Abstract
OBJECTIVE
To assess the feasibility of HIV rapid testing for pregnant women at maternity hospital admission and of subsequent interventions to reduce perinatal HIV transmission.
METHODS
Study based on a convenience sample of women unaware of their HIV serostatus when they were admitted to delivery in public maternity hospitals in Rio de Janeiro and Porto Alegre, Brazil, between March 2000 and April 2002. Women were counseled and tested using the Determine HIV1/2 Rapid Test. HIV infection was confirmed using the Brazilian algorithm for HIV infection diagnosis. In utero transmission of HIV was determined using HIVDNA-PCR. There were performed descriptive analyses of sociodemographic data, number of previous pregnancies and abortions, number of prenatal care visits, timing of HIV testing, HIV rapid test result, neonatal and mother-to-child transmission interventions, by city studied.
RESULTS
HIV prevalence in women was 6.5% (N=1,439) in Porto Alegre and 1.3% (N=3.778) in Rio de Janeiro. In Porto Alegre most of women were tested during labor (88.7%), while in Rio de Janeiro most were tested in the postpartum (67.5%). One hundred and forty-four infants were born to 143 HIV-infected women. All newborns but one in each city received at least prophylaxis with oral zidovudine. It was possible to completely avoid newborn exposure to breast milk in 96.8% and 51.1% of the cases in Porto Alegre and Rio de Janeiro, respectively. Injectable intravenous zidovudine was administered during labor to 68.8% and 27.7% newborns in Porto Alegre and Rio de Janeiro, respectively. Among those from whom blood samples were collected within 48 hours of birth, in utero transmission of HIV was confirmed in 4 cases in Rio de Janeiro (4/47) and 6 cases in Porto Alegre (6/79).
CONCLUSIONS
The strategy proved feasible in maternity hospitals in Rio de Janeiro and Porto Alegre. Efforts must be taken to maximize HIV testing during labor. There is a need of strong social support to provide this population access to health care services after hospital discharge.
Keywords: Pregnant Women; Prenatal Care; Breast Feeding; AIDS Serodiagnosis; HIV Infections, diagnosis; Infectious Disease Transmission, Vertical; Acquired Immunodeficiency Syndrome, prevention & control
INTRODUCTION
The prevention of mother-to-child transmission (PMTCT) has been a major successful public health effort to prevent HIV infection in developed countries. The use of highly active antiretroviral therapy (HAART) regimens during pregnancy for PMTCT, along with scheduled cesarean delivery and breastfeeding avoidance, have reduced HIV transmission rates to under 2%.4
In developing countries, where the HIV impact is greatest, success has been limited not only by the cost involved on universal implementation of these interventions, but also by the weakness of health systems.6 Brazil was the first developing country to implement a countrywide program to prevent HIV vertical transmission. HIV counseling and testing, HAART and infant formula are provided free of charge to patients.21 Although significant progress in reducing HIV mother-to-child transmission (MTCT) has been seen in Brazil,7 a significant number of new HIV cases among infants continue to occur yearly. Women are either not tested during pregnancy or results are not available by the time of delivery.20 Rapid assays emerged to meet the demand where HIV testing is the main barrier to PMTCT.15
In Brazil, over 95% of women give birth in hospitals,a creating a key opportunity for systematic offering of HIV rapid testing, and other PMTCT interventions. The objective of the present study was to assess the feasibility of HIV rapid testing for pregnant women at maternity hospital admission and of interventions to reduce perinatal HIV transmission.
METHODS
We conducted a cross-sectional study. The study population was a convenience sample of women with unknown HIV serostatus, admitted for delivery in middle- and high-complexity maternity departments of charity or state-run hospitals in the metropolitan areas of Rio de Janeiro (RJ) and Porto Alegre (POA), Southeastern and Southern Brazil, respectively. The study was conducted between March 2000 and April 2002. The study sites in the city of POA started the study on May 2001.
The inclusion criteria included: unknown HIV serostatus (not tested in the current pregnancy or tested but women were not aware of the test result) by the time of admission for delivery; and signed informed consent. Women younger than 18 years old, not married or living with a partner or whose parents could not provide an informed consent for their participation were excluded as well as those with any clinical condition that could prevent them from being interviewed. Liveborn infants delivered by women found to be HIV infected were enrolled.
Women admitted were approached before delivery or in the postpartum. The underlying reasons for ineligibility or for refusing to participate were recorded in a contact form.
Women were informed that, although a positive result in the rapid testing would not be a final diagnosis, PMTCT intervention (intravenous AZT, oral AZT and infant formula feeding) would be provided following the Brazilian Ministry of Health guidelines.b
Women were counseled and tested on-site using the Determine HIV 1/2 Rapid Test (Abbott, Chicago, IL, USA) on whole blood. All positive results were confirmed by local laboratories following the Brazilian Ministry of Health algorithm for HIV diagnosis (HIV-1 EIA followed by HIV indirect immunofluorescence or HIV Western blot assay). Women with positive test results were seen once by a study team member in the postpartum and referred to HIV/AIDS specialized care in reference centers. At discharge, study outpatient visits were scheduled at one, three and six months for infants born to these women.
For infant's HIV diagnosis, blood samples were collected within 48 hours of birth and during study visits. HIV-1 infection in infants was defined as the detection of HIV DNA by polymerase chain reaction (PCR) on two peripheral blood samples collected in different visits or the development of AIDS or death from an HIV-1-related cause. A child was classified as HIV-1 uninfected if he or she was PCR negative on at least two occasions (with the second sample being obtained at three months of age or later). Infants with a positive DNA PCR in the blood sample collected within 48 hours of birth were defined as in utero-infected.2 For children who missed study visits, serology data were retrospectively collected and persistence or absence of antibody to HIV-1 beyond 18 months was considered for the determination of HIV infection status.
Sociodemographic, reproductive and prenatal care data were collected by trained interviewers through of a structured questionnaire. All forms were piloted in the field by at least one member of local study teams. Complementary clinical and laboratory data were obtained from women's and infant's charts. Ethnicity/skin color was classified by the interviewers. The EpiInfo software 6.04 version was used to create study forms, enter data and minimize errors in data entry process. Data analysis was performed using the Statistical Package for Social Sciences (SPSS), version 7.0 for Windows.
Descriptive statistics were generated for all variables: age, schooling, skin color/ethnicity, family income, number of prenatal care visits, number of previous pregnancies and abortions, timing of HIV testing, HIV rapid test results, PMTCT intervention (intravenous AZT, oral AZT and infant formula feeding) and HIV MTCT. Mean (standard deviation, SD) and median (interquartile interval, IQI) were used to describe continuous variables. Contingency table statistics were used to verify non-homogeneity of proportions to compare women's sociodemographic, reproductive characteristics and prenatal care use in RJ and POA.
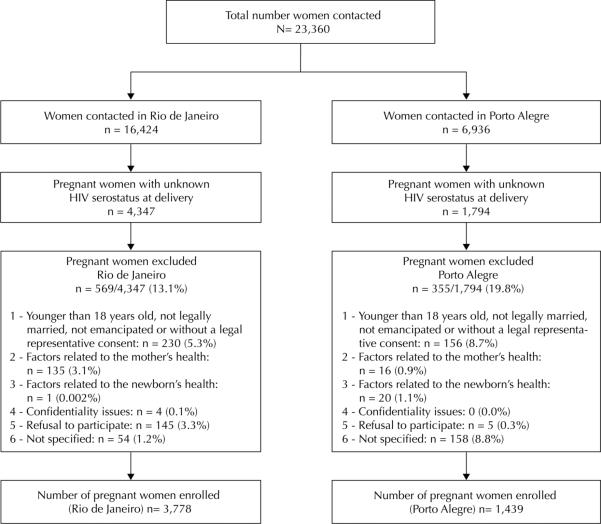
In RJ and POA, 23,360 women were contacted; of them, 73.5% and 74.1%, respectively, were tested during the current pregnancy and were unaware of their HIV serostatus. Among pregnant women with unknown HIV serostatus at delivery, 3.3% in RJ (4,347) and 0.3% in POA (1,794) refused to participate in this study. Other reasons for exclusion are presented in the Figure.
Figure.
Study population for HIV rapid testing and perinatal intervention in Brazil. Cities of Rio de Janeiro and Porto Alegre, Southeastern and Southern Brazil, 2000–2002.
The study protocol was approved by Institutional Review Boards of each maternity hospital and by the National Research Ethics Committee (CONEP) (Process Nr. 25000.002537/99-67; Approval date 02/26/1999).
RESULTS
Table 1 shows sociodemographic, reproductive and prenatal characteristics of pregnant women studied. Mean age was 24.6 (SD=6.5) and median age was 23 (IQI: 12;47). Overall, 82.6% of the women had eight or less years of schooling.
Table 1.
Sociodemographic, reproductive and prenatal care characteristics of the study participants. Cities of Rio de Janeiro and Porto Alegre, Southeastern and Southern Brazil, 2000–2002.
| Variable | Rio de Janeiro (n = 3,778) | Porto Alegre (n = 1,439) | Total (n = 5,217) | p-value | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Age (years) | |||||||
| < 20 | 987 | 26.1 | 295 | 20.5 | 1,282 | 24.6 | 0.000 |
| 20–24 | 1,260 | 33.4 | 458 | 31.8 | 1,718 | 32.9 | |
| 25–29 | 736 | 19.5 | 302 | 21.0 | 1,038 | 19.9 | |
| 30–34 | 433 | 11.4 | 204 | 14.2 | 637 | 12.2 | |
| ≥ 35 | 351 | 9.3 | 159 | 11.0 | 510 | 9.8 | |
| Missing information | 11 | 0.3 | 21 | 1.5 | 32 | 0.6 | |
| Schooling (years) | |||||||
| ≤ 4 | 1,224 | 32.4 | 461 | 32.0 | 1,685 | 32.3 | 0.183 |
| 5–8 | 1,879 | 49.7 | 746 | 51.9 | 2,625 | 50.3 | |
| >8 | 669 | 17.7 | 226 | 15.7 | 895 | 17.2 | |
| Missing information | 6 | 0.2 | 6 | 0.4 | 12 | 0.2 | |
| Skin color/ethnicity | |||||||
| White | 1,093 | 28.9 | 882 | 61.3 | 1,975 | 37.9 | 0.000 |
| Mixed | 1,531 | 40.5 | 204 | 14.2 | 1,735 | 33.2 | |
| Black | 1,134 | 30.1 | 338 | 23.5 | 1,472 | 28.2 | |
| Asian/native | 13 | 0.3 | 11 | 0.7 | 24 | 0.5 | |
| Missing information | 7 | 0.2 | 4 | 0.3 | 11 | 0.2 | |
| Familiar income in Brazilian monthly minimal wages | |||||||
| ≤1 | 1,182 | 31.3 | 401 | 27.9 | 1,583 | 30.3 | 0.262 |
| >1 and <3 | 1,260 | 33.3 | 450 | 31.3 | 1,710 | 32.8 | |
| ≥3 | 1,283 | 34.0 | 494 | 34.3 | 1,777 | 34.1 | |
| Missing information | 53 | 1.4 | 94 | 6.5 | 147 | 2.8 | |
| Number of prenatal care visits | |||||||
| None | 867 | 23.0 | 521 | 36.2 | 1,388 | 26.6 | 0.000 |
| 1–3 | 840 | 22.2 | 316 | 22,0 | 1,156 | 22.2 | |
| 4–6 | 1,371 | 36.3 | 305 | 21.2 | 1,676 | 32.1 | |
| ≥7 | 693 | 18.3 | 211 | 14.6 | 904 | 17.3 | |
| Missing information | 7 | 0.2 | 86 | 6.0 | 93 | 1.8 | |
| Number of previous pregnancies | |||||||
| None | 1,051 | 27.8 | 268 | 18.6 | 1,319 | 25.3 | 0.000 |
| 1–2 | 1,684 | 44.6 | 625 | 43.4 | 2,309 | 44.3 | |
| ≥3 | 1,043 | 27.6 | 514 | 35.8 | 1,557 | 29.8 | |
| Missing information | – | – | 32 | 2.2 | 32 | 0.6 | |
| Number of abortions | |||||||
| None | 2,882 | 76.3 | 1,146 | 79.6 | 4,028 | 77.2 | 0.001 |
| 1 | 649 | 17.2 | 201 | 14.0 | 850 | 16.3 | |
| >1 | 242 | 6.4 | 57 | 4.0 | 299 | 5.7 | |
| Missing information | 5 | 0.1 | 35 | 2.4 | 40 | 0.8 | |
| Timing of HIV testing | |||||||
| During labor | 1,228 | 32.5 | 1,277 | 88.7 | 2,505 | 48.0 | 0.000 |
| Postpartum | 2,550 | 67.5 | 155 | 10.8 | 2,705 | 51.8 | |
| Missing information | – | – | 7 | 0.5 | 7 | 0.2 | |
| Rapid test result | |||||||
| Positive | 50 | 1.3 | 93 | 6.5 | 143 | 2.7 | 0.000 |
| Negative | 3,726 | 98.6 | 1,344 | 93.4 | 5,070 | 97.2 | |
| Missing information | 2 | 0.1 | 2 | 0.1 | 4 | 0.1 | |
About 60.0% of women were white in POA, and 70.0% were black or mixed ethnicity in RJ (p=0.000). Mean and median family income in Brazilian monthly minimum wages (BMMWs) in the last month was 2.5 (SD=2.3) and 2.0 (IQI: 0;60) in RJ and 2.6 (SD= 2.4) and 2.0 (IQI: 0;40) in POA. Family income up to one BMMW in the last month was reported by 30.3% of the women.
The proportion of women who did not attend prenatal care visits was higher in POA than in RJ. In RJ, women attended a higher number of prenatal visits compared to those in POA. Mean and median number of prenatal visits in RJ was 3.8 (SD=3.0) and 4.0 (IQI= 0;22) and in POA 2.9 (SD=3.1) and 2.0 (IQI: 0;23).
Mean and median number of previous pregnancies was 2.8 (SD=1.9) and 3.3 (SD=2.1) in RJ and 2.0 (IQI: 1;15) and 3.0 (IQI: 1;13) in POA; 27.8% of women in RJ and 18.6% in POA were primiparous.
The proportion of women who reported at least one abortion was 23.6% in RJ and 18% in POA (p=0.001).
In RJ, 67.5% of women were tested in the postpartum period, while in POA, 88.7% were tested during labor (p=0.000). HIV infection was diagnosed in 6.5% and 1.3% of women in POA and in RJ, respectively (p=0.000). One hundred and forty-two singletons and a pair of twins were born to 143 HIV-infected women. One stillbirth and one newborn died within a few minutes after birth and were not considered for the description of PMTCT interventions in RJ.
All but one newborn in each city received oral zidovudine. Among the newborns, 27.7% and 68.8% in RJ and POA, respectively, were benefited from in utero ZDV exposure. Complete avoidance of newborn exposure to breast milk was possible in 96.8% of the cases in POA and 51.1% in RJ while they were in the maternity hospital (Table 2).
Table 2.
Prevention of mother-to-child transmission interventions provided to women and their newborns. Cities of Rio de Janeiro and Porto Alegre, Southeastern and Southern Brazil, 2000–2002.
| Interventions to the newborn – n (%) | Rio de Janeiro | Porto Alegre | Total (n = 140)d,e,f | ||||
|---|---|---|---|---|---|---|---|
| Labor (n = 17) | Postpartum (n = 30)e,f | Total (n = 47)e,f | Labor (n = 86) | Postpartum (n = 7)d | Total (n = 93)d | ||
| PREP AZTa + NAMb + PEP AZTc | 13 (76.5) | – | 13 (27.7) | 64 (74.4) | – | 64 (68.8) | 77 (55.0) |
| NAM + PEP AZT | 1 (5.9) | 10 (33.3) | 11 (23.4) | 18 (20.9) | 7 (100.0) | 25 (26.9) | 36 (25.7) |
| NAM only | – | – | – | 1 (1.2) | – | 1 (1.1) | 1 (0.7) |
| PEP AZT only | 2 (11.8) | 20 (66.7) | 22 (46.8) | 3 (3.5) | – | 3 (3.2) | 25 (17.9) |
| No intervention | 1 (5.9) | – | 1 (2.1) | – | – | – | 1 (0.7) |
PREP ZDV: Pre-exposure prophylaxis with intravenous zidovudine.
NAM: No breastfeeding while in the maternity hospital.
PEP ZDV: Post-exposure prophylaxis with oral zidovudine.
Information regarding PREP ZDV and PEP ZDV were not available for one newborn in Porto Alegre (mother tested during labor). This newborn was not included in the table as we could not determine which set of interventions he received (missing data).
Information about breastfeeding while in the maternity hospitals was not available for one newborn in Rio de Janeiro. This newborn received PEP AZT (mother tested in the postpartum period). This newborn was not included in the table as we could not determine which set of interventions he received (missing data).
One stillbirth and one newborn who died within a few minutes after birth both in Rio de Janeiro were not included in the table.
About 75% of the newborns from those women tested during labor received pre- and post-exposure ZDV and were not breastfeed during their stay in the maternity hospital. One newborn in RJ did not receive any of the three recommended PMTCT interventions.
Among the newborns whose mothers were tested in the postpartum, 100% in RJ and POA received post-exposure prophylaxis with ZDV. In RJ, 33.3% of newborns from women tested in the postpartum period were not breastfeed while in the maternity hospital. In POA, none of the newborns were breastfeed (Table 2).
Perinatal HIV transmission was confirmed in 14.6% and 11.7% of the newborns in RJ and POA, respectively. Blood samples collected within 48 hours from birth for DNA PCR were obtained for 126 newborns and in utero transmission of HIV was confirmed in ten newborns, of which four (4/47) in RJ and six (6/79) in POA. Two newborns had a positive HIV DNA PCR result in the sample collected within 48 hours of birth, but their diagnosis could not be confirmed due to the lack of a subsequent sample. Three infants in RJ had an undetermined DNA PCR within 48 hours from birth, with no subsequent sample for confirmation. HIV infection status could not be determined in 44.4% of the infants because they were lost to follow-up early during the study.
DISCUSSION
We found a high level of acceptance of HIV rapid testing among women admitted for delivery in RJ and POA. Similar acceptance rates (98%) were reported in RJ14 and India.16 Lower rates were reported in the United States by the Miriad study (84.0%)3 and in Russia (89.2%).12
Considering the wide availability of PMTCT interventions in Brazil, the proportion of women contacted during this study who reported unknown HIV serostatus is unacceptably high (26.3%). Ideally, all women should be screened for HIV during an initial prenatal visit. Among those enrolled in our study, the overwhelming majority had access to prenatal both in RJ and POA, with roughly 50% having had four or more visits. In spite of this, they were not tested or were unaware of their HIV test results.
In the study, 26.6% of women reported no prenatal care. For these women, HIV testing during delivery is the last opportunity for infants born to them. Although not as effective as when started earlier during pregnancy, clinical trials and observational studies have demonstrated that short-course interventions administered late in pregnancy can reduce MTCT,5,9 even when initiated within 48 hours after birth.22
During labor and delivery, intravenous or oral AZT is administered as pre- and post-exposure prophylaxis for the newborn. Overall, 48% of women in our study were tested during labor and 51.8% in the postpartum period. A striking difference can be noted between RJ and POA. While in POA the majority was tested during labor, in RJ most of them were tested in the postpartum. The reasons why health teams in POA were most often able to test women before delivery than in RJ are out of the scope of the present study and we could not identify an objective reason for this difference. It should be noted that POA sites started the study almost a year later than RJ sites when HIV rapid testing was already available for regular care in maternity hospitals.
One important aspect in the assessment of the use of HIV rapid testing in the delivery setting is to examine how feasible the implementation of other PMTCT interventions is when a test result is positive. In our study, intravenous AZT was administered to 73.1% of women tested before delivery. Except for one infant for whom this information was missing, all liveborn infants of women with a positive test result received oral AZT. Regimens that include only intrapartum and postpartum drug administration have been shown to be effective in reducing perinatal transmission of HIV.13,17 However, intrapartum pre-exposure prophylaxis alone with nucleoside reverse transcriptase inhibitor (NRTIs), with no prolonged post-exposure prophylaxis of the infant is not effective.17
Knowledge of the mother's HIV status provides opportunities for other effective interventions such as formula feeding. In our study, 18.3% of infants born to HIV-infected women were breastfeed at least for one day, in most cases because the mother's HIV serostatus was only determined in the postpartum. This delay in HIV diagnosis unnecessarily exposed these infants to the risk of HIV infection. Incremental risk of HIV transmission through breastfeeding has been estimated to be 14% among chronically infected women.8 Dose-response effect of breastfeeding has been demonstrated. In a study carried out by the Italian Register for HIV Infection11 in children, the adjusted infection odds ratio for one day of breastfeeding versus exclusive formula feeding was 1.19.11 The probability of HIV-1 infection per liter of breast milk ingested by an infant is 0.00064, comparable to the risk of transmission through one unprotected act of intercourse with an HIV-1-positive individual.18
Available data indicate that without intervention 25% to 30% of perinatal HIV infection occur in utero.19 In our study, ten infants were confirmed to have been infected in utero and two others had a positive HIV DNA PCR result in the 48-hour sample, but there was no subsequent sample to confirm this diagnosis. Unfortunately, for infants infected in utero, interventions provided during labor and delivery are not effective.2
The high proportion of infants lost to follow-up early in the study is a matter of concern. The fact that mothers and infants were not necessarily followed up in the same care service may have contributed to this high rate of lost to follow-up. We do not know whether these mothers and infants got the care they needed. It points out to the need to develop a better referral system for this population with tailored outreach strategies.
We found a higher prevalence of HIV infection among women enrolled in POA when compared to those in RJ. This reflects the differences on the scope, severity and dynamics of the HIV epidemic in south and southeast Brazil. A study applying spatial analysis techniques using information from AIDS case reporting database and liveborn registers found an HIV prevalence of up to 8% in some impoverished areas of POA.1
According to the Brazilian Ministry of Health data, by the end of 2002, in RJ and POA regions, 52% and 35% of HIV-infected women, respectively, were not identified during pregnancy due to a variety of factors. The population of women who were not identified with HIV during pregnancy, in POA, may comprise a higher proportion of marginalized women with lower or no access to prenatal services and highly vulnerable to HIV infection when compared to women enrolled in RJ sites. The differences found regarding social demographic data and prenatal care use seen in the study population in POA compared to those of the general female population supports this hypothesis.
One of the main strengths of our study is its large sample size that favors its comprehensiveness, in spite of being a convenience sample. The high level of HIV rapid testing acceptance among the population studied reinforces the generalization of our results on the feasibility of other PMTCT interventions in the context of HIV diagnosis made during labor and delivery. To the best of our knowledge, our study is the largest assessment conducted during labor and delivery in Brazil and, so far, the only one that assessed the feasibility of other PMTCT interventions following a positive HIV rapid test result.
Some limitations of the study should be also considered. Our findings about acceptance rates may not directly reflect other contexts, such as non-research settings. Because patient records from prenatal care are not available at maternity hospitals and HIV test results are not always recorded on prenatal cards women bring to maternity hospitals, we relied on self-reports that are potentially subject to response bias and not subject to independent verification. We also relied on self-reports for the collection of sensitive information which may result in social desirability response bias. Nonetheless, considerable validity research studies support the accuracy of self-reports in the area of sexual and reproductive health behavior.10
Although our data were generated some years ago, we believe that our results remain relevant in Brazil. In many places in Brazil, the health system continues to struggle with a variety of barriers to prevent HIV vertical transmission. According to the Brazilian Ministry of Health data, in 2008, 49.7% of HIV-infected pregnant women received intravenous ZDV during delivery.c
We should pursue the goal of providing quality prenatal to all pregnant women in Brazil, where HIV Voluntary Counseling and Testing can be performed adequately and timely. However, rapid testing during labor as well as antiretroviral prophylaxis needs to be available in all maternity hospitals 24 hours a day 7 days a week.
In conclusion, our data show high acceptance and feasibility of HIV rapid testing during labor and postpartum. Administration of antiretrovirals to mother and newborn and avoidance of breastfeeding when HIV rapid test is positive were also shown to be feasible and acceptable for these women.
Acknowledgments
Research supported by the National Institutes of Health (Grant U01 AI275) and Brazilian Ministry of Health National AIDS Program.
Footnotes
Article based on the doctoral thesis by Veloso VG presented to the Graduate Program in Public Health at Escola Nacional de Saúde Pública Sérgio Arouca, Fundação Oswaldo Cruz, in 2008.
Ministério da Saúde. Pesquisa Nacional de Demografia e da Saúde da Criança e da Mulher. Brasília; 2008.
Ministério da Saúde. Departamento de Vigilância em Saúde. Programa nacional de DST/AIDS. Recomendações para a prevenção da transmissão vertical do HIV e tratamento antiretroviral para gestantes. Brasília; 2006.
Ministério da Saúde. Sistema de Monitoramento de Indicadores do Programa Nacional de DST/Aids. Brasília; 2004[cited 2010 Jul 30]. Available from: http://www.aids.gov.br/monitoraids
The authors declare that there are no conflicts of interests.
REFERENCES
- 1.Barcellos C, Acosta LM, Lisboa EP, Brito MR, Flores R. Estimate of HIV prevalence in pregnant women by means of spatial analysis in Southern Brazil. Rev Saude Publica. 2006;40(5):928–30. doi: 10.1590/s0034-89102006000600025. DOI:10.1590/S0034-89102006005000007. [DOI] [PubMed] [Google Scholar]
- 2.Bryson Y, Luzuriaga K, Sullivan J, Wara D. Proposed definition from in utero versus intrapartum transmission of HIV-1. N Engl J Med. 1992;327(17):1246–7. doi: 10.1056/NEJM199210223271718. [DOI] [PubMed] [Google Scholar]
- 3.Bulterys M, Jamieson DJ, O'Sullivan MJ, Cohen MH, Maupin R, Nesheim S, et al. Rapid HIV-1 testing during labor: a multicenter study. JAMA. 2004;292(2):219–23. doi: 10.1001/jama.292.2.219. DOI:10.1001/jama.292.2.219. [DOI] [PubMed] [Google Scholar]
- 4.Cooper ER, Charurat M, Mofenson L, Hanson C, Pitt J, Diaz C, et al. Combination antiretroviral strategies for the treatment of pregnant HIV-1-infected women and prevention of perinatal HIV-1 transmission. J Acquir Immune Defic Syndr. 2002;29(5):484–94. doi: 10.1097/00126334-200204150-00009. [DOI] [PubMed] [Google Scholar]
- 5.Dabis F, Msellati P, Meda N, Welffens-Ekra C, You B, Manigart O, et al. 6-month efficacy, tolerance, and acceptability of a short regimen of oral zidovudine to reduce vertical transmission of HIV in breastfed children in Côte d'Ivoire and Burkina Faso: a double-blind placebo-controlled multicentre trial. DITRAME Study Group. DIminution de la Transmission Mère-Enfant. Lancet. 1999;353(9155):786–92. doi: 10.1016/s0140-6736(98)11046-2. [DOI] [PubMed] [Google Scholar]
- 6.Dao H, Mofenson LM, Ekpini R, Gilks CF, Barnhart M, Bolu O, et al. International recommendations on antiretroviral drugs for treatment of HIV-infected women and prevention of mother-to-child HIV transmission in resource-limited settings: 2006 update. Am J Obstet Gynecol. 2007;197(3 Suppl):S42–55. doi: 10.1016/j.ajog.2007.03.001. DOI:10.1016/j.ajog.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Brito AM, de Sousa JL, Luna CF, Dourado I. Trends in maternal-infant transmission of AIDS after antiretroviral therapy in Brazil. Rev Saude Publica. 2006;40(Suppl):18–22. doi: 10.1590/s0034-89102006000800004. DOI:10.1590/S0034-89102006000800004. [DOI] [PubMed] [Google Scholar]
- 8.Dunn DT, Newell ML, Ades AE, Peckham CS. Risk of human immunodeficiency virus type 1 transmission through breastfeeding. Lancet. 1992;340:585–8. doi: 10.1016/0140-6736(92)92115-v. DOI:10.1016/0140-6736(92)92115-V. [DOI] [PubMed] [Google Scholar]
- 9.Guay LA, Musoke P, Fleming T, Bagenda D, Allen M, Nakabiito C, et al. Intrapartum and neonatal single-dose nevirapine compared with zidovudine for prevention of mother to child transmission of HIV-1 in Kampala, Uganda: HIV-1NET 012 randomised trial. Lancet. 1999;354(9181):795–802. doi: 10.1016/S0140-6736(99)80008-7. [DOI] [PubMed] [Google Scholar]
- 10.Hatch MC, Misra D, Kabat GC, Kartzmer S. Proxy respondents in reproductive research: a comparison of self- and partner-reported data. Am J Epidemiol. 1991;133(8):826–31. doi: 10.1093/oxfordjournals.aje.a115962. [DOI] [PubMed] [Google Scholar]
- 11.Italian register of HIV infection in Children Human Immunodeficiency Virus type 1 infection and breast milk. Acta Paediatr Suppl. 1994;400:51–8. doi: 10.1111/j.1651-2227.1994.tb13348.x. [DOI] [PubMed] [Google Scholar]
- 12.Kissin DM, Akatova N, Rakhmanova AG, Vinogradova EN, Voronin EE, Jamieson DJ, et al. Rapid HIV testing and prevention of perinatal HIV transmission in high-risk maternity hospitals in St. Petersburg, Russia. Am J Obstet Gynecol. 2008;198(2):183–7. doi: 10.1016/j.ajog.2007.09.005. DOI:10.1016/j.ajog.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 13.Moodley D, Moodley J, Coovadia H, Gray G, McIntyre J, Hofmyer J, et al. A multicenter randomized controlled trial of nevirapine versus a combination of zidovudine and lamivudine to reduce intrapartum and early postpartum mother-to-child transmission of HIV-1. J Infect Dis. 2003;187(5):725–35. doi: 10.1086/367898. [DOI] [PubMed] [Google Scholar]
- 14.Nogueira SA, Lambert JS, Albuquerque AL, Rodrigues R, Reis S, Bornia R, et al. Assessment of a rapid HIV test strategy during labor: a pilot study from Rio de Janeiro, Brazil. J Hum Virol. 2001;4(5):278–82. [PubMed] [Google Scholar]
- 15.Pai NP, Tulsky JP, Cohan D, Colford JM, Jr, Reingold AL. Rapid point-of-care HIV testing in pregnant women: a systematic review and meta-analysis. Trop Med Int Health. 2007;12(2):162–73. doi: 10.1111/j.1365-3156.2006.01812.x. [DOI] [PubMed] [Google Scholar]
- 16.Pai NP, Barick R, Tulsky JP, Shivkumar PV, Cohan D, Kalantri S, et al. Impact of round-the-clock, rapid oral fluid HIV testing of women in labor in rural India. PLoS Med. 2008;5(5):e92. doi: 10.1371/journal.pmed.0050092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Petra Study Team Efficacy of three short-course regimens of zidovudine and lamivudine in preventing early and late transmission of HIV-1 from mother to child in Tanzania, South Africa, and Uganda (Petra study): a randomized, double-blind, placebo-controlled trial. Lancet. 2002;359(9313):1178–86. doi: 10.1016/S0140-6736(02)08214-4. DOI:10.1016/S0140-6736(02)08214-4. [DOI] [PubMed] [Google Scholar]
- 18.Richardson BA, Hughes JP. Modeling breastmilk infectivity in HIV-1 infected mothers. Biometrics. 2003;59(1):179–85. doi: 10.1111/1541-0420.00021. DOI:10.1111/1541-0420.00021. [DOI] [PubMed] [Google Scholar]
- 19.Rogers MF, Ou CY, Rayfield M, Thomas PA, Schoenbaum EE, Abrams E, et al. Use of the polymerase chain reaction for early detection of the proviral sequences of human immunodeficiency virus in infants born to seropositive mothers. New York City Collaborative Study of Maternal HIV Transmission and Montefiore Medical Center HIV Perinatal Transmission Study Group. N Engl J Med. 1989;320(25):1649–54. doi: 10.1056/NEJM198906223202503. [DOI] [PubMed] [Google Scholar]
- 20.Souza PRB, Jr, Szwarcwald CL, Barbosa A, Jr, Carvalho MF, Castilho EA. HIV infection during pregnancy: the Sentinel Surveillance Project, Brazil, 2002. Rev Saude Publica. 2004;38(6):764–72. doi: 10.1590/s0034-89102004000600003. DOI:10.1590/S0034-89102004000600003. [DOI] [PubMed] [Google Scholar]
- 21.Veloso VG, Vasconcelos AL, Grinsztejn B. Prevenção da transmissão vertical no Brasil. Bol Epidemiol AIDS. 1999;12(3):16–25. [Google Scholar]
- 22.Wade NA, Birkhead GS, Warren BL, Charbonneau TT, French PT, Wang L, et al. Abbreviated regimens of zidovudine prophylaxis and perinatal transmission of the human immunodeficiency virus. N Engl J Med. 1998;339(20):1409–14. doi: 10.1056/NEJM199811123392001. DOI:10.1056/NEJM199811123392001. [DOI] [PubMed] [Google Scholar]