Abstract
Background
We aimed to expand the literature on child obesity and school outcomes by examining associations between obesity and high school dropout, including the role of obesity onset and duration as well as ethnicity.
Methods
Data on 5066 children obtained between 1986 and 2010 from the child cohort of the 1979 National Longitudinal Study of Youth (NLSY79) were analyzed. Group-based trajectory analysis identified obesity trajectories from 6-18 years. School completion information from age 14 into young adulthood was used to calculate school dropout. Chi-square and pairwise comparison tests were used to identify significant associations between obesity trajectories and school dropout.
Results
Adolescents belonging to an increasing trajectory (adolescent-onset obesity) had a higher likelihood of dropping out of high school compared to those belonging to chronic, decreasing (childhood-only obesity), and non-obese trajectories. This association was particularly salient among white adolescents.
Conclusions
Obesity onset during early adolescence increased risk of high school dropout. White adolescents were particularly vulnerable. Given that early adolescence is marked by significant biological and social changes, future research should seek to identify the underlying processes linking adolescent-obesity and school dropout to decrease school dropout risk among this vulnerable population.
Keywords: early adolescence, ethnic differences, obesity, school dropout, social acceptance
Both obesity and school dropout rates are significant problems faced by schools across the United States (US). The prevalence of child obesity has substantially increased in past decades,1 with estimates during 2009-2010 showing rates have leveled off but remain high among children 6-19 years (18.2%).2 Although school dropout rates have decreased, estimates from 2012 indicate that about 7% of 16-to-24-year-olds are neither enrolled in high school nor have completed a high school credential.3 As the role of physical health on school outcomes has begun to gain widespread attention among educators, researchers, and public policymakers4-7 a growing literature examining associations between obesity on academic achievement has identified obesity as a potential marker of negative school outcomes.8-12 However, this line of inquiry has not expanded to include school dropout, which is somewhat surprising as school dropout is strongly tied to poor academic performance and school disengagement.13,14 Determining whether obesity predicts school dropout is likely to inform prevention efforts aimed at improving school outcomes among an increasingly salient at-risk group. Furthermore, considering developmental timing and duration of obesity as well as established ethnic disparities within obesity and school dropout is likely to elucidate associations between physical health and school outcomes.
Previous research examining associations between child obesity and school outcomes is vital for understanding potential links between obesity and school dropout, as poorer school achievement and school disengagement increases risk of dropout. Past studies have indicated that child obesity is related to poorer academic achievement.6,15,16 For instance, increasing body mass index (BMI) and obesity status have been found to be negatively related to math, reading, and language scores among large samples of ethnically-diverse children and adolescents.8,9,17 Additionally, national samples have reported that adolescents at risk for and meeting obesity status have lower grade point averages than non-obese adolescents.8,11,12,18 Furthermore, obesity has been linked to greater school disengagement, including greater absenteeism, expectations to quit school, and identification as poorer students.19-22 Potentially, long-term school disengagement and poorer school achievement among obese children may ultimately culminate in school dropout. One reason why studies have yet to examine school dropout rates is the lack of longitudinal studies measuring obesity from childhood and school outcomes into young adulthood.
In addition to evaluating whether child obesity poses a risk for school dropout, a more nuanced question is whether onset or duration of obesity during specific developmental periods increases the risk of school dropout. Although the literature is limited, past studies suggest that chronic obesity poses a greater risk of negative psychosocial outcomes compared to more acute forms of obesity.23,24 Given these findings, chronic obesity as opposed to more acute forms of obesity may pose a greater risk of school dropout. In other words, if negative consequences of obesity accumulate in magnitude over time, chronically obese children (children meeting obesity status across childhood and adolescence) may experience a higher school dropout rate compared to those children who only meet obesity status during childhood or adolescence.
Moreover, taking into account ethnic disparities that exist among both child obesity and school dropout is likely to inform potential ethnic differences on obesity and school dropout. Generally, white children are at lower risk for obesity and school dropout compared to African-American and Latino children. African-American and Latino children have higher rates of obesity (25.7% and 22.9%, respectively) and school dropout (8.6% and 12.7%, respectively) compared to white children (15.2% for obesity and 4.3% for school dropout).2,3 These ethnic disparities often have been explained by the overrepresentation of ethnic minorities living in resource-deprived neighborhoods, where means to engage children in school and physical activity, and access to nutritional food, are more limited.25-27 This lack of resources may help explain potential links between childhood obesity and school dropout among African Americans and Latinos.19 However, prior to identifying underlying processes, determining whether ethnic differences exist must first be addressed.
Our current study sought to examine associations between childhood obesity and school dropout by utilizing a subsample of 5066 children from the child cohort of the National Longitudinal Study of Youth (NLSY79). Using obesity data across 6-18 years and school completion information starting at age 14, we conducted group-based trajectory analyses to determine whether: (1) child obesity is associated with school dropout; (2) specific onset and duration of obesity during the developmental periods of childhood and adolescence increases risk of school dropout; and (3) certain ethnic groups are more vulnerable to school dropout as a result of obesity status. We hypothesized that children belonging to a trajectory characterized by chronic obesity status (obese across childhood and adolescence) would be most likely to drop out of school compared to other obese and non-obese trajectory groups. We also expected that African-American and Latino children belonging to obesity trajectories would be at greater risk of school dropout compared to white children belonging to obesity groups.
Methods
Participants
We utilized data from 5066 children recruited from mother respondents of the 1979 National Longitudinal Survey of Youth (NLSY79). Since 1986, children of mother respondents have been interviewed biennially to provide information on children's physical, psychosocial, and educational outcomes. Informed consent was obtained from caregivers and assent from children. Additional information on study procedures can be found at https://www.nlsinfo.org/content/cohorts/nlsy79-children. In 1986, 4971 children were interviewed. Newborn children were added in each subsequent wave. By 2010, 11,504 children had participated. Data from 13 waves of surveys (1986-2010) were integrated and examined for the current study.
Although 11,504 children were interviewed, 44% were part of a younger birth cohort (those born after 1992) that had not reached adolescence by the time of assessment in 2010. Consequently, obesity trajectories were not estimated for these children, as the estimated trajectory may not be an accurate indicator of obesity across childhood and adolescence. To ensure sufficient data on each child to estimate his/her obesity status trajectory accurately from age 6 to18, only children who had 8 or more waves of data on obesity status were included in the analysis. Additionally, children who were currently enrolled in high school during the last available wave of the survey (2010) were excluded from this school dropout analysis because their high school completion status was not yet available (N = 90). Consequently, a total of 5066 participants were included in the analytic sample (50.1% female; 41.3% white; 35.1% African-American; 21.8% Latino; 1.8% other).
Instrumentation
Obesity status
Obesity status at each wave of assessment was measured with body mass index (BMI; kg/m2). Using BMI scores calculated with self-reported height and weight (mother report used between 6-9 years), age- and sex-specific BMI percentiles were obtained with the Centers for Disease Control and Prevention (CDC) 2000 growth charts.28 Children with a BMI percentile at or above 95% met obesity status at the given wave of assessment (1 = obese, 0 = not obese). To identify trajectories of obesity from ages 6 to 18 (with age intervals of 2 years), obesity status across 13 waves of data (1986-2010) were temporally rearranged based upon the participant's age at each interview. For example, obesity status at age 6 was obtained from a corresponding wave of interviews at which the respondent was age 6.
School dropout
Starting at age 14 and continuing at every wave of assessment, adolescents were asked about their school enrollment and completion status. To create a school dropout variable, a question asking participants whether they had completed high school or obtained an equivalent credential was used. Specifically, respondents were asked: “Do you have a high school diploma or have you ever passed a high school equivalency or GED test?” Responses across multiple waves of surveys were cross checked to determine whether an adolescent had completed high school or its equivalency by the end of the observation period (2010). As previously stated, those who were still enrolled in high school at the last wave of assessment (2010) were excluded (N = 90) from school dropout analyses. Of the 5066 participants with school dropout information available, 100% were age 18 or older, and 97% were age 20 or older by the end of the observation period.
Data Analysis
Using the SAS PROC TRAJ procedure29 group-based trajectory modeling30 was conducted to identify trajectory groups based on obesity status from 6-18 years and evaluate whether specific trajectories were associated with higher rates of school dropout. Using presence or absence of obesity (BMI ≥ 95%) at each age interval (2 years), a logit model was applied to estimate distinctive longitudinal patterns of obesity from ages 6 to 18. Maximum likelihood was used to estimate model parameters. Trajectories of obesity status were indicated by curvilinear curves with intercept, slope, and quadratic parameters; sex and ethnicity were also included as time-invariant covariates in the model. Each individual was placed into one trajectory group based upon estimated membership probabilities. A similar procedure was conducted previously to identify obesity trajectories in a larger subsample of the NLSY79 child cohort without inclusion of ethnicity or sex covariates to assess model fit.31 To identify the best-fitting class model, a series of models with increasing number of trajectory groups was separately fitted. Among these models, the optimal model was determined based on the Bayesian Information Criterion (BIC),32 as well as interpretability and distinctiveness of classes. To assess associations between obesity trajectories and school dropout, first a chi-square test was conducted to examine school dropout rates among the identified trajectory groups and then pairwise comparisons with the least-significant-difference procedure were applied to identify differences between each trajectory group pair. Following this, stratified analyses by ethnicity were conducted to assess ethnic differences in associations between obesity trajectories and school dropout.
Results
Obesity Trajectories
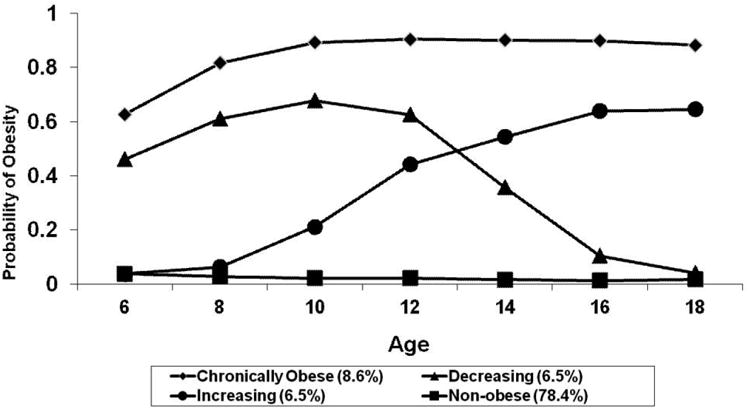
Increasing group models from 2 to 6 trajectories were separately fitted to identify the optimal model. The BIC value increased from -9128.9 in the 2-trajectory model to -8868.2 in the 4-trajectory model, and then decreased to -8870.0 in the 5-trajectory model. The 6-trajectory model did not converge. Given that the 4-trajectory model had the highest BIC value, and interpretable and distinct groups, the 4-trajectory model was chosen as the best-fitting model. Figure 1 illustrates the 4 identified obesity trajectories. The majority of individuals (78.4%) were classified into a non-obese trajectory group, representing those who did not meet obesity status across childhood and adolescence (6-18 years). The remaining 3 trajectories correspond to individuals meeting obesity status at some point during childhood or adolescence. Individuals with a high probability of meeting obesity status across both childhood and adolescence were classified into a chronically obese trajectory (8.6%). Another 6.5% were classified into a decreasing trajectory (childhood-only obesity). This group was characterized by individuals generally meeting obesity status in childhood (6-9 years) with a gradual decrease in obesity status from early adolescence (age 10). The remaining 6.5% belonged to an increasing trajectory (adolescent-onset obesity). This group represented individuals who generally did not meet obesity status in childhood but whose obesity risk increased from early adolescence.
Figure 1. Trajectories of Obesity (N = 5066).
School Dropout Rate by Obesity Trajectory
The upper portion of Table 1 presents school dropout rates by obesity trajectory group and significant differences between trajectory groups on school dropout rates. Overall, 13.8% of participants did not complete high school or its equivalency. School dropout rates significantly differed among the four trajectory groups (χ2(3) = 8.11, p < .05). Those in the Increasing trajectory group reported the highest rate of school dropout (19.6%); followed by the chronically obese (14.1%), decreasing (13.5%), and non-obese (13.4%) trajectory groups. Pairwise comparisons on school dropout rates between each pair of trajectory groups indicated that individuals belonging to the Increasing trajectory compared to the chronically obese, Decreasing and non-obese trajectories, respectively, were significantly (p < .05) less likely to complete high school or its equivalency.
Table 1. School Dropout by Obesity Trajectories and Stratified by Ethnicity.
| Chronically obese (N = 440) | Decreasing (N = 289) | Increasing (N = 266) | Non-obese (N = 4071) | Total (N = 5066) | |
|---|---|---|---|---|---|
| School dropout (%) *, IC, ID, IN | 14.1 | 13.5 | 19.6 | 13.4 | 13.8 |
|
| |||||
| School dropout for each ethnic stratum | |||||
| African-American (N) | 207 | 107 | 121 | 1,345 | 1,780 |
| School dropout (%) | 12.6 | 12.2 | 19.0 | 13.6 | 13.8 |
| Hispanic (N) | 92 | 73 | 52 | 887 | 1,104 |
| School dropout (%) | 21.7 | 19.2 | 21.2 | 17.7 | 18.3 |
| White (N) | 132 | 107 | 84 | 1,769 | 2,092 |
| School dropout (%), IN | 11.4 | 10.3 | 17.9 | 10.6 | 10.9 |
Significant chi-square test among the 4 trajectory groups is indicated by * p < .05.
Significant pairwise comparisons (p < .05) between each pair of trajectory groups are indicated by IC (Increasing vs. Chronically obese), ID (Increasing vs. Decreasing), and IN (Increasing vs. Non-obese).
Obesity and School Dropout by Ethnicity
The lower portion of Table 1 presents school dropout rates by trajectories and significant pairwise comparisons on school dropout rates by ethnicity. African Americans (24.4%) were more likely to be classified into one of the 3 obesity trajectories (chronically obese, decreasing, or increasing) versus the non-obesity trajectory, compared to Latinos (19.6%) and Whites (15.4%). In terms of school dropout rates, Latinos had the highest rate (18.3%), followed by African Americans (13.8%) and Whites (10.9%). Comparing across all obesity trajectories, school dropout rates did not significantly differ among African Americans (χ2(3) = 3.32, p > .05), Latinos (χ2(3) = 1.26, p > .05), or Whites (χ2(3) = 4.37, p > .05); however, significant pairwise comparisons (p < .05) were found among Whites. White adolescents belonging to the Increasing trajectory group were less likely to complete high school or its equivalency than those belonging to the non-obese trajectory group.
Discussion
Given the growing interest in examining associations between obesity and school outcomes,6,19 we sought to expand this line of inquiry by evaluating whether obesity status was related to school dropout. Results indicated that obesity status was associated with an increase risk of school dropout, with timing and duration of obesity as well as ethnicity playing a significant role. Trajectory groups based on obesity status across childhood and adolescence revealed that obesity onset and persistence in adolescence was associated with a greater school dropout rate compared to other trajectory groups. Furthermore, findings suggest this may be more specific among Whites compared to African Americans and Latinos. Although these findings highlight a significant relationship between obesity and school outcomes that is specific to developmental timing of obesity and ethnicity, the underlying mechanisms explaining these associations requires further research.
We expected that a trajectory characterized by chronic obesity in childhood and adolescence would be most predictive of school dropout compared to other obesity and non-obesity trajectories, given past studies indicating more chronic forms of child obesity pose greater risk for poorer developmental outcomes.23,24 In contrast, findings revealed that higher school dropout rates were linked to the trajectory group characterized by obesity emerging in early adolescence and continuing across adolescence, not the trajectory group characterized by obesity emerging in childhood and persisting across childhood and adolescence. Previous studies focused on obesity and school outcomes prior to middle school have indicated weaker relations compared to adolescence,33-35 suggesting adolescent-onset obesity is a unique contributor to school failure. Furthermore, school dropout rates were higher among this adolescent-onset trajectory group compared to the non-obese group, highlighting obesity as a potential marker of school dropout. However, the reasons for why adolescent-onset obesity is particularly associated with higher school dropout rates are currently unknown. Potentially, biological and socio-contextual changes occurring during the transition between childhood and adolescence may inform the relationship between adolescent-onset obesity and school dropout.
Recognizing that obesity emerging in early adolescence is particularly problematic for high school completion is critical for understanding how obesity ultimately impacts school outcomes. The results from the current study turn our attention to the developmental transition from childhood to adolescence, and how obesity-onset during this unique developmental period may have a long-lasting negative impact. A combination of both biological and socio-cultural processes is likely to explain why obesity onset in early adolescence is specifically linked to higher risk of school dropout. Potentially, significant weight gain resulting from physiological changes associated with puberty and increasing important placed on social standing among peers may be significant processes linking adolescent-onset obesity to school dropout. Some studies have indicated significant associations between increased BMI and poorer cognitive functioning among adolescents, which may be especially problematic for obese youth as adolescence marks a period of heightened cognitive development.36,37 Furthermore, for those transitioning into adolescence earlier onset of puberty is not only associated with obesity onset, particularly among girls,38 but it is also a predictor of risk behaviors among both boys and girls, including high-risk substance use, sexual risk-taking, deviant peer affiliation, and school truancy, which contribute to risk of school dropout.39 Because early adolescence is characterized as a period of heightened social awareness, fitting in with social norms and having positive social standing among peers becomes critically important.40,41 Obese adolescents are less likely to be socially accepted by peers because they do not fit social norms for physical appearance.42-44 Obese adolescents may disengage from school in order to avoid negative social interactions with peers.45,46 Adolescents becoming obese during early adolescence versus childhood may be at a significant disadvantage because they have not had time to develop adaptive coping strategies.
In addition to the various developmental processes occurring in early adolescence that may inform the relationship between adolescent-onset obesity and higher risk of school dropout, future research also needs to consider the role of ethnicity. Although we expected the relationship between obesity and school dropout to be more salient among African Americans and Latinos given the higher proportion of rates among these groups,2,3 membership in an obesity trajectory was not related to school dropout among African Americans or Latinos. On the other hand, white adolescents characterized by adolescent-onset obesity had higher rates of dropout compared to white adolescents never meeting obesity status. Because adolescent-onset obesity was again specifically associated with school dropout, ethnic differences in pubertal onset and social stigmatization of obesity may largely explain this finding. On average, African-American and Latina girls experience earlier pubertal onset than white girls;47,48 consequently, white girls experiencing earlier onset puberty and increased risk of obesity may be more likely to encounter negative developmental outcomes because it is less normative for their ethnic group. Moreover, there is some research to suggest that greater significance is placed on body size among white adolescents than African-American and Latino adolescents,49,50 which may explain why obese white adolescents experience poorer peer status than their non-obese counterparts.51,52 The greater social stigma placed on white individuals meeting obesity status versus ethnic-minorities likely contributes to decreased social acceptance among White adolescents during a developmental period when social standing is critical to psychosocial adjustment and future school outcomes.
Limitations
Several limitations need to be considered. First, although differences in reliability between self-reported and measured BMI among children and adolescents have been found to be minor,53-55 self-reported height and weight data were used in this study. Second, just under half (44%) of the children born to mothers in the NLSY79 study were not included in the current study as a result of being born in later stages of the study; thus, these children did not have sufficient data to estimate obesity trajectories from 6-18 years. In addition, 90 participants with available obesity trajectory data were still in high school during the last wave of analysis for the current study and, thus, excluded from school dropout analyses. However, the remaining sample was sufficient to identify obesity trajectories and prevalence rates similar to what has been reported previously in an epidemiological sample.24 Third, we must acknowledge that some participants who dropped out of school but later returned or completed an equivalency were included in the non-dropout group, although this number is suspected to be small. Last, the study sought to identify links between obesity and high school dropout, but the lack of knowledge about the influence of biological and socio-contextual factors increases difficulty in knowing the direct impact of obesity on school outcomes.
Conclusions
Our study utilized a large, ethnically-diverse longitudinal sample of US children to identify patterns of obesity across childhood and adolescence, assess whether specific developmental trajectories are associated with higher school dropout rates, and also evaluate potential ethnic differences among associations. Two findings from this study substantially inform the relationship between obesity and high school dropout. First, findings show that individuals who begin to meet obesity status around early adolescence (adolescent-onset obesity) are more vulnerable to dropping out of high school compared to others experiencing chronic obesity (obesity across childhood and adolescence), a decreasing obesity trajectory (childhood-only obesity), and those never meeting obesity status in childhood or adolescence. Potentially, the high significance placed on social status during early adolescence combined with significant physiological changes as a result of puberty may have an especially adverse impact on those becoming obese during this transitional period. Second, it appears that associations between obesity and school dropout may be particularly important for white adolescents with adolescent-onset obesity, which may ultimately be explained by greater social stigma placed on white versus African-American or Latino adolescents meeting obesity status. Future empirical work should consider the processes and pathways by which obesity is linked to school dropout, with a specific emphasis on developmental timing of obesity and ethnic differences among associations.
Implications for School Health
Evidence implicates child obesity as a risk factor for poorer academic performance, as well other maladaptive physical and psychosocial outcomes. To reduce risk and prevalence of child obesity, schools have become a primary vehicle by which prevention and intervention programs are delivered. Many of these programs have seen at least partial success in decreasing obesity risk,56-58 increasing the belief that the school context can have significant influence over children's health. Our study shows that obesity is associated with high school dropout, which is seen by many as the ultimate performance outcome for the K-12 educational system. Importantly, the findings give schools a specific subgroup of students to focus prevention/intervention efforts on white adolescents that become obese during the middle school years, as they appear to be most vulnerable to dropout as a result of weight status. Additionally, school administrators, health professionals, and teachers can have an invaluable role in providing information on potential underlying processes linking obesity to school dropout. For instance, school professionals have a unique perspective of how physical characteristics, whether it be weight gain, emerging secondary sexual characteristics, or ethnicity, can affect children's academic performance through its impact on social standing among peers. Future research should seek to actively use knowledge from health professionals to develop studies that will increase understanding of how obesity is related to school dropout.
Acknowledgments
This study was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (R03HD064619) and the National Institute of Drug Abuse (RO3DA033497; P30DA016383; T32DA007272).
Footnotes
Human Subjects Approval Statement: This study was exempted from institutional review as it utilized a publically available dataset without identification data.
Contributor Information
H. Isabella Lanza, Email: Isabella.Lanza@csulb.edu, California State University, Long Beach, Human Development, 1250 Bellflower Blvd., LA3-202, Long Beach, CA 90804, USA, Phone: (562) 985-6498, Fax: (562) 985-4237.
David Y.C. Huang, Email: yhuang@ucla.edu, University of California, Los Angeles, Semel Institute for Neuroscience and Human Behavior, Integrated Substance Abuse Programs, 11075 Santa Monica Blvd., Suite 200, Los Angeles, CA 90025, USA, Phone: (310) 267-5288, Fax: (310) 312-0538.
References
- 1.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999- 2002. JAMA. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009-2010. JAMA. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Child Trends. High school dropout rates. [Accessed August 4, 2014];2013 Available at: http://www.childtrends.org/?indicators=high-school-dropout-rates.
- 4.Foster GD, Sherman S, Borradaile KE, Grundy KM, Vander Veur SS, Nachmani J, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. 2008;121(4):e794–e802. doi: 10.1542/peds.2007-1365. [DOI] [PubMed] [Google Scholar]
- 5.Shaya FT, Flores D, Gbrarayor CM, Wang J. School-based obesity interventions: a literature review. J Sch Health. 2008;78(4):189–196. doi: 10.1111/j.1746-1561.2008.00285.x. [DOI] [PubMed] [Google Scholar]
- 6.Taras H, Potts-Datema W. Obesity and student performance at school. J Sch Health. 2005;75(8):291–295. doi: 10.1111/j.1746-1561.2005.00040.x. [DOI] [PubMed] [Google Scholar]
- 7.Winter SM, Sass DA. Healthy & ready to learn: examining the efficacy of an early approach to obesity prevention and school readiness. J Res Child Educ. 2011;25(3):304–325. [Google Scholar]
- 8.Crosnoe R, Muller C. Body mass index, academic achievement, and school context: examining the educational experiences of adolescents at risk of obesity. J Health Soc Behav. 2004;45(4):393–407. doi: 10.1177/002214650404500403. [DOI] [PubMed] [Google Scholar]
- 9.Datar A, Sturm R, Magnabosco IL. Childhood overweight and academic performance: national study of kindergartners and first-graders. Obes Res. 2004;12(1):56–68. doi: 10.1038/oby.2004.9. [DOI] [PubMed] [Google Scholar]
- 10.Roberts CK, Freed B, McCarthy WJ. Low aerobic fitness and obesity are associated with lower standardized test scores in children. J Pediatr. 2010;156(5):711–718. doi: 10.1016/j.jpeds.2009.11.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shore SM, Sachs ML, Lidicker JR, Brett SN, Wright AR, Libonati JR. Decreased scholastic achievement in overweight middle school students. Obesity. 2008;16(7):1535–1538. doi: 10.1038/oby.2008.254. [DOI] [PubMed] [Google Scholar]
- 12.MacCann C, Roberts RD. Just as smart but not as successful: obese students obtain lower school grades but equivalent test scores to nonobese students. Int J Obes. 2013;37(1):40–46. doi: 10.1038/ijo.2012.47. [DOI] [PubMed] [Google Scholar]
- 13.Christenson SL, Thurlow ML. School dropouts: prevention considerations, interventions, and challenges. Curr Dir Psychol Sci. 2004;13(1):36–39. [Google Scholar]
- 14.Garnier HE, Stein JA, Jacobs JK. The process of dropping out of high school: a 19-year perspective. Am Educ Res J. 1997;34(2):395–419. [Google Scholar]
- 15.Arora T, Hosseini-Araghi M, Bishop J, Yao GL, Thomas GN, Taheri S. The complexity of obesity in UK adolescents: relationships with quantity and type of technology, sleep duration and quality, academic performance and aspiration. Pediatr Obes. 2012;8(5):358–366. doi: 10.1111/j.2047-6310.2012.00119.x. [DOI] [PubMed] [Google Scholar]
- 16.Kamijo K, Khan NA, Pontifex MB, Scudder MR, Drollette ES, Raine LB, et al. The relation of adiposity to cognitive control and scholastic achievement in preadolescent children. Obesity. 2012;20(12):2406–2411. doi: 10.1038/oby.2012.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gable S, Krull JL, Chang Y. Boys' and girls' weight status and math performance from kindergarten entry through fifth grade: a mediated analysis. Child Dev. 2012;83(5):1822–1839. doi: 10.1111/j.1467-8624.2012.01803.x. [DOI] [PubMed] [Google Scholar]
- 18.Judge S, Jahns L. Association of overweight with academic performance and social and behavioral problems: an update from the Early Childhood Longitudinal Study. J Sch Health. 2007;77(10):672–678. doi: 10.1111/j.1746-1561.2007.00250.x. [DOI] [PubMed] [Google Scholar]
- 19.Daniels DY. Examining attendance, academic performance, and behavior in obese adolescents. J Sch Nurs. 2008;24(6):379–387. doi: 10.1177/1059840508324246. [DOI] [PubMed] [Google Scholar]
- 20.Falkner NH, Neumark-Sztainer D, Story M, Jeffery RW, Beuhring T, Resnick MD. Social, educational, and psychological correlates of weight status in adolescents. Obes Res. 2001;9(1):32–42. doi: 10.1038/oby.2001.5. [DOI] [PubMed] [Google Scholar]
- 21.Li Y, Raychowdhury S, Tedders SH, Lyn R, Lòpez-De Fede A, Zhang J. Association between increased BMI and severe school absenteeism among US children and adolescents: findings from a national survey, 2005-2008. Int J Obes. 2012;36(4):517–523. doi: 10.1038/ijo.2012.15. [DOI] [PubMed] [Google Scholar]
- 22.Pan L, Sherry B, Park S, Blanck HM. The association of obesity and school absenteeism attributed to illness or injury among adolescents in the United States, 2009. J Adolesc Health. 2013;52(1):64–69. doi: 10.1016/j.jadohealth.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Datar A, Sturm R. Childhood overweight and elementary school outcomes. Int J Obes. 2006;30(9):1449–1460. doi: 10.1038/sj.ijo.0803311. [DOI] [PubMed] [Google Scholar]
- 24.Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003;111(4 Pt 1):851–859. doi: 10.1542/peds.111.4.851. [DOI] [PubMed] [Google Scholar]
- 25.Eccles JS, Roeser RW. Schools, academic motivation, and stage-environment fit. In: Lerner R, Steinberg L, editors. Handbook of Adolescent Psychology. 3rd. New York, NY: Wiley; 2009. pp. 404–434. [Google Scholar]
- 26.Kwate NO. Fried chicken and fresh apples: racial segregation as a fundamental cause of fast food density in black neighborhoods. Health Place. 2008;14(1):32–44. doi: 10.1016/j.healthplace.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 27.Reidpath DD, Burns C, Garrard J, Mahoney M, Townsend M. An ecological study of the relationship between social and environmental determinants of obesity. Health Place. 2002;8(2):141–145. doi: 10.1016/s1353-8292(01)00028-4. [DOI] [PubMed] [Google Scholar]
- 28.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC Growth Charts: United States. Adv Data. 2000;(No.314):1–27. [PubMed] [Google Scholar]
- 29.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Socio Meth Res. 2001;29(3):374–393. [Google Scholar]
- 30.Nagin DS. Group-based Modeling of Development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 31.Huang DYC, Lanza HI, Wright-Volel K, Anglin MD. Developmental trajectories of childhood obesity and risk behaviors in adolescence. J Adolesc. 2013;36(1):121–128. doi: 10.1016/j.adolescence.2012.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schwartz G. Estimating the dimension of a model. Ann Stat. 1978;6(2):461–464. [Google Scholar]
- 33.Bisset S, Fournier M, Pagani L, Janosz M. Predicting academic and cognitive outcomes from weight status trajectories during childhood. Int J Obes. 2013;37(1):154–159. doi: 10.1038/ijo.2012.106. [DOI] [PubMed] [Google Scholar]
- 34.LeBlanc MM, Martin CK, Han H, Newton R, Sothern M, Webber LS, et al. Adiposity and physical activity are not related to academic achievement in school-aged children. J Dev Behav Pediatr. 2012;33(6):486–494. doi: 10.1097/DBP.0b013e31825b849e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li J, O'Connell AA. Obesity, high-calorie food intake, and academic achievement trends among U.S. school children. J Educ Res. 2012;105(6):391–403. [Google Scholar]
- 36.Maayan L, Hoogendoom C, Sweat V, Convit A. Disinhibited eating in obese adolescents is associated with orbitofrontal volume reductions and executive dysfunction. Obesity. 2011;19(7):1382–1387. doi: 10.1038/oby.2011.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schwartz DH, Leonard G, Perron M, Richer L, Syme C, Veillette S, et al. Visceral fat is associated with lower executive functioning in adolescents. Int J Obes. 2013;37(10):1336–1343. doi: 10.1038/ijo.2013.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jasik CB, Lustig RH. Adolescent obesity and puberty: the “perfect storm”. Ann N Y Acad Sci. 2008;1135:265–279. doi: 10.1196/annals.1429.009. [DOI] [PubMed] [Google Scholar]
- 39.Downing J, Bellis M. Early pubertal onset and its relationship with sexual risk taking, substance use and anti-social behaviour: a preliminary cross-sectional study. BMC Public Health. 2009;9:446–457. doi: 10.1186/1471-2458-9-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Eccles JS. The development of children ages 6 to 14. Future Child. 1999;9(2):30–44. [PubMed] [Google Scholar]
- 41.Fulgni AJ, Eccles JS, Barber BL, Clements P. Early adolescent peer orientation and adjustment during high school. Dev Psychol. 2001;37(1):28–36. [PubMed] [Google Scholar]
- 42.LaFontana KM, Cillessen AHN. Developmental changes in the priority of perceived status in childhood and adolescence. Soc Dev. 2010;19(1):130–147. [Google Scholar]
- 43.Strauss RS, Pollack HA. Social marginalization of overweight children. Arch Pediatr Adolesc Med. 2003;157(8):746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- 44.Latner JD, Stunkard AJ. Getting worse: the stigmatization of obese children. Obes Res. 2003;11(3):452–456. doi: 10.1038/oby.2003.61. [DOI] [PubMed] [Google Scholar]
- 45.Geier A, Foster G, Womble L, McLaughlin J, Borradaile KE, Nachmani J, et al. The relationship between relative weight and school attendance among elementary school children. Obesity. 2007;15(8):2157–2161. doi: 10.1038/oby.2007.256. [DOI] [PubMed] [Google Scholar]
- 46.Krukowski RA, West DS, Philyaw Perez A, Bursac Z, Phillips MM, Raczynski JM. Overweight children, weight-based teasing and academic performance. Int J Pediatr Obes. 2009;4(4):274–280. doi: 10.3109/17477160902846203. [DOI] [PubMed] [Google Scholar]
- 47.Kaplowitz PB, Slora EJ, Wasserman RC, Pedlow SE, Herman-Giddens ME. Earlier onset of puberty in girls: relation to increased body mass index and race. Pediatrics. 2001;108(2):347–353. doi: 10.1542/peds.108.2.347. [DOI] [PubMed] [Google Scholar]
- 48.Salsberry PJ, Reagan PB, Pajer K. Growth differences by age of menarche in African American and White girls. Nurs Res. 2009;58(6):382–390. doi: 10.1097/NNR.0b013e3181b4b921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Latner JD, Stunkard AJ, Wilson GT. Stigmatized students: age, sex, and ethnicity effects in the stigmatization of obesity. Obes Res. 2005;13(7):1226–1231. doi: 10.1038/oby.2005.145. [DOI] [PubMed] [Google Scholar]
- 50.van den Berg P, Neumark-Sztainer D, Eisenberg M, Haines J. Racial/ethnic differences in weight-related teasing in adolescents. Obesity. 2008;16(Suppl 2):S3–S10. doi: 10.1038/oby.2008.445. [DOI] [PubMed] [Google Scholar]
- 51.BeLue R, Francis LA, Colaco B. Mental health problems and overweight in a nationally representative sample of adolescents: effects of race and ethnicity. Pediatrics. 2009;123(2):697–702. doi: 10.1542/peds.2008-0687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lanza HI, Echols L, Graham S. Deviating from the norm: body mass index (BMI) differences and psychosocial adjustment among early adolescent girls. J Pediatr Psychol. 2013;38(4):376–386. doi: 10.1093/jpepsy/jss130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brener ND, McManus T, Galuska DA, Lowry R, Wechsler H. Reliability and validity of self-reported height and weight among high school students. J Adolesc Health. 2003;32(4):281–287. doi: 10.1016/s1054-139x(02)00708-5. [DOI] [PubMed] [Google Scholar]
- 54.Field AE, Aneja P, Rosner B. The validity of self-reported weight change among adolescents and young adults. Obesity. 2007;15(9):2357–2364. doi: 10.1038/oby.2007.279. [DOI] [PubMed] [Google Scholar]
- 55.Goodman E, Hinden BR, Khandewal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106(1 Pt 1):52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- 56.Hollar D, Lombardo M, Lopez-Mitnik G, Hollar TL, Almon M, Agatston AS, et al. Effective multi-level, multi-sector, school-based obesity prevention programming improves weight, blood pressure, and academic performance, especially among low-income, minority children. J Health Care Poor Underserved. 2010;21(2):93–108. doi: 10.1353/hpu.0.0304. [DOI] [PubMed] [Google Scholar]
- 57.Johnston CA, Moreno JP, El-Mubasher A, Gallagher M, Tyler C, Woehler D. Impact of a school-based pediatric obesity prevention program facilitated by health professionals. J Sch Health. 2013;83(3):171–181. doi: 10.1111/josh.12013. [DOI] [PubMed] [Google Scholar]
- 58.Prelip M, Slusser W, Thai CL, Kinsler J, Erausquin JT. Effects of a school-based nutrition program diffused throughout a large urban community on attitudes, beliefs, and behaviors related to fruit and vegetable consumption. J Sch Health. 2011;81(9):520–529. doi: 10.1111/j.1746-1561.2011.00622.x. [DOI] [PubMed] [Google Scholar]


