Abstract
Background
Adults with congenital heart defects (ACHD) face long-term complications related to prior surgery, abnormal anatomy, and acquired cardiovascular conditions. Although self-care is an important part of chronic illness management, few studies have explored self-care in the ACHD population. The purpose of this study is to describe self-care and its antecedents in the ACHD population.
Methods
Persons with moderate or severe ACHD (N=132) were recruited from a single ACHD center. Self-care (health maintenance behaviors, monitoring and management of symptoms), and potential antecedents including sociodemographic and clinical characteristics, ACHD knowledge, behavioral characteristics (depressive symptoms and self-efficacy), and family-related factors (parental overprotection and perceived family support) were collected via self-report and chart review. Multiple regression was used to identify antecedents of self-care maintenance, monitoring, and management.
Results
Only 44.7%, 27.3%, and 23.3% of participants performed adequate levels of self-care maintenance, monitoring and management, respectively. In multiple regression analysis, self-efficacy, education, gender, perceived family support, and comorbidities explained 25% of the variance in self-care maintenance (R2=.248, F(5, 123)=9.44, p<.001). Age, depressive symptoms, self-efficacy, and NYHA Class explained 23% of the variance in self-care monitoring (R2=.232, F(2, 124)=10.66, p<.001). Self-efficacy and NYHA Class explained 9% of the variance in self-care management (R2=.094, F(2, 80)=5.27, p=.007).
Conclusions
Low levels of self-care are common among persons with ACHD. Multiple factors, including modifiable factors of self-efficacy, depressive symptoms, and perceived family support, are associated with self-care and should be considered in designing future interventions to improve outcomes in the ACHD population.
Keywords: self-care, self-management, adult congenital heart disease
Introduction
Fifty years ago only one third of children born with congenital heart disease survived to 10 years of age, but today 90% of children survive to adulthood and over one million adults are living with congenital heart disease (ACHD).1,2 Although the majority of adults had surgical repair in childhood, they are not cured. Surgical sequelae and residual defects cause late complications such as arrhythmia, heart failure, and the development of renal, pulmonary, and hepatic comorbidities.3 With the exception of those with mild heart defects, complications are universal and require lifelong surveillance and illness management. Although self-care is a vital component of chronic illness management, little is understood about the practice of self-care in ACHD. A small number of studies have provided beginning evidence indicating that low levels of self-care may be a significant problem for persons with ACHD. Between 40-60% of adults, for instance, are not engaged in routine care,4,5 and up to 85% do not meet physical activity recommendations.6 Further, at least 20% of women do not attend pre-pregnancy counseling despite high rates of maternal and fetal complications.4,7
Lower levels of self-care have been associated with poor health outcomes. In ACHD, those with a three-year lapse in care are over three times more likely to require emergent interventions, receive additional diagnoses, and experience more symptoms,5 and those who are less physically active have greater reductions in functional capacity.8 Thus, improving self-care may be an effective means of reducing ACHD morbidity, but the development of interventions to promote self-care is limited by the lack of evidence regarding antecedents of self-care in this population. Few have studied ACHD self-care behaviors and there is no consensus on the individual and clinical factors that may explain self-care. Furthermore, no studies of self-care in an adult cohort of patients with congenital heart disease have examined typical antecedents important in other chronically ill populations such as knowledge, behavioral characteristics of self-efficacy or depressive symptoms, and social support. The purpose of this study is thus to describe the practice of self-care and identify possible antecedents of self-care, so that meaningful interventions to improve self-care behaviors can be designed for the ACHD population.
Methods
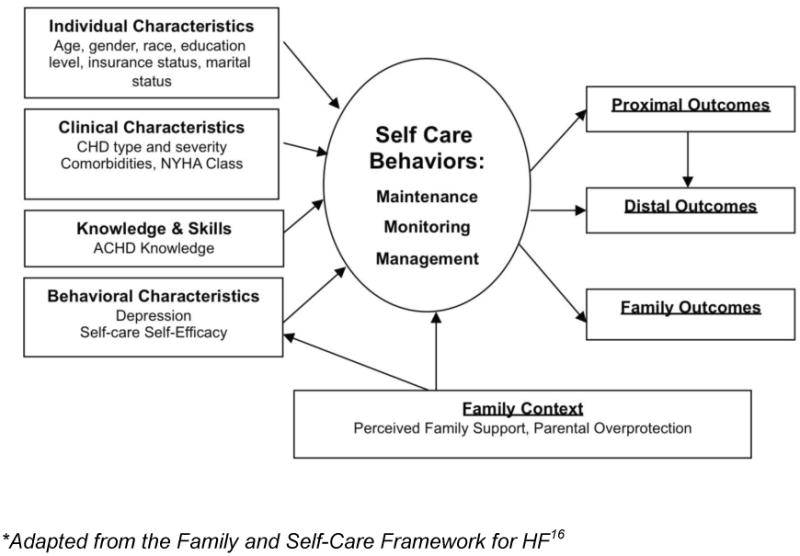
Given its holistic perspective and utility in the similar acquired heart failure (HF) population, antecedent factors were chosen based on the Family and Self-Care Framework (Figure 1), including individual, clinical, behavioral, and family-related factors.9 A cross-sectional, descriptive study design was used to describe self-care and to determine the relationship antecedent factors and self-care.
Figure 1. Family and Self-Care Framework for ACHD*.
Sample and Setting
After receiving IRB approval, all eligible adults were recruited from a large ACHD clinic located in the southeastern US. Eligible adults were identified through medical chart review and recruited directly from clinic appointments. Inclusion criteria included 1) aged 18 years and older, 2) having moderate or severe CHD per American Heart Association/American College of Cardiology guidelines18, and 3) English-speaking. Exclusion criteria were 1) developmental delay impairing ability to independently complete surveys, 2) adult diagnosis of ACHD, and potential confounders of a walking test including 3) current pregnancy, 4) disability preventing ability to walk, and 5) less than one month post-op from cardiac surgery. A total of 341 persons were screened for eligibility; 168 (49%) did not meet inclusion criteria and 23 (12%) declined participation. Of the 150 patients consented, 132 (88%) completed baseline data collection.
Procedures
Once informed consent was obtained, participants completed a six-minute walk test (6MWT) and received study surveys. Participants completed surveys at the clinic appointment or at home either electronically via a secure, electronic database survey system or via paper surveys. Clinical information was collected via medical chart review. Participants were compensated with a parking voucher and $10 gift card.
Measurement
Self-Care
Self-care was operationalized as three separate constructs: maintenance (behaviors that maintain physiologic stability), monitoring (attention to changes in symptoms), and management (response to symptoms when they occur). Self-care was measured using the 32-item Self-care Index for ACHD (SCI-ACHD), a modified version of the Self-Care in HF Index.11 Subscales of self-care maintenance, monitoring, management (completed only by persons experiencing heart-related symptoms in past month), and self-care confidence were scored independently. Scores were standardized on a 100-point scale with higher scores reflecting higher levels of self-care.
Individual and Clinical Characteristics
Sociodemographic variables (age, gender, race, educational level, marital status, employment status, and insurance status) were collected by self-report. Clinical variables (type and severity of heart defect, NYHA Class, comorbidities) were collected via medical chart review. Severity of heart defect was classified as moderate or severe based on AHA guidelines.38 The Charlson Comorbidity Index (CCI), widely used in the acquired HF population was used to measure comorbidity severity.12
ACHD Knowledge
ACHD Knowledge was measured using a 22-item survey developed by the investigator and based on the ACHD Patient Health Passport, a 7-page booklet used to store personal health information, including health history, health risks, and self-care needs.13 All questions are scored as correct or incorrect, summed for total score and then standardized on a 100-point scale.
Behavioral Characteristics
Behavioral characteristics evaluated in this study included depressive symptoms and self-care self-efficacy. Depressive symptoms were measured using the Patient Health Questionnaire-9 (PHQ-9), a widely used 9-item, self-reported scale14 with excellent reliability in ACHD populations (CA of 0.88).15 Self-care self-efficacy, or perceived confidence in self-care ability, was measured using the 6-item self-care confidence subscale of the SCI-ACHD.
Family Factors
Family factors measured in this study included family self-care self-efficacy and parental overprotection. Family self-care self-efficacy, or perceived support for self-care from family, and was measured using the 4-item Stanford Chronic Illness Family, Friends, and Community Self-Efficacy Scale.16 Language related to friends and community was removed from questions so that family remained the only support mechanism. Parental overprotection, a rating of attitudes and behaviors of parents in the first 16 years of life, was measured using the Parenting Bonding Inventory Overprotectiveness subscale,17 a 13-item scale with excellent reliability in the ACHD population (CA=0.89).18
Data Analysis
Descriptive statistics were analyzed for all study variables. All instruments were scored in accordance with author guidelines and Cronbach's α was calculated for the instruments not previously tested in the ACHD population. Bivariate relationships between individual, clinical, knowledge, behavioral, and family antecedents and each self-care construct (maintenance, monitoring, management) were determined using Pearson's correlation. Multivariate stepwise regression analysis was used to statistically evaluate the relationship between antecedent factors and each self-care construct. All antecedent factors (age, gender, race, education, insurance status, marital status, CHD severity, comorbidities, NYHA Class, depressive symptoms, self-care self-efficacy, parental overprotection, and perceived family support) were included in regression analysis. Factors entered the model at a .10 level of significance and stayed in the model at a .05 level of significance. Dichotomized data was used for race (white, nonwhite/other), education (high school graduate, any college or more), insurance status (private, public/uninsured), marital status (married/living with partner, widowed/divorced/single), and NYHA Class (I/II, III/IV). Multicollinearity was tested for in each regression model and no confounding was present (variance inflation factor <2). All data was analyzed using SPSS version 22 and an alpha set at 0.05.
Results
Sample Characteristics
Participants were on average 36 years old with slightly more females than males (Table 1). The majority of participants were Caucasian, had at least some college education, and private insurance. Approximately half of participants were married and had severe CHD, with the most common diagnoses being single ventricle physiology, Tetralogy of Fallot, and Transposition of the Great Arteries. The average participant was NYHA Class II and had 2 comorbidities. Mean for CHD Knowledge was 70.7 [SD, 13.5], with only 8% scoring at or below the 50th percentile indicating overall average to high levels of knowledge. The majority of participants had no depressive symptoms, but 15 (11.4%) persons screened positive for major depressive disorder and were followed-up according to study protocol. On average, participants scored somewhat to very confident on their self-care self-efficacy (mean 74.4 [SD, 13.9]). Participants were on average very confident in the support for self-care they received from family (mean 33.2, [SD 7.8]). Fifty-six (42.4%) of participants screened positive for parental overprotection (mean 12.6 [SD, 7.8]).
Table 1. Individual and Clinical Characteristics.
| Variable | Mean [SD]/N (%) |
|---|---|
| Age | 35.8 [11.4] |
| Gender | |
| Male | 59 (44.7) |
| Female | 73 (55.3) |
| Race | |
| White | 107 (81.1) |
| Black | 18 (13.6) |
| American Indian/Alaskan | 1 (0.8) |
| Asian | 4 (3.0) |
| >1 Race | 2 (1.5) |
| Marital Status | |
| Single | 57 (43.2) |
| Married | 63 (47.7) |
| Living with Partner | 5 (3.8) |
| Divorced | 6 (4.5) |
| Widowed | 1 (0.8) |
| Insurance | |
| Private | 81 (61.4) |
| Medicare/Medicaid | 43 (32.6) |
| Uninsured | 8 (6.1) |
| Education | |
| < High school | 2 (1.5) |
| High school | 59 (44.7) |
| College degree | 50 (37.9) |
| Graduate degree | 21 (15.9) |
| Heart Defect Severity | |
| Moderate | 61 (46.2) |
| Severe | 71 (53.8) |
| NYHA Class | |
| I | 22 (16.7) |
| II | 73 (55.3) |
| III | 36 (27.3) |
| IV | 1 (0.8) |
| Charlson Comorbidity Index | 1.61 [1.66] |
Internal consistency reliability for the SCI-ACHD was acceptable (self-care maintenance, CA=.62; self-care monitoring, CA=.73; self-care management, CA=.60; self-care confidence, CA=.83). Reliability of the ACHD Knowledge Survey was less than adequate, CA=0.59. Low internal consistency is evidenced in other knowledge surveys in this population and may indicate low conceptual relatedness between items.22 Reliability of the Stanford Chronic Illness Family, Friends, and Community Self-Efficacy Scale was excellent (CA=.83).
Description of Self-Care
Overall, persons scored a mean of 67.5 [SD, 13.7] on self-care maintenance, 57.2 [SD, 15.6] on self-care monitoring, and for the 86 persons who indicated that they experienced heart-related symptoms in the past month, a mean of 59.2 [SD, 18.7] on self-care management. Based on a cut-off score of 70 suggested by the developers of the original Self-Care Index for Heart Failure, less than half of the participants (44.7%) performed adequate levels of self-care maintenance, and only 27.3% and 23.3% performed adequate levels of self-care monitoring and management, respectively.11
Factors Associated with Self-Care
Individual factors: Being older, male, having at least some college education, and having public insurance/uninsured were all moderately associated with self-care (r=.19-.37, p<.05) (Table 2). Clinical factors: Having more comorbidities and being NYHA Class III/IV had a small to moderate association with self-care (r=.23-.30, p<.05). No statistically significant relationship was found between knowledge and self-care (r=.05-.06, p>.05) Behavioral factors: Lower levels of depressive symptoms and higher levels of self-care self-efficacy had a moderate relationship with self-care (r=.24-.32, p<.05). Family factors: Higher confidence in family support was moderately associated with self-care (r=.18-.29, p<.05).
Table 2. Bivariate Relationships Between Self-Care and Antecedent Factors.
| Antecedent Factor | Self-Care Maintenance (r, p-value) | Self-Care Monitoring (r, p-value) | Self-Care Management (r, p-value) |
|---|---|---|---|
| Age | -0.05, .57 | 0.37, <.001 | 0.08, .45 |
| Gender | 0.27, .002 | -0.14, .10 | -0.07, .51 |
| Race | 0.08, .39 | 0.06, .50 | -0.10, .38 |
| Education Level | 0.32, <.001 | -0.19, .03 | -0.07, .54 |
| Insurance Status | 0.16, .07 | -0.22, .01 | -0.05, .68 |
| Marital Status | 0.04, .68 | 0.10, .27 | -0.12, .26 |
| Severity Heart Defect | 0.10, .25 | 0.07, .41 | -0.03, .77 |
| NYHA Class | -0.14, .10 | 0.30, .001 | 0.18, .09 |
| Charlson Index | 0.13, .13 | 0.23, .008 | 0.15, .17 |
| ACHD Knowledge | 0.06, .50 | -0.05, .59 | -0.05, .66 |
| Depressive Symptoms | -0.29, .001 | 0.24, .005 | -0.05, .65 |
| Self-Care Self-Efficacy | 0.32, <.001 | 0.11, .21 | 0.20, .07 |
| Parental Overprotection | -0.18, .04 | -0.06, .50 | 0.01, .93 |
| Perceived Family Support | 0.29, .001 | -0.10, .24 | -0.01, .91 |
Regression Analysis
The results of the multivariate analyses are summarized in Table 3. In the final model for self-care maintenance, self-care self-efficacy, education level, gender, perceived family support, and the Charslon Comorbidity Index, explained 24.8% of the variance in maintenance behaviors (R2=.248, F(5, 123)=9.44, p<.001). Participants who were more confident in their abilities to perform self-care behaviors, had more than a high school education, were men, had higher levels of perceived family support, and a higher Charlson Comorbidity Index (indicating greater severity or number of comorbidities) had higher levels of self-care maintenance. In the final model for self-care monitoring, age, depressive symptoms, self-care self-efficacy, and NYHA Class explained 23.2% of the variance in monitoring behaviors (R2=.232, F(2, 124)=10.66, p<.001). Participants who were older, had higher levels of depressive symptoms, higher levels of confidence in abilities to perform self-care behaviors, and were NYHA Class III/IV (versus I/II) had higher levels of self-care monitoring. In the final model for self-care management, NYHA Class and self-care self-efficacy explained 9.4% of the variance in levels of self-care management (R2=.094, F(2, 80)=5.27, p=.007). Participants who had higher levels of confidence in abilities to perform self-care behaviors and were NYHA Class III/IV (versus I/II) had higher levels of self-care management.
Table 3. Multiple Regression Analysis.
| Self-Care | ||||
|---|---|---|---|---|
|
|
||||
| β | SE | p-value | Model Statistics | |
| Self-Care Maintenance | Model F=9.44; R2=.248 p<.001 | |||
| Self-care Self-efficacy | 1.13 | .33 | .001 | |
| ≤Highschool Education | -6.22 | 2.25 | .007 | |
| Male Gender | 4.94 | 2.21 | .027 | |
| Perceived Family Support | 0.31 | 0.14 | .032 | |
| Charlson Comorbidity Index | 1.32 | 0.66 | .046 | |
| Self-Care Monitoring | Model F=10.66;R2=.232 p<.001 | |||
| Age | 0.10 | 0.03 | <.001 | |
| Depressive Symptoms | 0.21 | 0.07 | .004 | |
| Self-care Self-efficacy | 0.27 | 0.09 | .004 | |
| NYHA Class III/IV | 1.62 | 0.71 | .025 | |
| Self-Care Management | Model F=5.27; R2=.094 p=.007 | |||
| Self-care Self-efficacy | 0.21 | 0.08 | .008 | |
| NYHA Class III/IV | 1.36 | 0.53 | .011 | |
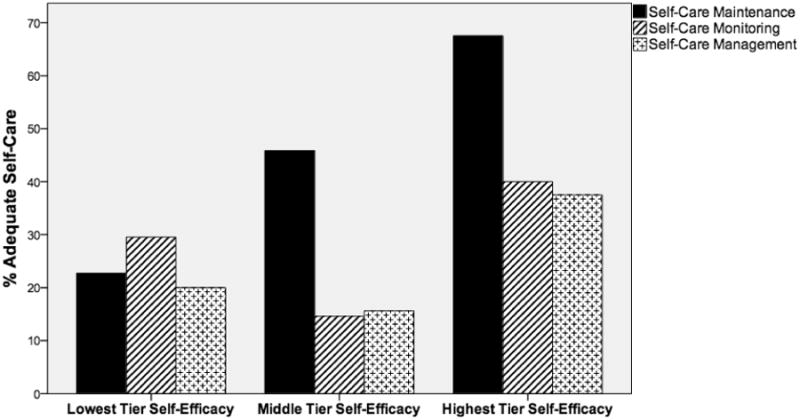
Self-care self-efficacy was the only antecedent factor that significantly contributed to each construct of self-care, explaining 10%, 2.3%, and 4.2% of the variance in self-care maintenance, monitoring, and management, respectively. Adequate levels of self-care maintenance, monitoring, and management (SCI-ACHD score >70) were found in 22%, 29%, and 20% of persons with the lowest tier of self-care self-efficacy versus 68%, 40%, and 39% of persons with the highest tier of self-care self-efficacy, respectively (Figure 2).
Figure 2. Relationship Between Adequate Level of Self-care and Self-efficacy.
Discussion
This is the first known study to report overall self-care levels in the ACHD population, and the results indicate that suboptimal self-care is common. Specific self-care behaviors frequently reported as suboptimal were physical activity, pregnancy related behaviors (birth control use and pre-pregnancy planning), stress reducing behaviors (recreation, sleep), and monitoring or management of symptoms. Low levels of physical activity and pregnancy planning are consistent with the current literature.6,7,20 Level of symptom self-care has not been previously reported, but is unsurprisingly low, as persons with ACHD may be less likely to see a change in their condition due to adaption to functional limitations over a lifetime. These particular self-care behaviors may be strategic areas for intervention development.
The factors associated with self-care behavior in this population included multiple domains of influence in concordance with the FSC Framework. Individual characteristics of self-care in this study included age, gender, and education level. Older age predicted higher levels of self-care monitoring, which may reflect the experience that older persons have with complications and symptoms. Females had lower levels of self-care maintenance, which may be due to the low levels of pregnancy-related self-care behaviors reported. However, this finding is consistent with other populations of chronically ill adults.21 The relationship between lower education level and self-care is also a consistent finding across multiple chronic conditions, including adults with other lifelong conditions.22,23
Race, marital status, and insurance status were not found to be predictors of self-care in this study. A lack of racial disparities in level of self-care is consistent with other studies on self-care behavior in this population.24 Marital status and insurance status, however, are often important predictors of level of self-care in other chronically ill populations. Persons who are in supportive marriages are known to have higher levels of self-care in acquired HF.25 In this study, half of participants were married, but most participants indicated that they had high levels of confidence for support from family whether they were or were not married. Adults with a lifelong condition may have access to broader family support since their families were their primary caregivers in childhood. In other populations, lack of insurance is known to influence self-care through access to care, and lack of insurance has been cited as a primary reason persons with ACHD have lapses in routine care.26 However, no relationship was found in this study.
Clinical characteristics of self-care in this study included NYHA Class and Charlson Comorbidity Index, but not type or severity of heart defect. This indicates that functional severity, rather than structural severity of ACHD is most important for self-care in this population. This finding is significant because while functional severity is an important classification of disease severity in the acquired HF population, it is not commonly used in the ACHD population. Instead, disease severity is classified by structural severity. In the similar adult cystic fibrosis population, disease severity also lacks significance in relationship with self-care. Rather, treatment burden is a critical factor, highlighting the importance of functional disability as a target for self-care interventions in adults living with a lifelong condition irrespective of starting point, i.e., type of heart defect.27 The direction of the relationship between self-care and functional severity is an interesting but not uncommon finding in other populations. Persons with greater functional limitations (lower NYHA Class) performed higher levels of self-care. Being sicker may indicate that a person is more experienced in dealing with his or her condition or more attuned to self-care needs due to being more symptomatic. Personal experience with ACHD may be an important factor in level of self-care, as it is in the acquired HF population.23
Increasing number and severity of comorbidities was significantly related to higher levels of self-care maintenance in this study. Comorbidities tend to increase the burden of self-care through complex medication regimens, difficulty distinguishing symptoms, and disease management conflicts.23 In the acquired HF population, for instance, comorbidities are associated with lower medication and diet adherence, difficulty interpreting healthcare professionals' instructions for multiple illnesses, and decreased self-efficacy.23 In this study, the relationship was opposite. That is, persons with more comorbidities were more likely to have higher levels of self-care maintenance. Of note, persons had on average only 2 comorbidities in this study, whereas in the acquired HF population, persons commonly average five or more comorbidities.28 A window may exist in which one or two comorbidities increases awareness and motivation to perform maintenance behaviors, but a higher number of comorbidities increases self-care complexity too much and reduces ability to perform maintenance behaviors. More objective clinical measures, such as ventricular function, may also be important antecedents of self-care, but were not explored in this study.
ACHD Knowledge was not associated with self-care in this study. Although knowledge is recognized as an important prerequisite of self-care, the lack of association has been reported in other populations.23 ACHD knowledge overall was average in this study, slightly better than the low levels of knowledge previously reported in this population. In a recent study in the acquired HF population, a lack of relationship between knowledge and self-care was explained by the interaction between knowledge and psychological distress.29 Persons with higher levels of depression and anxiety may be less likely to recognize or respond to symptoms despite have adequate knowledge of self-care.
Behavioral characteristics associated with self-care included self-care self-efficacy and depressive symptoms. The importance of self-care self-efficacy for self-care is consistent with other chronically ill populations including the similar adult cystic fibrosis population.11 In this study, depressive symptoms and self-care were related as expected, but the direction of the relationship was inconsistent with other populations.23 Higher level of depressive symptoms was related to higher level of self-care monitoring. It is possible that persons with higher levels of depressive symptoms may be more vigilant in watching for changes in their symptoms, whether or not this increased attention leads to better outcomes. Other behavioral characteristics unexplored in this study may also be important for self-care such as health beliefs and anxiety.
Family characteristics are increasingly recognized as an important factor influencing level of self-care in chronic illness, and in this study, a significant relationship was found between perceived confidence in family support and self-care maintenance even after adjusting for multiple individual, clinical, and behavioral antecedent factors.9 Support from family is generally positive, but it has also been shown to have a negative influence on self-care through critical or controlling behavior.30 Children growing up with a chronic illness experience more controlling behaviors, and in persons with ACHD, parental overprotection in childhood has been associated with symptoms of anxiety, health distress, and activity limitations.18 In this study, however, parental overprotection had no relationship with self-care. It is possible that other family factors, such as current family functioning, may be more important. From a clinical perspective, family is an integrative part of ACHD care, and future research should continue to pursue which factors could be targets for self-care interventions.
Limitations
Although this study fills an important gap in understanding ACHD self-care, it is not without limitations. First, validated measures of ACHD self-care have not been previously established in the literature. Although the instrument developed by the researcher in this study is based on a well-validated instrument in acquired HF, it may require additional revisions to improve reliability and validity. Also, self-care was measured via self-reported surveys and may not reflect actual behavior. Second, cross-sectional and descriptive design does not allow for the determination of cause and effect relationships. This study did, however, allow for the exploration of many potential antecedents of self-care to generate future hypotheses and guide intervention development. Also, participants were recruited from one ACHD center, potentially limiting generalizability of findings and causing selection bias as adults followed in non-specialty centers or those not currently engaged in routine care (as high as 60% in the United States26) were not included. The importance of antecedent factors of self-care may vary in these groups. Although multiple factors were identified as important for self-care, there may be other factors not represented in this study that may add to explanation of variance in self-care. Factors important in other populations include cognition, sleep, health literacy, patient-physician interactions, and general social support.23
Conclusions
The distribution of congenital heart disease has changed dramatically over the last four decades, with the burden of disease shifting from the acute, life-threatening illness of the newborn to the chronic, life-limiting illness of the adult.2 Evidence-based treatment and management of ACHD remains in its early stages, with the first AHA/ACC guidelines published just six years ago.10 The role of self-care, a vital component of chronic illness management, also remains evidence-scarce in this population. Overall, this study indicates that a large portion of persons with ACHD perform suboptimal levels of self-care. Certain behaviors may be particularly important for improvement including physical activity and pregnancy-related. Although some predictors of self-care in this study were nonmodifiable (age, gender, education level), these factors may help to identify persons at risk for suboptimal self-care. Modifiable risk factors including self-care self-efficacy and perceived confidence in family support may be important targets for future interventions to improve self-care in the ACHD population. Another important finding in this study was the difference between self-care maintenance, monitoring, and management. Varying factors best explained these constructs, indicating both the complexity of self-care and the importance of targeting different subpopulations or different interventions based on the aspect of self-care that is trying to be improved. Future research is needed in to shape guidelines and policies to support ACHD self-care. This study is an important first step in expanding the evidence-base for the specific antecedents associated with self-care in ACHD that will lead to the development of evidence-based interventions supporting self-care, and ultimately, improved quality and quantity of life for the ACHD population.
Acknowledgments
Grant Support: This study was partially funded by the National Institute of Nursing Research, F31NR01460901 and T32NR012715
Footnotes
Conflict of Interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Macmahon B, McKeown T, Record RG. The incidence and life expectation of children with congenital heart disease. Br Heart J. 1953 Apr;15(2):121–129. doi: 10.1136/hrt.15.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van der Bom T, Zomer AC, Zwinderman AH, Meijboom FJ, Bouma BJ, Mulder BJ. The changing epidemiology of congenital heart disease. Nat Rev Cardiol. 2011 Jan;8(1):50–60. doi: 10.1038/nrcardio.2010.166. [DOI] [PubMed] [Google Scholar]
- 3.Warnes CA. The adult with congenital heart disease: born to be bad? J Am Coll Cardiol. 2005 Jul 5;46(1):1–8. doi: 10.1016/j.jacc.2005.02.083. [DOI] [PubMed] [Google Scholar]
- 4.Gurvitz M, Verstappen A, Valente AM, Broberg C, Cook S, Stout K, Kay J, Ting J, Kuehl K, Earing M, Webb G, Opotowsky A, Graham D, Khairy P, Landzberg M. Prevalence and Predictors of Lapses in Care in Adults with Congenital Heart Disease (Health, Education And Access Research Trial, Heart-ACHD) 2011 [Google Scholar]
- 5.Yeung E, Kay J, Roosevelt GE, Brandon M, Yetman AT. Lapse of care as a predictor for morbidity in adults with congenital heart disease. Int J Cardiol. 2008 Mar 28;125(1):62–65. doi: 10.1016/j.ijcard.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 6.Dua JS, Cooper AR, Fox KR, Graham Stuart A. Physical activity levels in adults with congenital heart disease. Eur J Cardiovasc Prev Rehabil. 2007 Apr;14(2):287–293. doi: 10.1097/HJR.0b013e32808621b9. [DOI] [PubMed] [Google Scholar]
- 7.Bowater SE, Selman TJ, Hudsmith LE, Clift PF, Thompson PJ, Thorne SA. Long-term Outcome Following Pregnancy in Women with a Systemic Right Ventricle: Is the Deterioration due to Pregnancy or a Consequence of Time? Congenit Heart Dis. 2012 Sep 12; doi: 10.1111/chd.12001. [DOI] [PubMed] [Google Scholar]
- 8.Winter MM, Bouma BJ, van Dijk AP, Groenink M, Nieuwkerk PT, van der Plas MN, Sieswerda GT, Konings TC, Mulder BJ. Relation of physical activity, cardiac function, exercise capacity, and quality of life in patients with a systemic right ventricle. Am J Cardiol. 2008 Nov 1;102(9):1258–1262. doi: 10.1016/j.amjcard.2008.06.053. [DOI] [PubMed] [Google Scholar]
- 9.Dunbar SB, Clark PC, Quinn C, Gary RA, Kaslow NJ. Family influences on heart failure self-care and outcomes. J Cardiovasc Nurs. 2008 May-Jun;23(3):258–265. doi: 10.1097/01.JCN.0000305093.20012.b8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, del Nido P, Fasules JW, Graham TP, Jr, Hijazi ZM, Hunt SA, King ME, Landzberg MJ, Miner PD, Radford MJ, Walsh EP, Webb GD. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease) Circulation. 2008 Dec 2;118(23):e714–833. doi: 10.1161/CIRCULATIONAHA.108.190690. [DOI] [PubMed] [Google Scholar]
- 11.Riegel B, Lee CS, Dickson VV, Carlson B. An update on the self-care of heart failure index. J Cardiovasc Nurs. 2009 Nov-Dec;24(6):485–497. doi: 10.1097/JCN.0b013e3181b4baa0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 13.Adult Congenital Heart Association. Personal Health Passport. Cardiology ACo. 2013 ed. [Google Scholar]
- 14.Martin A, Rief W, Klaiberg A, Braehler E. Validity of the Brief Patient Health Questionnaire Mood Scale (PHQ-9) in the general population. Gen Hosp Psychiatry. 2006 Jan-Feb;28(1):71–77. doi: 10.1016/j.genhosppsych.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 15.Pike NA, Evangelista LS, Doering LV, Eastwood JA, Lewis AB, Child JS. Quality of Life, Health Status, and Depression: Comparison Between Adolescents and Adults After the Fontan Procedure With Healthy Counterparts. J Cardiovasc Nurs. 2011 Sep 9; doi: 10.1097/JCN.0b013e31822ce5f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lorig KR, Sobel DS, Ritter PL, Laurent D, Hobbs M. Effect of a self-management program on patients with chronic disease. Eff Clin Pract. 2001 Nov-Dec;4(6):256–262. [PubMed] [Google Scholar]
- 17.Parker G. The Parental Bonding Instrument: psychometric properties reviewed. Psychiatr Dev. 1989 Winter;7(4):317–335. [PubMed] [Google Scholar]
- 18.Ong L, Nolan RP, Irvine J, Kovacs AH. Parental overprotection and heart-focused anxiety in adults with congenital heart disease. Int J Behav Med. 2011 Sep;18(3):260–267. doi: 10.1007/s12529-010-9112-y. [DOI] [PubMed] [Google Scholar]
- 19.Yang HL, Chen YC, Wang JK, Gau BS, Chen CW, Moons P. Measuring knowledge of patients with congenital heart disease and their parents: validity of the ‘Leuven Knowledge Questionnaire for Congenital Heart Disease’. Eur J Cardiovasc Nurs. 2012 Mar;11(1):77–84. doi: 10.1177/1474515111429662. [DOI] [PubMed] [Google Scholar]
- 20.Drenthen W, Pieper PG, Roos-Hesselink JW, van Lottum WA, Voors AA, Mulder BJ, van Dijk AP, Vliegen HW, Yap SC, Moons P, Ebels T, van Veldhuisen DJ. Outcome of pregnancy in women with congenital heart disease: a literature review. J Am Coll Cardiol. 2007 Jun 19;49(24):2303–2311. doi: 10.1016/j.jacc.2007.03.027. [DOI] [PubMed] [Google Scholar]
- 21.Cameron J, Worrall-Carter L, Riegel B, Lo SK, Stewart S. Testing a model of patient characteristics, psychologic status, and cognitive function as predictors of self-care in persons with chronic heart failure. Heart Lung. 2009 Sep-Oct;38(5):410–418. doi: 10.1016/j.hrtlng.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 22.Kettler LJ, Sawyer SM, Winefield HR, Greville HW. Determinants of adherence in adults with cystic fibrosis. Thorax. 2002 May;57(5):459–464. doi: 10.1136/thorax.57.5.459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, Gurvitz MZ, Havranek EP, Lee CS, Lindenfeld J, Peterson PN, Pressler SJ, Schocken DD, Whellan DJ. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009 Sep 22;120(12):1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 24.Mackie AS, Ionescu-Ittu R, Therrien J, Pilote L, Abrahamowicz M, Marelli AJ. Children and adults with congenital heart disease lost to follow-up: who and when? Circulation. 2009 Jul 28;120(4):302–309. doi: 10.1161/CIRCULATIONAHA.108.839464. [DOI] [PubMed] [Google Scholar]
- 25.Graven LJ, Grant JS. Social support and self-care behaviors in individuals with heart failure: An integrative review. Int J Nurs Stud. 2013 Jul 11; doi: 10.1016/j.ijnurstu.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 26.Gurvitz M, Valente AM, Broberg C, Cook S, Stout K, Kay J, Ting J, Kuehl K, Earing M, Webb G, Houser L, Opotowsky A, Harmon A, Graham D, Khairy P, Gianola A, Verstappen A, Landzberg M. Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (The Health, Education, and Access Research Trial) J Am Coll Cardiol. 2013 May 28;61(21):2180–2184. doi: 10.1016/j.jacc.2013.02.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sawicki GS, Sellers DE, Robinson WM. High treatment burden in adults with cystic fibrosis: challenges to disease self-management. J Cyst Fibros. 2009 Mar;8(2):91–96. doi: 10.1016/j.jcf.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Page RL, 2nd, Lindenfeld J. The comorbidity conundrum: a focus on the role of noncardiovascular chronic conditions in the heart failure patient. Curr Cardiol Rep. 2012 Jun;14(3):276–284. doi: 10.1007/s11886-012-0259-9. [DOI] [PubMed] [Google Scholar]
- 29.Hwang B, Moser DK, Dracup K. Knowledge is insufficient for self-care among heart failure patients with psychological distress. Health Psychol. 2014 Jul;33(7):588–596. doi: 10.1037/a0033419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rosland AM, Heisler M, Piette JD. The impact of family behaviors and communication patterns on chronic illness outcomes: a systematic review. J Behav Med. 2012 Apr;35(2):221–239. doi: 10.1007/s10865-011-9354-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


