Abstract
Background
Cognitive behavioral therapy (CBT) can be delivered efficaciously through various modalities, including telephone (T-CBT) and face-to-face (FtF-CBT). The purpose of this study was to explore predictors of outcome in T-CBT and FtF-CBT for depression.
Method
A total of 325 depressed participants were randomized to receive eighteen 45-min sessions of T-CBT or FtF-CBT. Depression severity was measured using the Hamilton Depression Rating Scale (HAMD) and the Patient Health Questionnaire-9 (PHQ-9). Classification and regression tree (CART) analyses were conducted with baseline participant demographics and psychological characteristics predicting depression outcomes, HAMD and PHQ-9, at end of treatment (week 18).
Results
The demographic and psychological characteristics accurately identified 85.3% and 85.0% of treatment responders and 85.7% and 85.0% of treatment non-responders on the HAMD and PHQ-9, respectively. The Coping self-efficacy (CSE) scale predicted outcome on both the HAMD and PHQ-9; those with moderate to high CSE were likely to respond with no other variable influencing that prediction. Among those with low CSE, depression severity influenced response. Social support, physical functioning, and employment emerged as predictors only for the HAMD, and sex predicted response on the PHQ-9. Treatment delivery method (i.e. telephone or face-to-face) did not impact the prediction of outcome.
Conclusions
Findings suggest that the predictors of improved depression are similar across treatment modalities. Most importantly, a moderate to high level of CSE significantly increases the chance of responding in both T-CBT and FtF-CBT. Among patients with low CSE, those with lower depressive symptom severity are more likely to do well in treatment.
Keywords: CART, CBT, depression, outcome, predictors, telephone therapy
Introduction
Depressive disorders are common mental health affiictions. In the United States alone, lifetime morbid risk of major depressive disorder is 29.9% and the 12-month prevalence is estimated to be between 6.6% and 10.3% (Kessler et al. 2003, 2005, 2012; Reeves et al. 2011). Psychological treatments for depression are effective (Cuijpers et al. 2008) and desirable to patients (Priest et al. 1996; Brody et al. 1997; Bedi et al. 2000; Churchill et al. 2000; Dwight-Johnson et al. 2000). Cognitive behavioral therapy (CBT) is the most studied psychotherapy for the treatment of depression and carries the strongest body of evidence for its effectiveness (Dobson, 1989; Butler et al. 2006; Cuijpers et al. 2013). Increasingly, the delivery of CBT through different media has been investigated, including via telephone (Mohr et al. 2005), internet websites (Andersson & Cuijpers, 2009), and bibliotherapy (Cuijpers, 1997). While CBT is effective when delivered across many different media, improvement is not inevitable in any of them.
A vast literature of baseline predictors of outcome for CBT for depression exists. Most predictors tend to be prognostic indicators, or factors that identify patients that may do better in treatment in general. Positive outcomes are often found among patients with: (1) lower symptom severity (Jarrett et al. 1991; Sotsky et al. 1991; Shapiro et al. 1994; Thase et al. 1994; Agosti & Ocepek-Welikson, 1997; Persons et al. 1999; Hamilton & Dobson, 2002; Coffman et al. 2007); (2) shorter current episode duration (Sotsky et al. 1991; Rush et al. 1977; Hamilton & Dobson, 2002); (3) absence of family history of depression (Sotsky et al. 1991); (4) older age of initial onset (Jarrett et al. 1991; Sotsky et al. 1991; Agosti & Ocepek-Welikson, 1997; Hamilton & Dobson, 2002); (5) lower number of previous episodes (Sotsky et al. 1991; Hamilton & Dobson, 2002; Bockting et al. 2006; Fournier et al. 2009); and (6) absence of comorbid conditions (Reich et al. 1995; Gelhart & King, 2001; Driessen & Hollon, 2010).
Identifying prognostic variables is difficult and applying them to clinical practice introduces additional challenges. Statistical techniques for identifying moderators are often underpowered to uncover these relationships in individual studies (Brown et al. 2013). Furthermore, most studies explore only a few variables that investigators selected a priori. These findings can then only support that the variable selected was meaningful, but not whether another variable would have been more useful. Practically, clinicians need to know which are the main factors to consider in determining questions of prognosis. However, attempting to predict outcomes from multiple predictors might lead to classification issues especially in cases of high multi-collinearity between predictors. Classification and Regression Tree (CART) analysis is a data-mining technique that uses recursive binary partitioning to select optimal splits of predictor variables to obtain increasingly homogenous groups with respect to the outcome (Breiman et al. 1984; King & Resick, 2014). The benefits of this method over more commonly used analyses for predicting outcomes include the interpretability (i.e. the trees demonstrate if-then conditions that are often considered to be easily interpreted), the capability of including many possible predictor variables, and that these models are robust to violations of normality and linearity to which typical regression models are bound. Thus, CART is an ideal method for exploratory analyses using a broad number of variables.
In exploring predictors of treatment response to CBT, it is important to understand them in the context of different forms of delivery beyond face-to-face (FtF-CBT). The most prominent alternative delivery medium for CBT is via the telephone (T-CBT). For the treatment of depression, T-CBT and FtF-CBT produce similar changes in depression severity at treatment completion (Mohr et al. 2012), and produce similar therapeutic alliance ratings from both the patient and therapist perspectives (Stiles-Shields et al. 2014b). As the use of the telephone to provide psychotherapy becomes more widespread (Novotney, 2011), it will be important to understand whether any subset of patients might be more likely to benefit from a particular approach. A number of studies have examined the usefulness of patient variables, such as marital status, employment status, severity of baseline depression, presence of personality disorders, stress, reactance, and internalizing v. externalizing coping to differentially predict responsiveness to various forms of psychotherapy and pharmacotherapy (Beutler et al. 1991; Dimidjian et al. 2006; Fournier et al. 2008). In addition, people with a diagnosis of co-morbid anxiety at baseline experience less benefit from T-CBT, relative to FtF-CBT (Stiles-Shields et al. 2014a). Thus, it is worth exploring whether predictors of outcome are similar across T-CBT and FtF-CBT.
The primary aim of this study was to use CART analyses to explore patient predictors of response to CBT for depression in T-CBT and FtF-CBT. An exploratory aim of the study was to explore whether patient predictors vary between treatment delivery method (i.e. telephone v. face-to-face).
Method
This study is a secondary analysis of data from a randomized controlled trial comparing the efficacy and retention rates of T-CBT and FtF-CBT in a cohort of 325 depressed participants (Mohr et al. 2012).
Participants
Recruitment of participants occurred from November 2007 to December 2010 from primary-care clinics located in an academic medical center in the Chicago area.
Participants were eligible for randomization if they met criteria for major depressive disorder, had a minimum score of 16 on the Hamilton Depression Rating Scale (HAMD), were at least 18 years of age, spoke English, and were able to participate in face-to-face or telephone therapy. Exclusion criteria included having visual or hearing impairments preventing participation, meeting criteria for depression of an organic etiology or a severe psychiatric disorder, reporting severe alcohol or substance abuse, meeting criteria for dementia; exhibiting severe suicidality (i.e. plan and intent), receiving or planning to receive individual psychotherapy, or initiation of antidepressant pharmaco-therapy in the previous 10 days.
In compliance with the University’s Institutional Review Board, participants were sent a consent form. Research staff reviewed the consent with them over the phone and participants were given an opportunity to ask questions. Consent forms were signed and returned prior to baseline interviews.
Treatments
Participants were randomized to either T-CBT or FtF-CBT, stratified by antidepressant status and research study therapist (n = 9) by a blinded statistician. The treatment delivery medium was the only experimental factor to vary between the two groups, with both treatments using the same CBT protocol (Beck, 1995) adapted and validated for use over the phone (Mohr et al. 2005). To eliminate therapist effects, PhD-level psychologists acted as therapists for both conditions. All therapists received training and supervision from the Beck Institute for Cognitive Behavioral Therapy. All therapy sessions were recorded and 8% were randomly selected and rated by the supervisor on the Cognitive Therapy Rating Scale (Vallis et al. 1986) for fidelity. Further detail of therapist training and fidelity are noted elsewhere (Mohr et al. 2012).
FtF-CBT participants were seen in the Preventive Medicine Clinic at Northwestern University, whereas T-CBT was conducted exclusively via the telephone. Participants in the T-CBT condition received instructions to conduct the telephone sessions in a private, safe, and distraction-free environment. All participants received eighteen 45-min sessions, with two sessions weekly for the first weeks, followed by 12 weekly sessions, and two final booster sessions over 4 weeks. Participants also received a client workbook that explained CBT concepts and provided worksheets for topics including behavioral activation, cognitive restructuring, and social support. Optional chapters addressed common co-morbidities, such as anxiety management, relaxation training, assertiveness training, anger management, and insomnia.
Assessment
CART analyses included measures of depression severity, measured from baseline and end of treatment (week 18). Self-reported depression severity was measured using the Patient Health Questionnaire-9 (PHQ-9; Kroenke & Spitzer, 2002), which has high internal consistency (Cronbach’s alphas were 0.75–0.91 for this trial) and face validity (Corson et al. 2004). Interviewer-based depression severity was evaluated using the 17-item HAMD (Hamilton, 1960). Bachelor-level research assistants, who were trained and supervised by a licensed clinical psychologist, administered the HAMD. To ensure inter-rater reliability, one audio-tape of the HAMD assessment was randomly selected every 1–2 weeks for calibration ratings with all evaluators. The mean interclass correlations were 0.96.
In addition to measures of depression severity, bachelor-level research assistants administered the Mini International Neuropsychiatric Interview (MINI; Sheehan et al. 1997) at baseline over the telephone. This semi-structured diagnostic interview diagnosed any DSM-IV-TR co-morbid conditions (APA, 2000). Baseline data included in the CART analysis included age, sex, ethnicity, race, marital status, education, employment status, household income, antidepressant medication status, trauma and abuse history (Wolfe & Kimberling, 1997), presence of a co-morbid anxiety disorder from the MINI (Sheehan et al. 1997; Stiles-Shields et al. 2014a), the HAMD total score, the PHQ-9 total score, the Insomnia Severity Index total score (ISI; Doghramji, 2006), the Life Experiences Survey total score (LES; Sarason et al. 1978), the Generalized Anxiety Disorder-7 total score (GAD-7; Spitzer et al. 2006), the Alcohol Use Disorders Identification Test total score (AUDIT; Babor et al. 1992), the Positive and Negative Affect Scale total score (PANAS; Watson et al. 1988), Medical Outcomes Study 36 total and subscale (Vitality, Physical Functioning, Bodily Pain, General Health Perceptions, Physical Role Functioning, Emotional Role Functioning, Social Role Functioning, Mental Health) scores (SF-36; Brazier et al. 1992), the Brief Symptom Inventory total and subscale (Somatization, Obsessive-Compulsive, Interpersonal Sensitivity, Depression, Anxiety, Anger-Hostility, Phobic Anxiety, Paranoid Ideation, Psychoticism) scores (Lehman et al. 2012), the Coping Self-Efficacy Scale total score (CSE; Chesney et al. 2006), the Life Stressors and Social Resources total score (LISRES-A; Moos et al. 1988), the Nijmegen Motivation Questionnaire-2 total score (NML-2; Keijsers et al. 1999), Outcome Expectations Questionnaire – Patient Version, Perceived Barriers to Psychotherapy total score (PBP; Mohr et al. 2006), Social Provisions Scale total score (SPS; Russell & Cutrona, 1984), Scale for Interpersonal Behavior total score (SIBS; Arrindell & van der Ende, 1985), Perceived Stress Scale total score (PSS; Cohen et al. 1983), and Apathy Evaluation Scale total score (AES; Marin et al. 1991). Treatment assignment was also included to explore whether predictors would vary as a function of treatment delivery medium.
Data analysis
CART analyses use recursive partitioning algorithms to find optimal ‘splits’ of any variable to separate responders from non-responders. For each systematic split or step, one or more rules are assessed to determine how or whether to proceed down the tree. This process results in a visualization that is reminiscent of an inverted tree, with a single root at the top that leads to branches, finalizing in non-branching leaves at the bottom. Each split or stop in a branch is referred to as a node. Each node denotes a predictor variable critical for that decision point and provides the amount of the sample that were impacted by that variable for the prediction (for a more detailed description of CART analyses in psychological treatment research, see King & Resick, 2014).
CART analyses were conducted with all baseline covariates. Treatment response was defined as end of treatment scores below 16 and 10 for the HAMD and PHQ-9, respectively. The cut-off of 16 on the HAMD was determined as it produces a comparative sample to that of a PHQ-9 cut-off of 10, which is consistent with the MacArthur recommendations for referrals to psychotherapy at the cut-off for mild depressive symptoms (The MacArthur Foundation’s Initiative on Depression and Primary Care, 2004). The cut-offs for both measures create a sample of roughly 2/3 response, which is consistent with response rates for the treatment of depression with CBT (Driessen & Hollon, 2010).
The trees were fit using the rpart package in R version 3.0.1 (R Core Team, 2013), and pruned with a complexity parameter set at the largest value that was within a standard error of the minimum cross-validated error.
For increased understanding and validation of the findings from the CART analyses, Random Forest analyses were also run (Breiman, 2001). Random Forests is a method of generating many trees and aggregating their results. This is done through creating a large number of trees, each of which is constructed using a bootstrap of the sample dataset. Each node in these trees is split using the best among a subset of predictors randomly chosen at that node. An estimate of the error rate for Random Forests is obtained by predicting the data not in the bootstrap sample at each bootstrap iteration [referred to as ‘out of the bag’ (OOB) data]. The OOB data is beneficial in determining variable importance. The value of variable importance is measured through the program examining how much the prediction error (OOB) increases when data for that variable is permuted, with all other variables left unchanged (Breiman, 2001; Liaw & Wiener, 2002). Random Forests were run using the randomForest package in R version 3.0.1 (R Core Team, 2013) to obtain the OOB and variable importance for the HAMD and PHQ-9 prediction trees.
Results
Participants
Baseline participant demographic and clinical characteristics are displayed in Table 1. Among the 325 participants entered into the trial, there were no significant differences in demographics across treatment groups.
Table 1.
Participants’ baseline demographics and psychiatric characteristics
| Variable | FtF-CBT (n = 162) | T-CBT (n = 163) | p value |
|---|---|---|---|
| Age, mean (S.D.) | 47.5 (13.5) | 47.8 (12.6) | 0.87 |
| Female, n (%) | 127 (78.4) | 125 (76.7) | 0.71 |
| Ethnicity, n (%) | |||
| Hispanic or Latino | 21 (13.0) | 23 (14.2) | 0.76 |
| Race, n (%) | |||
| African American | 36 (24.0) | 36 (24.3) | |
| Caucasian | 98 (65.3) | 89 (60.1) | 0.63 |
| More than one race | 12 (8.0) | 18 (12.2) | |
| Other | 4 (2.7) | 5 (3.4) | |
| Married/cohabitating, n (%) | 51 (31.7) | 56 (34.4) | 0.61 |
| Education, n (%) | |||
| <9th grade | 0 (0.0) | 2 (1.2) | |
| Some high school | 2 (1.2) | 7 (4.3) | |
| General Education Diploma | 12 (7.4) | 13 (8.0) | |
| Some college | 31 (19.1) | 26 (16.0) | |
| Associate’s degree | 10 (6.2) | 14 (8.6) | 0.77 |
| Bachelor’s degree | 64 (39.5) | 55 (33.7) | |
| Master’s degree | 30 (18.5) | 33 (20.2) | |
| Doctoral degree | 4 (2.5) | 5 (3.1) | |
| Professional degree | 9 (5.6) | 10 (6.1) | |
| Employment, n (%) | |||
| Employed | 90 (55.6) | 95 (58.3) | |
| Unemployed | 33 (20.4) | 32 (19.6) | |
| Disability | 10 (6.2) | 16 (9.8) | 0.30 |
| Retired | 18 (11.1) | 16 (9.8) | |
| Other | 11 (6.8) | 4 (2.5) | |
| Household income, US$, mean (S.D.) | 73 480 (64 057) | 75 637 (75 989) | 0.79 |
| On active dose of antidepressant medication, n (%) | 56 (34.6) | 54 (33.1) | 0.78 |
| Total number of co-morbid diagnoses, mean (S.D.) | 1.34 (1.06) | 1.3 (1.11) | 0.67 |
| Co-morbid anxiety, n (%) | |||
| Agoraphobia, panic | 11 (8.7) | 12 (10.2) | 0.70 |
| GAD | 114 (90.5) | 106 (89.8) | 0.87 |
| OCD | 13 (10.3) | 9 (7.6) | 0.46 |
| PTSD | 15 (11.9) | 8 (6.8) | 0.17 |
| Social phobia | 25 (19.8) | 33 (28.0) | 0.14 |
| HAMD, mean (S.D.) | 22.8 (4.6) | 22.9 (4.6) | 0.77 |
| PHQ-9, mean (S.D.) | 16.4 (4.8) | 17.2 (4.7) | 0.12 |
| GAD-7, mean (S.D.) | 12.3 (5.0) | 11.8 (4.7) | 0.33 |
| PANAS, mean (S.D.) | 19.8 (5.9) | 19.9 (6.0) | 0.89 |
| LES, mean (S.D.) | −12.0 (10.6) | −11.4 (11.5) | 0.65 |
| NML, mean (S.D.) | 148.2 (13.1) | 148.2 (13.3) | 0.98 |
| SPS, mean (S.D.) | 70.2 (11.9) | 70.6 (10.6) | 0.79 |
| CSE, mean (S.D.) | 91.0 (42.9) | 98.2 (43.1) | 0.14 |
| AUDIT, mean (S.D.) | 3.7 (5.0) | 3.6 (4.5) | 0.94 |
| PBP, mean (S.D.) | 40.0 (11.3) | 39.5 (10.7) | 0.85 |
| SIBS, mean (S.D.) | 11.0 (5.8) | 10.4 (5.5) | 0.34 |
| PSS, mean (S.D.) | 27.1 (5.2) | 26.8 (5.4) | 0.50 |
| AES, mean (S.D.) | 48.4 (9.7) | 49.8 (8.6) | 0.14 |
| SF-36, mean (S.D.) | |||
| Bodily pain | 57.9 (26.6) | 51.2 (26.1) | 0.03 |
| General health perception | 50.1 (22.2) | 47.2 (24.4) | 0.24 |
| Mental health | 33.6 (13.6) | 34.0 (12.4) | 0.45 |
| Physical functioning | 74.1 (27.4) | 66.3 (30.7) | 0.02 |
| Emotional role functioning | 37.1 (22.8) | 38.7 (24.3) | 0.47 |
| Physical role functioning | 62.1 (31.6) | 57.7 (33.8) | 0.25 |
| Social role functioning | 37.7 (23.3) | 34.2 (20.4) | 0.26 |
| Vitality | 22.4 (14.5) | 21.0 (14.4) | 0.34 |
| Physical components summary | 51.7 (11.8) | 48.3 (12.6) | 0.02 |
| Mental components summary | 24.5 (9.4) | 25.4 (8.2) | 0.17 |
| Trauma/abuse history, n (%) | 92 (57.5) | 99 (59.9) | 0.67 |
FtF-CBT, Face-to-Face cognitive behavioral therapy; T-CBT, telephone cognitive behavioral therapy; HAMD, Hamilton Depression Rating Scale; PHQ-9, Patient Health Questionnaire-9; GAD-7, Generalized Anxiety Disorder Questionnaire-7; PANAS, Positive and Negative Affect Schedule; LES, Life Experiences Survey; NML, Nijmegen Motivation; SPS, Social Provisions Scale; CSE, Coping Self-Efficacy Scale; AUDIT, Alcohol Use Disorders Identification Test; PBP, Perceived Barriers to Psychotherapy; SIBS, Scale for Interpersonal Behavior; PSS, Perceived Stress Scale; AES, Apathy Evaluation Scale; SF-36, Medical Outcomes Study 36.
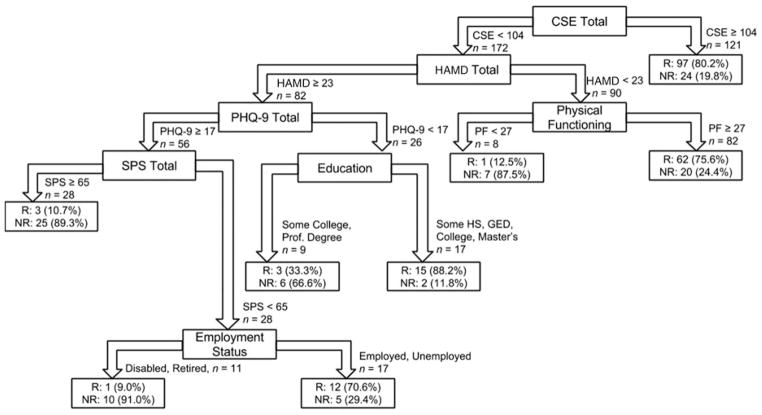
Predictors of treatment response and non-response based on the HAMD
The treatment response rate based on HAMD < 16 was 66.2% (49.5% for T-CBT and 50.5% for FtF-CBT). The CART model, pruned using the prune command, generated a tree based on the outcome of dichotomized HAMD scores at end of treatment. Fig. 1 displays the pruned tree. The model predicted that 231 participants would be treatment responders; 197 (85.3%) of these were accurately predicted. Of the 56 participants who were predicted to be treatment non-responders 48 (85.7%) were accurately predicted.
Fig. 1.
Classification and regression tree model developed for predicting outcomes on the Hamilton Depression Rating Scale (HAMD). CSE, Coping Self-Efficacy Scale; PHQ-9, Patient Health Questionnaire-9; PF, physical functioning (as measured by SF-36); SPS, Social Provisions Scale.
Variables (and scores) that predicted response included CSE (≥104), baseline depression severity (HAMD < 23, PHQ-9 < 17), physical functioning (PF ≥27), social support (SPS < 65), education level [some high school, general education diploma (GED), or bachelor’s/master’s degree], and employment status (employed or unemployed). Variables (and scores) that predicted non-response included CSE (< 104), baseline depression severity (HAMD ≥23, PHQ-9 ≥17), PF (< 27), social support (SPS ≥65), education level (some college or professional degree), and employment status (disability or retired). No other variables, including treatment assignment to FtF-CBT or T-CBT were related to response.
Predictors of treatment response and non-response based on the PHQ-9
The treatment response rate based on PHQ-9 < 10 was 73.8% (50.2% for T-CBT and 49.8% for FtF-CBT). The CART model, pruned using the prune command, generated a tree based on the outcome of dichotomized PHQ-9 scores at end of treatment. Fig. 2 displays the pruned tree. The model predicted 240 participants would be treatment responders; 204 (85.0%) of these were accurately predicted. Of the 46 participants predicted to be treatment non-responders, 39 (85.0%) were accurately predicted. Variables (and scores) that predicted response included CSE (≥104), baseline depression severity (PHQ-9 < 17, HAMD < 26), education level (some college, bachelor’s degree, or professional degree), and being male. Variables (and scores) that predicted non-response included CSE (< 104), baseline depression severity (PHQ-9 ≥17, HAMD ≥26), education level (some high school, GED or master’s degree/PhD), and being female. No other variables, including treatment assignment to FtF-CBT or T-CBT were related to response.
Fig. 2.
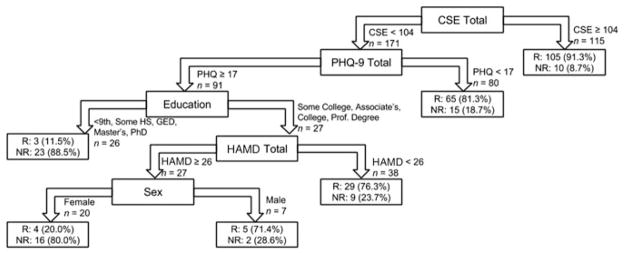
Classification and regression tree model developed for predicting outcomes on the Patient Health Questionnaire-9 (PHQ-9). CSE, Coping Self-Efficacy Scale; HAMD, Hamilton Depression Rating Scale.
Variables of importance
The Random Forest analyses yielded an OOB error rate of 30.8% for both the HAMD and PHQ-9 models. The top values of variable importance for both the HAMD and PHQ-9 are presented in Table 2. The top variables of importance for the HAMD Random Forests were education, CSE, interviewer-based assessment of depression through the HAMD, age, and self-reported anxiety through the GAD-7. The top variables of importance for the PHQ-9 Random Forests were CSE, self-report depression through the PHQ-9, interviewer-based assessment of depression through the HAMD, education, and self-reported anxiety through the GAD-7.
Table 2.
Top variables of importance as determined through Random Forest analyses
| HAMD
|
PHQ-9
|
||
|---|---|---|---|
| Variable | Importance value | Variable | Importance value |
| Education | 10 | CSE | 14 |
| CSE | 9 | PHQ-9 | 11 |
| HAMD | 7 | HAMD | 10 |
| Age | 7 | Education | 8 |
| GAD-7 | 7 | GAD-7 | 6 |
HAMD, Hamilton Depression Rating Scale; PHQ-9, Patient Health Questionnaire-9; CSE, Coping Self-Efficacy Scale; GAD-7, Generalized Anxiety Disorder Questionnaire-7.
Discussion
Demographic and psychological characteristics at baseline of participants receiving outpatient T-CBT and FtF-CBT for depression accurately identified 85.3% and 85.0% of treatment responders and 85.7% and 85.0% of treatment non-responders with response defined by the HAMD and PHQ-9, respectively. CSE, baseline depression severity, and education consistently predicted outcome using both the HAMD and PHQ-9. Social support, PF, and employment emerged as predictors only for the HAMD, and sex predicted response on the PHQ-9. Treatment delivery method (i.e. telephone or face-to-face) and presence of co-morbid anxiety did not impact the prediction of outcome. These findings were supported through the Random Forests top variables of importance, including CSE, baseline depression, and education.
Participant baseline scores on CSE, which measures a person’s confidence in his or her ability to cope effectively with situations that are appraised to be stressful (Chesney et al. 2006), was the primary predictive branch of the CART trees for response to treatment, regardless of how depression was measured. This measure alone predicted positive response outcomes for 41.3% and 40.2% of the total sample for the HAMD and PHQ-9, respectively. The value identified, surprisingly equivalent for both the HAMD and PHQ-9 (CSE = 104), is indicative of a moderate level of CSE according to previously established norms (Chesney et al. 2006), meaning that those with moderate levels of CSE or higher are more likely to respond relative to those with lower levels. To our knowledge, CSE has not been directly investigated or reported as a predictor of outcome in CBT for depression. However, studies investigating related concepts have shown findings consistent with these. For example, resourcefulness (Simons et al. 1985) as well as increased stressful life events (Fournier et al. 2009) have both been found to be prescriptive predictors of which patients benefit more from CBT compared to anti-depressant medication.
The CSE taps a person’s confidence in his or her ability to cope effectively with situations that are appraised to be stressful (Chesney et al. 2006). CBT often requires patients to confront difficult or stressful thoughts or situations through cognitive restructuring, exposure, behavioral experiments, and other strategies (Beck, 1995; Simos & Hofmann, 2013). Patients who come into therapy with high levels of CSE may be more willing and capable of tolerating the distress created by these strategies and more likely in general to persevere and succeed. This suggests that patients with low CSE may achieve better results if greater focus on enhancing CSE is provided earlier in treatment, which may provide patients more confidence in discussing and facing difficult life situations. Further research is needed to cross-validate these findings and explore their treatment implications.
It was interesting that the CART analyses found for both the PHQ-9 and HAMD outcomes, moderate to high CSE was the optimal split predicting response, with no additional covariates necessary. For those with low CSE, two constructs provided additional predictive value consistently across both models: depression and education. The finding that education consistently predicts response is not consistent with the available evidence indicating that education is not predictive of outcome in CBT (Jarrett et al. 1991; Hamilton & Dobson, 2002). Indeed, no gradient was identified in the current analyses; having attained a master’s degree was grouped with some high school, GED, and college; while some college education and professional degrees are grouped in another. Furthermore, some of the educational categories (e.g. some college, professional degree) predict response for one depression outcome, and non-response in the other.
By contrast, the finding that baseline depressive symptom severity contributes to the prediction of treatment response is consistent with and extends previous findings (Jarrett et al. 1991; Sotsky et al. 1991; Shapiro et al. 1994; Thase et al. 1994; Agosti & Ocepek-Welikson, 1997; Persons et al. 1999; Hamilton & Dobson, 2002; Coffman et al. 2007). However, severity of depressive symptoms was only valuable as a predictor of treatment response among those with CSE, suggesting that greater severity of symptoms only exerts its negative influence among those who do not have the confidence in the coping skills to manage stress and distress. This finding points to the utility of CART analyses in uncovering potentially complex relationships among predictor variables.
Other variables provided predictive value, however not consistently across the models. In the HAMD model, among those with lower CSE, more depressed individuals and those with higher perceived social support were at most risk for non-response. This finding is inconsistent with the literature on the influence of social support on outcomes for treatment of depression (George et al. 1989); however, given that social support was not a top variable of importance in the Random Forests, we are hesitant to over-interpret these findings.
Among individuals with low CSE and depressive severity, poorer PF predicted non-response in the HAMD model. Among those with both low CSE and higher depressive severity, individuals with good social support and employment further differentiated responders from non-responders. However, the grouping of employment (disabled and retired v. employed and unemployed) suggested that the variable might be acting as a surrogate for PF. Sex entered only the PHQ-9 model, with women with low CSE and higher depressive severity at greater risk of non-response than their male counterparts. However, the inconsistency of these variables across the models suggests that the findings may not be reliable.
Randomization to T-CBT or FtF-CBT did not appear in the CART analyses as a predictor variable. This is consistent with the findings of the parent trial, finding no difference in depression severity at post-treatment across the two treatment arms (Mohr et al. 2012). Thus, this investigator found no support for any prescriptive variables, it appears as though characteristics that predict response held regardless of the modality used. This might be due to the fact that the treatments were quite similar and the only difference in modality was whether the patient was in the room with the therapist or over the phone. Prescriptive variables might be more important for treatments that differ more markedly in mechanism of action such as psychotherapy v. medication. However, for a given type of treatment (e.g. CBT), prescriptive variables might be more valuable for media that differ more markedly, such as face-to-face v. internet CBT.
A number of other predictor variables included in the CART analyses that the literature has identified as predictors of CBT outcome, such as stress, motivation for treatment, and co-morbid anxiety, were included in the analyses, yet they were not significant predictors for this sample. It may be that CSE and depressive symptom severity account for most of the variance, leaving little room for other variables, which might, on their own, have some predictive power. Specifically, CSE may be associated with traits such as anxiety, and studies examining anxiety may not have accounted for coping, as it has not previously been identified as a potential confounder. This demonstrates the potential strength of CART analyses to identify new relationships one might not have predicted that could be more important than previously established relationships. It also demonstrates the clinical utility of CART analyses, as the interaction options provided by trees maps more closely to intuitive clinical decision making and is a further step towards personalized medicine.
There are several limitations and caveats that should be considered in interpreting these results. First, as a secondary, exploratory analysis, these findings should be viewed with caution until they are replicated or refuted. Second, this trial examined CBT for depression; it is unclear how these results generalize to other forms of psychotherapy, other mental health conditions, and other treatment delivery media. Third, while the sample was ethnically diverse, participants were fairly well educated. The small number of participants with lower levels of education may be partly responsible for the inconsistent findings with respect to education and certainly limit generalizability to less-educated populations. Fourth, we used response criteria based on level of symptoms used for referral or initiation of treatment. For the HAMD, this was identical to entry criteria. While patients overall showed a strong response to treatment, it is possible that a few patients may only have moved 1 or 2 points on the HAMD to reach response criteria. Furthermore, these decision trees may not generalize to other criteria, such as full remission of symptoms. Finally, although CART analysis is an effective data-mining tool, there are some disadvantages to these models. Trees minimize total variability in the data, both from the population as well as sample variability. Without adequate pruning, trees are often overfit, in that they minimize sample variability. Additionally, misclassification errors may build. Since each branch depends on a previous one, misclassification errors in early branches will continue down the tree. CART is a form of data mining, thus, these findings should be validated in another dataset before generalizing these findings more broadly. Nevertheless, a strength of CART analyses is that they can identify new relationships one might not have predicted that could be more important than previously established relationships. Additionally, a sensitivity analysis using Random Forests supported the findings of the CART analyses. Thus, although CART is an exploratory method, it has the potential to identify relationships that can be investigated in subsequent studies.
To the best of our knowledge, this is the first study to use exploratory CART analyses to evaluate patient characteristics that predict depression outcomes among patients receiving T-CBT or FtF-CBT for the treatment of major depressive disorder. The findings of the present study indicate that depressed patients with moderate to high CSE are likely to do well with CBT, regardless of other baseline characteristics. Among those with poor CSE, lower levels of depressive symptom severity also indicate a likely positive response. Those with low CSE and high depressive symptom severity were consistently found to be the most at risk of non-response. There was also a suggestion that in this group of low CSE, depressed individuals with low social support may be at risk for non-response. While these findings should be confirmed in future research, they point to the possibility of improving outcomes by enhancing CSE early in treatment as a strategy of mitigating potential treatment non-response to improve the overall impact of CBT.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health R01 MH059708 and R01 MH095753 (PI: Mohr); K08 MH102336 (PI: Schueller); and F31 MH106321 (PI: Stiles-Shields).
Footnotes
Declaration of Interest
None.
References
- Agosti V, Ocepek-Welikson K. The efficacy of imipramine and psychotherapy in early-onset chronic depression: a reanalysis of the National Institute of Mental health Treatment of Depression Collaborative Research Program. Journal of Affective Disorders. 1997;43:181–186. doi: 10.1016/s0165-0327(97)01428-6. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association; Washington, DC: 2000. Text Revision. [Google Scholar]
- Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cognitive Behavior Therapy. 2009;38:196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Arrindell W, Van Der Ende J. Cross-sample invariance of the structure of self-reported distress and difficulty in assertiveness. Advances in Behaviour Research and Therapy. 1985;7:205–243. [Google Scholar]
- Babor TF, De La Fuente JR, Saunders J, Grant M. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. World Health Organization; Geneva: 1992. (WHO Publication No. 92.4) [Google Scholar]
- Beck JS. Cognitive Therapy. Guilford Press; New York: 1995. [Google Scholar]
- Bedi N, Chilvers C, Churchill R, Dewey M, Duggan C, Fielding K, Gretton V, Miller P, Harrison G, Lee A, Williams I. Assessing effectiveness of treatment of depression in primary care. Partially randomised preference trial. British Journal of Psychiatry. 2000;177:312–318. doi: 10.1192/bjp.177.4.312. [DOI] [PubMed] [Google Scholar]
- Beutler LE, Engle D, Mohr D, Daldrup RJ, Bergan J, Meredith K, Merry W. Predictors of differential response to cognitive, experiential, and self-directed psychotherapeutic procedures. Journal of Consulting and Clinical Psychology. 1991;59:333–340. doi: 10.1037//0022-006x.59.2.333. [DOI] [PubMed] [Google Scholar]
- Bockting CL, Spinhoven P, Koeter MW, Wouters LF, Visser I, Schene AH, Group DS. Differential predictors of response to preventive cognitive therapy in recurrent depression: a 2-year prospective study. Psychotherapy and Psychosomatics. 2006;75:229–236. doi: 10.1159/000092893. [DOI] [PubMed] [Google Scholar]
- Brazier JE, Harper R, Jones NM, O’cathain A, Thomas KJ, Usherwood T, Westlake L. Validating the SF-36 health survey questionnaire: new outcome measure for primary care. British Medical Journal. 1992;305:160–164. doi: 10.1136/bmj.305.6846.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breiman L. Random forests. Machine Learning. 2001;45:5–32. [Google Scholar]
- Breiman L, Friedman J, Olshen RA, Stone CJ. Classification and Regression Trees. CRC Press; New York: 1984. [Google Scholar]
- Brody DS, Khaliq AA, Thompson TL., II Patients’ perspectives on the management of emotional distress in primary care settings. Journal of General Internal Medicine. 1997;12:403–406. doi: 10.1046/j.1525-1497.1997.00070.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CH, Sloboda Z, Faggiano F, Teasdale B, Keller F, Burkhart G, Vigna-Taglianti F, Howe G, Masyn K, Wang W. Methods for synthesizing findings on moderation effects across multiple randomized trials. Prevention Science. 2013;14:144–156. doi: 10.1007/s11121-011-0207-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clinical Psychology Review. 2006;26:17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Chesney MA, Neilands TB, Chambers DB, Taylor JM, Folkman S. A validity and reliability study of the coping self-efficacy scale. British Journal of Health Psychology. 2006;11:421–437. doi: 10.1348/135910705X53155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Churchill R, Khaira M, Gretton V, Chilvers C, Dewey M, Duggan C, Lee A. Treating depression in general practice: factors affecting patients’ treatment preferences. British Journal of General Practice. 2000;50:905–906. [PMC free article] [PubMed] [Google Scholar]
- Coffman SJ, Martell CR, Dimidjian S, Gallop R, Hollon SD. Extreme nonresponse in cognitive therapy: can behavioral activation succeed where cognitive therapy fails? Journal of Consulting and Clinical Psychology. 2007;75:531–541. doi: 10.1037/0022-006X.75.4.531. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Corson K, Gerrity MS, Dobscha SK. Screening for depression and suicidality in a VA primary care setting: 2 items are better than 1 item. American Journal of Managed Care. 2004;10:839–845. [PubMed] [Google Scholar]
- Cuijpers P. Bibliotherapy in unipolar depression: a meta-analysis. Journal of Behavior Therapy and Experimental Psychiatry. 1997;28:139–147. doi: 10.1016/s0005-7916(97)00005-0. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Berking M, Andersson G, Quigley L, Kleiboer A, Dobson KS. A meta-analysis of cognitive-behavioural therapy for adult depression, alone and in comparison with other treatments. Canadian Journal of Psychiatry. 2013;58:376–385. doi: 10.1177/070674371305800702. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Van Straten A, Andersson G, Van Oppen P. Psychotherapy for depression in adults: a meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology. 2008;76:909–922. doi: 10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, Gallop R, Mcglinchey JB, Markley DK, Gollan JK, Atkins DC, Dunner DL, Jacobson NS. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74:658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Dobson KS. A meta-analysis of the efficacy of cognitive therapy for depression. Journal of Consulting and Clinical Psychology. 1989;57:414–419. doi: 10.1037//0022-006x.57.3.414. [DOI] [PubMed] [Google Scholar]
- Doghramji K. The epidemiology and diagnosis of insomnia. American Journal of Managed Care. 2006;12:S214–S220. [PubMed] [Google Scholar]
- Driessen E, Hollon SD. Cognitive behavioral therapy for mood disorders: efficacy, moderators and mediators. Psychiatric Clinics of North America. 2010;33:537–555. doi: 10.1016/j.psc.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwight-Johnson M, Sherbourne CD, Liao D, Wells KB. Treatment preferences among depressed primary care patients. Journal of General Internal Medicine. 2000;15:527–534. doi: 10.1046/j.1525-1497.2000.08035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier JC, Derubeis RJ, Shelton RC, Gallop R, Amsterdam JD, Hollon SD. Antidepressant medications v. cognitive therapy in people with depression with or without personality disorder. British Journal of Psychiatry. 2008;192:124–129. doi: 10.1192/bjp.bp.107.037234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fournier JC, Derubeis RJ, Shelton RC, Hollon SD, Amsterdam JD, Gallop R. Prediction of response to medication and cognitive therapy in the treatment of moderate to severe depression. Journal of Consulting and Clinical Psychology. 2009;77:775–787. doi: 10.1037/a0015401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelhart RP, King HL. The influence of comorbid risk factors on the effectiveness of cognitive-behavioral treatment of depression. Cognitive and Behavioral Practice. 2001;8:18–28. [Google Scholar]
- George LK, Blazer DG, Hughes DC, Fowler N. Social support and the outcome of major depression. British Journal of Psychiatry. 1989;154:478–485. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- Hamilton KE, Dobson KS. Cognitive therapy of depression: pretreatment patient predictors of outcome. Clinical Psychology Review. 2002;22:875–893. doi: 10.1016/s0272-7358(02)00106-x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarrett RB, Eaves GG, Grannemann BD, Rush AJ. Clinical, cognitive, and demographic predictors of response to cognitive therapy for depression: a preliminary report. Psychiatry Research. 1991;37:245–260. doi: 10.1016/0165-1781(91)90061-s. [DOI] [PubMed] [Google Scholar]
- Keijsers PJ, Schaap PDR, Hoogduin C, Hoogsteyns B, De Kemp ECM. Preliminary results of a new instrument to assess patient motivation for the treatment of cognitive-behavioural therapy. Behavioural and Cognitive Psychotherapy. 1999;27:165–179. [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) Journal of the American Medical Association. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012;21:169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King MW, Resick PA. Data mining in psychological treatment research: a primer on classification and regression trees. Journal of Consulting and Clinical Psychology. 2014;82:895–905. doi: 10.1037/a0035886. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:1–7. [Google Scholar]
- Lehman KA, Burns MN, Gagen EC, Mohr DC. Development of the brief inventory of perceived stress. Journal of Clinical Psychology. 2012;68:631–644. doi: 10.1002/jclp.21843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liaw A, Wiener M. Classification and regression by randomForest. R News. 2002;2:18–22. [Google Scholar]
- Marin RS, Biedrzycki RC, Firinciogullari S. Reliability and validity of the Apathy Evaluation Scale. Psychiatry Research. 1991;38:143–162. doi: 10.1016/0165-1781(91)90040-v. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Hart SL, Howard I, Julian L, Vella L, Catledge C, Feldman MD. Barriers to psychotherapy among depressed and nondepressed primary care patients. Annals of Behavioral Medicine. 2006;32:254–258. doi: 10.1207/s15324796abm3203_12. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Hart SL, Julian L, Catledge C, Honos-Webb L, Vella L, Tasch ET. Telephone-administered psychotherapy for depression. Archives of General Psychiatry. 2005;62:1007–1014. doi: 10.1001/archpsyc.62.9.1007. [DOI] [PubMed] [Google Scholar]
- Mohr DC, Ho J, Duffecy J, Reifler D, Sokol L, Burns MN, Jin L, Siddique J. Effect of telephone-administered vs. face-to-face Cognitive Behavioral Therapy on Adherence to therapy and depression outcomes among primary care patients: a randomized trial. Journal of the American Medical Association. 2012;307:2278–2285. doi: 10.1001/jama.2012.5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Fenn CB, Billings AG. Life stressors and social resources: an integrated assessment approach. Social Science and Medicine. 1988;27:999–1002. doi: 10.1016/0277-9536(88)90291-2. [DOI] [PubMed] [Google Scholar]
- Novotney A. A new emphasis on telehealth: how can psychologists stay ahead of the curve – and keep patients safe? Monitor on Psychology. 2011;42:40. [Google Scholar]
- Persons JB, Bostrom A, Bertagnolli A. Results of randomized controlled trials of cognitive therapy for depression generalize to private practice. Cognitive Therapy and Research. 1999;23:535–548. [Google Scholar]
- Priest RG, Vize C, Roberts A, Roberts M, Tylee A. Lay people’s attitudes to treatment of depression: results of opinion poll for Defeat Depression Campaign just before its launch. British Medical Journal. 1996;313:858–859. doi: 10.1136/bmj.313.7061.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. [Google Scholar]
- Reeves WC, Strine TW, Pratt LA, Thompson W, Ahluwalia I, Dhingra SS, McKnight-Eily LR, Harrison L, D’angelo DV, Williams L, Morrow B, Gould D, Safran MA Centers for Disease Control and Prevention (CDC) Mental illness surveillance among adults in the United States. Morbidity and Mortality Weekly Report. Surveillance Summaries. 2011;60 (Suppl 3):1–29. [PubMed] [Google Scholar]
- Reich J, Warshaw M, Peterson LG, White K. Comorbidity of panic and major depressive disorder. Journal of Psychiatric Research. 1995;20:23–33. doi: 10.1016/0022-3956(93)90015-t. [DOI] [PubMed] [Google Scholar]
- Rush AJ, Beck AT, Kovacs M, Hollon SD. Comparative efficacy of cognitive therapy and pharmacotherapy in the treatment of depressed outpatients. Cognitive Therapy and Research. 1977;1:17–37. [Google Scholar]
- Russell DW, Cutrona CE. Social Provisions Scale. Paper presented at the American Psychological Association Meeting; August, 1984; Toronto, ON, Canada. Iowa State University; 1984. [Google Scholar]
- Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the Life Experiences Survey. Journal of Consulting and Clinical Psychology. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- Shapiro DA, Barkham M, Rees A, Hardy GE, Reynolds S, Startup M. Effects of treatment duration and severity of depression on the effectiveness of cognitive-behavioral and psychodynamic-interpersonal psychotherapy. Journal of Consulting and Clinical Psychology. 1994;62:522–534. doi: 10.1037/0022-006x.62.3.522. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Janavs J, Weiller E, Keskiner A, Schinka E, Knapp E, Sheehan MF, Dunbar GC. The validity of the Mini International Neuropsychiatric Interview (MINI) according to the SCID-P and its reliability. European Psychiatry. 1997;12:232–241. [Google Scholar]
- Simons AD, Lustman PJ, Wetzel RD, Murphy GE. Predicting response to cognitive therapy of depression: the role of learned resourcefulness. Cognitive Therapy and Research. 1985;9:79–89. [Google Scholar]
- Simos G, Hofmann SG. CBT for Anxiety Disorders: A Practitioner Book. John Wiley & Sons; Oxford: 2013. [Google Scholar]
- Sotsky SM, Glass DR, Shea MT, Pilkonis PA, Collins JF, Elkin I, Watkins JT, Imber SD, Leber WR, Moyer J, Oliveri ME. Patient predictors of response to psychotherapy and pharmacotherapy: findings in the NIMH Treatment of Depression Collaborative Research Program. American Journal of Psychiatry. 1991;148:997–1008. doi: 10.1176/ajp.148.8.997. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives of Internal Medicine. 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Stiles-Shields C, Kwasny M, Cai X, Mohr DC. Comorbid anxiety as a differential treatement predictor for telephone vs. face-to-face administered cognitive behavioral therapy for depression. Depression and Anxiety. 2014a;31:934–940. doi: 10.1002/da.22323. [DOI] [PubMed] [Google Scholar]
- Stiles-Shields C, Kwasny MJ, Cai X, Mohr DC. Therapeutic alliance in face-to-face and telephone-adminstered cognitive behavioral therapy. Journal of Consulting and Clinical Psychology. 2014b;82:349–354. doi: 10.1037/a0035554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thase ME, Reynolds CF, Frank E, Simons AD, Garamoni GD, McGeary J, Harden T, Fasiczka AL, Cahalane JF. Response to cognitive-behavioral therapy in chronic depression. Journal of Psychotherapy Practice and Research. 1994;3:204–214. [Google Scholar]
- The Macarthur Foundation’s Initiative on Depression and Primary Care. The Macarthur Initiative on Depression and Primary Care at Darmouth and Duke: Depression Management Toolkit. Dartmouth; Hanover, NH: 2004. [Google Scholar]
- Vallis TM, Shaw BF, Dobson KS. The cognitive therapy scale: psychometric properties. Journal of Consulting and Clinical Psychology. 1986;54:381–385. doi: 10.1037//0022-006x.54.3.381. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wolfe J, Kimberling R. Gender issues in the assessment of posttraumatic stress disorder. In: Wilson J, Keane TM, editors. Assessing Psychological Trauma and PTSD. Guilford; New York: 1997. pp. 192–238. [Google Scholar]