Abstract
Background
The global burden of hypertension and other non-communicable diseases (NCDs) is rapidly increasing, and the African continent seems to be the most affected region in the world. The prevalence of hypertension in Nigeria forms a substantial portion of the total burden in Africa because of the large population of the country currently estimated to be over 170 million.
Objective
The purpose of this systematic review is to summarise up to date data on the prevalence and distribution of hypertension in Nigeria from prevalence studies.
Methods
A search of the following databases: PubMed, EMBase and WHO cardiovascular InfoBase from 1968 till date was conducted to identify studies which provide estimates of prevalence of hypertension in Nigeria.
Results
The search yielded a total of 1748 hits from which 45 relevant studies met the inclusion criteria for the review. The overall crude prevalence of hypertension ranged from 0.1% (95%CI:-0.1 to 0.3) to 17.5% (95% CI: 13.6 to 21.4) in children and 2.1% (95%CI: 1.4 to 2.8) to 47.2% (95%CI: 43.6 to 50.8) in adults depending on the benchmark used for diagnosis of hypertension, the setting in which the study was conducted, sex and ethnic group. The crude prevalence of hypertension ranged from 6.2% (95%CI: 4.0 to 8.4) to 48.9% (95%CI: 42.3 to 55.5) for men and 10% (95%CI: 8.1 to 12) to 47.3% (95%CI: 43 to 51.6%) for women. In most studies, prevalence of hypertension was higher in males than females. In addition, prevalence across urban and rural ranged from 9.5% (95%CI: 13.6 to 21.4) to 51.6% (95%CI: 49.8 to 53.4) and 4.8% (95%CI: 2.9 to 6.7) to 43% (95%CI: 42.1 to 43.9) respectively.
Conclusions
The prevalence of hypertension is high among the Nigerian population. Appropriate interventions need to be developed and implemented to reduce the preventable burden of hypertension especially at Primary Health Care Centres which is the first point of call for over 55% of the Nigerian population.
Introduction
The “big three” infectious diseases- Malaria, tuberculosis and HIV/AIDS coupled with childhood and maternal mortality are still the prominent causes of mortality within Nigeria and Africa as a whole [1, 2]. However, globally, the burden of hypertension and other non-communicable diseases (NCDs) is rapidly increasing, and the African continent may be the most affected region in the world [3]. The United Nations (alongside other major public health stakeholders) has declared NCDs a cause for global concern [3, 4].
It is estimated that hypertension affects about 1 billion people all over the world and it is the main risk factor for many other cardiovascular diseases [4, 5, 6, 7]. The prevalence of hypertension in Nigeria may form a substantial proportion of the total burden in Africa because of the large population of the country currently estimated to be over 170 million [4, 7,8].
With an increasing adult population and changing lifestyle of Nigerians, the burden of hypertension may continue to increase as time unfolds [9, 10]. In suggesting an evidence-based context for government and other health policy planners on strategies to reduce this burden in low-resource settings like Nigeria, it is important to have detailed up to date information on the prevalence of hypertension in order to match this with available resources.
In Nigeria, the last two decades has seen a rise in the number of prevalence studies concerning hypertension and other non-communicable diseases [11–16]. Similarly, a number of systematic reviews of the various prevalence studies on hypertension have been done, the most recent being the study by Adeloye et al [4, 11,17]. The study by Adeloye et al [4] was quite detailed in its presentation and analysis in that, it conducted several appropriate meta-analysis of data points from different studies as well as epidemiological models to predict prevalence of hypertension in the future.
However, the study did not consider studies conducted in different Nigerian health care settings i.e. primary, secondary and tertiary health centres. In addition, studies on prevalence of hypertension in children were not included. Given the potential importance of different health care settings in the prevention, treatment and control of hypertension among all age groups, it is pertinent to have a broader picture of the prevalence of hypertension in Nigeria. Therefore, this study builds up on the robust work of Adeloye et al to include prevalence studies conducted in hospitals and among children to inform further research and actions.
Country Profile
Amongst black nations of the world, Nigeria is the most populous and it is the most populated country in Africa with a population of over 160 million people [16, 18]. About 48% of this large population reside in cities while the remaining 52% reside in rural areas. Nigeria has over 250 ethnic groups [18, 19].
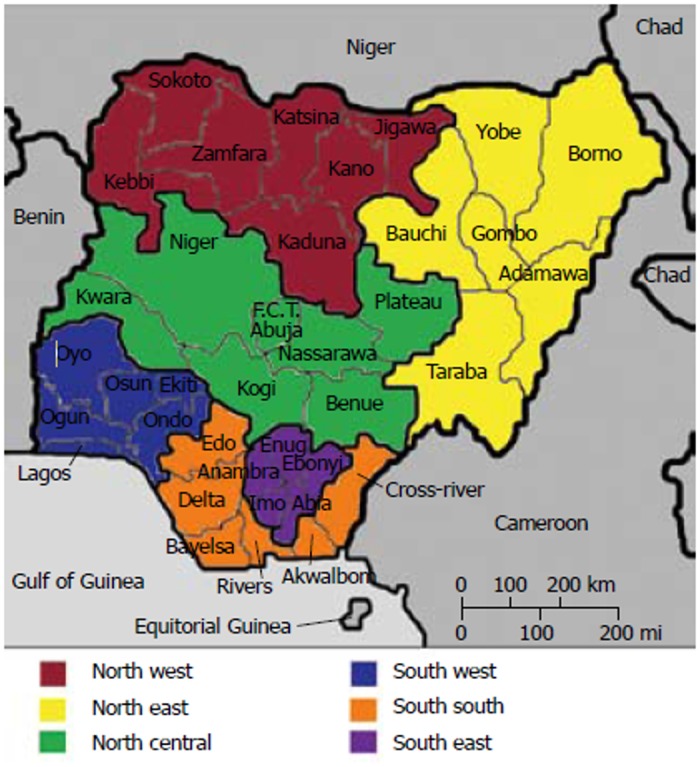
There is a democratically elected government and parliament at the three tiers of government namely: federal, state and local government within thirty six states, 6 geo-political zones and a federal capital territory [19] (see Fig 1).
Fig 1. Map of Nigeria showing the 6 geo-political zones, 36 states and federal capita territory (adapted from [11].
“According to UNDP (2008), the literacy rate in Nigeria is 69.1%, with poverty rate of under $1.25 per day for 64.4% of the population and under $2 for 83.9%” (pg 25) [19]. Life expectancy at birth was 53 years old for males and 55 years for females in 2012. The Total expenditure on health per capita (Intl $, 2012) was 161. Total expenditure on health as % of GDP (2012) was 6.1 [20].
Methods
Eligibility Criteria
Eligibility criteria and the protocol adopted for the study was patterned after that recommended by the National health and medical research council document 1999 for systematic reviews of cross-sectional studies [21].
Types of studies
Cross Sectional studies conducted in rural or urban areas (including hospital based studies) with study sample size of 400 or more were selected for this review. It was calculated that to be able to estimate a prevalence of between 10–50% with a 5% margin of error and 95% level of confidence, a minimum sample size of 400 was required [22]. Studies included must have employed random sampling of a well-defined population or studies using whole populations [23]. The Response rate should be greater than 70% and the study should be conducted on Nigerians only [24]. In addition, studies included should have reported prevalence of hypertension (age adjusted or unadjusted) [25].
Type of participants/case definitions
Studies of prevalence of hypertension in all age groups and both sexes with standard methods of measuring blood pressure were considered [26]. For studies conducted on younger children (Pre-school age group); studies with hypertension defined as “systolic or diastolic blood Pressure greater than or equal to the 95th percentile for age and gender measured on at least three separate occasions” were included (pp 1) [27].
For studies conducted on adolescents and adults, studies with hypertension defined as at least 140 mmHg for SBP and 90 mmHg for DBP were included. This diagnostic criteria/Case definition is based on the definitions of hypertension by the; Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure (JNC6 and JNC7); the 1999 WHO/International Society of Hypertension (WHO/ISH) definitions and classification of blood pressure levels [28,29,30] and the 2003 WHO/ISH Statement on Management of Hypertension [31]. These organisations all put their threshold for hypertension at 140/90mmHg.
However, it is worthy of note that many prevalence studies conducted before 1999 used a cut-off point of ≥160/95mmHg for diagnosing high blood pressure. Because the aim of this study is not to synthesize the data but to appraise the available data from different studies to give a broad picture of the problem, all these studies were included as well, and comparison made between studies that used different definitions.
Sources of Information
All Studies were found by searching through the electronic databases (MEDLINE AND EMBASE), WHO cardiovascular InfoBase and looking through reference list of articles identified for relevant articles not indexed in the databases. Government bulletins and documents such as the federal Ministry of health of Nigeria’s National Non Communicable Disease surveys were also assessed. No language limits were applied to the search strategy. The electronic search was applied to MEDLINE (1966 till present date) and adapted to EMBASE (1980 till present date). The current content of the WHO cardiovascular InfoBase was also reviewed. The Last search was conducted on the 17th of February 2015.
Search Strategy
The following search terms were used to search all databases: prevalence, estimate*, hypertension, “blood pressure”, “raised blood pressure”, “high blood pressure”, Nigeria*. For the purpose of comprehensiveness of search, both free text terms and medical subject headings search was done in both databases. In addition, both free text terms and medical subject headings were exploded and truncated to capture as many articles as possible. No language, publication year or restriction of publication status was imposed in the search strategy. The limit “non-human” was included in the search strategy to exclude all articles conducted in non-humans. See S1 appendix for details of search strategy for EMBASE (ovidSP) and MEDLINE (ovidSP).
Study Selection
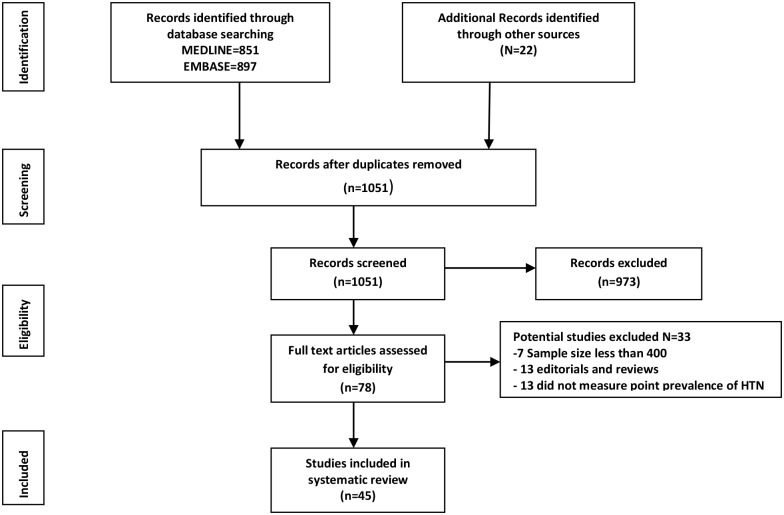
The process of study selection and extraction is presented in a PRISMA flow chart [32], in Fig 2 below. The search returned 1748 publications from MEDLINE (851), EMBASE (897), two (2) government documents from the federal ministry of health, Nigeria, ten (10) from WHO cardiovascular InfoBase and ten (10) relevant articles from references of already identified articles. After removing duplicates and applying the limit “humans only”, one thousand and fifty-one (1051) studies remained. After screening titles and abstracts for relevance i.e. prevalence studies conducted primarily on Nigerians, 973 studies were excluded. Therefore 78 full texts were assessed and after applying the eligibility criteria and quality criteria, a further 33 studies were excluded. Finally, a total of 45 studies [33–78] were included in the review. A table containing list of all potentially-eligible studies with reasons for exclusion is presented in S2 Appendix.
Fig 2. Study selection and extraction adapted from [32].
Data Collection Process
Data from included studies were extracted in duplicate by two authors (JTA and AMU). Any uncertainties were resolved by discussion. The methods were developed and piloted on first 10 papers using a modified Data Extraction Template. Data extracted included the following items: year of survey, state and region where the study was conducted; age of participants; sampling methods; response rate; sample size, health-care setting, and BP definition used for hypertension. In addition, where available, prevalence of high blood pressure (adjusted and unadjusted) and percentage of people with high blood pressure who had been diagnosed before and on treatment were also retrieved.
Risk of Bias in Individual Studies
Because the review question is that of frequency of a health problem, the risk of bias in studies focused on 3 main areas: Sample frame, Case ascertainment and adequate response rate [21]. These areas of bias were addressed in the eligibility criteria hence to ascertain the validity of eligible studies, the eligibility criteria described above which were based on the recommendations of the NATIONAL HEALTH and MEDICAL RESEARCH COUNCIL document were applied [21].
Synthesis and Statistical Methods
The principal purpose of the study was to appraise the available data to give a broad understanding of the scale of the problem of hypertension and the variation between different settings and populations in Nigeria.
Because of the differences in design and context of different studies, and our interest in the differences between the estimates of hypertension prevalence in different contexts, we did not undertake quantitative synthesis of the results of the included studies (Meta analysis) but conducted a narrative synthesis.
In addition, we conducted limited numbers of new Chi Square tests to examine differences between studies addressing our objectives.
Results
Description of studies
Forty-four (44) independent studies [27, 33–77] were included in this review. These studies were published between the years 1968 and 2015. 41 studies [27, 33–77] were conducted across the 6 geopolitical zones of Nigeria and 3 studies [37, 73, 75] were conducted nationally. The numbers of those conducted in the zones are as follows: south- west 15[35–48,54–59,64,67,68]; south-east 8 [27,42,47,51–53,63,66,74]; south-south 10[33,45,60–62,65,70–72,76]; north-central 4 [34,46,48,51]; north-east 1[49] and north-west 4 [39,40,50,69].
Table 1 shows the characteristics of all studies included for the review including crude prevalence of hypertension reported for each study. The included studies were generally large; community based [33–52,54–63,68–70,73–76]; schools based [27,65–67]; hospital based [36,53,69]; and workers (civil-servants and factory workers)[64,71,72]. Sample sizes of studies ranged from 400 [33] to 13,591 [73]. The age of participants ranged from 0 to 110 years old. The setting where the studies were conducted included rural (14 studies), urban (22 studies including urban slums and semi-urban) and mixed (8 studies) i.e. urban and rural at the same time.
Table 1. Characteristics of all studies included in the systematic review.
| CRUDE PREVALENCE % | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| FIRST AUTHOR | REGION | BP cut-off | TARGET POPULATION | SETTING | Age (years) | SAMPLE SIZE (Response Rate %) | OVERALL (95%CI) | MEN(95%CI) | WOMEN(95%CI) |
| Odetunde,201427 | SE | >95th Pα | school based | Urban | 2–5 | 630(100) | 1.9(0.83–2.96) | 1.3(0.4–2.1) | 0.63(0.01–1.3) |
| Abegunde,201335 | SW | 140/90 | community based | urban/rural | 60–110 | 630(98.4) | 36.5 (32.7–40.3) | NA | NA |
| Ekore,200936 | SW | 140/90 | hospital based | Urban | 18–44 | 405(100) | 30.6(26.1–35.1) | 34.4(26.9–41.9) | 28.3(22.7–33.9) |
| Cooper,199737 | national | 140/90 | community based | Rural | 25–74 | 2509(96) | 14.5(13.1–15.9) | 14.7(12.7–16.7) | 14.30(12.4–16.2) |
| Daniel,201338 | SW | 140/90 | community based | urban slum | 20–81 | 964(100) | 38.2(35.1–41.3) | 44.5(39.1–49.9) | 34.9(31.1–38.6) |
| Makusidi,201339 | NW | 140/90 | community based | Urban | 15–80 | 535(99) | 30.2(26.3–34.1) | NA | NA |
| Murthy,201373 | national | 140/90 | community based | urban/rural | ≥40 | 13,591(99.4) | 44.7(43.5–46.3) | 42.6(40.9–44.4) | 46.8(45.3–48.4) |
| Isezuo,201140 | NW | 140/90 | community based | Rural | 15–65 | 782(100) | 24.8(21.8–27.8) | 24.9(20.7–29.1) | 23.60(19.2–27.9) |
| Olatunbosun,200041 | SW | 160/95 | community based | Urban | ≥ 18 | 998(100) | 10.3(8.4–12.2) | 13.9(11.1–16.7) | 5.3(3.2–7.5) |
| okpechi,201342 | SE | 140/90 | community based | urban/rural | ≥18 | 2983(99) | 31.4(29.7–33.1) | 34.9(32.1–37.4) | 28.1(25.9–30.3) |
| Oladapo,201043 | SW | 140/90 | community based | Rural | 18–64 | 2000(100) | 20.8(19.0–22.6) | 21.1(18.4–23.8) | 20.5(18.1–22.9) |
| Ige,201344 | SW | 140/90 | community based | Urban | 28–50 | 525(95.9) | 21.5(17.9–25.0) | 21.9(6.9–26.8) | 21.1(16.1–26.1) |
| Ekanem,201345 | SS | 140/90 | community based | Urban | 15–65 | 442(99) | 47.0(42.3–51.7) | 30.1(24.1–36.1) | 16.8(11.8–21.8) |
| Hendriks,201246 | NC | 140/90 | community based | Rural | ≥18 | 2678(99) | 19.3 # (17.3–21.3) | NA | NA |
| Ulasi,201047 | SE | 140/90 | community based | urban/rural | 25–65 | 1458(75.8) | 32.8(30.4–35.2) | NA | NA |
| Johnson,197148 | SW | 160/95 | community based | Urban | 10–102 | 1392(100) | 8.9(7.4–10.4) | 7.9(5.8–10) | 9.9(7.8–12.0) |
| Okesina,199949 | NE | 140/90 | community based | Rural | ≥18 | 500(100) | 15.2(12.0–18.3) | 19.1(14.5–23.7) | 10.3(6.3–14.3) |
| Ejike,201034 | NC | >95th Pα | community based | urban/rural | 13–18 | 843(100) | 10.1(8.1–12.1) | 9.0(6.4–11.7) | 11.3(8.2–14.4) |
| Mijinyawa,200850 | NW | 140/90 | community based | Urban | 13–19 | 1000(100) | 7.2(5.6–8.9) | 6.2(4.0–8.4) | 7.7(5.3–10.1) |
| Ekezie,201151 | NC/SE | 140/90 | community based | urban/rural | 20–80 | 567(82.7) | 21.7(18.3–25.1) | NA | NA |
| Ulasi,201152 | SE | 140/90 | community based | Urban | ≥20 | 731(94.1) | 42.2(38.5–35.9) | 46.3(43.6–48.9) | 37.7(32.5–42.9) |
| Ike,200953 | SE | 140/90 | hospital based | Urban | ≥20 | 1360(100) | 18.4(17.5–19.2) | 17.2(16.1–18.3) | 18.9(17.5–20.3) |
| Adedoyin,200854 | SW | 140/90 | community based | semi urban | 21–100 | 2097(92.3) | 36.6(34.5–38.7) | 36.8(33.6–39.9) | 36.4(33.7–39.1) |
| Lawoyin,200255 | SW | 160/95 | community cohort | Urban | ≥18 | 2144(99.4) | 12.4(11.0–13.8) | 12.1(10.6–14.0) | 12.7(10.4–13.6) |
| Adebayo,201356 | SW | 140/90 | community based | Rural | 15–90 | 1000(100) | 26.4(23.7–29.1) | 27.3(23.3–31.3) | 25.4(21.6–29.2) |
| Ekpeyong,201276 | SS | 140/90 | community based | Rural | 18–60 | 2780(96.3) | 14.4(13.1–15.7) | 12.6(10.9–14.3) | 12.2(10.4–13.9) |
| Suleiman,201333 | SS | 140/90 | community based | Rural | ≥20 | 400(100) | 15(11.5–18.5) | 18.8(12.7–24.9) | 12.5(8.3–16.7) |
| Oluyombo,201457 | SW | 140/90 | community based | semi urban | ≥18 | 750(89.8) | 47.2(43.6–50.8) | 48.9(42.3–55.5) | 47.3(43.0–51.6) |
| Okpara,201548 | NC | 140/90 | Community based | Urban | ≥16 | 471(100) | 15.7(12.4–18.9) | 16.5(12.4–20.6) | 14.1(8.6–19.6) |
| Ezenwaka,199759 | SW | 140/90 | community based | urban/rural | ≥55 | 500(100) | 30(25.9–34.0) | 25.8(19.8–31.8) | 36.6(31.1–42.1) |
| Andy,201260 | SS | 140/90 | community based | Rural | ≥18 | 3869(96.7) | 23.6(23.3–24.9) | 31.2(28.9–33.5) | 18.1(15.8–20.4) |
| Onwuchekwa,201261 | SS | 140/90 | community based | Rural | ≥18 | 1078(95) | 18.3(15.9–20.6) | NA | NA |
| Omuemu,200762 | SS | 140/90 | community based | Rural | ≥18 | 590(98) | 20.2(16.9–23.4) | 26.2(21.2–31.2) | 13.2(9.3–17.1) |
| Onwubere,201163 | SE | 140/90 | community based | Rural | 40–60 | 858(70.4) | 46.4(43.1–49.7) | 50.2(43.9–56.4) | 44.8(40.9–48.7) |
| Ogunlesi,199164 | SW | 160/95 | male factoryworkers | Urban | ≥18 | 541(100) | 8(5.7–10.3) | NA | NA |
| Okpere,201365 | SS | >95th Pα | school based | Urban | 10–17 | 820(100) | 3.2(1.9–4.4) | 3.3(1.5–5.1) | 3.1(1.4–4.8) |
| Ujunwa,201366 | SE | >95th Pα | school based | Urban | 10–18 | 2694(100) | 5.4(4.5–6.3) | 3.8(2.8–4.8) | 6.9(5.6–8.2) |
| Oyewole,201267 | SW | >95th Pα | school based | Urban | 12–18 | 1638(100) | 0.1(-0.1–0.3) | 0.1(-0.2–0.33) | 0.1(-0.2–0.33) |
| Akinkugbe,196868 | SW | 140/90 | community based | Rural | ≥18 | 3602(100) | 10.1(9.1–11.1) | 9.1(8.1–10.1) | 11.2(10.2–12.2) |
| Jain,197769 | NW | 160/95 | hospital based | Urban | ≥18 | 2950(99.7) | 3.8(3.1–4.5) | 2.9(2.2–3.6) | 4.9(4.2–5.6) |
| Oviasu,197770 | SS | 160/100 | community based | Rural | ≥19 | 1482(96.8) | 2.1(1.4–2.8) | 2.8(2.1–3.5) | 0.5(0.2–2.1) |
| Oviasu,198071 | SS | 140/90 | civil servants | Urban | ≥18 | 1265(99) | 13.3(11.4–15.2) | 14(12.1–15.9) | 10(8.1–12.0) |
| Idahosa,198572 | SS | 140/90 | civil servants | Urban | ≥18 | 1450(98.2) | 15.1(13.3–16.9) | NA | NA |
| Akinkugbe,199775 | National | 160/95 | community based | urban/rural | ≥18 | 4930(98.4) | 11.2(10.3–12.1) | NA | NA |
# = age standardised prevalence rate;
NA = not available;SW = south west;SE = south east;SS = south south;NC = north central;NW = north west;NE = north east;α = 95th percentile
Only 5 studies [27,34,65–67] were conducted on children between 0 to18 years old. Although the search yielded more studies on this age group, most were concerned with pattern of blood pressure in this age group and not prevalence of hypertension.
Diagnosis of hypertension
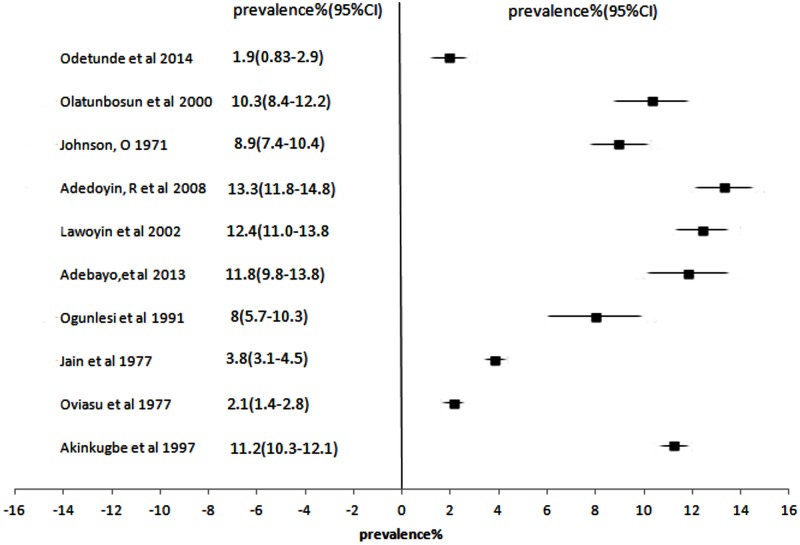
Fig 3 illustrates the prevalence of hypertension for 8 studies [41,48,54–56,64,69,75] that used 160/95mmHg as their benchmark for diagnosing hypertension. Only one study used 160/100mmHg as cut-off [70]. Five studies [27,34,65–67] used the 95th percentile value for age, sex and height as cut-off for hypertension in preschool and adolescents below 18 years of age. The remaining 32 studies used 140/90mmHg as cut-off.
Fig 3. Forest Plot showing prevalence of hypertension% & 95%CI across studies that used BP cut-off ≥ 160/90mmHg.
Prevalence of hypertension amongst children
Overall Crude Prevalence of hypertension recorded in studies conducted on children less than 18 years old [27,34,65–67] ranged from 0.1% (95%CI:-0.1 to 0.3) to 17.5% (95% CI: 13.6 to 21.4). The distribution of hypertension differed highly significantly across different studies conducted on children in Nigeria, χ2 (df, 5) = 155.686, p < 0.0001.
With respect to settings (rural/urban): The highest crude prevalence of hypertension 17.5% (95% CI: 13.6 to 21.4) was recorded in an urban area in the North Central zone. Similarly, the lowest prevalence 0.1% (95%CI:-0.1 to 0.3) was recorded in an urban area in the South West. However, the only study that compared adjusted prevalence between rural and urban children showed a slightly higher value for urban compared to rural (17.5% versus 4.6%).
With respect to sex: where reported the overall prevalence in males and females was very similar.
With respect to increasing age: The 2 studies done in the South East zone showed substantial differences in the crude prevalence (5.4% versus 1.9%). But the crude prevalence of 5.4% (95%CI: 4.5 to 6.3) was for the age group 10–18 years old while 1.9% (95%CI: 0.83 to2.96) was for age group 2–5 years. The prevalence recorded for 10–18 years old in the south-east zone study is relatively similar to the study conducted in Kano (North-West zone) which showed an overall prevalence of 7.2% (95%CI: 5.6 to 8.9) using BP cut off of 140/90mmhg amongst children aged 13–19 years old.
Prevalence of hypertension amongst adults
The overall crude prevalence for studies conducted on adults aged 18 years and above ranged from 2.1% (95%CI: 1.4 to 2.8) to 47.2% (95%CI: 43.6 to 50.8).
With regards to sex: crude prevalence of hypertension ranged from 2.8% to 13.9% and 0.5% to 12.7% for males and females respectively in studies that used the BP benchmark of 160/95mmHg. In studies that used BP benchmark of 140/90mmHg crude prevalence rate of hypertension ranged from 6.2% to 48.9% and 10% to 47.3% for males and females respectively. Where male and female data are available irrespective of BP cut-off, overall crude prevalence rates were generally higher in males than in females (22 studies reported higher prevalence in males compared to females while 11 studies had higher prevalence in females compared to males. However, based on BP cut-off of 160/95mmHg, more studies had higher crude prevalence in females compared to males.
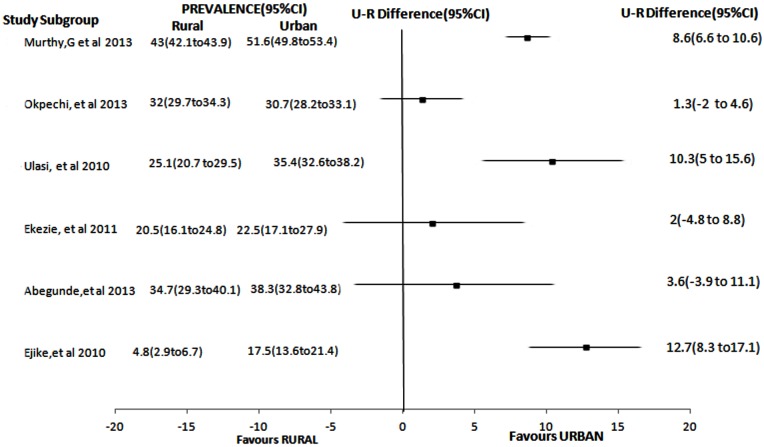
With regards to settings (Urban/Rural): Fig 4 illustrates rural versus urban and urban-rural difference of crude prevalence in 6 available mixed studies (i.e. rural and urban in the same study) [34,35,42,51,52,73]. It is clearly demonstrated in the forest plot that using urban-rural differences in prevalence rates, all mixed studies showed higher prevalence in urban compared to rural areas. Estimates from all mixed studies showed an overall prevalence ranging from 17.5% to 51.6% in urban areas and 4.6% to 43% in rural areas. In 5 out of the 6 studies conducted in mixed settings, prevalence were relatively higher in urban than in rural areas. However, only one of the studies [42] reported that prevalence rate was higher in rural compared to urban area.
Fig 4. Forest Plot showing U-R difference of prevalence of hypertension in studies comparing rural and urban populations.
U-R difference = Urban-Rural difference
With regards to BP cut-off point: Generally the prevalence differed by wide margins when the BP cut-off point changed from 140/90mmHg to 160/90mmHg. Table 2 shows how prevalence changes with different BP cut-off. Four studies compared different BP cut-off points in their analysis [37,54,56,73]. In all the studies there appears to be a decrease in value of prevalence when BP cut-off was increased.
Table 2. Showing changing prevalence (%) using different BP cut-off.
| prevalence rate%(95%CI) | |||||
|---|---|---|---|---|---|
| No | First Author | Year of study | Setting | definition 1 | definition 2 |
| 1 | Murthy73 | 2013 | national | 44.9(43.5–46.3) | 24.3(23.6–25.0) |
| 2 | Cooper37 | 1997 | national | 14.5(13.1–15.9) | 6.9(6.2–7.6) |
| 3 | Adedoyin54 | 2008 | SW | 36.6(34.5–38.7) | 13.3(11.8–14.8) |
| 4 | Adebayo,56 | 2013 | SW | 26.4(23.7–29.1) | 11.8(9.8–13.8) |
Definition 1: Systolic BP ≥140 mmHg or Diastolic BP ≥ 90 mmHg; Definition 2: Systolic BP ≥ 160 mmHg ≥ or Diastolic BP ≥ 90mmHg
SW = south west
With regards to trends: Although pooled estimates were not done in this review, it appears that the mean blood pressure levels may have risen over time. The prevalence figures from the 2 national surveys done in 1997 and 2013 were 11.2% (95% CI: 10.3 to12.1) and 24.3% (95% CI: 23.6 to 25) respectively using BP cut off of ≥160/90mmHg. When a threshold of 140/90mmHg was used in the 2013 national prevalence study, the prevalence rate increased to 45.9% (95% CI: 43.5–46.3%).
Prevalence of hypertension amongst hospital clients
Only three studies [36,53,69] included in the review were carried out in a hospital setting. Two (2) of the studies [36,53] were conducted in 2009 using a BP cut-off of 140/90mmHg while one (1) [69] was conducted in 1977 with a BP cut off of 160/95mmHg. Crude prevalence recorded in these studies were 3.8% (95% CI: 3.1 to 4.5), 18.4% (95% CI: 17.5 to 19.2) and 30.6% (95% CI: 26.1 to 35.1) conducted in 1977 and 2009 respectively. Although a BP cut-off of 160/95mmHg was used for the 1977 study, the results show a very low prevalence of hypertension among hospital attendees in 1977 compared to later years. This increasing pattern of prevalence rates amongst hospital attendees is similar to that experienced in community based studies.
The hospital based study that revealed a prevalence of 18.4% [36] also showed that during the period of review, 26.5% of all hospital cases and 46.1% of hypertension related complications respectively were due to hypertensive heart failure. A study which reviewed complications of hypertension also showed that the commonest risk factor for stroke, heart failure, and ischemic heart disease and chronic kidney disease in Nigeria was high blood pressure [77].
Prevalence of hypertension by ethnic groups and Geopolitical zones
There are over 250 distinct ethnic groups in Nigeria. But, only 2 studies have reported prevalence studies by ethnic groups [60,73]. The study by Andy et al [60] compared prevalence of hypertension among only 3 ethnic groups (Obolo, Efiks, Ibibios) resident in the south- south region of the country. The prevalence rates ranged from 14.9% to 25.6% [60]. The lowest rate was recorded amongst the “Obolo” ethnic group while the highest rate was in the “Efiks”.
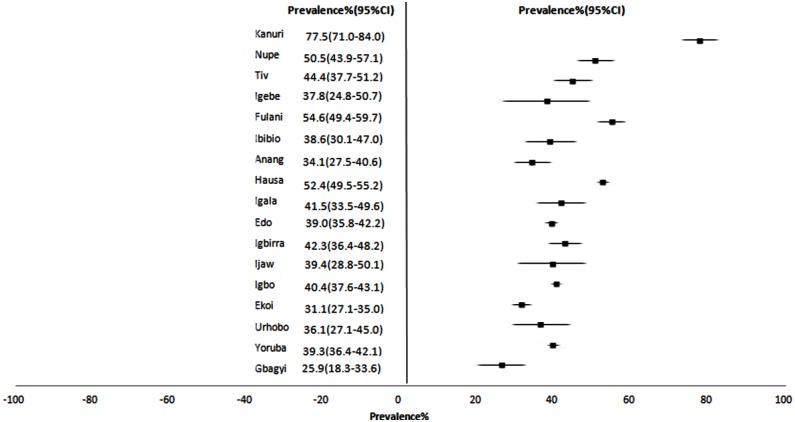
But the national survey by Murthy, G. et al [73] cut across 17 major ethnic groups scattered all over the country as illustrated in Fig 5. Using BP cut off of 140/90mmHg, prevalence rates ranged from 25.9% (95%CI: 18.3 to 33.6) to 77.5% (95%CI: 71.0 to 84.0) with the highest being in the Kanuri group and lowest in the Gbagyi group. Prevalence figures obtained among Ibibios(25.5%) in the Andy, J et al [60] study was lesser than in the Murthy, G et al study (38.6%(95%CI:30.1 to 47.0)).
Fig 5. Forest plot showing hypertension prevalence and 95% CI across 17 ethnic groups in the Murthy, G et al 2013 study[73].
The distribution of hypertension differed highly significantly across ethnic groups in Nigeria, χ2 (df, 16) = 361.464, p < 0.0001.
In addition, the only study that reported prevalence by geopolitical zone was the national survey by Murthy, G et al [73]. The crude prevalence of hypertension by geopolitical zones (North-east, south-east, south-south, North-west, South-west, North-central) using BP cut off of 140/90mmHg were 60.4% (95%CI:55.1 to 65.8), 41.0%(95%CI:38.0 to 44.0), 34.2%(95%CI:31.2 to 37.2), 51.5%(95%CI:48.7 to 54.2), 40.1%(95%CI:37.1 to 43.2), and 39.5%(95%CI:35.7 to 43.3) respectively. Also, the distribution of hypertension differed highly significantly across geopolitical zones in Nigeria, χ2 (df, 5) = 375.656, p < 0.0001.
Discussion
Most studies reported only the crude prevalence of hypertension. Most of the studies carried out in the last 20 years reported a higher prevalence of hypertension compared to older studies [74,79,80]. Reported values of prevalence of hypertension in Nigeria vary widely. These wide variations in values are in part dependent on the blood pressure criteria used. Some of the variations can also be explained by methodological differences (e.g. some have focused on only rural populations) but variation in the age groups studied is likely to be a major factor. Information on trends in the prevalence of hypertension is limited because there were no follow up studies on similar population groups. Although, these populations might be located in the same geo-political zone or state, characteristics of each village or group or tribe differ significantly. A systematic review of hypertension prevalence studies by Adeloye et al[4] observed that pooled prevalence of hypertension increased from 8.6% over the period 1970–1979 to 22.5% over the period 2000–2011.
Many of the studies mentioned in this review that used cut-off of 140/90mmhg reported that prevalence of hypertension was higher in males than females but the reverse was reported for studies that used 160/90mmhg. This pattern is difficult to explain and adequate comparison can only be made with age and sex-adjusted figures which was lacking in most of the included studies. However, the pattern of higher blood pressure in males compared to females of middle age group is similar to findings in other Africans, African Americans and blacks in Caribbean region [81]. Similarly, in a related study, it was shown that men have higher blood pressure than women of the same age group before women attain the age of menopause [82]. This could be due to societal socio-economic roles assigned to men in the home where they have to provide most of the finances for family maintenance [79].
Most of the cross-sectional studies used for this review include middle-age subjects. However, some cross-sectional studies were conducted among older population groups [59,63] or children [27,34,65–67]. Values of Prevalence of hypertension in children are much lower than that reported in adults. Also, there appears to be no gender preponderance for prevalence of hypertension when other risk factors such as obesity have been excluded [27]. Nevertheless, research has shown that blood pressure readings increases with age development and growth and results in high blood pressure by middle-age [83]. In addition, Children with high blood pressure tend to continue to have hypertension as they grow older[84].
The differences in prevalence of hypertension in rural versus urban is evident in most of the included studies. Pooled results from the review done by Adeloye et al also showed a higher urban prevalence compared to rural (31% versus 26%)[4]. This is contextually similar to other studies done in African countries where higher prevalence rates have been reported among urban dwellers [22]. The higher prevalence amongst urban populations may portray a different lifestyle pattern. Urban dwellers are more likely to consume foods that are processed and foods that have high salt and fat content [85]. Furthermore, the lower rural prevalence may indicate higher physical activities levels from trekking long distances and physically taxing farming activities, in addition to greater consumption of freely available vegetables and fruits taking place in majority of rural areas [86, 87]. However, in few studies [42] especially in the eastern part of Nigeria, it was noted that prevalence rate of hypertension was higher in rural than urban area (see Fig 4). This finding is similar to findings in some studies [88–90] in the United States and European population. It is likely that the rural population age pattern is older because it is a popular practice for older people to migrate to rural areas after retirement from active work.
The distribution of hypertension differed among ethnic groups and across geopolitical zones. However, the high hypertension prevalence rate recorded among the Kanuri ethnic group [73] indicates a need for further investigation for possible explanations because this ethnic group is concentrated in only 1 region of the country and the prevalence estimates may be confounded by other factors. Some evidence of ethnic variations has been reported in Kenya with statistically significant differences after adjusting for cardiovascular and socio-demographic risk factors [91].
Report of data from studies done in hospitals reveal that hypertension and cardiovascular disease complications are the commonest NCDs in Nigeria [36,53,69]. This report is very similar to a rate of 30% obtained from Tanzania[92].
A key limitation of this review was that across all studies retained for the review crucial data on sex, age and other descriptive statistics adjusted across rural and urban settings were not always available (see table 1 for overall characteristics of studies included in review).
Comments
This review has summarised available reports on the prevalence of hypertension in Nigeria. From these reports, it is evident that hypertension is a major public health problem in Nigeria. These prevalence estimates were gleaned from studies conducted in community and hospital based settings. Most of the community based studies were either conducted using house to house surveys or places of mass gathering such as churches, mosques and markets. All of the hospitals were either secondary or tertiary health care centres. However, hypertension studies have not been undertaken specifically on clients who visit primary health care centres which are often the first port of call for people living in both rural and urban areas. This is partly because the focus of primary health care in Nigeria has been on preventive and curative services for endemic communicable diseases and for maternal and child health-related issues in the community.
The effect of non-communicable diseases on development is two-fold [–119–11]. They worsen poverty levels as well as reduce national income available for meaningful development [4,6]. “It is projected that in the next 10 years, China, India and Britain will lose USD 558 billion, USD237 billion, and USD33 billion respectively due to heart disease, stroke and diabetes mellitus”(pg260)[12].
Similarly, in Nigeria the economic burden posed by hypertension and its complications are very high [13]. For example, a study on monthly cost of hypertension treatment per person in a community in the south-western part of Nigeria showed that an average of ten united state dollars (10USD) was spent on drugs alone aside from other direct cost. This is untenable in a population where many live below 2USD a day [4,14].
Moreover, it has been shown that the average monthly cost of treatment of hypertension could be higher especially in cases where the patients have to go back for follow-up more frequently than expected due to complications of management [15].
The low levels of awareness, treatment and control of hypertension, suggest that rates of cardiovascular complications such as cerebro-vascular accidents, heart failure, and renal failure will increase in coming years [4]. As health care services are currently organised in Nigeria, most of these complications will present at secondary and tertiary health care centres and may overwhelm these centres and their resources if measures are not taken to ensure adequate prevention and treatment.
This suggests that there is a need for additional resources for the detection and control of hypertension and other NCDs in addition to resources being allocated for the control of major communicable diseases and neglected tropical diseases. Interventions and strategies will be required to increase adherence to life-style changes and life-long medications. It is clear that hypertension and its complications will cause both governments and societies large financial and societal cost but the government needs to respond to this emerging challenge to ensure the future health of Nigerians.
The implication is that more hypertension and other NCDs strategies should be developed and evaluated specifically in primary health care centres to achieve sustainable policies and practices required for expanding preventive and curative services available at the primary health care level for hypertension and other NCDs in Nigeria.
Supporting Information
(DOCX)
(DOC)
(DOC)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This review forms part of research work towards a PhD (AKINLUA JT) at the University College London, funded by the NYSC Presidential Scholarship Scheme through the Nigerian Universities Commission/Tertiary Education Fund. The sponsor had no role in study design, data collection, analysis, interpretation, or writing of the report.
References
- 1. De-Graft Aikins A, Unwin N, Agyemang C, Allotey P, Campbell C, Arhinful D. Tackling Africa’s chronic disease burden: from the local to the global. Global Health; 2010;6:5 10.1186/1744-8603-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Akinboboye O, Idris O, Akinboboye O, Akinkugbe O. Trends in coronary artery disease and associated risk factors in sub-Saharan Africans. J Hum Hypertens 2003; 17: 381–387. [DOI] [PubMed] [Google Scholar]
- 3. World Health Organization. A global brief on hypertension: silent killer, global public health crises (World Health Day 2013). Geneva: WHO; 2013; Available: http://apps.who.int/iris/bitstream/10665/79059/1/WHO_DCO_WHD_2013.2_eng.pdf Accessed 2015 Feb 11. [Google Scholar]
- 4. Adeloye D, Basquill C, Aderemi AV, Thompson JY, Obi FA. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. J Hypertens 2015;33: 230–242. 10.1097/HJH.0000000000000413 [DOI] [PubMed] [Google Scholar]
- 5. Beaglehole R, Bonita R, Alleyne G, Horton R, Li L, Lincoln P, et al. UN high-level meeting on non-communicable diseases: addressing four questions. Lancet 2011; 378:449–455. 10.1016/S0140-6736(11)60879-9 [DOI] [PubMed] [Google Scholar]
- 6. World Health Organisation. Global status report on non-communicable diseases. Geneva: WHO; 2011. [Google Scholar]
- 7.World Bank Nigeria 2013. Available: http://data.worldbank.org/country/nigeria. Accessed 2015 Jan 29.
- 8.World Health Organisation AFRO, editor. Report of regional director: cardiovascular diseases in the African region: current situation and perspectives. Regional committee for Africa 2005; Maputo, Mozambique: The WHO Regional Office for Africa.
- 9. Kayima J, Wanyenze RK, Katamba A, Leontsini E, Nuwaha F. Hypertension awareness, treatment and control in Africa: a systematic review. BMC Cardiovasc Disord 2013; 13:54 10.1186/1471-2261-13-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Perkovic V, Huxley R, Wu Y, Prabhakaran D, MacMahon S. The burden of blood pressure-related disease: a neglected priority for global health. Hypertension 2007; 50:991–997. [DOI] [PubMed] [Google Scholar]
- 11. Ogah OS, Okpechi I, Chukwuonye II, Akinyemi JO, Onwubere BJC, Falase AO, et al. Blood pressure, prevalence of hypertension and hypertension related complications in Nigerian Africans: a review. World J Cardiol 2012; 4:327–340. 10.4330/wjc.v4.i12.327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ekpenyong CE, Udokang NE, Akpan EE, Samson TK. Double burden, non communicable diseases and risk factors evaluation in sub-Saharan Africa: The Nigerian experience. Eur J Sustain Develop 2012; 1(2):249–270. [Google Scholar]
- 13. Abegunde DO, Mathers CD, Adam T, Ortegon M, Strong K. Chronic diseases 1: the burden and costs of chronic diseases in low-income and middle-income countries. Lancet 2007; 370:1929–1938. [DOI] [PubMed] [Google Scholar]
- 14. Ilesanmi OS, Ige OK, Adebiyi AO. The managed hypertensive: the costs of blood pressure control in a Nigerian town. Pan Afr Med J. 2012; 12:96 [PMC free article] [PubMed] [Google Scholar]
- 15. Ukwaja KN, Onyedum CC. Reaction to Ilesanmi OS et al. the managed hypertensive: the costs of blood pressure control in a Nigerian town. Pan Afr Med J. 2013; 14:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Bank website. Available: http://www.worldbank.org/. Accessed 2015 Jan 29.
- 17. Commodore-Mensah Y, Samuel LJ, Dennison-Himmelfarb CR, Agyemang C. Hypertension and overweight/obesity in Ghanaians and Nigerians living in West Africa and industrialized countries: a systematic review. Journal of Hypertension. 2014; 32:464–472. 10.1097/HJH.0000000000000061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Population Commission website. Available: www.population.gov.ng. Accessed on 2015 Feb 19.
- 19.Akinlua, JT. An exploratory study into the emergency and disaster management systems in Nigeria. A dissertation submitted to Liverpool John Moores University, UK in partial fulfilment of MSc in international public health 2012.
- 20.Nigeria’s Demographic profile 2013. Available: http://www.indexmundi.com/Nigeria/demographics_profile.html.Accessed 2015 Feb 16
- 21.National Health and Medical Research guidelines. Available: www.nhmrc.gov.au. Accessed 2015 Feb 10
- 22. Addo J, Smeeth L, Leon D. Hypertension in sub-saharan Africa: a systematic review. Hypertensio. 2007; 50: 1012–1018 available: http://hyper.ahajournals.org/content/50/6/1012. Accessed 2015 Feb 15. [DOI] [PubMed] [Google Scholar]
- 23. Seedat YK. Recommendations for hypertension in sub-Saharan Africa. Cardiovasc J S Afr. 2004; 15:157–158. [PubMed] [Google Scholar]
- 24. Khor GL. Cardiovascular epidemiology in the Asia-Pacific region. Asia Pac J Clin Nutr.2001; 10: 76–80. [DOI] [PubMed] [Google Scholar]
- 25.World Health Organisation Expert Committee on Arterial Hypertension (Technical report Series No. 628). Geneva: WHO 1978. [PubMed]
- 26.World Health Organisation Collaborating Centre for Surveillance of Cardiovascular Disease. Epidemiological profiles of cardiovascular and cerebrovascular diseases in the world. Global Cardiovascular Infobase 2006. Available at: http://cvdinfobase.ca/. Accessed 2015 Feb 15.
- 27. Odetunde I, Emeka E, Josephat M, Henrietta U, Oluwatoyin A, Osita U, et al. Elevated arterial blood pressure and body mass index among Nigerian preschool children population. BMC Pediatrics. 2014; 14:64 10.1186/1471-2431-14-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mabadeje AF. World Health Organisation WHO-ISH Guidelines for the management of hypertension: implementation in Africa: the Nigerian experience. Clin Exp Hypertens.1999; 21:671–681. [DOI] [PubMed] [Google Scholar]
- 29. Whitworth JA. World Health Organization (WHO)/International Society of Hypertension (ISH,) statement on management of hypertension. J Hypertens.2003; 21:1983–1992. [DOI] [PubMed] [Google Scholar]
- 30. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL.The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension.2003; 42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 31.The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 6) (1997) Washington DC: U.S. Department of Health and Human Services.
- 32. Moher D, Liberati A, Tetzlaff J, Altman DG. Group PRISMA Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol.2009; 62:1006–1012. [DOI] [PubMed] [Google Scholar]
- 33. Suleiman IA, Amogu EO, Ganiyu KA. Prevalence and control of hypertension in a Niger Delta semi urban community, Nigeria. Pharmacy Practice Jan-Mar 2013; 11(1):24–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ejike C, Ugwu CE, Ezeanyika L. Variations in the prevalence of point (pre)hypertension in a Nigerian school-going adolescent population living in a semi-urban and an urban area. BMC Pediatrics. 2010; 10:13 10.1186/1471-2431-10-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Abegunde KA, Owoaje ET. Health problems and associated risk factors in selected urban and rural elderly population groups of South-West Nigeria. Ann Afr Med[serialonline] 2013; 12: 907 Available: http://www.annalsafrmed.Org/text.asp?2013/12/2/90/112398. Accessed 2015 Jan 29. [DOI] [PubMed] [Google Scholar]
- 36. Ekore RI, Ajayi IO, Arije A.Case finding for hypertension in young adult patients attending a missionary hospital in Nigeria. Afr Health Sci. 2009; 9:193–9. [PMC free article] [PubMed] [Google Scholar]
- 37. Cooper RS, Rotimi CN, Ataman S, McGee D, Osotimehin B, Kadiri S, et al. The Prevalence of Hypertension in Seven Populations of West African Origin. Am J Public health. 1997; 87: 160 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Daniel OJ, Adejumo OA, Adejumo EN, Owolabi RS, Braimoh RW. Prevalence of hypertension among urban slum dwellers in Lagos, Nigeria. J Urban Health,2013; 90: 1016–1025. 10.1007/s11524-013-9795-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Makusidi MA, Liman HM, Yakubu A, Isah MDA, Jega RM, Adamu H et al. Prevalence of Non-communicable Diseases and it’s awareness among inhabitants of Sokoto Metropolis; Outcome of a Screening Program for Hypertension, Obesity, Diabetes Mellitus and Overt Proteinuria. Arab Journal of Nephrology and Transplantation.2013; 6 (3):189–91. [PubMed] [Google Scholar]
- 40. Isezuo SA, Sabir AA, Ohwovorilole AE, Fasanmade OA. Prevalence, associated factors and relationship between prehypertension and hypertension: a study of two ethnic African populations in Northern Nigeria. J Hum Hypertens. 2011; 25: 224–230. [DOI] [PubMed] [Google Scholar]
- 41. Olatunbosun ST, Kaufman JS, Cooper RS, Bella AF. Hypertension in a black population: prevalence and biosocial determinants of high blood pressure in a group of urban Nigerians. J Hum Hypertens.2000; 14: 249–257. [DOI] [PubMed] [Google Scholar]
- 42. Okpechi IG, Chukwuonye II, Tiffin N, Madukwe OO, Onyeonoro UU, et al. Blood Pressure Gradients and Cardiovascular Risk Factors in Urban and Rural Populations in Abia State South Eastern Nigeria Using the WHO STEPwise Approach. PLoS ONE 2013;8(9): e73403 10.1371/journal.pone.0073403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Oladapo OO, Salako L, Sodiq O, Shoyinka K, Adedapo K, et al. A prevalence of cardiometabolic risk factors among a rural Yoruba south-western Nigerian population: a population-based survey. Cardiovasc J Afr.2010; 21: 26–31. [PMC free article] [PubMed] [Google Scholar]
- 44. Ige OK, Owoaje TE, Adebiyi OA. Non communicable disease and risky behaviour in an urban university community Nigeria African Health Sciences 2013;13(1):62–67 10.4314/ahs.v13i1.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ekanem US Opara DC, Akwaowo CD. High blood pressure in a semi-urban community in south-south Nigeria: a community—based study African Health Sciences.2013;13 (1):56–6. 10.4314/ahs.v13i1.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hendriks ME, Wit FW, Roos MT, Brewster LM, Akande TM, de Beer IH, et al. Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PLoS One. 2012; 7(3): e32638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ulasi II, Ijoma CK, Onodugo OD (2010) A community-based study of hypertension and cardio-metabolic syndrome in semi-urban and rural communities in Nigeria. BMC Health Serv Res; 10: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Johnson TO. Arterial blood pressures and hypertension in an urban African population sample. Br J Prev Soc Med. 1971; 25: 26–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Okesina AB, Oparinde DP, Akindoyin KA, Erasmus RT. Prevalence of some risk factors of coronary heart disease in a rural Nigerian population. East Afr Med J,1999. 76(4):212–6. [PubMed] [Google Scholar]
- 50. Mijinyawa MS, Iliyasu Z, Borodo MM. Prevalence of hypertension among teenage students in Kano, Nigeria. Niger J Med, 2008; 17:173–8. [DOI] [PubMed] [Google Scholar]
- 51. Ekezie J, Anyanwu EG, Danborno B, Anthony U. Impact of urbanization on obesity, anthropometric profile and blood pressure in the Igbos of Nigeria. North Am J Med Sci.2011; 3:242–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ulasi II, Ijoma CK, Onwubere BJ, Arodiwe E, Onodugo O, Okafor C. High prevalence and low awareness of hypertensionin a market population in enugu, Nigeria. Int J Hypertens.2011;8: 669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Ike SO. Prevalence of hypertension and its complications among medical admissions at the University of Nigeria Teaching Hospital, Enugu (Study 2). Niger J Med.2009; 18: 68–72. [PubMed] [Google Scholar]
- 54. Adedoyin RA, Mbada CE, Balogun MO, Martins T, Adebayo RA, Akintomide A, et al. Prevalence and pattern of hypertension in a semiurban community in Nigeria. Eur J Cardiovasc Prev Rehabil. 2008; 15: 683–687. [DOI] [PubMed] [Google Scholar]
- 55. Lawoyin TO. Prevalence of cardiovascular risk factors in an African, urban inner city community. West African journal of medicine.2002; 21(3):208–211. [DOI] [PubMed] [Google Scholar]
- 56. Adebayo RA, Balogun MO, Adedoyin RA, Obashoro- John OA, Bisiriyu LA, Abiodun OO.Prevalence of hypertension in three rural communities of Ife north local Government Area of Osun state, south West Nigeria. International Journal of General Medicine. 2013;6: 863–868. 10.2147/IJGM.S51906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Oluyombo R, Olamoyegun MA, Olaifa O, Iwuala SO, Babatunde OA. Cardiovascular risk factors in semi-urban communities in southwest Nigeria: Patterns and prevalence, J Epidemiol Global Health, 2014. Available: 10.1016/j.jegh.2014.07.002 Accessed 2015 Feb 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Okpara I, Utoo P, Bako I.Prevalence and awareness of hypertension amongst staff and students of a tertiary institution in Nigeria. Global Advanced Research Journal of Medicine and Medical Sciences (GARJMMS) ISSN: 2315-5159, 2015; January Vol. 4(1), pp. 061–066. [Google Scholar]
- 59. Ezenwaka CE, Akani AO, Akanji BO, Unwin NC, Adejuwon CA. The Prevalence of Insulin Resistance and Other Cardiovascular Disease Risk Factors in Healthy Elderly South-western Nigerians. Atherosclerosis. 1997; 128(2):201–11. [DOI] [PubMed] [Google Scholar]
- 60. Andy JJ, Peters EJ, Ekrikpo UE, Akpan NA, Unadike BC, Ekott JU. Prevalence and correlates of hypertension among the Ibibio/Annangs, Efiks and Obolos: a cross sectional community survey in rural South- South Nigeria. Ethn Dis. 2012; 22(3): 335–339. [PubMed] [Google Scholar]
- 61. Onwuchekwa AC, Mezie-Okoye MM, Babatunde S. Prevalence of hypertension in Kegbara-Dere, a rural community in the Niger Delta region, Nigeria. Ethn Dis. 2012; 22: 340–346. [PubMed] [Google Scholar]
- 62. Omuemu VO, Okojie OH, Omuemu CE. Awareness of high blood pressure status, treatment and control in a rural community in Edo State. Niger J Clin Pract. 2007; 10: 208–212. [PubMed] [Google Scholar]
- 63. Onwubere BJ, Ejim EC, Okafor CI, Emehel A, Mbah AU, Onyia U. Pattern of Blood Pressure Indices among the Residents of a Rural Community in South East Nigeria. Int J Hypertens 2011;621074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ogunlesi A, Osotimehin B, Abbiyessuku F, Kadiri S, Akinkugbe O, Liao YL, et al. Blood pressure and educational level among factory workers in Ibadan, Nigeria. J Hum Hypertens.1991; 5: 375–380. [PubMed] [Google Scholar]
- 65. Okpere AN, Anochie IC, Eke FU.Pattern of blood pressure and hypertension in adolescents in Port Harcourt, Nigeria. West African Journal of Medicine,2013. 32(2):93–98. [PubMed] [Google Scholar]
- 66. Ujunwa FA, Ikefuna AN, Nwokocha ARC, Chinawa JM. Hypertension and pre-hypertension among adolescents in secondary schools in Enugu, South East Nigeria. Italian Journal of Pediatrics,2013; 39:70 10.1186/1824-7288-39-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Oyewole OO, Oritogun KS. Pre-hypertension and hypertension in adolescence: how much does it occur in a Nigerian community? West Afr J Med. Apr-Jun 2012; 31(2):71–5. [PubMed] [Google Scholar]
- 68. Akinkugbe OO, Ojo AO. The systemic blood pressure in a rural Nigerian population. Trop Geogr Med. 1968; 20: 347–356 [PubMed] [Google Scholar]
- 69. Jain PS, Gera SC, Abengowe CU. Incidence of hypertension in Ahmadu Bello University Hospital Kaduna—Nigeria J Trop Med Hyg.1977; 80: 90–94. [PubMed] [Google Scholar]
- 70. Oviasu VO. Arterial blood pressures and hypertension in a rural Nigerian community. Afr J Med Med Sci. 1977; 7: 137–143. [PubMed] [Google Scholar]
- 71. Oviasu VO, Okupa FE. Arterial blood pressure and hypertension in Benin in the equatorial forest zone of Nigeria. Trop Geogr Med. 1980; 32: 241–244. [PubMed] [Google Scholar]
- 72. Idahosa PE.Blood pressure pattern in urban Edos. J Hypertens Suppl 1985;3: S379–S381. [PubMed] [Google Scholar]
- 73. Murthy GV, Fox S, Sivasubramaniam S, Gilbert CE, Mahdi AM, Imam AU, et al. Prevalence and risk factors for hypertension and association with ethnicity in Nigeria: results from a national survey. Cardiovasc J Afr,2013; 24:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ogah OS, Madukwe OO, Chukwuonye II, Onyeonoro UU, Ukaegbu AU, Akhimien MO, et al. Prevalence and determinants of hypertension in Abia State Nigeria: Results from the Abia State Non-Communicable diseases and Cardiovascular Risk factors Survey. Ethn Dis 2012; In press. [PubMed] [Google Scholar]
- 75.Akinkugbe O. Non communicable diseases in Nigeria: final report of a national survey, Lagos. 1997: Federal Ministry of Health–National Expert Committee on Non-Communicable Diseases.
- 76. Ekpenyong CE, Udokang NE, Akpan EE, Samson TK. Double Burden, Non- Communicable Diseases And Risk Factors Evaluation In Sub-Saharan Africa: The Nigerian Experience. European Journal of Sustainable Development, 2012;1, 2, 249–270 ISSN: 2239-5938. [Google Scholar]
- 77. Ogah OS. Hypertension in Sub-Saharan African populations: the burden of hypertension in Nigeria. Ethn Dis. 2006; 16: 765. [PubMed] [Google Scholar]
- 78. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet.2005; 365:217–223. [DOI] [PubMed] [Google Scholar]
- 79. Bello M. Nigerians wake up to high blood pressure. Bull World Health Organ.2013; 91:242–243. 10.2471/BLT.13.020413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Onyemelukwe GC (2003) National survey of non communicable diseases (South-West zone), Abuja. 2003: Federal Ministry of Health–National Expert Committee on Non-Communicable Diseases.
- 81. Cooper RS, Amoah AG, Mensah GA.High blood pressure: the foundation for epidemic cardiovascular disease in African populations. EthnDis. 2003; 13:S48–S52. [PubMed] [Google Scholar]
- 82. Hajar I, Kotchen JM, Kotchen TA. Hypertension: trends in prevalence, incidence, and control. Annu Rev Public Health, 2006; 27:465–490. [DOI] [PubMed] [Google Scholar]
- 83. Chadha SL, Tandon R, Shekhawat S, Gopinath N. An epidemiology study of blood pressure in school children (5–14 years) in Delhi. Indian Heart J,1999; 51:178–182. [PubMed] [Google Scholar]
- 84. Anjana P, Kaur N, Kumari K, Sidhu S. Variation in blood pressure among school children of Amritsar (Punjab). Anthropologist, 2005; 7:201–204. [Google Scholar]
- 85. Mezue K. The increasing burden of hypertesnsion in Nigeria: can dietary salt reduction strategy change the trend? Perspect Public Health 2013.[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 86. Assah FK, Ekelund U, Brage S, Mbanya JC, Wareham NJ. Urbanization, physical activity, and metabolic health in sub-Saharan Africa. Diabetes Care, 2011; 34:491–496. 10.2337/dc10-0990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Lancet, 2010; 376:1775–1784. 10.1016/S0140-6736(10)61514-0 [DOI] [PubMed] [Google Scholar]
- 88. Banegas JR, Rodríguez-Artalejo F, de la Cruz Troca JJ, Guallar- Castillón P, del Rey Calero J. Blood pressure in Spain: distribution, awareness, control, and benefits of a reduction in average pressure. Hypertension, 1998; 32: 998–1002. [DOI] [PubMed] [Google Scholar]
- 89. Mainous AG, King DE, Garr DR, Pearson WS. Race, rural residence, and control of diabetes and hypertension. Ann Fam Med.2004; 2: 563–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Psaltopoulou T, Orfanos P, Naska A, Lenas D, Trichopoulos D, Trichopoulou A Prevalence, awareness, treatment and control of hypertension in a general population sample of 26,913 adults in the Greek EPIC study. Int J Epidemiol.2004; 33: 1345–1352. [DOI] [PubMed] [Google Scholar]
- 91. Mathenge W, Foster A, Kuper H. Urbanization, ethnicity and cardiovascular risk in a population in transition in Nakuru, Kenya: a population based survey. BMC Public Health, 2010; 10: 569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Edwards R, Unwin N, Mugusi F, Whiting D, Rashid S, Kissima J. Hypertension prevalence and care in an urban and rural area of Tanzania. J Hypertens 2000; 18: 145–152 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.