Abstract
Background
One of the effects of diabetes mellitus (DM), peripheral neuropathy, affects the sensation in the feet and can increase the chance of falling. The purpose of the study was to investigate the effect of 8 weeks of Tai Chi (TC) training combined with mental imagery (MI) on improving balance in people with diabetes and an age matched control group.
Material/Methods
Seventeen healthy subjects and 12 diabetic sedentary subjects ranging from 40–80 years of age were recruited. All subjects in both groups attended a Yang style of TC class using MI strategies, 2 sessions a week for 8 weeks. Each session was one hour long. Measures were taken using a balance platform test, an Activities-specific Balance Confidence (ABC) Scale, a one leg standing test (OLS), functional reach test (FRT) and hemoglobin A1C. These measures were taken twice, pre and post-study, for both groups.
Results
Both groups experienced significant improvements in ABC, OLS, FRT (P<0.01) after completing 8 weeks of TC exercise with no significant improvement between groups. Subjects using the balance platform test demonstrated improvement in balance in all different tasks with no significant change between groups. There was no significant change in HbA1C for the diabetic group.
Conclusions
All results showed an improvement in balance in the diabetic and the control groups; however, no significant difference between the groups was observed. Since the DM group had more problems with balance impairment at baseline than the control, the diabetic group showed the most benefit from the TC exercise.
MeSH Keywords: Aging, Diabetic Neuropathies, Exercise, Postural Balance
Background
Diabetes mellitus (DM) is a silent systematic disease that threatens world health [1]. It can be present for a few years with no symptoms, and most people do not know that they have the disease until they experience complications or advanced symptoms [1]. In addition, most people with DM do not notice the onset of symptoms such as frequent urination or extreme thirst because these symptoms increase gradually over a period of years, making it difficult for patients to notice the changes [2]. According to the World Health Organization (WHO), more than 347 million people worldwide have diabetes, and prevalence will increase to double or even triple that number by the year 2030 [1]. One of the effects of DM, peripheral neuropathy, affects the feet sensation which can increase the chance of falling [3].
The central nervous system integrates the afferent information from the vestibular, visual and somatosensory systems to control balance [3–5]. The autonomic nervous system maintains blood flow for proper muscle and organ function [6]. During activities that require balance, blood flow increases to help the somatic and central nervous systems to control balance by providing sufficient blood flow to somatosensory organs [7–9]. The combination of aging and living with DM can impair blood flow to tissues. This, in turn, can reduce the effectiveness of all three balance system components and, as a consequence, lead to impaired somatosensory sensation, proprioception (vestibular system) and vision [3–5]. After a few years, a patient’s muscles become weaker, reducing their ability to maintain their center of gravity in a stable position over their base of support without falling [10]. As somatosensory information from the foot and ankle is affected, it causes postural instability, leading to foot injuries, foot ulcers, and possibly lower limb extremity amputation [1]. It has been estimated that more than 60% of non-traumatic lower-limb amputations are related to DM [5,11]. Falling is an expected result of postural instability and considered a major problem in older people and people with DM. Studies have shown that balance training such as Tai Chi (TC) exercise can improve postural stability [12–21]. Other studies have shown an increase in balance with mental imagery (MI) [22,23].
Tai Chi, as a traditional exercise regimen, has been practiced in China to improve balance and postural control. It is called a body-mind technique because the person uses his or her mind while accomplishing the exercise [24]. TC is a combination exercise involving weight shifting, postural alignment, and slow coordinated movements with synchronized deep breathing. This combination involves many different mental and physical elements, such as calm concentration on the movement, following the instructor’s example to achieve the proper form to improve muscle elasticity, while tying the movement to deep breathing in order to enhance cardiac output and support the muscles with adequate blood flow [25,26].
Tai Chi differs from other forms of exercise such as running, because the complex series of movements requires the individual to concentrate while performing each movement. Concentration during repetitive tasks aids in the learning process, especially in the damaged nervous system [27]. In many patients with diabetes, the feet provide false (signal) information to the brain about ground reaction forces due to impaired sensory function [28]. In TC, subjects move slowly, visualizing the movement while concentrating on how each movement feels; this helps people to become more aware of sensation. Previous studies have supported the role of MI in terms of re-learning or re-conditioning [29,30].
Many studies have shown that TC has positive results in elderly people in terms of minimizing the chance of falls and improving balance [12–16,31–35], proprioception [25,36], circulation [17,37] and blood pressure [18]. In a majority of the studies, program interventions were lengthy, varying between 4 months to 5 years [12–14,16,19–21,25,34,36,38,39]. Shorter periods of Tai Chi have been shown to have benefits in stroke patients, Parkinson’s disease and cardiovascular disease [40–43]. No reports have examined the effect of Tai Chi for short periods (less than 4 months) in people with diabetes. Diabetes is of interest in that it is characterized by enhanced loss in sensation, balance and motor control leading to more reliance on the visual system. Therefore, Tai Chi may be more effective if it includes more visual cues to help this population.
Motor or mental imagery (MI) is defined as “the mental representation of movement without any movement” [29]. It is a process of imagining an action without executing it. The subject relies on memory to understand the process of the action. During mental practice, the subject repeats the imagined acts to improve the actual performance of the movement [29]. The combination of physical and mental practice helps to restore successful movement. In this process, the person mentally and explicitly rehearses the sequence of movements required while doing the task. The focus and planning increases awareness of the required task [29,30,44].
The purpose of this study was to investigate the effect of 8 weeks of TC training, combined with mental imagery, on improving balance in people with diabetes and an age matched control group. This is unique in that no one has combined TC with MI, a logical conclusion for people with somatosensory and vestibular impairments. In this study, it was hypothesized that focusing on MI strategies during exercise with TC would help in optimizing and improving balance and sensation in a shorter treatment time in people with diabetes compared to age matched controls.
Material and Methods
Subjects
Subjects 40 to 80 years of age were recruited. The following inclusion/exclusion criteria were used to determine eligibility for enrollment in the study. Inclusion criteria included: 1) had not practiced TC in the last 4 months; 2) did not exercise more than once per week; 3) body mass index (BMI) between 10 and 35 Kg/m2; 4) normal or controlled blood pressure; and 5) normal range of motion, at least 5/5 muscle power bilateral. Subjects were excluded if they: 1) took medications which could affect balance; 2) had a history of frequent falling; 3) had vision problems; and 4) had orthopedic/ neuromuscular/ cardiovascular impairments that restricted exercise.
A convenience sample of 40 subjects, 20 of them diagnosed with Type 2 diabetes and 20 subjects who were in the control group. Eleven subjects withdrew due to conflicts with the TC class schedule. Data analysis was based on the remaining 29 subjects who completed the study. Twelve were diagnosed with Type 2 and 17 were in the control group.
Measurements
The following tools were used as valid and reliable clinical measures of balance that have been used in many studies.
Balance platform test
The balance platform used in this study was developed by Petrofsky et al. (2009) and has been validated in a previous study [45]. This device consisted of four stainless steel bars mounted at four corners of the platform (TML Strain Gauge FLA-6, 350-17, Tokyo, Japan). The output of the strain gauge bridge was amplified by four BioPac 100C low-level bio-potential amplifiers and recorded on a BioPac MP 150 system through a 24-bit A/D converter. The sampling rate was 2000 samples per second.
During the test, a gait belt was placed around the subject’s waist as a safety precaution and a researcher remained nearby to prevent falls. Each subject stood over the platform while performing eight different tasks, or positions. Each position was executed with eyes opened and closed. At the beginning, the subject was asked to keep their eyes fixed on a target on the wall, with arms crossed on the chest and standing quietly on the platform with feet apart for 10 seconds. The center of mass provided weight distribution among the four sensors. The device recorded sway. The subjects were asked to perform the eight tasks in random order for 10 seconds each with one minute rest time between each task. The eight tasks were: 1) Feet apart, eyes opened and firm surface (this task used as referent for each subject); 2) Feet apart, eyes closed and firm surface (FAEC-FIRM); 3) Tandem standing, eyes opened and firm surface (TEO-FIRM); 4) Tandem standing, eyes closed and firm surface (TEC-FIRM); 5) Feet apart, eyes opened and foam surface (FAEO-FOAM); 6) Feet apart, eyes closed and foam surface (FAEC-FOAM); 7) Tandem standing, eyes opened and foam surface TEC-FOAM); and 8) Tandem standing, eyes closed and foam surface (TEC-FOAM). The basic task was to stand with feet apart on a firm surface with eyes open. For each subject, this task was used as referent for all tasks. This test was used to alter and challenge different sensory systems. In this study, three factors were used, both singly and in combination, to investigate the effect on balance. These factors were base of support, surface challenge, and vision. The mean coefficient variation was calculated to compare pre- and post-test results using the basic task as a referent for each subject.
The Activities-specific Balance Confidence (ABC) Scale
Subjects completed the 16-item Activities-specific Balance Confidence (ABC) scale [46] that subjectively quantifies patient confidence when performing mobility tasks. Among the elderly, researchers demonstrated that the ABC scale has excellent test-retest reliability)r=0.92, p<0.001) [46]. Furthermore, a previous study had shown that the ABC scale has adequate criteria and construct validity [47]. The ABC score was calculated as following:
Function reach test (FRT)
The FRT was used to assess dynamic balance [48]. A yardstick was placed on the wall at shoulder level and the subjects were asked to stand with their dominant shoulder next to the wall without touching or leaning on the wall and then elevate their arm to 90 degrees of shoulder flexion parallel to the wall. The investigator recorded the starting position at the distal end of the third metacarpal head on the yardstick. The subject then was asked to reach forward as much as possible without taking a step forward, and the maximum reaching point was recorded. The investigator demonstrated the task and asked the subject repeat to it as to ensure that the subject performed the test correctly. The subject performed the task three times and the average was recorded. The FRT has excellent test retest reliability (ICC=0.92) and inter rater reliability (ICC=0.98) [48]. Previous studies indicated that FRT has good criterion validity [49,50] and responsiveness [51].
One leg standing test (OLS)
This test was performed to assess static balance [52,53]. The subject was asked to stand on one leg with eyes open and arms on the hips. The length of time was recorded from when the patient’s foot was off the floor until it touched the floor again. The investigator demonstrated the task and asked the subject to repeat it. The subject then performed the task three times and the average was recorded. Researchers have found that the OLS has a good interclass correlation coefficient (ICC range=0.95 to 0.099) and within the rater interclass correlation coefficient (ICC=0.73 to 0.93) [54].
The HemoglobinA1C test for diabetic group
The Hemoglobin A1C (HbA1C), a blood test which measures the average concentration of blood glucose over a 3-month period, is the most common outcome measure for glucose control [55,56]. Approximately 5 μL of blood (from finger stick) was obtained and used to measure the HbA1C level with a Food and Drug Administration (FDA) approved device called the DCV Vantage analyzer (SIEMENS®, Tarrytown, NY, USA).
Intervention (Tai Chi exercise combined with Mental Imaginary)
All subjects in both groups underwent the same TC exercise program. A certified TC instructor handled the class for the whole program. TC has many styles, and we found that the Yang style was the most appropriate because it had the important characteristics relevant to MI and somatosensory enhancement. These characteristics included slow coordinated movement, weight shifting with wide steps, a one-leg stance, stretching, and mental concentration. The exercise was conducted over a thick mat and with shoes off for greater sensory enhancement and challenge as indicated in previous studies [57,58]. In this study, we used MI strategies, for example, subjects were asked to concentrate on sequence of each movement in TC. Also, they were asked to mentor the exercise visually from the TC instructor before they executed any movement. Then, they were instructed to do and feel the movement sequence while they visually were watching themselves in the front of the mirror with supervision from the instructor to correct any movement if needed to achieve better outcomes as reported in a previous study [59].
Procedures
After screening for inclusion and exclusion criteria, subjects were provided with detailed information regarding the purpose of the study, procedures and tests, potential risks and scheduled time of the TC exercise. If the subject agreed to proceed, he/she signed the informed consent form as approved by Institutional Review Board (IRB) at Loma Linda University before proceeding to testing and taking measurements.
A researcher took all subject measurements. Baseline measurements were taken to assess balance using the following tools: 1) balance platform test; 2) the activities-specific balance confidence (ABC) Scale, 3) one leg standing test (OLS), and 4) function reach test (FRT). In addition, HbA1C blood test was done for the diabetic group only.
Subjects participated in 1 hour sessions, 2 times a week for 8 weeks. Each session consisted of 15 minutes of warming-up exercises, including stretching, loosening the muscles, and breathing exercises, and followed by 45 minutes of TC exercise, Yang style. All subjects had the same type intervention of TC exercise. The first test was conducted during the informed consent process, and then outcome measures taken after the subjects completed the 8-week TC exercise intervention. The measurements took around 2–3 hours to complete each measure.
Data analysis
Data were analyzed using SPSS 22.0 (IBM, Armonk, NY). The demographic characteristics of the subjects were compared between the diabetic and control groups using independent t-test for the quantitative variables and Chi-square for independence for categorical variables. The normality of the outcome variables at baseline and post intervention was examined using One-sample Kolmogorov-Smirnov test. Since the distribution of these variables was not approximately normal, the baseline scores and differences between post and pre measures for ABC, FRT and OLS were compared between the two groups using Mann-Whitney U test. In each study group, comparisons between post and pre measures after the TC exercise were assessed using the Wilcoxon Signed rank test. For the different balance tasks, changes between post and pre measures were examined using paired t-test and between diabetic and control groups using an independent t-test. The level of significance was set at p≤0.05.
Results
Twenty nine subjects completed the study, 12 (41.4%) diabetics and 17 (58.6%) controls. The distribution of age, gender, and BMI were similar in both study groups. Among subjects with diabetes, the average duration of the disease was 10.8±5.4 years with a mean HbA1C of 6.8±0.8 (Table 1).
Table 1.
Demographic characteristics of participants (N=29).
| Characteristic | Diabetic (n=12) | Control (n=17) | P valuea | ||
|---|---|---|---|---|---|
| Mean (SD) | n (%) | Mean (SD) | n (%) | ||
| Age (years) | 63.8 (8.1) | 63.6 (6.5) | 0.91 | ||
| Gender (female)b | 8 (66.7) | 13 (76.5) | 0.43 | ||
| Weight (Kg) | 86.8 (17.2) | 77.4 (17.4) | 0.16 | ||
| Height (m) | 1.8 (0.1) | 1.7 (0.1) | <0.01 | ||
| BMI (Kg/m2) | 27.9 (5.5) | 27.1 (4.3) | 0.66 | ||
| Duration of diabetes (years) | 10.8 (5.4) | ||||
| A1C at baseline | 6.8 (0.8) | ||||
SD – standard deviations; BMI – body mass index.
P value from Independent t-test;
Chi square.
The mean ABC score improved significantly in both groups. Among subjects with diabetes, the average dropped from17.7±3.3 to 6.5±1.3 (p<0.01) and from 7.5±2.8 to 3.5±1.1 in the healthy controls (p<0.01). However, there was no significant difference between the two groups (p=0.17). Similar findings were observed for the functional reach test and the one leg standing test. In the diabetic group, the mean FRT distance increased from11.2±0.5 to 12.8±0.6 inches (p<0.001) and from 11.7±0.4 to 13.3±0.5 inches in the controls (p<0.01) and this difference was not significant between the two study groups (p=0.91). Also, the mean one leg standing score increased from 29.8±12.3 to 48.5±17.3 (p<0.01) and from 44.4±10.4 to 80.5±14.6 in the healthy controls (p<0.01) and this improvement was not significantly different between the two groups (p=0.17; Table 2). In the diabetic group, there was no significant difference between HbA1C at baseline and after 8 weeks of TC training (6.8±0.8 to 7.0±1.4, p=0.50).
Table 2.
Changes in ABC, functional reach test and one leg standing test in diabetic (n=12) and control (n=17) subjects.
| Tool | Group | Mean (SE) | Pre-post P valuea | Between Group P valueb | |
|---|---|---|---|---|---|
| ABC | Diabetic | Pre | 17.7 (3.3) | <0.01 | 0.17 |
| Post | 6.5 (1.3) | ||||
| Control | Pre | 7.5 (2.8) | <0.01 | ||
| Post | 3.6 (1.1) | ||||
| Functional Reach Test | Diabetic | Pre | 11.2 (0.5) | <0.001 | 0.91 |
| Post | 12.8 (0.6) | ||||
| Control | Pre | 11.7 (0.4) | <0.01 | ||
| Post | 13.3 (0.5) | ||||
| One Leg Standing Test | Diabetic | Pre | 29.8 (12.4) | <0.01 | 0.17 |
| Post | 48.5 (17.4) | ||||
| Control | Pre | 44.4 (10.4) | <0.01 | ||
| Post | 80.5 (14.6) | ||||
SE – standard error;
P value from Wilcoxon Signed Rank Test;
P value from Mann-Whitney U Test.
Both groups had balance improvements for the various tasks of balance platform; however, this improvement did not differ between groups (Figures 1, 2). Both groups experienced significant improvement for the following tasks in stations TEO-FIRM, FAEC-FOAM and TEC-FOAM.
Figure 1.
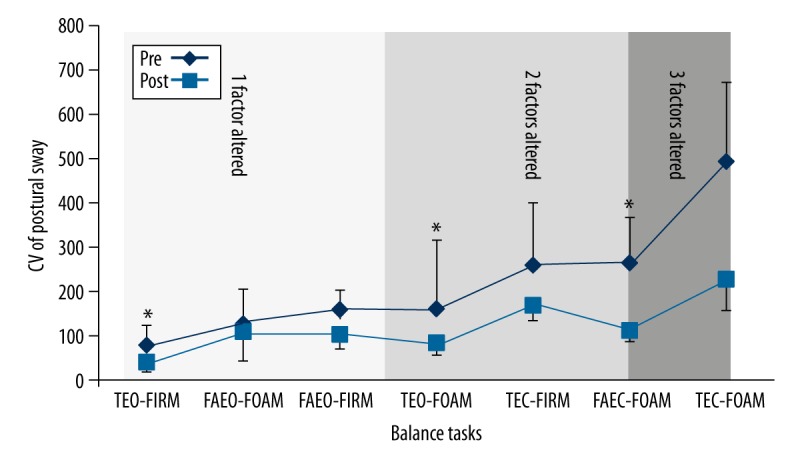
Mean ± standard error of postural sway (Coefficient of Variation of the postural sway) in diabetic group. * Significant difference between pre and post exercise.
Figure 2.
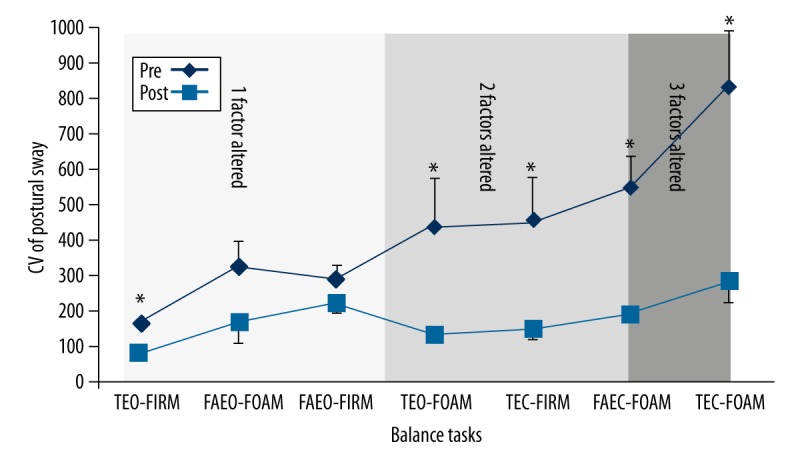
Mean ± standard error of postural sway (Coefficient of Variation of the postural sway) in control group. * Significant difference between pre and post exercise.
Discussion
Fear of falling and impaired balance are two of the complications of diabetes and aging. Reflexes are generally more sluggish with older people and people with diabetics. Loss in balance occurs slowly over years. Falls increase medical costs in the elderly [60].
The primary purpose of this prospective clinical study was to examine the effect of 8 weeks of TC exercise plus mental imagery in improving balance in a diabetic group compared to age matched controls. To our knowledge, this was the first study using TC that focused on MI to get the maximum benefit of 8 weeks of exercise. Other studies have examined both short intense daily basis of TC [31,33,61] and long term effects of TC [12–14,16,19–21,25,34,36,38,39] but none have added MI.
In this study, it was hypothesized that TC exercise combined with focusing on MI would improve balance control and confidence from fear of falling. Diabetes and aging may lead to some impairment in the sensory input in the foot, which increases the risk of falling [3–5]. Combining TC exercise and MI used for applying the concept of “re-learning” enhanced the somatosensory system and helped restore some functions lost due to aging and/or diabetes such as increased balance and reduced fear of falling.
These findings were in line with other clinical studies which concluded that TC exercise improves balance and function. The intervention program for those studies was longer than 8 weeks [12–16,19–21,34,36,38,39] or for a more intensive daily course [31,33,61]. This study was only two times a week for 8 weeks. Comparing Tai Chi used in other studies alone on people with diabetes for 4 months, there was an increase of 47% in one leg stance time in one study [62]. In the present investigation a 63% increase was seen in just 8 weeks, half the time and better increase in balance. In another study in people with diabetes by Ahn, with 12 weeks of tai chi on people with type 2 diabetes, the one leg stance time was improved by about 25% [63]. Thus while many of the parameters were not the same in different studies on people with diabetes, the use of MI seems to have increased the recovery of balance and fear of falling better than Tai Chi alone.
The results of this study indicated that both groups achieved significant improvement in balance in 8 weeks. The improvement in both groups was similar but considered more beneficial to the diabetic group as this group had more balance impairment at baseline. The findings of this clinical trial were consistent with other studies which reported improving balance in a longer term of intervention of TC exercise with different populations [12–21]. The results of this study supported this short term program in improving balance. Practicing TC in the long term induced some changes in the brain structure (brain morphometry) [64]. This reveals the effect of MI in changing brain structure.
The ABC scale was calculated as the percent change, meaning a smaller percent indicates more improvement. In this study, a comparison between the two study groups at baseline indicated that the diabetic group had more balance impairment. However, both groups improved significantly, with no difference between groups. For the FRT test, the baseline measurements were similar with significant improvement in both groups. However, this change was not significantly different between groups.
For the OLS, the baseline time was less in the diabetes group compared to the control group. However, the improvement was significant in both groups. This result was consistent with the other balance outcome measures in this study that showed the diabetic group saw more improvement because their impairment was more significant at baseline.
Similarly, the results of all tasks using the balance platform improved in both groups with no significant difference between groups. This indicates that TC exercise was beneficial for both groups. The three- altered sensory factors together (TEC-FOAM) showed significant improvement in both groups. It is the most difficult of the tests and alters 3 conditions during attempted balance as has been well documented [65].
Based on this study’s findings, physical therapists are encouraged to recommend TC exercise for diabetic and geriatric patients. The results of this study suggested that teaching the patient to focus on mental theory while doing TC exercise is the best way to promote and accelerate the “re-learning” process in order to improve balance.
The strengths of this study include duration, intensity of the exercise, and use of MI to accelerate the “re-learning” process and improve function. The findings of this study showed an improvement at 8 weeks with mild intensity TC exercise (1 hour/2 times/week) while most studies used similar or longer duration interventions more intense daily programs. One limitation of the study was that measurements were not taken at the mid-point (4 weeks) to check the subjects’ progress.
Conclusions
This clinical trial supported the effectiveness of TC exercise combed with MI in improving balance in 8 weeks for diabetic and control groups. However, since the level of impairment was higher in the diabetic group at baseline, TC exercise was more beneficial for the diabetic group compared to the control group, which is related to the disease pathology.
Acknowledgments
We would like to thank the TC instructor Mr. Harvey Kurland and his assistant Ms. Myra Allen for handling the TC class during the study in a professional manner.
Footnotes
Source of support: Departmental sources
References
- 1.World Health Organization, Facts Sheets. 2015. Jan, 2015 [cited 2015 1/25]; Available from: http://www.who.int/mediacentre/factsheets/fs312/en/
- 2.Resnick HE, Stansberry KB, Harris TB, et al. Diabetes, peripheral neuropathy, and old age disability. Muscle Nerve. 2002;25(1):43–50. doi: 10.1002/mus.1217. [DOI] [PubMed] [Google Scholar]
- 3.van Deursen RW, Simoneau GG. Foot and ankle sensory neuropathy, proprioception, and postural stability. J Orthop Sports Phys Ther. 1999;29(12):718–26. doi: 10.2519/jospt.1999.29.12.718. [DOI] [PubMed] [Google Scholar]
- 4.Fitzpatrick R, McCloskey DI. Proprioceptive, visual and vestibular thresholds for the perception of sway during standing in humans. J Physiol. 1994;478( Pt 1):173–86. doi: 10.1113/jphysiol.1994.sp020240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peterka RJ, Benolken MS. Role of somatosensory and vestibular cues in attenuating visually induced human postural sway. Exp Brain Res. 1995;105(1):101–10. doi: 10.1007/BF00242186. [DOI] [PubMed] [Google Scholar]
- 6.Tan MP, Kenny RA. Cardiovascular assessment of falls in older people. Clin Interv Aging. 2006;1(1):57–66. doi: 10.2147/ciia.2006.1.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kario K, Tobin JN, Wolfson LI, et al. Lower standing systolic blood pressure as a predictor of falls in the elderly: a community-based prospective study. J Am Coll Cardiol. 2001;38(1):246–52. doi: 10.1016/s0735-1097(01)01327-4. [DOI] [PubMed] [Google Scholar]
- 8.Seifer CM, Parry SW. Monitoring devices for falls and syncope. Clin Geriatr Med. 2002;18(2):295–306. doi: 10.1016/s0749-0690(02)00011-3. [DOI] [PubMed] [Google Scholar]
- 9.Sihvonen S, Era P, Helenius M. Postural balance and health-related factors in middle-aged and older women with injurious falls and non-fallers. Aging Clin Exp Res. 2004;16(2):139–46. doi: 10.1007/BF03324543. [DOI] [PubMed] [Google Scholar]
- 10.Allen MD, Kimpinski K, Doherty TJ, Rice CL. Decreased muscle endurance associated with diabetic neuropathy may be attributed partially to neuromuscular transmission failure. J Appl Physiol (1985) 2015;118(8):1014–22. doi: 10.1152/japplphysiol.00441.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Diabetes Statistics Report. 2014. [cited 2015 1/25]; Available from: http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf.
- 12.Wu G, Zhao F, Zhou X, Wei L. Improvement of isokinetic knee extensor strength and reduction of postural sway in the elderly from long-term Tai Chi exercise. Arch Phys Med Rehabil. 2002;83(10):1364–69. doi: 10.1053/apmr.2002.34596. [DOI] [PubMed] [Google Scholar]
- 13.Voukelatos A, Cumming RG, Lord SR, Rissel C. A randomized, controlled trial of tai chi for the prevention of falls: the Central Sydney tai chi trial. J Am Geriatr Soc. 2007;55(8):1185–91. doi: 10.1111/j.1532-5415.2007.01244.x. [DOI] [PubMed] [Google Scholar]
- 14.Wong AM, Pei YC, Lan C, et al. Is Tai Chi Chuan effective in improving lower limb response time to prevent backward falls in the elderly? Age (Dordr) 2009;31(2):163–70. doi: 10.1007/s11357-009-9094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sattin RW, Easley KA, Wolf SL, et al. Reduction in fear of falling through intense tai chi exercise training in older, transitionally frail adults. J Am Geriatr Soc. 2005;53(7):1168–78. doi: 10.1111/j.1532-5415.2005.53375.x. [DOI] [PubMed] [Google Scholar]
- 16.Li F, Harmer P, Fisher KJ, McAuley E. Tai Chi: improving functional balance and predicting subsequent falls in older persons. Med Sci Sports Exerc. 2004;36(12):2046–52. doi: 10.1249/01.mss.0000147590.54632.e7. [DOI] [PubMed] [Google Scholar]
- 17.Wang JS, Lan C, Wong MK. Tai Chi Chuan training to enhance microcirculatory function in healthy elderly men. Arch Phys Med Rehabil. 2001;82(9):1176–80. doi: 10.1053/apmr.2001.24305. [DOI] [PubMed] [Google Scholar]
- 18.Tsai JC, Wang WH, Chan P, et al. The beneficial effects of Tai Chi Chuan on blood pressure and lipid profile and anxiety status in a randomized controlled trial. J Altern Complement Med. 2003;9(5):747–54. doi: 10.1089/107555303322524599. [DOI] [PubMed] [Google Scholar]
- 19.Tsang WW, Hui-Chan CW. Effects of exercise on joint sense and balance in elderly men: Tai Chi versus golf. Med Sci Sports Exerc. 2004;36(4):658–67. doi: 10.1249/01.mss.0000122077.87090.2e. [DOI] [PubMed] [Google Scholar]
- 20.Manor B, Lough M, Gagnon MM, et al. Functional benefits of tai chi training in senior housing facilities. J Am Geriatr Soc. 2014;62(8):1484–89. doi: 10.1111/jgs.12946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li F. The effects of Tai Ji Quan training on limits of stability in older adults. Clin Interv Aging. 2014;9:1261–68. doi: 10.2147/CIA.S65823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Taube W, Lorch M, Zeiter S, Keller M. Non-physical practice improves task performance in an unstable, perturbed environment: motor imagery and observational balance training. Front Hum Neurosci. 2014;8:972. doi: 10.3389/fnhum.2014.00972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taube W, Mouthon M, Leukel C, et al. Brain activity during observation and motor imagery of different balance tasks: An fMRI study. Cortex. 2014;64c:102–14. doi: 10.1016/j.cortex.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 24.Posadzki P, Jacques S. Tai chi and meditation: A conceptual (re)synthesis? J Holist Nurs. 2009;27(2):103–14. doi: 10.1177/0898010108330807. [DOI] [PubMed] [Google Scholar]
- 25.Xu D, Hong Y, Li J, Chan K. Effect of tai chi exercise on proprioception of ankle and knee joints in old people. Br J Sports Med. 2004;38(1):50–54. doi: 10.1136/bjsm.2002.003335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu G, Liu W, Hitt J, Millon D. Spatial, temporal and muscle action patterns of Tai Chi gait. J Electromyogr Kinesiol. 2004;14(3):343–54. doi: 10.1016/j.jelekin.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 27.Ilett P, Lythgo N, Martin C, Brock K. Balance and gait in people with multiple sclerosis: a comparison with healthy controls and the immediate change after an intervention based on the Bobath concept. Physiother Res Int. 2015 doi: 10.1002/pri.1624. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Petrofsky J, Lee S, Bweir S. Gait characteristics in people with type 2 diabetes mellitus. Eur J Appl Physiol. 2005;93(5–6):640–47. doi: 10.1007/s00421-004-1246-7. [DOI] [PubMed] [Google Scholar]
- 29.Dickstein R, Deutsch JE. Motor imagery in physical therapist practice. Phys Ther. 2007;87(7):942–53. doi: 10.2522/ptj.20060331. [DOI] [PubMed] [Google Scholar]
- 30.Malouin F, Richards CL. Mental practice for relearning locomotor skills. Phys Ther. 2010;90(2):240–51. doi: 10.2522/ptj.20090029. [DOI] [PubMed] [Google Scholar]
- 31.Zhang JG, Ishikawa-Takata K, Yamazaki H, et al. The effects of Tai Chi Chuan on physiological function and fear of falling in the less robust elderly: an intervention study for preventing falls. Arch Gerontol Geriatr. 2006;42(2):107–16. doi: 10.1016/j.archger.2005.06.007. [DOI] [PubMed] [Google Scholar]
- 32.Hain TC, Fuller L, Weil L, Kotsias J. Effects of T’ai Chi on balance. Arch Otolaryngol Head Neck Surg. 1999;125(11):1191–95. doi: 10.1001/archotol.125.11.1191. [DOI] [PubMed] [Google Scholar]
- 33.Gatts SK, Woollacott MH. How Tai Chi improves balance: biomechanics of recovery to a walking slip in impaired seniors. Gait Posture. 2007;25(2):205–14. doi: 10.1016/j.gaitpost.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 34.Li F, Harmer P, Fisher KJ, et al. Tai Chi and fall reductions in older adults: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2005;60(2):187–94. doi: 10.1093/gerona/60.2.187. [DOI] [PubMed] [Google Scholar]
- 35.Li F, Harmer P, Mack KA, et al. Tai Chi: moving for better balance – development of a community-based falls prevention program. J Phys Act Health. 2008;5(3):445–55. doi: 10.1123/jpah.5.3.445. [DOI] [PubMed] [Google Scholar]
- 36.Tsang WW, Hui-Chan CW. Effects of tai chi on joint proprioception and stability limits in elderly subjects. Med Sci Sports Exerc. 2003;35(12):1962–71. doi: 10.1249/01.MSS.0000099110.17311.A2. [DOI] [PubMed] [Google Scholar]
- 37.Wang JS, Lan C, Chen SY, Wong MK. Tai Chi Chuan training is associated with enhanced endothelium-dependent dilation in skin vasculature of healthy older men. J Am Geriatr Soc. 2002;50(6):1024–30. doi: 10.1046/j.1532-5415.2002.50256.x. [DOI] [PubMed] [Google Scholar]
- 38.Song QH, Zhang QH, Xu RM, et al. Effect of Tai-chi exercise on lower limb muscle strength, bone mineral density and balance function of elderly women. Int J Clin Exp Med. 2014;7(6):1569–76. [PMC free article] [PubMed] [Google Scholar]
- 39.Wong AM, Chou SW, Huang SC, et al. Does different exercise have the same effect of health promotion for the elderly? Comparison of training-specific effect of Tai Chi and swimming on motor control. Arch Gerontol Geriatr. 2011;53(2):e133–37. doi: 10.1016/j.archger.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 40.Cheon SM, Chae BK, Sung HR, et al. The efficacy of exercise programs for Parkinson’s disease: Tai Chi versus combined exercise. J Clin Neurol. 2013;9(4):237–43. doi: 10.3988/jcn.2013.9.4.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kim H, Kim YL, Lee SM. Effects of therapeutic Tai Chi on balance, gait, and quality of life in chronic stroke patients. Int J Rehabil Res. 2015;38(2):156–61. doi: 10.1097/MRR.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 42.Taylor-Piliae RE, Haskell WL, Stotts NA, Froelicher ES. Improvement in balance, strength, and flexibility after 12 weeks of Tai chi exercise in ethnic Chinese adults with cardiovascular disease risk factors. Altern Ther Health Med. 2006;12(2):50–58. [PubMed] [Google Scholar]
- 43.Yang Y, Hao YL, Tian WJ, et al. The effectiveness of Tai Chi for patients with Parkinson’s disease: study protocol for a randomized controlled trial. Trials. 2015;16:111. doi: 10.1186/s13063-015-0639-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jackson PL, Lafleur MF, Malouin F, et al. Potential role of mental practice using motor imagery in neurological rehabilitation. Arch Phys Med Rehabil. 2001;82:1133–41. doi: 10.1053/apmr.2001.24286. [DOI] [PubMed] [Google Scholar]
- 45.Petrofsky JS, Lohman E, Lohman T. A device to evaluate motor and autonomic impairment. Med Eng Phys. 2009;31(6):705–12. doi: 10.1016/j.medengphy.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 46.Powell LE, Myers MA. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 47.Talley KM, Wyman JF, Gross CR. Psychometric properties of the activities-specific balance confidence scale and the survey of activities and fear of falling in older women. J Am Geriatr Soc. 2008;56(2):328–33. doi: 10.1111/j.1532-5415.2007.01550.x. [DOI] [PubMed] [Google Scholar]
- 48.Duncan PW, Weiner DK, Chandler J, Studenski S, et al. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192–97. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- 49.Bennie S, Bruner K, Diozn A, et al. Measurements of balance: comparison of the Timed “Up and Go” test and Functional Reach test with the Berg Balance Scale. Journal of Physical Therapy Science. 2003;15(2):93–97. [Google Scholar]
- 50.Weiner DK, Duncan PW, Chandler J, Studenski SA, et al. Functional reach: a marker of physical frailty. J Am Geriatr Soc. 1992;40(3):203–7. doi: 10.1111/j.1532-5415.1992.tb02068.x. [DOI] [PubMed] [Google Scholar]
- 51.Thomas JI, Lane JV. A pilot study to explore the predictive validity of 4 measures of falls risk in frail elderly patients. Arch Phys Med Rehabil. 2005;86(8):1636–40. doi: 10.1016/j.apmr.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 52.Vellas BJ, Wayne SJ, Romero L, et al. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45(6):735–38. doi: 10.1111/j.1532-5415.1997.tb01479.x. [DOI] [PubMed] [Google Scholar]
- 53.Jonsson E, Seiger A, Hirschfeld H. One-leg stance in healthy young and elderly adults: a measure of postural steadiness? Clin Biomech (Bristol, Avon) 2004;19(7):688–94. doi: 10.1016/j.clinbiomech.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 54.Franchignoni F, Tesio L, Martino MT, Ricupero C. Reliability of four simple, quantitative tests of balance and mobility in healthy elderly females. Aging (Milano) 1998;10(1):26–31. doi: 10.1007/BF03339630. [DOI] [PubMed] [Google Scholar]
- 55.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. N Engl J Med. 1993;329(14):977–86. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 56.Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–53. [PubMed] [Google Scholar]
- 57.Menant JC, Steele JR, Menz HB, et al. Optimizing footwear for older people at risk of falls. J Rehabil Res Dev. 2008;45(8):1167–81. [PubMed] [Google Scholar]
- 58.Tsai YJ, Lin SI. Older adults adopted more cautious gait patterns when walking in socks than barefoot. Gait Posture. 2013;37(1):88–92. doi: 10.1016/j.gaitpost.2012.06.034. [DOI] [PubMed] [Google Scholar]
- 59.Sakamoto M, Muraoka T, Mizuguchi N, Kanosue K. Combining observation and imagery of an action enhances human corticospinal excitability. Neurosci Res. 2009;65(1):23–27. doi: 10.1016/j.neures.2009.05.003. [DOI] [PubMed] [Google Scholar]
- 60.Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc. 2001;49(5):664–72. [PubMed] [Google Scholar]
- 61.Huang TT, Yang LH, Liu CY. Reducing the fear of falling among community-dwelling elderly adults through cognitive-behavioural strategies and intense Tai Chi exercise: a randomized controlled trial. J Adv Nurs. 2011;67(5):961–71. doi: 10.1111/j.1365-2648.2010.05553.x. [DOI] [PubMed] [Google Scholar]
- 62.Orr R, Tsang T, Lam P, et al. Mobility impairment in type 2 diabetes: association with muscle power and effect of Tai Chi intervention. Diabetes Care. 29(9):2120–22. doi: 10.2337/dc06-1130. 2. [DOI] [PubMed] [Google Scholar]
- 63.Ahn S, Song R. Effects of Tai Chi Exercise on glucose control, neuropathy scores, balance, and quality of life in patients with type 2 diabetes and neuropathy. J Altern Complement Med. 2012;18(12):1172–78. doi: 10.1089/acm.2011.0690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wei GX, Xu T, Fan FM, et al. Can Taichi reshape the brain? A brain morphometry study. PLoS One. 2013;8(4):e61038. doi: 10.1371/journal.pone.0061038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Wei GX, Xu T, Fan FM, et al. Postural sway and rhythmic electroencephalography analysis of cortical activation during eight balance training tasks. Med Sci Monit. 2013;19:175–86. doi: 10.12659/MSM.883824. [DOI] [PMC free article] [PubMed] [Google Scholar]


