Abstract
Background
The optimal treatment for Bankart lesion remains controversial. Therefore, we performed this meta-analysis to compare the clinical outcomes of patients managed with open Bankart repair versus arthroscopic Bankart repair.
Material/Methods
After systematic review of online databases, a total of 11 trials with 1022 subjects were included. The methodological quality of randomized controlled trials (RCTs) was assessed using the PEDro critical appraisal tool, and non-RCTs were evaluated by Newcastle-Ottawa (NO) quality assessment tool. Outcomes of shoulder stability, range of motion (ROM), functional scales, and surgical times were analyzed.
Results
Data synthesis showed significant differences between the two strategies, with regards to stability of the shoulder (P=0.008, RR=0.94, 95% CI: 0.89 to 0.98), and ROM (P<0.001, SMD=−0.47, 95% CI: −0.72 to −0.22).
Conclusions
Open Bankart repair produced a more stable shoulder but had a relatively poor shoulder motion, compared with arthroscopic Bankart repair, for the treatment of Bankart lesion.
MeSH Keywords: Arthroscopy, Orthopedics, Shoulder Dislocation
Background
Bankart lesion, initially reported in 1938 on a series of 27 patients with anterior shoulder instability by Bankart, is cause by the detachment of the anterior inferior labrum from the glenoid rim and in general affects people who are younger than 35 years of age. Traditional open Bankart repair (OBR) was previously considered as the accepted standard treatment for shoulder stabilization by many surgeons [1,2]. OBR has been shown to improve glenohumeral joint stability, with recurrence rates below 10% [3–5] and low failure rates varying between 0 and 11% [6–9]. However, restriction of external rotation and secondary osteoarthritis are the weakness of the open surgery.
Arthroscopic Bankart repair (ABR), first described in 1993 [10], was gradually advocated by some surgeons over the past two decades due to rapid development in arthroscopic instruments and implants and increased experience of surgeons [11–13]. Compared with open procedure, arthroscopic treatment has some advantages, such as smaller skin incisions, shorter surgical times, less postoperative pain and decreased rates of complications [14–16]. Nevertheless, some investigations reported that the patients with ABR had a higher recurrence rate compared with standard open procedure [17–19]. Moreover, arthroscopic technique requires experienced surgeons with a relatively long learning curve and expensive instruments. Up to now, newer techniques for ABR, such as suture anchor fixation, have been introduced with similar failure rates compared to traditional open procedure. However, theses available data were obtained just at short- and mid-term follow-up, instead of long-term. Therefore, there is a lack of powerful evidence to determine the preferred method between OBR and ABR for Bankart lesion.
Although several previous studies have summarized the published studies about OBR versus ABR, most of them are systematic reviews. Some authors concluded open repair has a decreased rate of recurrence; however, the others considered there are no significant differences in failure rates between OBR and ABR. Moreover, several new high-quality studies [20–24] have been recently published. Therefore, we performed this meta-analysis to determine which procedure has better clinical outcomes in the treatment of Bankart lesion.
Material and Methods
Search strategy
The search was performed in the online databases PubMed (1966 to January 2015) and EMBASE (1966 to January 2015). Only studies published in English were included. The reference lists were also checked for possible eligible article. The keywords used for retrieval were: anterior shoulder instability, Bankart lesion, dislocation, and subluxation.
Inclusion and exclusion criteria
Inclusion criteria were set as follows: 1) English literature, 2) comparison of open versus arthroscopic shoulder stabilization for Bankart lesion, 3) all included patients aged 18 years or older, 4) a minimum of 2-year follow-up, and 5) available data for recurrence, and shoulder functional scores. Exclusion criteria were: 1) non-English language literature; 2) studies with less than 2-year follow-up; 3) original data being insufficient for a meta-analysis; 4) vitro studies or non-comparable studies; 5) included patients with younger than 18 years; and 6) sample size being less than 50. To avoid repetition, if multiple articles included the same patient population, then the results were pooled.
Data extraction and evaluation of methodological quality
Data were extracted and evaluated independently by two researchers and then verified by the third senior researcher. The extracted information included: 1) the characteristics of the included studies, including the authors, the type of study design, and publication date; 2) the demographics of included subjects, including sample size, age, gender, duration of follow-up, from injury to surgery time, and the surgical details; and 3) details of outcomes. Disagreement between the authors was resolved by discussion. In cases of missing necessary data, corresponding authors the eligible trials were contacted to obtain this data. The methodological quality of each randomized controlled trial (RCT) was assessed using the Physiotherapy Evidence Database (PEDro) scale [25]. The Newcastle-Ottawa (NO) quality assessment tool [26] was used to assess the quality of each non-randomized study. The NO scales based on standard quality ratings were as follows: 1) selection of study groups; 2) comparability of study groups; and 3) ascertainment of the outcome of interest (cohort study).
Outcome measurement
The stability and range of motion (ROM) of shoulder were postoperatively applied as the primary outcome in patients with open versus arthroscopic repair for Bankart lesion. Shoulder was considered stable if recurrent dislocations and subluxations were not observed, or apprehension test was negative. The ROM mainly included loss of external rotation with the arm in 90° of abduction. Secondary outcomes under investigation included functional outcomes evaluated using the Rowe grading system [27], Constant score [28], American Shoulder and Elbow Surgeons (ASES) Scale [29], University of California Los Angeles (UCLA) shoulder rating scale [30], and surgical time.
Statistical analysis
All statistical analyses were conducted using Review Manager 5.3. Dichotomous data were analyzed by risk ratios (RR), and continuous outcomes were determined by weighted mean difference (WMD), both with 95% confidence intervals (CIs). Chi-squared test was performed to evaluate heterogeneity, which was determined to be significant at I2>50%. Funnel plot was used to evaluate publication bias. A fixed-effects model was initially employed when the heterogeneity was not significant, and a random-effects model was used if the significant heterogeneity was observed. Data not available for the meta-analysis were analyzed descriptively.
Results
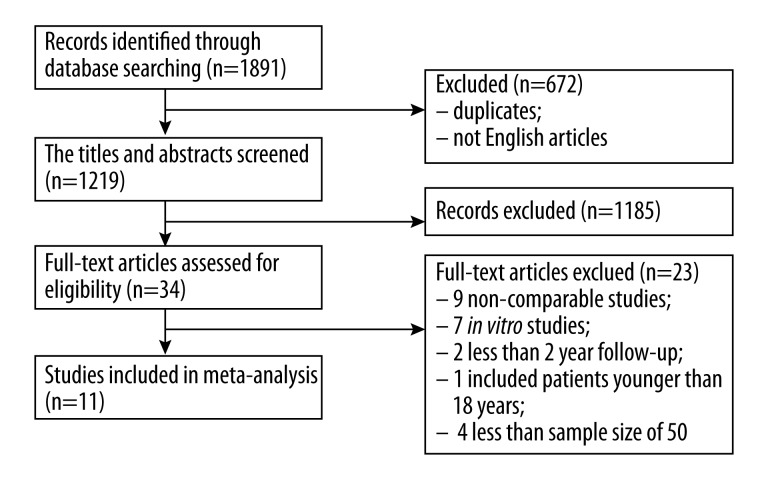
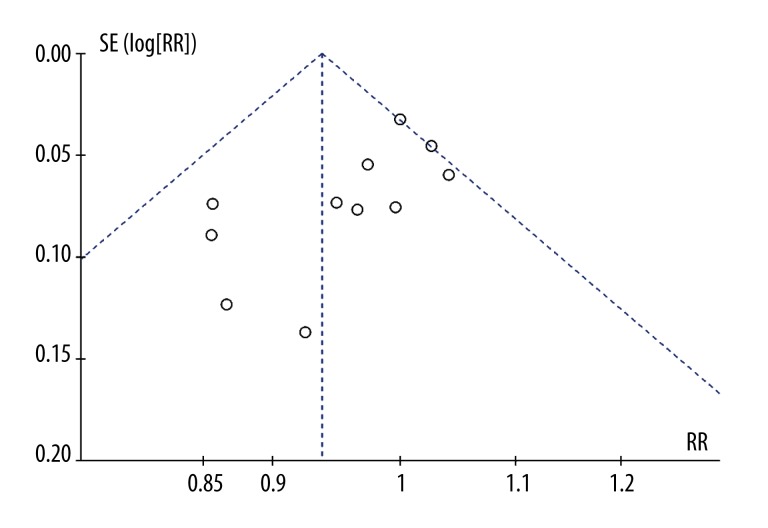
The flow diagram of the study search process is displayed in Figure 1. After full-text reviews, a total of 11 independent studies [13,20,22,31–38] were included in this meta-analysis, with a cumulative sample size of 1022 at final follow-up (Table 1). Four of all included studies [20,31–33] were RCTs and the rest [13,22,34–38] were cohort study. The pooled characteristics of the included studies are shown in Table 1. The methodological quality of RCTs is provided in Table 2. Table 3 represents the quality of the four cohort studies, as determined using the NO scale. As shown in Figure 2, publication bias was evaluated using funnel plot, which was acceptably symmetrical.
Figure 1.
Flow diagram of study selection.
Table 1.
Characteristics of studies included in this meta-analysis.
| Study | Year | Country | Design | Age (y) | Gender (M/F) | IDB | TFTTR (m) | Follow-up (m) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| As | Open | As | Open | As | Open | As | Open | As | Open | ||||
| Sperber [31] | 2001 | Sweden | Level I RCT | 25 | 27.5 | 21/9 | 19/7 | 21 (70%) | 11 (42%) | 57.6 | 42 | 24 | |
| Fabbriciani [32] | 2004 | Italy | Level I RCT | 24.5 | 26.8 | 24/6 | 26/4 | 22 (73%) | 17 (57%) | 25.3 | 20.2 | 24 | |
| Bottoni [33] | 2006 | USA | Level I RCT | 25.3 | 25.2 | 30/1 | 29/0 | 27 (87%) | 14 (48%) | 40 | 35.1 | 29.1 | 28.5 |
| Mohtadi [20] | 2014 | Canada | Level I RCT | 27.2 | 27.8 | 80/18 | 80/18 | 31 (32%) | 45 (46%) | 54 | 75 | 24 | |
| Cole [13] | 2000 | USA | Prospective | 28 | 27 | 33/4 | 18/4 | 18 (49%) | 8 (36%) | 35 | 47 | 52 | 55 |
| Karlsson [34] | 2001 | Sweden | Prospective | 26 | 27 | 45/15 | 38/10 | N/A | N/A | 31 | 42 | 28 | 36 |
| Kim [35] | 2002 | South Korea | Retrospective | 19.5 | 20.3 | 50/8 | 26/4 | N/A | N/A | 58.8 | 69.6 | 39 | |
| Tjoumakaris [36] | 2005 | USA | Retrospective | 30.8 | 28 | 48/11 | 16/8 | 34 (58%) | 12 (50%) | >12 | >12 | 40 | 56 |
| Lützner [37] | 2009 | Germany | Retrospective | 25 | 27 | 35/5 | 124/35 | 109 (55%) | 32 | 21 | 31 | ||
| Mahiroğulları [38] | 2010 | Turkey | Retrospective | 24.9 | 25.8 | 34M | 30M | 23 (68%) | 27 (90%) | 45.6 | 52.8 | 26.1 | 26.6 |
| Zaffagnini [22] | 2012 | Italy | Retrospective | 35 | 38 | N/A | N/A | 30 (61%) | 19 (58%) | N/A | N/A | 164.4 | 188.4 |
As – arthroscopic; M – male; F – female; IDB – involved dominant shoulder; TFTTR – time from trauma to repair; N/A – not applicable.
Table 2.
RCTs quality ratings (determined using the PEDro critical appraisal score).
| Sperber [31] | Fabbriciani [32] | Bottoni [33] | Mohtadi [20] | |
|---|---|---|---|---|
| Eligibility criteria | Yes | Yes | Yes | Cole |
| Random allocation | Yes | Yes | Yes | Yes |
| Concealed allocation | Yes | Yes | Yes | Yes |
| Baseline comparability | Yes | Yes | Yes | Yes |
| Blind subject | No | Yes | Yes | No |
| Blind clinician | No | No | No | Yes |
| Blind assessor | No | No | Yes | No |
| Adequate follow-up | Yes | Yes | Yes | Yes |
| Intention-to treat analysis | No | No | No | Yes |
| Between-group analysis | Yes | Yes | Yes | Yes |
| Point estimates and variability | Yes | Yes | Yes | Yes |
| Total score | 7 | 8 | 9 | 9 |
Table 3.
Cohort study quality rating (determined using the Newcastle-Ottawa scale).
| Study | Year | Selection | Comparability | Outcomes |
|---|---|---|---|---|
| Cole [13] | 2000 | **** | – | ** |
| Karlsson [34] | 2001 | **** | ** | *** |
| Kim [35] | 2002 | **** | – | *** |
| Tjoumakaris [36] | 2005 | *** | – | ** |
| Lützner [37] | 2009 | *** | * | ** |
| Mahiroğulları [38] | 2010 | *** | * | *** |
| Zaffagnini [22] | 2012 | *** | ** | *** |
Assessment strategies: selection (max. 4 stars), comparability (max. 2 stars), and outcome (max. 3 stars).
Figure 2.
Funnel plot to evaluate publication bias.
Primary outcomes
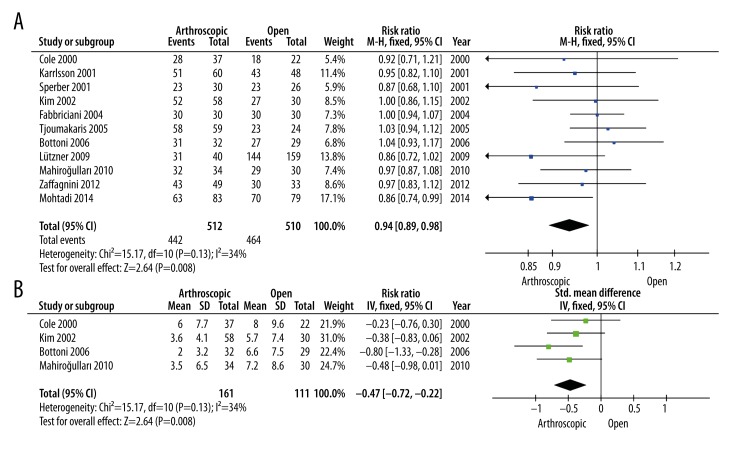
All 11 studies assessed stability of the shoulder postoperatively (Figure 3A), including 512 patients in arthroscopic group and 510 patients in open group. After meta-analysis using a fixed-effects model (I2=34%), a statistically significant difference was observed between the two treatment groups in respect to shoulder stability (P=0.008, RR=0.94, 95% CI: 0.89 to 0.98). Data on ROM were provided in four studies (Figure 3B). As one of the study’s primary outcome, the result of analysis revealed a better ROM in patients managed with arthroscopic repair, compared to those who received OBR (P<0.001, SMD=−0.47, 95% CI: −0.72 to −0.22), without significant heterogeneity.
Figure 3.
Meta-analysis on primary outcomes; (A) Forest plot to assess stability of shoulder between two treatment strategies; (B) Forest plot to assess loss of external rotation with the arm in 90° of abduction between the two treatment strategies.
Secondary outcomes
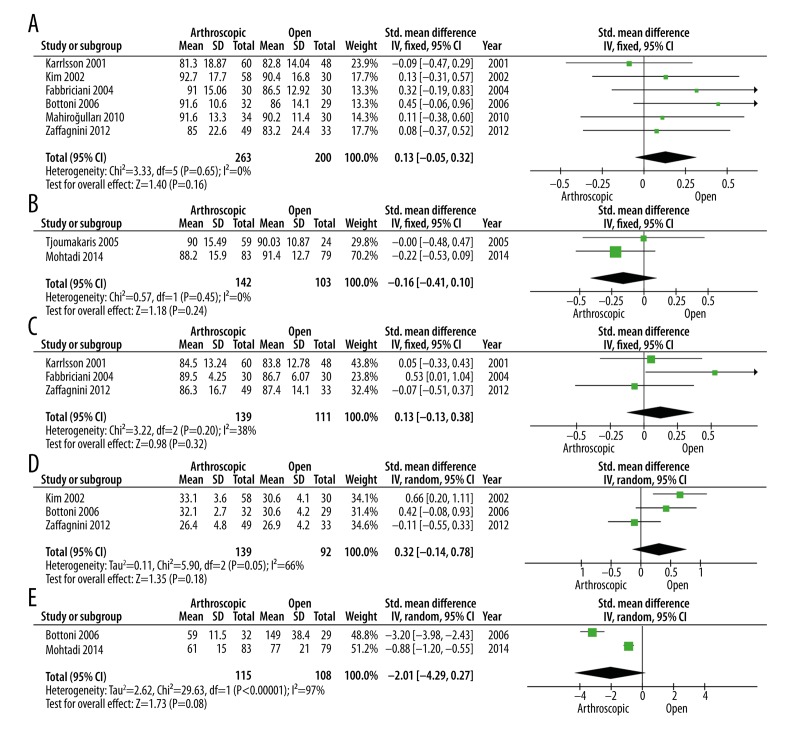
After meta-analysis on postoperatively functional outcomes, no significant differences were shown between the two treatment strategies, in terms of Rowe (P=0.16), ASES (P=0.24), Constant (P=0.32), and ULCA score (P=0.18) (Figure 4A–4D). Intraoperative surgical times were only obtained in two trials, which included 115 patients in ABR group and 108 patients in OBR group. There was no significant difference between the two groups (P=0.08, SMD=−2.01, 95% CI: −4.29 to 0.27), with a highly significant heterogeneity (I2=97%) (Figure 4E). However, there was a trend towards decreased surgical times in the arthroscopic group, compared to those who received open treatment procedure.
Figure 4.
(A) Forest plot to assess Rowe events between two treatment strategies; (B) Forest plot to assess ASES between two treatment strategies; (C) Forest plot to assess Constant score between the two treatment strategies; (D) Forest plot to assess ULCA events between the two treatment strategies; (E) Forest plot to assess surgical time events between the two treatment strategies.
Discussion
In this meta-analysis, a total of 11 studies were included and analyzed. The results showed patients who received arthroscopic procedure had an increased risk of postoperative instability and obtained a better ROM, compared with those with open repair procedure.
For the treatment of Bankart lesion, Rowe et al. [1] first introduced OBR, which was previously regarded as the criterion standard. Recently, arthroscopic techniques have been developed in order to obtain similar outcomes to open strategy without the defects associated with OBR. Arthroscopic techniques can achieve decreased pain, shorter hospital stay, improved cosmesis, and earlier return to activity [39]. However, the optimal strategy for the treatment of Bankart lesion remains controversial, based on the comparison of postoperative outcomes, especially on instability recurrence.
Hobby et al. [40] indicated similar instability recurrence between open and arthroscopic group. They also showed that patients who underwent ABR with suture anchor repair had lower instability recurrence compared to those with other arthroscopic techniques. A case-control study published by Kim et al. [35] showed no significant difference in instability recurrence between the two treatment strategies; however, arthroscopic treatment achieved a better functional result with Rowe score. Nevertheless, Mothadi et al. [41] reported the open technique obtained better outcomes in terms of recurrence and time to return to activity. After meta-analysis in the present study, the results demonstrated that patients with OBR might have more stable shoulders postoperatively but less ROM, compared with those who underwent ABR. However, the finding should be interpreted with great caution because 7 of the included studies were non-RCTs and had a relatively lower quality in contrast to RCTs. Therefore, further trials with better design are needed.
In this meta-analysis we also observed that the patients who underwent arthroscopic technique had better external rotation compared with those with OBR. This finding was similar to other studies. Fabbriciani et al. [32] reported that arthroscopic procedure led to a significantly better ROM compared with the open group, but Mohtadi et al. [20] demonstrated no significant differences in ROM between the arthroscopic-repair and the open-repair groups.
Regarding functional outcomes, we found no differences between the ABR and OBR groups, but the clinical relevance of this finding is questionable. All studies included used different functional evaluations, including Rowe score, ASES, Constant score, and ULCA. Given the variety of functional evaluations used, it is difficult show convincing results. Therefore, there is urgent need to develop a standard evaluation system that is more effective to assess shoulder function postoperatively.
Several limitations of the present meta-analysis should be mentioned. Firstly, a lack of high-level evidence on the comparison of the arthroscopic-repair and the open-repair procedures limited the strength of the meta-analysis. Only four out of all included studies were RCTs. Moreover, three out of seven cohort studies included showed poor quality based on the NO scale. Secondly, sample size of each study included was relatively small. Clinical heterogeneity might be inevitable due to the various surgical indications and the difference of experience of each surgeon. Finally, the shortage of a standard evaluation system might have a limit the strength of the evidence.
Conclusions
In summary, more stable shoulders but relatively poor shoulder motions were observed in the OBR group compared with the ABR group for the treatment of Bankart lesion. Furthermore, further trials including a larger number of patients and a better-designed method are urgently needed.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Source of support: Self financing
References
- 1.Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60(1):1–16. [PubMed] [Google Scholar]
- 2.Rowe CR, Zarins B, Ciullo JV. Recurrent anterior dislocation of the shoulder after surgical repair. Apparent causes of failure and treatment. J Bone Joint Surg Am. 1984;66(2):159–68. [PubMed] [Google Scholar]
- 3.Hovelius L, Thorling J, Fredin H. Recurrent anterior dislocation of the shoulder. Results after the Bankart and Putti-Platt operations. J Bone Joint Surg Am. 1979;61(4):566–69. [PubMed] [Google Scholar]
- 4.Morrey BF, Janes JM. Recurrent anterior dislocation of the shoulder. Long-term follow-up of the Putti-Platt and Bankart procedures. J Bone Joint Surg Am. 1976;58(2):252–56. [PubMed] [Google Scholar]
- 5.Walch G, Boileau P, Levigne C, et al. Arthroscopic stabilization for recurrent anterior shoulder dislocation: results of 59 cases. Arthroscopy. 1995;11(2):173–79. doi: 10.1016/0749-8063(95)90063-2. [DOI] [PubMed] [Google Scholar]
- 6.Freedman KB, Smith AP, Romeo AA, et al. Open Bankart repair versus arthroscopic repair with transglenoid sutures or bioabsorbable tacks for Recurrent Anterior instability of the shoulder: a meta-analysis. Am J Sports Med. 2004;32(6):1520–27. doi: 10.1177/0363546504265188. [DOI] [PubMed] [Google Scholar]
- 7.Jolles BM, Pelet S, Farron A. Traumatic recurrent anterior dislocation of the shoulder: two- to four-year follow-up of an anatomic open procedure. J Shoulder Elbow Surg. 2004;13(1):30–34. doi: 10.1016/j.jse.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Pagnani MJ, Dome DC. Surgical treatment of traumatic anterior shoulder instability in american football players. J Bone Joint Surg Am. 2002;84-A(5):711–15. doi: 10.2106/00004623-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Uhorchak JM, Arciero RA, Huggard D, Taylor DC. Recurrent shoulder instability after open reconstruction in athletes involved in collision and contact sports. Am J Sports Med. 2000;28(6):794–99. doi: 10.1177/03635465000280060501. [DOI] [PubMed] [Google Scholar]
- 10.el Akad AM, Winge S, Molinari M, Eriksson E. Arthroscopic Bankart procedures for anterior shoulder instability. A review of the literature. Knee Surg Sports Traumatol Arthrosc. 1993;1(2):113–22. doi: 10.1007/BF01565465. [DOI] [PubMed] [Google Scholar]
- 11.Green MR, Christensen KP. Arthroscopic versus open Bankart procedures: a comparison of early morbidity and complications. Arthroscopy. 1993;9(4):371–74. doi: 10.1016/s0749-8063(05)80308-1. [DOI] [PubMed] [Google Scholar]
- 12.Speer KP, Deng X, Borrero S, et al. Biomechanical evaluation of a simulated Bankart lesion. J Bone Joint Surg Am. 1994;76(12):1819–26. doi: 10.2106/00004623-199412000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Cole BJ, L’Insalata J, Irrgang J, Warner JJ. Comparison of arthroscopic and open anterior shoulder stabilization. A two to six-year follow-up study. J Bone Joint Surg Am. 2000;82-A(8):1108–14. doi: 10.2106/00004623-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Arciero RA, Taylor DC, Snyder RJ, Uhorchak JM. Arthroscopic bioabsorbable tack stabilization of initial anterior shoulder dislocations: a preliminary report. Arthroscopy. 1995;11(4):410–17. doi: 10.1016/0749-8063(95)90192-2. [DOI] [PubMed] [Google Scholar]
- 15.Bacilla P, Field LD, Savoie FH., III Arthroscopic Bankart repair in a high demand patient population. Arthroscopy. 1997;13(1):51–60. doi: 10.1016/s0749-8063(97)90209-7. [DOI] [PubMed] [Google Scholar]
- 16.Kartus J, Ejerhed L, Funck E, et al. Arthroscopic and open shoulder stabilization using absorbable implants. A clinical and radiographic comparison of two methods. Knee Surgery Sports Traumatol Arthrosc. 1998;6(3):181–88. doi: 10.1007/s001670050096. [DOI] [PubMed] [Google Scholar]
- 17.Hawkins RB. Arthroscopic stapling repair for shoulder instability: a retrospective study of 50 cases. Arthroscopy. 1989;5(2):122–28. doi: 10.1016/0749-8063(89)90007-8. [DOI] [PubMed] [Google Scholar]
- 18.Guanche CA, Quick DC, Sodergren KM, Buss DD. Arthroscopic versus open reconstruction of the shoulder in patients with isolated Bankart lesions. Am J Sports Med. 1996;24(2):144–48. doi: 10.1177/036354659602400204. [DOI] [PubMed] [Google Scholar]
- 19.Geiger DF, Hurley JA, Tovey JA, Rao JP. Results of arthroscopic versus open Bankart suture repair. Clin Orthop Relat Res. 1997;(337):111–17. doi: 10.1097/00003086-199704000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Mohtadi NG, Chan DS, Hollinshead RM, et al. A randomized clinical trial comparing open and arthroscopic stabilization for recurrent traumatic anterior shoulder instability: two-year follow-up with disease-specific quality-of-life outcomes. J Bone Joint Surg Am. 2014;96(5):353–60. doi: 10.2106/JBJS.L.01656. [DOI] [PubMed] [Google Scholar]
- 21.Archetti Netto N, Tamaoki MJ, Lenza M, et al. Treatment of Bankart lesions in traumatic anterior instability of the shoulder: a randomized controlled trial comparing arthroscopy and open techniques. Arthroscopy. 2012;28(7):900–8. doi: 10.1016/j.arthro.2011.11.032. [DOI] [PubMed] [Google Scholar]
- 22.Zaffagnini S, Marcheggiani Muccioli GM, Giordano G, et al. Long-term outcomes after repair of recurrent post-traumatic anterior shoulder instability: comparison of arthroscopic transglenoid suture and open Bankart reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):816–21. doi: 10.1007/s00167-011-1674-y. [DOI] [PubMed] [Google Scholar]
- 23.Bessiere C, Trojani C, Pelegri C, et al. Coracoid bone block versus arthroscopic Bankart repair: a comparative paired study with 5-year follow-up. Orthop Traumatol Surg Res. 2013;99(2):123–30. doi: 10.1016/j.otsr.2012.12.010. [DOI] [PubMed] [Google Scholar]
- 24.Shymon SJ, Roocroft J, Edmonds EW. Traumatic anterior instability of the pediatric shoulder: a comparison of arthroscopic and open bankart repairs. J Pediatric Orthop. 2015;35(1):1–6. doi: 10.1097/BPO.0000000000000215. [DOI] [PubMed] [Google Scholar]
- 25.Maher CG, Sherrington C, Herbert RD, et al. Reliability of the PEDro scale for rating quality of randomized controlled trials. Physical Therapy. 2003;83(8):713–21. [PubMed] [Google Scholar]
- 26.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25(9):603–5. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 27.Jobe FW, Giangarra CE, Kvitne RS, Glousman RE. Anterior capsulolabral reconstruction of the shoulder in athletes in overhand sports. Am J Sports Med. 1991;19(5):428–34. doi: 10.1177/036354659101900502. [DOI] [PubMed] [Google Scholar]
- 28.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160–64. [PubMed] [Google Scholar]
- 29.Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347–52. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 30.Ellman H, Hanker G, Bayer M. Repair of the rotator cuff. End-result study of factors influencing reconstruction. J Bone Joint Surg Am. 1986;68(8):1136–44. [PubMed] [Google Scholar]
- 31.Sperber A, Hamberg P, Karlsson J, Sward L, Wredmark T. Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study. J Shoulder Elbow Surg. 2001;10(2):105–8. doi: 10.1067/mse.2001.112019. [DOI] [PubMed] [Google Scholar]
- 32.Fabbriciani C, Milano G, Demontis A, et al. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy. 2004;20(5):456–62. doi: 10.1016/j.arthro.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 33.Bottoni CR, Smith EL, Berkowitz MJ, et al. Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. Am J Sports Med. 2006;34(11):1730–37. doi: 10.1177/0363546506288239. [DOI] [PubMed] [Google Scholar]
- 34.Karlsson J, Magnusson L, Ejerhed L, et al. Comparison of open and arthroscopic stabilization for recurrent shoulder dislocation in patients with a Bankart lesion. Am J Sports Med. 2001;29(5):538–42. doi: 10.1177/03635465010290050201. [DOI] [PubMed] [Google Scholar]
- 35.Kim SH, Ha KI, Kim SH. Bankart repair in traumatic anterior shoulder instability: open versus arthroscopic technique. Arthroscopy. 2002;18(7):755–63. doi: 10.1053/jars.2002.31701. [DOI] [PubMed] [Google Scholar]
- 36.Tjoumakaris FP, Abboud JA, Hasan SA, et al. Arthroscopic and open Bankart repairs provide similar outcomes. Clin Orthop Relat Res. 2006;446:227–32. doi: 10.1097/01.blo.0000205883.73705.19. [DOI] [PubMed] [Google Scholar]
- 37.Lutzner J, Krummenauer F, Lubke J, et al. Fuctional outcome after open and arthroscopic bankart repair for traumatic shoulder instability. Eur J Med Res. 2009;14(1):18–24. doi: 10.1186/2047-783X-14-1-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mahirogullari M, Ozkan H, Akyuz M, et al. Comparison between the results of open and arthroscopic repair of isolated traumatic anterior instability of the shoulder. Acta Orthop Traumatol Turc. 2010;44(3):180–85. doi: 10.3944/AOTT.2010.2289. [DOI] [PubMed] [Google Scholar]
- 39.Doshi D, Firke R. A new patient-controlled technique for shoulder relocation in emergency departments. Am J Case Rep. 2014;15:485–87. doi: 10.12659/AJCR.891269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hobby J, Griffin D, Dunbar M, Boileau P. Is arthroscopic surgery for stabilisation of chronic shoulder instability as effective as open surgery? A systematic review and meta-analysis of 62 studies including 3044 arthroscopic operations. J Bone Joint Surg Br. 2007;89(9):1188–96. doi: 10.1302/0301-620X.89B9.18467. [DOI] [PubMed] [Google Scholar]
- 41.Mohtadi NG, Bitar IJ, Sasyniuk TM, et al. Arthroscopic versus open repair for traumatic anterior shoulder instability: a meta-analysis. Arthroscopy. 2005;21(6):652–58. doi: 10.1016/j.arthro.2005.02.021. [DOI] [PubMed] [Google Scholar]