as well as circumferential involvement, should strongly suggest the diagnosis. On dynamic examination the GCTTS does not move with the tendon as it arises from the sheath rather than the tendon itself. On Doppler imaging there is usually increased vascularity (fig. 6).
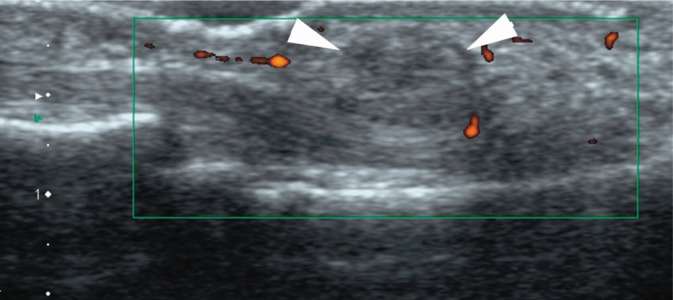
Fig. 6.
Giant cell tumors of the tendon sheath (GCTTS). Hypoechoic mass (arrowheads) intimately related to the ring finger flexor tendon sheath
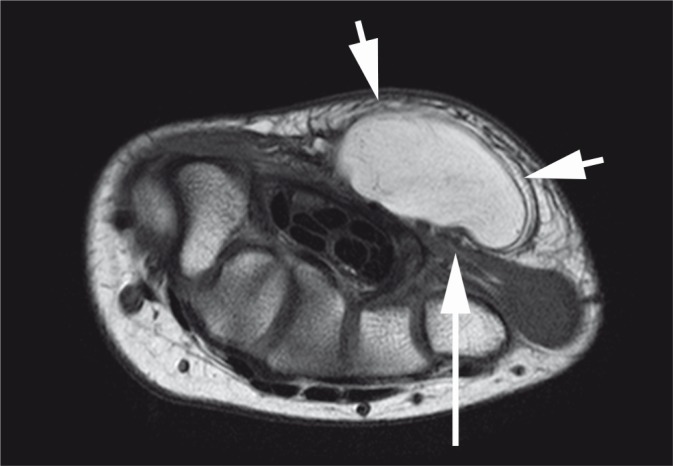
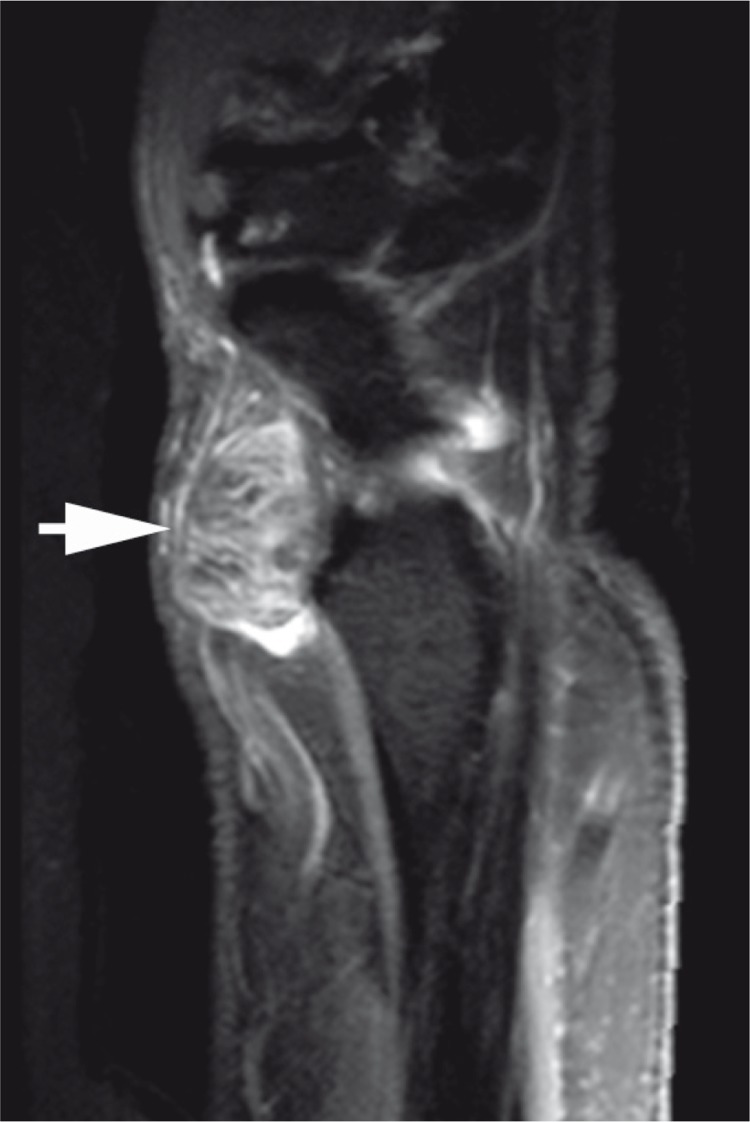
MRI also shows a well-defined mass adjacent to, or enveloping a tendon. Characteristically the lesion is hypointense on T1-weighted images, similar to skeletal muscle. On T2-weighted images there is typically low signal due to chronic hemorrhage with hemosiderin deposition (fig. 7). Blooming artefact may occur on gradient echo sequences due to hemosiderin. This feature usually allows a confident diagnosis, and MRI is therefore considered the imaging investigation of choice. Enhancement may be seen with intravenous gadolinium.
Fig. 7.
Same patient as fig. 6. Axial T2 fat-saturated image showing a low T2 signal mass (arrow) related to the ring finger flexor tendon sheath
Fibromatosis
Fibromatosis refers to a group of benign proliferative lesions comprised of myofibroblasts which can be locally aggressive. They are characterized by infiltrative growth, and are often mistaken for a malignant lesion on imaging. Superficial lesions manifest as Dupuytren's contracture, whereas deeper lesions are referred to as deep musculoaponeurotic fibromatosis. There is an association with plantar fibromatosis and Peyronie's disease.
Dupuytren's contracture
Proliferation of fibrous tissue within the palmar aponeurosis of the hand results in Dupuytren's contracture(14). The typical patient is an elderly man. Most commonly the 3rd and 4th rays are involved. Patients present with subcutaneous nodules on the palmar surface of the distal crease of the hand which progresses to cords and bands and finally the characteristic flexion contracture secondary to fibrous attachments to the underlying tendon sheath(15). On ultrasound the superficial palmar aponeurosis appears as a thin echogenic lamellar structure overlying the flexor tendons. The presence of hypoechoic bands adhering to the margin of the flexor tendons and deep surface of the dermis is characteristic of the disease. Early nodules are hypoechoic in relation to tendons and typically demonstrate increased vascularity whereas older nodules are more hyperechoic, without vascularity. Arterial encasement by fibrous or scar tissue may be seen in late disease (fig. 8).
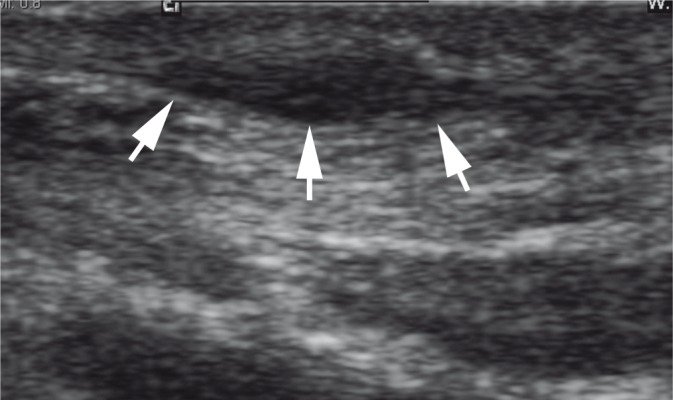
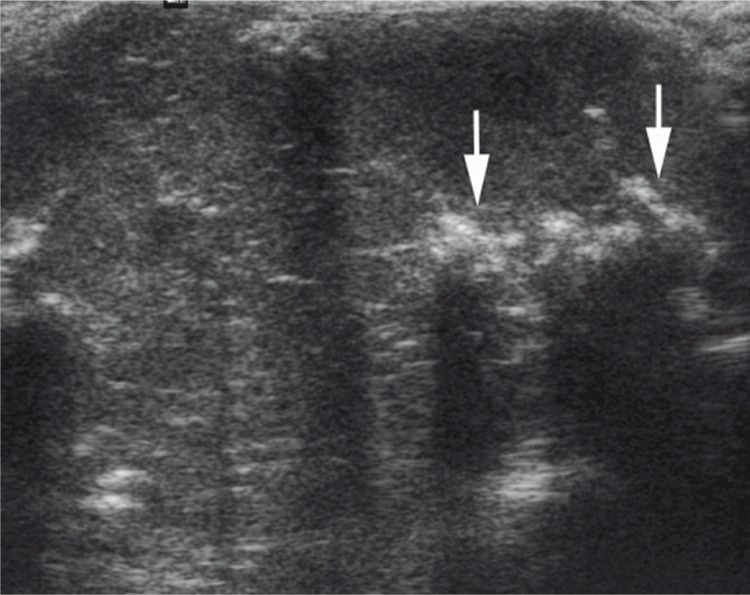
Fig. 8.
Dupuytren's contracture. Longitudinal US shows a hypoechoic nodule (arrows) arising from the superficial fascia of the palm, adjacent to the flexor tendon.
On MRI focal nodules or cords may be seen arising from the palmar aponeurosis extending distally and superficially parallel to the flexor tendons. Lesions with high cellularity are typically of higher signal on T2-weighted images than those with a large collagenous component, which tend to be low signal on T2-weighted images(14) (fig. 9).
Fig. 9.
Same patient as fig. 8. Sagittal T1-weighted image showing a low signal nodule of the superficial palmar fascia
Deep musculoaponeurotic fibromatosis
Deep musculoaponeurotic fibromatosis is rare in the hand but typically occurs between the ages of 10–40 years, with equal sex predominance. Usually the lesions are solitary. Plain films may show bone erosion. On ultrasound the lesions usually have poorly defined margins and appear infiltrative. There may be increased vascularity on Doppler. On MRI the signal characteristics can be variable depending on the degree of cellularity and collagen content(16).
Fibroma of the tendon sheath
A fibroma of the tendon sheath is a rare benign tumor, which may easily be confused with GCTTS. On ultrasound the lesion appears as a hypoechoic welldefined mass attached to the tendon sheath, often in relation to an annular pulley. The MRI appearance is variable but usually the presence of fibrous tissue results in low signal on both T1- and T2-weighted images, similar to GCTTS(17) (fig. 10).
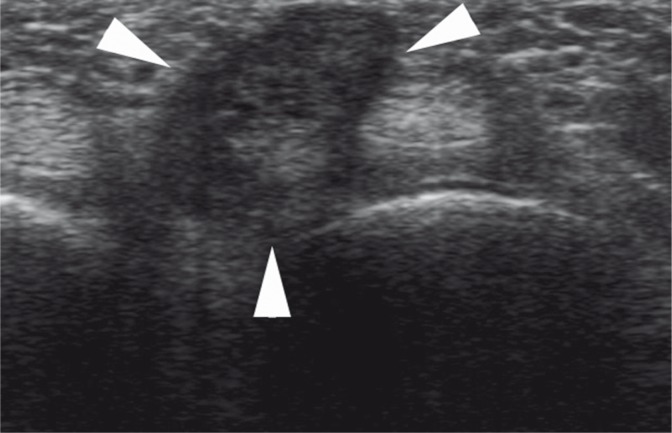
Fig. 10.
Annular pulley fibroma. Small avascular hypoechoic mass (arrowheads) arising from the A2 pulley
Lipoma
Simple benign lipomas are the commonest soft tissue tumor, but they are infrequent in the hand(18). The lesions are composed of mature adipose tissue, which may occur in a subcutaneous or deep location, presenting as a slow growing painless mass. Typically, they occur at the thenar or hypothenar eminence. The majority of lesions measure less than 5 cm(19). Compression of neighboring structures such as nerves and vessels may occur if the lipoma occurs in a confined space such as the carpal tunnel or Guyon's canal. Rarely lipomas can occur with a tendon sheath.
On ultrasound lipomas are well-demarcated lesions that are classically described as hyperechoic and homogeneous. They may however be hypoechoic or isoechoic(20). Superficial lipomas may be difficult to visualize, as they may blend in with the adjacent fat (fig. 11). On MRI they demonstrate fat signal with homogeneous high signal on T1-weighted and low signal on STIR or T2 fat-saturated images(21) (fig. 12). Septations may be seen with benign lipomas, but nodules or solid components indicate an atypical lipoma or liposarcoma. With intramuscular lipomas fatty tissue infiltrates between muscle fibers.
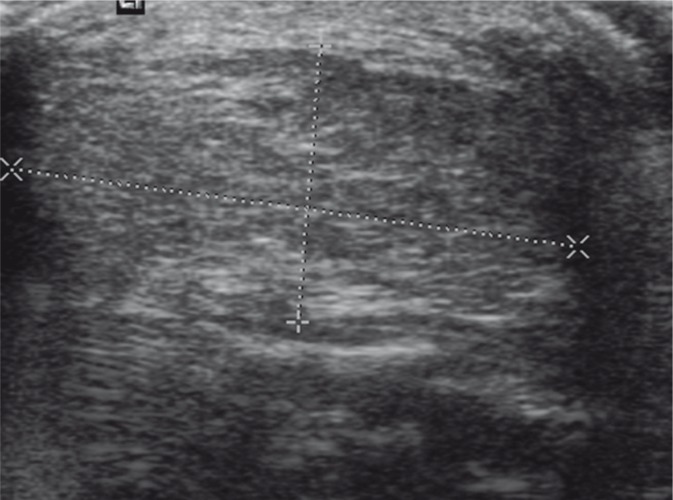
Fig. 11.
Benign lipomas. Transverse ultrasound showing an isoechoic uniform mass in the palm
Fig. 12.
Same patient as fig. 11. Axial T1-weighted image showing a well-defined homogeneous high T1-signal mass (arrows) in the palm
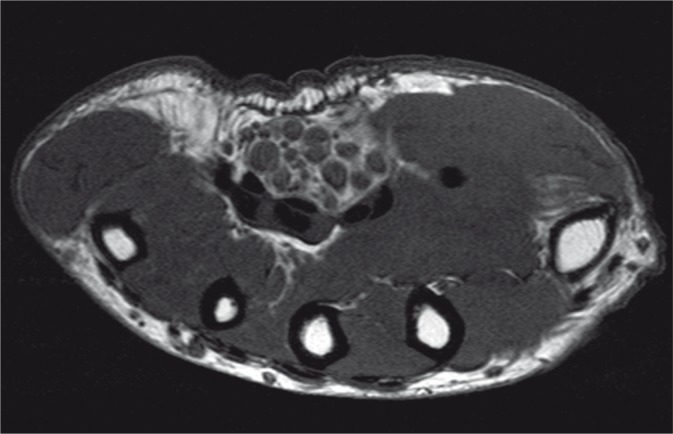
Fibrolipomatous hamartoma
A hamartoma is a benign focal malformation that resembles a neoplasm in the tissue of its origin. It is comprised of tissue elements normally found at that site, but which are growing in a disorganized mass. The fibrolipomatous hamartoma is composed of hypertrophic mature fat and fibroblasts in the epineurium(22). It typically presents in young adulthood with a slow growing mass on the volar aspect of the wrist and may be associated with macrodactyly, a condition known as macrodystrophia lipomatosa. There is a marked predilection for the median nerve with up to 85% occurring at this location. Patients may complain of pain or paresthesia. The US and MRI appearances are pathognomonic with longitudinally orientated cylindrical structures representing nerve fascicles, giving a spaghetti-like appearance on coronal planes and co-axial cable appearance on axial images(22). The fascicles are surrounded by fatty tissue. On MRI areas of low and high signal are seen on both T1- and T2-weighted images representing the fatty and fibrous contributions of the tumor (figs. 13, 14).
Fig. 13.
Fibrolipomatous hamartoma of the median nerve. Transverse ultrasound showing a coaxial cable sign, pathognomonic for this condition
Fig. 14.
Same patient as fig. 13. Axial T1-weighted image shows enlarged nerve fascicles surrounded by fat
Hemangioma/vascular malformations
According to Mulliken and Golwacki's classification of vascular anomalies, a hemangioma is a tumor characterized by increased cell turnover of endothelium, mast cells, fibroblasts and macrophages(23). Hemangiomas are usually not present at birth (although congenital hemangiomas may occur) but become apparent in the first few weeks of life as a firm non-compressible mass, after which there is a proliferative phase with rapid growth followed 6–10 months later by an involuting phase. In 70% there is resolution by 7 years and the remainder continue to diminish until the age of 12 years. On MRI, serpentine vascular flow voids may be evident on both T1 and T2 sequences and there is uniform enhancement with intravenous gadolinium. With involution there is decrease in size of the mass with replacement by variable and increasing amounts of fat, loss of the high flow signal voids and absence of enhancement.
Vascular malformations are not true neoplasms but are errors of vascular morphogenesis with a normal rate of endothelial turnover, and hence grow commensurately with the child(23). Occasionally they can suddenly enlarge due to hemorrhage, infection or hormonal influence at puberty. They are present at birth although they may not become apparent until adolescence or early adulthood.
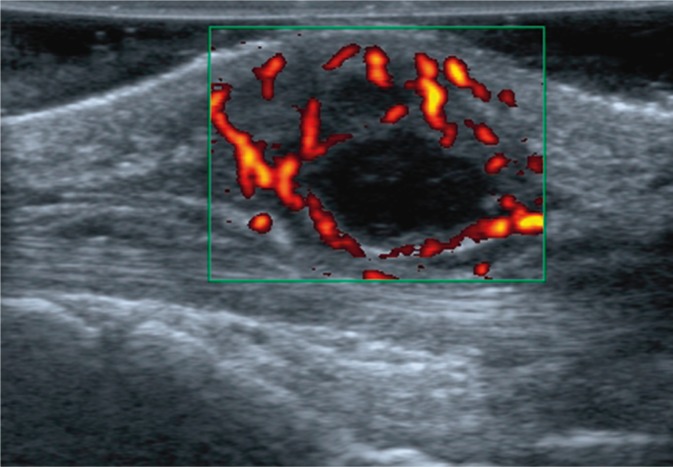
The lesions can be subdivided according to vessel type into the following groups: capillary, venous, arterial and lymphatic. On US, these lesions have a variable appearance, but often are well-defined, compressible, solid, echogenic or hypoechoic masses with cystic serpiginous areas representing dilated vessels. Broadly speaking lesions can be subdivided into low flow (capillary, venous, lymphatic or a combination) or high flow (arteriovenous)(24).
Capillary malformations are the equivalent of the port wine stain, and usually occur superficially. A clinical diagnosis may be made in most instances. On imaging skin thickening is seen with no demonstrable vascular channels.
Venous malformations are simple malformations comprised of dilated slow flowing vascular spaces and channels forming a venous network, with no solid tissue component apart from septations. On ultrasound venous malformations appear as hypoechoic or heterogeneous lesions in 80% of cases. Anechoic channels can be visualized in less than 50% of cases. Sometimes, thickening of the subcutaneous tissues without a solid mass or discernible vascular channels is the only feature. Hyperechoic foci may be present indicating the presence of phleboliths. Doppler US demonstrates monophasic, low-velocity flow. In 20% of lesions, no flow is demonstrated (figs. 15–17). They appear on MRI as septated high signal soft tissue masses on T2-weighted images with no evidence of high flow velocity signal voids. On T1-weighted images they are isointense to muscle. The presence of phleboliths results in foci of signal void. Gradient echo imaging is useful to document slow flow and exclude the presence of any high flow. With contrast, there is uniform or inhomogeneous enhancement of the vascular spaces.
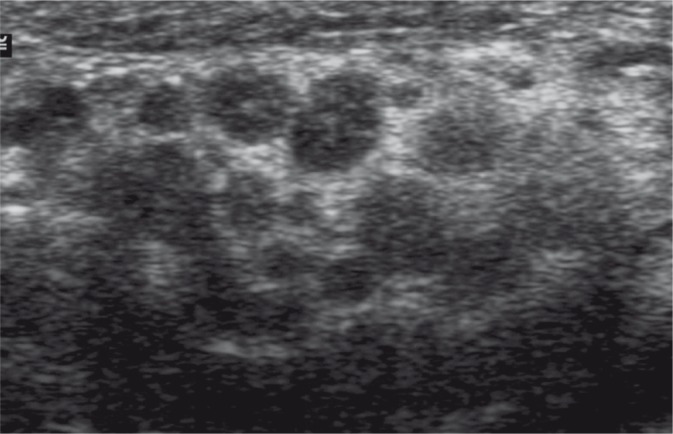
Fig. 15.
Vascular malformation. Transverse image showing a heterogeneous mass (arrowheads) containing a central focus of mineralization (phlebolith) with posterior acoustic shadowing
Fig. 17.
Vascular malformation. Coronal T2 fat-saturated image showing a heterogeneous mass with a low signal phlebolith
Fig. 16.
Vascular malformation. Plain radiograph confirming the presence of a phlebolith (arrowhead)
Lymphatic malformations consist of multiple lymphatic fluid containing spaces with intervening septa. On MRI they are comprised of septated cysts of variable size. Fluid-fluid levels may be seen. Stranding of the adjacent subcutaneous tissue may be seen due to associated lymphatic obstruction and may simulate cellulitis(25).
Arteriovenous malformations (AVMs) are high flow vascular malformations with abnormal connections between arteries and veins. AVMs have an intervening central nidus whereas arteriovenous fistulae do not. US shows enlarged vessels with high flow on Doppler. On MRI they appear as enlarged vascular channels without a discrete soft tissue mass which on spin echo imaging appear as signal voids with corresponding bright signal on flow-enhanced GE sequences. MR arthrography can be used to delineate the arterial supply. Skin thickening and fat deposition may be seen in association as well as perilesional edema(25) (figs. 18, 19).
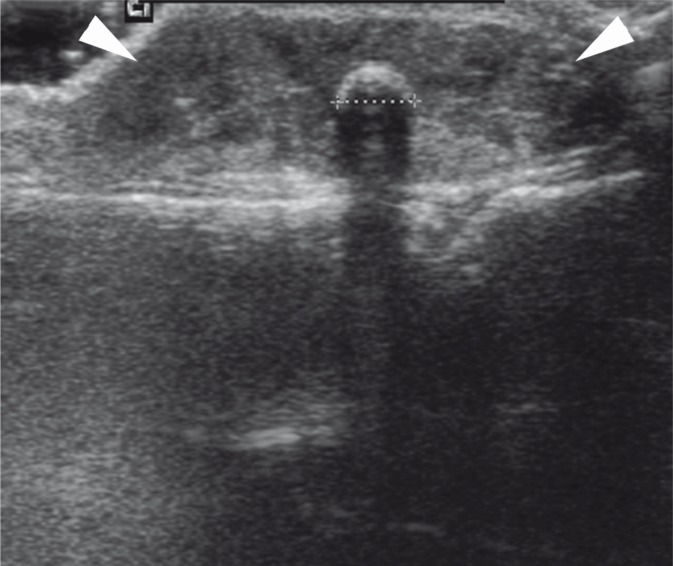
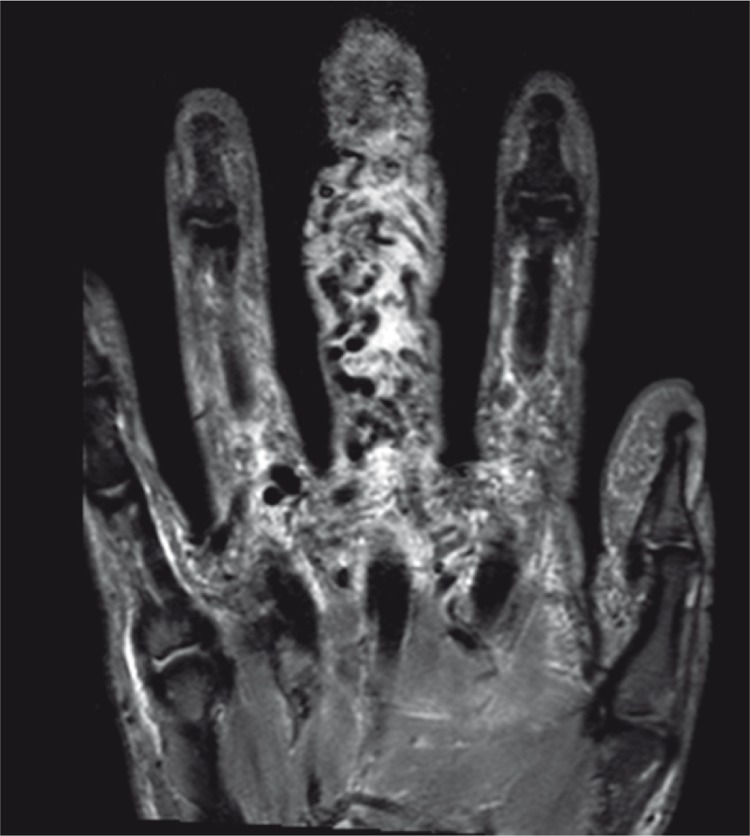
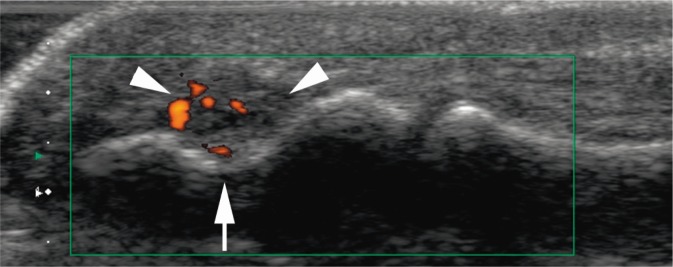
Fig. 18.
Arteriovenous fistula. Longitudinal image showing a leash of high flow vessels in the pulp of the middle finger (arrowheads) with marked flow on power Doppler
Fig. 19.
Arteriovenous fistula. Coronal T2 fat-saturated image showing an enlarged digit with flow void in multiple dilated vessels
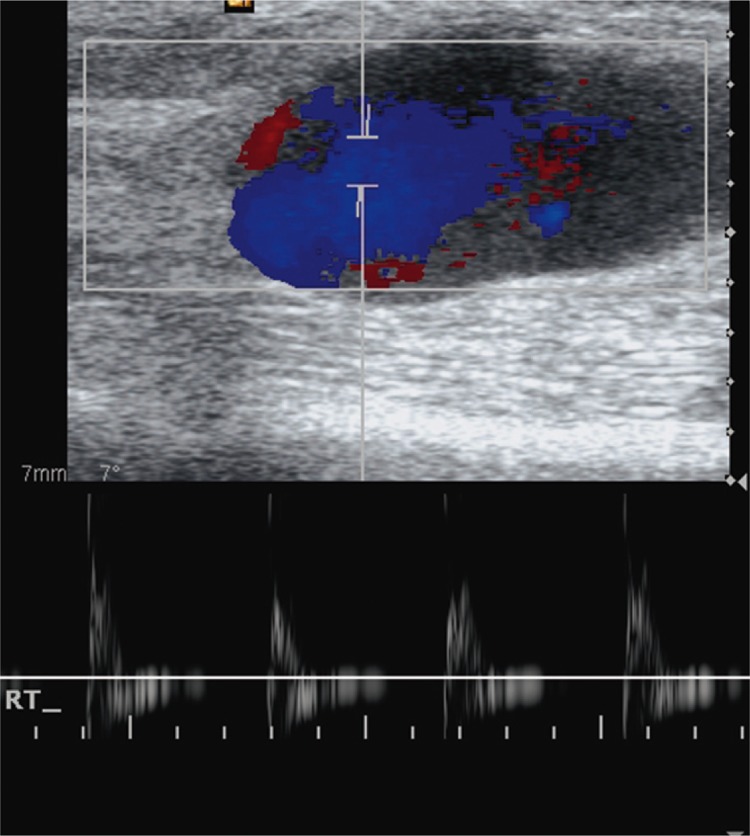
Pseudoaneurysms, also known as false aneurysms, are perfused sacs that form outside the arterial wall, and are contained by the surrounding tissues. It arises from damage or a defect of the arterial wall so typically follows trauma or arterial puncture. Under the influence of sustained arterial pressure, blood dissects into the tissues around the damaged artery. A true aneurysm on the other hand is a localized dilatation of an artery including all the layers of the vessel wall. On ultrasound there is a cystic mass arising adjacent to an artery, with high flow on Doppler (fig. 20).
Fig. 20.
Ulnar aneurysm. Transverse Doppler US showing high flow within an anechoic structure. B-mode ultrasound shows arterial flow
Benign peripheral nerve sheath tumors
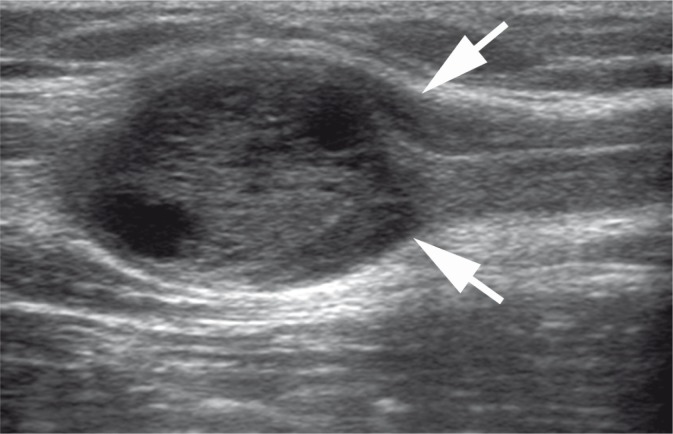
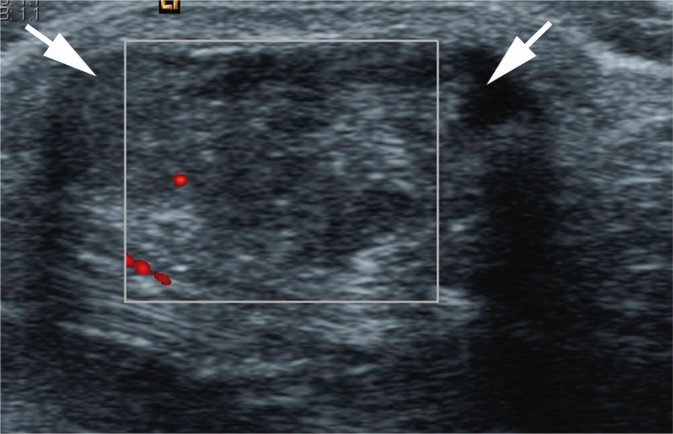
Benign peripheral nerve sheath tumors (PNST) have classically been divided into schwannomas and neurofibromas. Schwannomas arise from the Schwann cells surrounding the nerve whereas neurofibromas arise from the central nerve fascicles(26). They are relatively common masses of the hand and wrist. In general, schwannomas tend to arise from deeper and larger nerves (in particular the ulnar nerve) whereas neurofibromas tend to involve the smaller cutaneous nerves. PNST present in adulthood, usually between the ages of 20 to 30, and are small, solitary and slow growing. The vast majority of these are not associated with neurofibromatosis(18).
The characteristic imaging feature of neurogenic tumors is of a fusiform mass with a “dural tail”, representing the entering and exiting nerve(26). This may be clearly visualized when the nerve is large or deep, but with superficial small PNST this feature may not be seen (fig. 21). Schwannomas tend to lie eccentrically in relation to the nerve which may allow its differentiation from a neurofibroma. Furthermore, schwannomas are also usually more heterogeneous because of the presence of cysts, necrosis, and hemorrhage (figs. 22, 23).
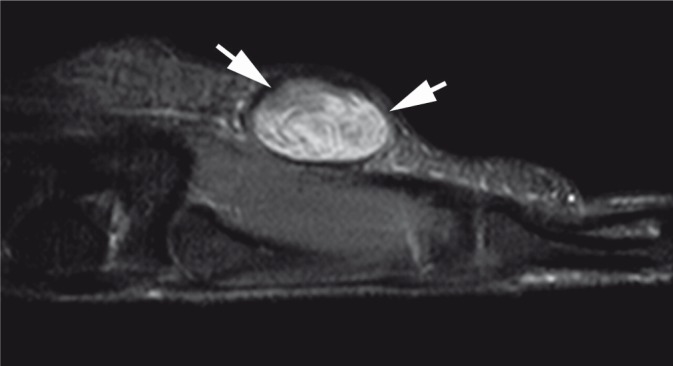
Fig. 21.
Neurofibroma. Ovoid mass with small areas of cyst formation demonstrating a dural tail (arrows)
Fig. 22.
Schwannoma. Heterogeneous mass with poor vascularity. The findings are rather non-specific
Fig. 23.
Same patient as fig. 22. Sagittal T2 fat-saturated sequence showing a heterogeneous ovoid mass (arrows) thought to be arising from a superficial branch of the ulnar nerve
The “split fat” sign may be seen around PNST, and occurs because the nerve bundle is surrounded by fat, so masses arising from this location maintain a rim of fat around them(27).
The echogenicity of neurogenic tumors is fairly nonspecific, and lesions may appear heterogeneous. A target sign with a central area of low echogenicity corresponds to central fibromatosis and surrounding myxomatosis tissue(27). A layer of connective tissue or epineurium surrounds each nerve trunk. Bundles of nerve fibers in turn are surrounded by perineurium. This gross appearance can be recognized on imaging particularly in large nerve trunks, which has been described as the fascicular appearance. This sign can also be seen in PNST and manifests as multiple small ring like structures corresponding to the fascicular bundles within the nerve(26).
Muscle denervation and subsequent atrophy may be appreciated on MRI or US in patients with neuropathy due to PNST. On US there is increased echogenicity of the muscle. Fatty infiltration is best shown on T1-weighted images and may require the contra lateral side for comparison.
Features suggestive of malignancy on MRI and US include large size (greater than 5 cm), infiltrative margins, marked heterogeneity and rapid growth(26, 27).
Glomus tumor
Glomus bodies are responsible for thermoregulation and are present throughout the dermis of the body but are particularly concentrated in the digits of the hand and foot. Glomus tumors are small hamartomas of the neuromyoarterial apparatus within the glomus body and account for up to 5% of soft tissue tumors of the hand(28). Histologically, they have uniform rounded cells that have distinct cell borders, round nuclei, and pale eosinophilic cytoplasm. They are most commonly found at the finger tip, either in the pulp or beneath the fingernail, and typically present in the 4th and 5th decades as exquisitely painful lesions with pinpoint tenderness exacerbated by temperature changes. The disappearance of pain after application of a tourniquet proximally on the arm is pathognomonic of the tumor and is known as the Hildreth's sign.
On X-ray, smooth extrinsic bone erosions adjacent to the lesion may be seen with chronic large lesions. On ultrasound glomus tumors appear as small well-circumscribed hypoechoic masses with increased vascularity. Often the appearance is of an AV malformation on Doppler. Bone erosion may be evident. The patient is usually able to localize the position of the tumor accurately due to pinpoint tenderness (fig. 24).
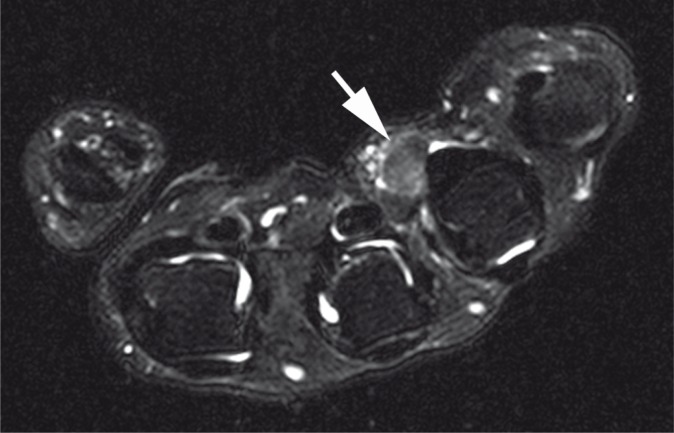
Fig. 24.
Glomus tumor of finger pulp. Small vascular tumor in the pulp (arrowheads) with erosion of the underlying distal phalanx (arrow)
Lesions as small as 2 mm may be detected with MRI. They are usually of low or intermediate signal on T1-weighted images and homogenous signal high on T2-weighted images. They enhance uniformly following gadolinium.
Malignant masses
Malignant soft tissue tumors of the hand are uncommon(1, 2, 5). The lesions most often encountered are undifferentiated pleomorphic sarcoma (previously called malignant fibrous histiocytoma) in the older population, synovial sarcoma, rhabdomyosarcoma, malignant nerve sheath tumors, liposarcomas and extraskeletal chondrosarcomas(18). Because of nonspecific morphological features, these tumors can be confused with benign lesions such as aggressive fibromatosis or ganglion cysts, particularly when they are small. The possibility of a malignant lesion needs to be considered when the mass does not have an unequivocal benign diagnosis on imaging(29).
The imaging features that should raise the possibility of malignancy are a rapidly growing, large lesion with poorly defined margins.
Using a combination of Doppler imaging with spectral wave analysis, researchers have attempted to differentiate benign from malignant lesions(8, 30). Malignant tumors have vessels with an irregular margin and lack a muscle layer. On Doppler imaging, these vessels may show an anarchic pattern, with occlusions, stenoses, arteriovenous shunts, and loops(31). Benign tumors usually have a simple branching vascular morphology. The morphologic analysis of tumor vessels appears to be more reliable than quantitative parameters such as flow velocities or resistive indices. In practice, a cautious approach should be taken as not all malignant soft-tissue tumors have an anarchic pattern. Furthermore some necrotic lesions and low-grade neoplasms may not demonstrate neovascularity and therefore the absence of flow does not necessarily indicate benignity (figs. 25, 26).
Fig. 25.
Chondrosarcoma of hand. Large lobulated mass with areas of echogenic mineralization
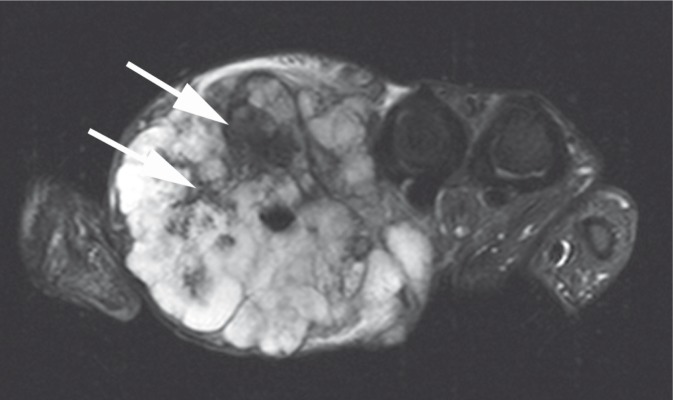
Fig. 26.
Chondrosarcoma of hand. Coronal STIR image showing a large lobulated high T2 signal mass with foci of low signal mineralization (arrows)
On MRI of malignant tumors there may be inhomogeneity on T2-weighted images, irregular enhancement following intravenous contrast and the presence of necrosis. Often the imaging findings are non-specific and biopsy is required to provide a histological diagnosis.
Pseudomasses
Synovial pathology
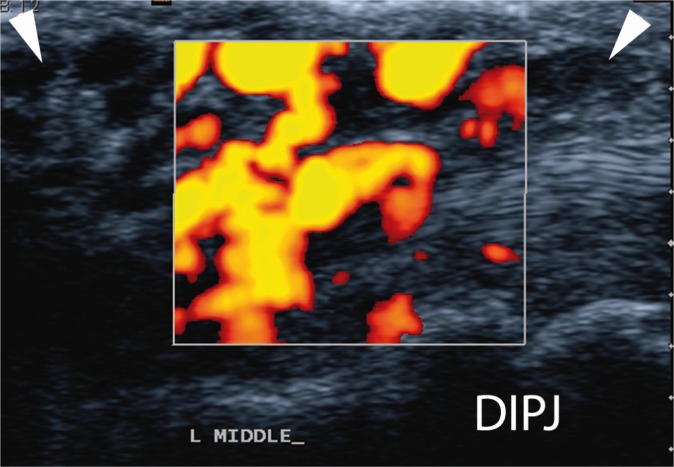
Synovial hyperplasia, tenosynovitis and crystal arthropathies can present as a focal masses around joints and tendons. This may occur as an isolated abnormality or in the setting of a known systemic disease, particularly rheumatoid arthritis. Ultrasound and MRI are both useful for defining the extent of disease. Ultrasound has the advantage of assessing vascularity in real time, and is superior at delineating associated calcification (figs. 27, 28).
Fig. 27.
Pseudogout of the wrist. Echogenic mass (arrowheads) arising from the volar radiocarpal joint with multiple foci of increased echogenicity in keeping with mineralization
Fig. 28.
Pseudogout of the wrist. Same patient as fig. 27. Sagittal T2 fat-saturated image showing a heterogeneous mass with foci of low signal mineralization
Anomalous muscles
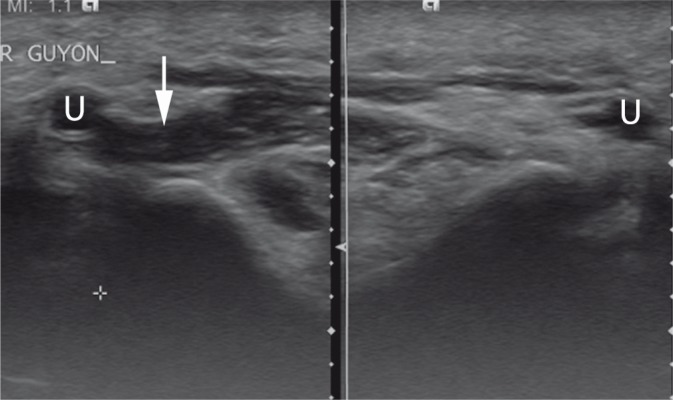
Anomalous muscles of the wrist and hand are common(32). Although they are usually clinically silent, they may cause compressive symptoms or appear mass-like. Often lesions are not recognized on imaging, as the echotexture is identical to normal muscle. The sonographer therefore requires a thorough knowledge of anatomy and normal variation. The accessory abductor digiti minimi muscle is present in up to 24% of all wrists(32). A fusiform mass is present with the echotexture of muscle lateral and anterior to the pisiform bone at the level of the origin of the abductor digiti minimi muscle. This may result in compression of the ulnar nerve in Guyon's canal(33) (fig. 29). The extensor digitorum brevis manus muscle may be mistaken for a dorsal ganglion and occurs in up to 3% of the population. The muscle arises from the distal radius and inserts on the index finger. The muscle belly is seen medial to the tendon of the index finger at or distal to the level of the carpus. Lumbrical muscles may arise within the carpal tunnel causing carpal tunnel syndrome and may be seen in up to 22% of individuals(32).
Fig. 29.
Accessory abductor digiti minimi muscle in Guyon's canal (arrow). Comparison is made with the contralateral wrist. The ulnar artery is marked on both sides (U)
Soft tissue infection
A soft tissue infection with abscess formation may mimic a soft tissue mass. A prompt imaging evaluation of soft tissue infection will facilitate early diagnosis and treatment, and thus decrease the risk of complications. US can help delineate the extent of involvement and determine if there is associated tenosynovitis or periostitis, which may indicate osteomyelitis. US also has an invaluable role in allowing guided aspiration or biopsy of inflammatory collections.
With cellulitis US may demonstrate skin thickening with subcutaneous edema. Hypervascularity, indistinct tissue planes, and small linear fluid collections tracking along interlobular septa and encircling hyperechoic fat lobules may also be seen(34). Simple collections or abscesses are of low echogenicity with increased through transmission. Complex collections may show mixed echogenicity, and may be surrounded by a thick hyperechoic and hyperemic wall. Dynamic compression may demonstrate swirling of the contents. A phlegmon is a solid inflammatory mass, which may have a poorly defined margins and mixed echogenicity with increased vascularity (fig. 30).
Fig. 30.
Abscess and phlegmon on dorsum of wrist. A small anechoic abscess is present with marked surrounding soft tissue inflammation with increased vascularity
Infective tenosynovitis commonly occurs as the result of penetrating trauma and therefore most often affects flexor tendons of the hands(34). On ultrasound there is fluid in the tendon sheath with synovial thickening and increased vascularity. The appearances may be indistinguishable from inflammatory tenosynovitis.
Retained foreign bodies from penetrating trauma may give rise to pain and swelling. Often foreign bodies are undetectable on plain radiographs, particularly if they are organic material, such as wood. On ultrasound foreign bodies are easily detectable and appear as hyperechoic fragments, which may demonstrate posterior acoustic shadowing. Superadded infection may result in a phlegmon or abscess. Foreign body granulomas appear as a hypoechoic mass surrounding the foreign body (fig. 31).
Fig. 31.
Foreign body granuloma. An echogenic splinter (arrowhead) with posterior acoustic shadowing and surrounding foreign body granuloma (arrows)
Conflict of interest
Author does not report any financial or personal links with other persons or organizations, which might affect negatively the content of this publication and/or claim authorship rights to this publication.
References
- 1.Johnson J, Kilgore E, Newmeyer W. Tumorous lesions of the hand. J Hand Surg Am. 1985;10:284–286. doi: 10.1016/s0363-5023(85)80124-6. [DOI] [PubMed] [Google Scholar]
- 2.Capelastegui A, Astigarraga E, Fernandez-Canton G, Saralegui I, Larena JA, Merino A. Masses and pseudomasses of the hand and wrist: MR findings in 134 cases. Skeletal Radiol. 1999;28:498–507. doi: 10.1007/s002560050553. [DOI] [PubMed] [Google Scholar]
- 3.Miller TT, Potter HG, McCormack RR., Jr Benign soft tissue masses of the wrist and hand: MRI appearances. Skeletal Radiol. 1994;23:327–332. doi: 10.1007/BF02416985. [DOI] [PubMed] [Google Scholar]
- 4.Binkovitz LA, Berquist TH, McLeod RA. Masses of the hand and wrist: detection and characterization with MR imaging. AJR Am J Roentgenol. 1990;154:323–326. doi: 10.2214/ajr.154.2.2105024. [DOI] [PubMed] [Google Scholar]
- 5.Teh J, Whiteley G. MRI of soft tissue masses of the hand and wrist. Br J Radiol. 2007;80:47–63. doi: 10.1259/bjr/53596176. [DOI] [PubMed] [Google Scholar]
- 6.Hoglund M, Muren C, Brattstrom G. A statistical model for ultrasound diagnosis of soft-tissue tumours in the hand and forearm. Acta Radiol. 1997;38:355–358. doi: 10.1080/02841859709172082. [DOI] [PubMed] [Google Scholar]
- 7.Teefey SA, Middleton WD, Boyer MI. Sonography of the hand and wrist. Semin Ultrasound CT MR. 2000;21:192–204. doi: 10.1016/s0887-2171(00)90042-8. [DOI] [PubMed] [Google Scholar]
- 8.Teh J. Applications of Doppler imaging in the musculoskeletal system. Curr Probl Diagn Radiol. 2006;35:22–34. doi: 10.1067/j.cpradiol.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Klauser AS, Peetrons P. Developments in musculoskeletal ultrasound and clinical applications. Skeletal Radiol. 2009 doi: 10.1007/s00256-009-0782-y. [DOI] [PubMed] [Google Scholar]
- 10.Teefey SA, Dahiya N, Middleton WD, Gelberman RH, Boyer MI. Ganglia of the hand and wrist: a sonographic analysis. AJR Am J Roentgenol. 2008;191:716–720. doi: 10.2214/AJR.07.3438. [DOI] [PubMed] [Google Scholar]
- 11.Thornburg LE. Ganglions of the hand and wrist. J Am Acad Orthop Surg. 1999;7:231–238. doi: 10.5435/00124635-199907000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Murphey MD, Rhee JH, Lewis RB, Fanburg-Smith JC, Flemming DJ, Walker EA. Pigmented villonodular synovitis: radiologic-pathologic correlation. Radiographics. 2008;28:1493–1518. doi: 10.1148/rg.285085134. [DOI] [PubMed] [Google Scholar]
- 13.Middleton WD, Patel V, Teefey SA, Boyer MI. Giant cell tumors of the tendon sheath: analysis of sonographic findings. AJR Am J Roentgenol. 2004;183:337–339. doi: 10.2214/ajr.183.2.1830337. [DOI] [PubMed] [Google Scholar]
- 14.Yacoe ME, Bergman AG, Ladd AL, Hellman BH. Dupuytren's contracture: MR imaging findings and correlation between MR signal intensity and cellularity of lesions. AJR Am J Roentgenol. 1993;160:813–817. doi: 10.2214/ajr.160.4.8456670. [DOI] [PubMed] [Google Scholar]
- 15.Créteur V, Madani A, Gosset N. [Ultrasound imaging of Dupuytren's contracture] J Radiol. 2010;91:687–691. doi: 10.1016/s0221-0363(10)70098-6. [DOI] [PubMed] [Google Scholar]
- 16.Quinn SF, Erickson SJ, Dee PM, Walling A, Hackbarth DA, Knudson GJ, et al. MR imaging in fibromatosis: results in 26 patients with pathologic correlation. AJR Am J Roentgenol. 1991;156:539–542. doi: 10.2214/ajr.156.3.1899752. [DOI] [PubMed] [Google Scholar]
- 17.Horcajadas AB, Lafuente JL, de la Cruz Burgos R, Muñiz SH, Roca SA, Ortega SG, et al. Ultrasound and MR findings in tumor and tumor-like lesions of the fingers. Eur Radiol. 2003;13:672–685. doi: 10.1007/s00330-002-1477-0. [DOI] [PubMed] [Google Scholar]
- 18.Kransdorf MJ. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995;164:395–402. doi: 10.2214/ajr.164.2.7839977. [DOI] [PubMed] [Google Scholar]
- 19.Kransdorf MJ, Murphey MD. MR imaging of musculoskeletal tumors of the hand and wrist. Magn Reson Imaging Clin N Am. 1995;3:327–344. [PubMed] [Google Scholar]
- 20.Inampudi P, Jacobson JA, Fessell DP, Carlos RC, Patel SV, Delaney-Sathy L, et al. Soft-tissue lipomas: accuracy of sonography in diagnosis with pathologic correlation. Radiology. 2004;233:763–767. doi: 10.1148/radiol.2333031410. [DOI] [PubMed] [Google Scholar]
- 21.Laorr A, Greenspan A. Hand lipomas: detection and characterization by magnetic resonance imaging. Can Assoc Radiol J. 1993;44:14–18. [PubMed] [Google Scholar]
- 22.Marom EM, Helms CA. Fibrolipomatous hamartoma: pathognomonic on MR imaging. Skeletal Radiol. 1999;28:260–264. doi: 10.1007/s002560050512. [DOI] [PubMed] [Google Scholar]
- 23.Mulliken JB, Glowacki J. Classification of pediatric vascular lesions. Plast Reconstr Surg. 1982;70:120–121. [PubMed] [Google Scholar]
- 24.Fishman SJ, Mulliken JB. Hemangiomas and vascular malformations of infancy and childhood. Pediatr Clin North Am. 1993;40:1177–1200. doi: 10.1016/s0031-3955(16)38656-4. [DOI] [PubMed] [Google Scholar]
- 25.Robertson RL, Robson CD, Barnes PD, Burrows PE. Head and neck vascular anomalies of childhood. Neuroimaging Clin N Am. 1999;9:115–132. [PubMed] [Google Scholar]
- 26.Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiographics. 1999;19:1253–1280. doi: 10.1148/radiographics.19.5.g99se101253. [DOI] [PubMed] [Google Scholar]
- 27.Abreu E, Aubert S, Wavreille G, Gheno R, Canella C, Cotten A. Peripheral tumor and tumor-like neurogenic lesions. Eur J Radiol. 2011 doi: 10.1016/j.ejrad.2011.04.036. [DOI] [PubMed] [Google Scholar]
- 28.Glazebrook KN, Laundre BJ, Schiefer TK, Inwards CY. Imaging features of glomus tumors. Skeletal Radiol. 2011;40:855–862. doi: 10.1007/s00256-010-1067-1. [DOI] [PubMed] [Google Scholar]
- 29.Nakajima H, Matsushita K, Shimizu H, Isomi T, Nakano Y, Saito M, et al. Synovial sarcoma of the hand. Skeletal Radiol. 1997;26:674–676. doi: 10.1007/s002560050310. [DOI] [PubMed] [Google Scholar]
- 30.Widmann G, Riedl A, Schoepf D, Glodny B, Peer S, Gruber H. State-of-the-art HR-US imaging findings of the most frequent musculoskeletal soft-tissue tumors. Skeletal Radiol. 2009;38:637–649. doi: 10.1007/s00256-008-0602-9. [DOI] [PubMed] [Google Scholar]
- 31.Griffith JF, Chan DP, Kumta SM, Chow LT, Ahuja AT. Does Doppler analysis of musculoskeletal soft-tissue tumours help predict tumour malignancy? Clin Radiol. 2004;59:369–375. doi: 10.1016/j.crad.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 32.Timins ME. Muscular anatomic variants of the wrist and hand: findings on MR imaging. AJR Am J Roentgenol. 1999;172:1397–1401. doi: 10.2214/ajr.172.5.10227524. [DOI] [PubMed] [Google Scholar]
- 33.Harvie P, Patel N, Ostlere SJ. Prevalence and epidemiological variation of anomalous muscles at Guyon's canal. J Hand Surg Br. 2004;29:26–29. doi: 10.1016/j.jhsb.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 34.Chau CL, Griffith JF. Musculoskeletal infections: ultrasound appearances. Clin Radiol. 2005;60:149–159. doi: 10.1016/j.crad.2004.02.005. [DOI] [PubMed] [Google Scholar]