Abstract
The endocannabinoid system was discovered in 1988 but has received little attention for its potential therapeutic possibilities. That has started to change, and since 2000, a significant number of clinical trials of cannabinoids, principally for the control of spasticity in multiple sclerosis, have been undertaken. These studies have been difficult because of the nature of the disease and have involved patients for whom other therapies have failed or proved inadequate. This paper outlines the background to the use of cannabinoids available and discusses the principles of practice associated with their safe use. The focus has been on nabiximols, being the most studied and the only cannabinoid that has been both adequately researched for use in multiple sclerosis and granted a license by the regulators. However, what has emerged is that the effect for many patients can be much wider than just control of spasticity. Within and outside of neurology there seems to be an expanding range of possibilities for the therapeutic use of cannabinoids.
Electronic supplementary material
The online version of this article (doi:10.1007/s13311-015-0383-5) contains supplementary material, which is available to authorized users.
Key Words: Cannabinoids, pain, nabiximols, multiple sclerosis
Introduction
There is no doubt that multiple sclerosis (MS) and many other neurological conditions can be miserable diseases to have, potentially affecting all aspects of a person’s life. Not only may they experience progressive detrioration in the motor and other functions of the nervous system, but this is often accompanied by dreadful suffering from problems such as spasticity, neuropathic and nociceptive pain, dysaesthesia, cognitive dysfunction, lack of sleep, and anxiety and depression. This can also have a massive effect on the patient’s family, finances, employability, social life, and so on.
The only neurological disease that cannabinoids have been intensively investigated for is MS. There is some work on the use in chronic pain and emerging therapy for epilepsy and glioblastoma multiforma. However, is is reasonable to extrapolate from the experience gained both from the research and the clinical usage over the last 15 years, to inform the clinician on the practical aspects of the use of cannabinoids. Therefore, this paper will focus on the use in MS, although the author has experience in a wider range of diseases.
Current pharmacological research into MS has largely focused on disease-modifying therapies for the disease itself. However, there is some evidence that cannabinoids themselves have a disease-modifying effect [1]. Unfortunately, for many patients, control of many of the symptoms can prove difficult to achieve. There have been no recent advances in antispasticity medication, which has lead to the recommendation of use of medications such as diazepam and gabapetin for spasticity but with very limited data on effectiveness [2]. Therefore, there has been an urgent need to develop and assess new treatments.
There has now been >50 years of quality research into the basic science of cannabinoids since Mechoulam’s discovery of Δ9-tetrahydrocannabinol (THC) in 1964. The endocannabinoid system (ECS) was discovered in the late 1980s and has been shown to be a fundamentally important system controlling and modulating both neural and immune system activity [3, 4].
However, we have still barely started to explore the potential therapeutic benefits of these medicines for a number of reasons: 1) there has been a lack of appropriate medicinal grade cannabinoid materials; 2) the methods of delivery are limited and need development—smoking cannabis is not an option in modern medicine; 3) there is little widespread, accurate, and basic knowledge amongst health professionals of the ECS and its therapeutic potentials; 4) the media, politicians, and health authorities have even less understanding of the clinical potential of cannabinoids—commonly there is confusion between the therapeutic aspects, the recreational use, and perceived mental health problems; 5) the variable legal and regulatory frameworks in different nations make the widespread international introduction of medicinal cannabinoids very difficult; 6) currently, the cost of medicinal grade cannabinoids is high and holding back more widespread clinical usage, which is a result of the high cost of the research programmes to prove benefit and obtain licensing. Illicit cannabis is generally much cheaper, although of unknown quality and composition. As a result, many patients are prepared to commit an illegal act to obtain their cannabis when they cannot get medicinal grade material on prescription [5].
Potential Clinical Uses in Neurology
Cannabis has been used therapeutically for some 5000 years. Many of the uses being evaluated today with modern research techniques have appeared in observational studies dating back to the late 1800s. Had cannabis not been perceived to be addictive, principally because of the commercial and political skulduggery and the “Reefer Madness” campaigns in the 1930s, it is likely that it would have become an established element of clinical practice for a number of conditions. We now know that the clinical potential of cannabinoids appears to be wide, reflecting the ubiquitous nature of the ECS.
Currently, the major clinical trials of medicinal grade cannabinoids have been directed towards developing licenses for clinical use, which now include chemotherapy-induced nausea and vomiting (CINV), spasticity and spasms in MS, neuropathic and cancer pain, and AIDS-related anorexia. However, their use is only advocated when symptoms remain refractory to all other agents. Now that the safety of medicinal grade cannabinoids has been demonstrated, other uses are emerging. Many clinicians are resorting to prescribing “off label” in response to patient need.
MS
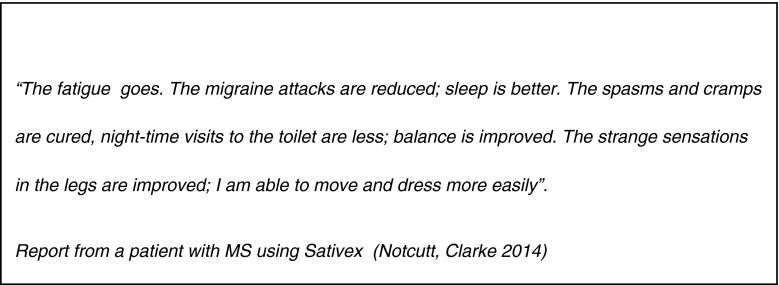
In the UK, in the 1990s, patients with MSc hampioned the use of cannabis as a medicine. This led to the development of a purified extract, nabiximols, allowing precise titration of a known amount. A series of randomized, placebo-controlled clinical trials with ongoing observational extension studies and other associated investigations, followed over the succeeding 12 years. The trials were difficult and complex owing to the heterogeneous nature of the symptoms of MS and the variety of responses that patients may experience from cannabinoids. The symptoms shown to be improved include spasticity, spasms, neuropathic pain, and bladder dysfunction, whilst also sometimes helping with fatigue, sleep disturbance, and dysesthesia [6–11] (Fig. 1). Consequently, the new combination cannabinoid therapy, nabiximols (Sativex; GWPharmaceuticals, Cambridge, UK), was eventually licensed in 2010 in the UK for spasticity and spasms in MS.
Fig. 1.
Report from a patient with multiple sclerosis using Sativex (GW Pharmaceuticals, Cambridge, UK) [5]
The Cannabis in Multiple Sclerosis randomized controlled trial by Zajicek et al. [12] assessed patient spasticity with a cannabis extract [principally a 2:1 ratio of THC and cannabidiol (CBD)], pure THC, or placebo—all used orally. They concluded that while there was no improvement shown when assessing spasticity on the Ashworth scale, there was an improvement in subjective perception of spasticity and also other secondary outcomes. In 2012, the Multiple Sclerosis and Extract of Cannabis trial concluded that the rate of relief of muscle stiffness in patients with MS patients after 12 weeks of therapy was doubled with the same cannabis extract compared with placebo [13].
Long-term Use in Spasticity and Spasms
Following on from some of the Nabiximols studies, many patients have had the option to enter extension studies to evaluate long-term effects. This has all been open-label, primarily assessing the maintenance of benefit alongside the possible emergence of side effects [14]. The most important outcome has been the maintenance or slow reduction of dosage used. An increase in dosage is rare, unlike with opiate use.
Additionally, Notcutt et al. [15] evaluated the ability of nabiximols to provide long-term relief from spasticity by assessing the effect of sudden withdrawal of the medicine after its use for at least 12 weeks, demonstrating the ongoing benefit patients were receiving, whilst also showing no evidence of a withdrawal syndrome. An observational study reviewed the benefits that patients continued to get with long-term use [16]: spasticity, pain, sleep, activities of daily living . This study also showed the improvements that the carers of the patients were experiencing.
Despite many patients stating that cannabis has altered the progression of their disease (and not merely their symptoms), no human trials have so far proved this. However, data from studies in animal models suggest some disease-modifying activity, which may augment the symptom control [1].
Neuropathic Pain
Neuropathic pain (due to central nerve damage) often accompanies MS. It is a type of pain that is commonly difficult to treat with conventional analgesic pharmacotherapy. Rog et al. [10] showed a benefit from nabiximols in MS, and this became an early indication for licensed use in Canada. There is also evidence to suggest that long-term use does not diminish the effects [17]. HIV sensory neuropathy has been studied based on smoked cannabis [18, 19].
Use as an analgesic agent beyond MS for chronic noncancer pain has been reviewed by Lynch and Campbell [20]. They recommended this as a modestly effective and safe treatment option for chronic noncancer (predominantly neuropathic) pain. Cichewicz et al. [21] and Karst et al. [22] stated that cannabinoids employ a different mechanism of action to opiates and therefore could augment an opiate effect and be a good possibility as an adjuvant choice for those with intractable pain. This would be the same rationale as the use of tricyclic antidepressants within chronic pain management. Migraine is another potential target [23]. Studies are also underway for the use of nabiximols in the treatment of cancer-related pain.
Other Emerging Uses in Neurological Disease
Whilst the focus has been on treating MS-related spasticity, there are other causes. The author has successfully treated patients with hereditary spasticity and stroke-related spasticity. Therefore, in situations where conventional medications have failed, cannabinoids present a potentially useful option.
In the nineteenth century cannabis was used for treating epilepsy, with varying results. More recently, CBD has been shown to be particularly effective in the treatment of intractable childhood epilepsies (e.g., Dravet’s syndrome etc.) [24]. Formal clinical trials are underway at present.
There is evidence that cannabinoids may have neuroprotective effects by down-regulation of excitatory amino acids such as glutamate, suggesting that there may be important effects in inflammatory and other neurological disease, including acute ischemia and trauma.
Glioblastoma multiforma is a particularly difficult brain tumor to treat successfully but enough evidence has emerged to start clinical trials of nabiximols as a form of chemotherapy. However, the desperation of patients with a variety of end-stage brain (and other) cancers is leading to the use of a variety of nonmedicinal cannabinoid preparations, based almost entirely on anecdotal evidence. Therefore, titrating the “medicine” of whatever source becomes little more than a guessing game.
The ECS is involved in the regulation of sleep, and patients in clinical trials have frequently identified significant improvements. They also identify the lack of a “hangover” effect, as is often seen with the use of opiates, tricyclic antidepressants, or hypnotics. Therefore, cannabinoids may have a major role for patients who suffer sleep disturbance because of chronic pain or other chronic illness [8]. Ware et al. [25] showed the benefit of nabilone in helping sleep in fibromyalgia.
Routes of Administration of Cannabinoids
Inhalational
The most common method of using cannabis recreationally is to smoke it. The heat vaporizes the ingredients whilst also converting THC acid into THC, thereby activating it. Inhalation produces a steep rise in the plasma levels, quickly beyond those needed for therapeutic use and often leading to the well-recognized effects of cannabis use. A further problem for the patient is that the smoke contains carcinogens, similarly to tobacco [26, 27].
No medicine is delivered by the inhalation of smoke. To avoid this, a vaporizer can be used, which will heat the plant material to a point whereby the cannabinoids are vaporized but avoids the smoke burning.
Undoubtedly, some patients can use these techniques with ease and control their intake. However, a novice patient with significant physical impairment from MS may find this impossible.
Oral
The oral route is slow in onset and the dose is difficult to titrate accurately because of slow and variable rates of absorption along with a “first pass” effect in the liver. Therefore, it maybe 1–2 h before benefit starts to be experienced.
Oro-mucosal
The oro-mucosal route gives rapid and direct access to the circulation through the mucosa of the mouth thereby avoiding the problems of the oral route. Titration is much easier to manage, and intermittent top-ups are easy.
Other
Other routes have been proposed (e.g., transdermal, parenteral, rectal) but the clinical need for these has yet to be established.
Available Medicinal Grade Cannabinoids
The available medicinal grade cannabinoids that are licensed for use varies from country to country. Similarly, the off-label use varies widely [28].
Nabilone is an analogue of THC and was originally licensed in 1985 for the treatment of CINV. Its use was supplanted by the development of the serotonin 5-HT3 receptor antagonists. Its availability only in a 1-mg oral form is a drawback to its use as an antiemetic (no parenteral form) [29]. Over the last 20 years there has been a minimal amount of research on its use beyond its license [30]. Titration can be difficult.
Dronabinol (synthetic THC) was also developed for the treatment of CINV and this has been extended to anorexia associated with weight loss in patients with AIDS. It is available in a range of capsule strengths or as an oral liquid thereby aiding titration.
Nabiximol is an extract of cannabis from cloned plants with an approximate 1:1 fixed ratio of THC to CBD [31]. This was developed in UK in response to widespread anecdotal reports that cannabis was a useful medicine for treating a number of MS-related symptoms. CBD was included to ameliorate side effects of THC.
It is administered oro-mucosally rather than swallowed. Absorption from the oral mucosa is slower than inhalation but this avoids the high plasma levels that occur with smoking or vaporizing. The route is also more rapid and consistent than the oral route. The results of studies in controlling spasticity in MS led to its UK license for use in this area [7].
Herbal cannabis of a medicinal grade (Bedrocan, Veendam, the Netherlands) has been developed. It is standardized and formally regulated as a medicine, and doctors can prescribe it. The usual methods of administration are as an oral infusion or vaporization.
In some countries, plant cannabis is sold as being of “medical grade”, and different types are promoted for different diseases. Oral cannabis extract as an oil is available in some places. In some areas, patients are allowed to grow small quantities of cannabis for their personal medicinal use. However, little, if any, of this will have been through any significant clinical trials for efficacy or quality controls as required by regulators for conventional medicines. However, knowledge of the pharmacology and of the experience gained from formal clinical trials can guide the clinician in optimizing the patient’s usage.
Managing the Patient in Clinical Practice
General Points
Currently, cannabinoids are seen as a treatment option when the conventional therapy has been ineffective or not tolerated. As with most medicines that affect the central nervous system (CNS), incremental dose titration is essential in order to achieve optimum effect and to minimize side effects. It is of no benefit to patients to exchange a state of immobility because of pain, spasticity, or nausea, for one of immobility caused by excessive plasma levels of cannabinoid.
Predicting response is an impossible art, particularly when other psychoactive medicines are being used. The most common side effects that determine dosing limits are drowsiness and dizziness, although sometimes these will lessen over time allowing for further small dose increases.
For most patients, initiating cannabinoids at night time is a good starting point, unless the patient is only symptomatic during the day. Many patients, particularly those with spasticity or pain problems, do not sleep well and so any drowsiness at night may lead to improved sleep with less fatigue and drowsiness during the day. This is often highly beneficial to partners/carers, too.
It is important to advise patients on the safe storage of their medicine in a similar way to opioids, especially if there are young people in the house. Informing others that such medicines are in the home might put oneself at risk of burglary.
Nabilone
When used for preventing CINV (its original designation), the manufacturers recommend a dosing of 1 or 2 mg twice a day, although this would often produce drowsiness and dysphoria. In the early 1990s some physicians, recognizing the therapeutic potential, started to explore other uses, particularly for pain and spasticity. From experience, the usual starting dose has been 1 mg, the only capsule strength available. However, this is often poorly tolerated owing to the above-mentioned side effects [32].
Experience has shown that the use of nabilone initially only at night commonly avoids the problem of drowsiness and dysphoria, with clinical benefit lasting well into the day. However, a lower-dose capsule (0.25 mg) would enable greater flexibility in titration of the optimum dose, particularly in daytime use.
Dronabinol
Dronabinol is primarily available in the USA but not in the UK. The principles of administration are similar to nabilone, with the benefit of a range of capsule strengths (2.5 mg, 5.0 mg, 10.0 mg capsules), making titration easier along with the ability to customize the dose more flexibly across the 24-h period.
Nabiximols (Sativex)
The oromucosal route was developed to provide a simple delivery system to enable a more convenient and accurate titration. Whilst the sublingual area is recommended, the buccal mucosa on the inside of the cheek is an alternative for some patients if the alcohol stings too much. As nabiximols may stimulate salivation, only 1 or 2 sprays should be used at one time and ideally the spray should be held in the mouth for at least 5 min or more to enable adequate absorption before swallowing or having a drink. A period of 15 min should elapse between spray applications.
The initial titration of nabiximols is a daily incremental increase of 1 spray dose, initially in the night and then the morning are targeted for dosing. However, this can be adjusted to include dosing at other times to customize according to the timing and severity of the symptoms being treated. Overall, the total daily dose should not increase by > 1 spray/day, to a maximum of 12/day—the limit at which the benefit is maximal. Some may consider this too slow but it has emerged as optimal to establish benefit with minimal side effects. Generally, the onset of drowsiness or dizziness is the limiting factor [33].
Comparative Doses
There have been no “head to head” studies comparing the effectiveness or dosing of the available medicinal cannabinoids. From clinical experience, 2 mg nabilone seems to be approximately equivalent to 8 sprays of nabiximols. In comparing nabiximols and dronabinol at equal THC levels the side effect profile is better with the former, probably because of the presence of CBD [34].
From the author’s clinical experience it is advised that careful titration should be undertaken when switching from one cannabinoid to another, especially if the patient is changing the mode of administration.
Breakthrough Pain, Spasms
Some patients may have significant fluctuations in their symptoms, and as with slow-release opiate therapy a breakthrough dose may be required. The oral preparations are slow in onset, and nabilone is particularly difficult to use in this way because of the lack of a range of doses. Nabiximols has a faster onset and is therefore more flexible. It should not be assumed that the breakthrough pain from another, unrelated disease process should be simply treated in this way.
Contraindications, Side Effects and Associated Issues
General Points
Most drugs that cross the blood–brain barrier have a range of adverse effects. Fortunately, medicinal cannabinoids seem to be remarkably benign and the side effect profile is well within the spectrum of problems seen with other psychoactive medicines used in neurology, psychiatry, and pain management. However, many patients may already be using other drugs that act on the CNS, thereby potentially increasing the risk of side effects.
It is important to realize that care should be taken in the elderly and the frail. Also, as there has been no significant research into the effect of cannabinoids in pregnant or lactating women, and children (<18 years old) the use in these patient groups is not advocated unless benefits outweigh the risks.
Contraindications
Long-term clinical trials have not identified any absolute contraindications as a result of other systemic disease processes. However, it would wise to exercise caution in use in severe cardiovascular, liver, kidney, and immunological disease, especially in acute illness. If a prescribed cannabinoid is controlling severe pain or spasticity, and so on, then stopping it suddenly may cause the patients to be plunged into a severe exacerbation of their symptoms, adding to the burden of their other medical problems [15].
Common side-effects of cannabinoids
Dizziness, drowsiness, and fatigue are common side effects, and usually determine the end point of dosing. The possibility of hypotonia may be a limiting factor for patients with MS to be aware of.
Gastrointestinal effects of diarrhea, nausea, and dry mouth sometimes occur. More specifically, nabiximols can cause hypersalivation, unpleasant taste, and a stinging sensation when given sublingually (oromucosally). Increased appetite is seen recreationally, but is not usually a problem with medicinal use [35].
Allergic phenomena are very rare.
Addiction and Abuse. At therapeutic levels of dosing it has been shown that the abuse potential of the clinical cannabinoids is very low [36–39]. There is no significant withdrawal syndrome from medicinal use [15, 36]. No evidence of tolerance to the effects of nabiximols with subsequent increased dose requirements has emerged in clinical trials to date [40, 41].
Euphoria is a common side effect of smoked cannabis owing to high plasma levels rapidly generated by inhaling it as a vapor. Orally and oromucosally, cannabinoids have a slower onset time and plasma levels are much lower. Therefore, the likelihood of a euphoric effect is also low when using these routes [40]. However, the nature of the cannabinoid used is also important and one may be more likely to see psychoactive effects when CBD is not a constituent. Incautious titration may lead to a relative overload for an individual, thereby generating euphoric, dysphoric, or intoxicating effects.
Psychosis is an associated risk for the regular recreational user of cannabis [42, 43], but this has not been demonstrated to be a problem for users of the medicinal preparations [44]. The likely important factors in this differentiation are the combination of much lower dosages, slower titration, and the presence of CBD, alongside the different end points of usage. Even so, it is still advised that medicinal cannabinoids should be avoided in patients with significant psychiatric disorders (e.g., psychosis, substance misuse disorders, personality disorders, etc.) until further data become available. However, it should be remembered that patients with MS can develop psychotic symptoms that are unrelated to their cannabinoid therapy (e.g., with severe acute infections such as pyelonephritis).
Anxiety and depression are very commonly associated with degenerative neurological diseases and chronic pain. The effective treatment of the underlying symptoms with cannabinoids may significantly improve these symptoms.
Panic and anxiety are side effects following overdose of cannabinoids and are therefore preventable with correct titration. These side effects are common features of uncontrolled recreational use. Memory changes and cognitive decline are possible side effects of cannabinoids, especially for the high-dose, long-term recreational user. Johns [45] stated that acute recreational cannabis use may cause confusion, and chronic use has been associated with amotivational syndrome. There is no evidence that this is a feature of medicinal cannabinoid use. MS itself can produce cognitive and memory changes.
Previous Recreational Cannabis Use
If the patient has a significant history of recreational cannabis use then the author will not prescribe medicinal cannabinoids, as there data and experience in prescribing for these patients are lacking. They may choose to continue to use their recreational source and this may render the use of medicinal cannabinoids pointless, as patients may look to find an end point of therapy in the range of the levels needed for recreational effects.
Driving
Different countries will have different attitudes and laws concerning driving and the use of cannabis (whether used recreationally or medicinally). Most will have yet to produce appropriate advice to patients. In the UK, recent law changes have targeted the recreational user. For the medicinal user, it is for them to determine their own fitness to drive. It may be that the underlying disease itself, its therapy, or other medication will hinders this. Most patients manage this decision satisfactorily. From studies of smoked cannabis in volunteers in driving simulators it has been shown that the main effects of cannabis on driving are: 1) that the ability to steer and maneuver may be mildly impaired; 2) that reaction times to sudden events may be increased; and 3) that the car is driven at a slower speed as the driver is aware of impairment [46].
Acute recreational cannabis consumption will increase the risk of accident [47, 48]. The likelihood of problems occurring with driving whilst using therapeutic doses is probably low. The intoxication levels in studies of therapeutic nabiximols show that these are little different from placebo [40]. The author cautions patients on driving not only within 4 h of cannabinoid ingestion, but also if their symptoms are poorly controlled (e.g., pain, spasticity, spasms etc.). The physician needs to document the advice given to the patient.
Overdose/Overload
In the medical literature, there is no recorded death directly from the ingestion of excess cannabis. The absence of cannabinoid receptors in the vital centers of the brain stem is probably the reason for this (in contrast to opiates, for example). However, patients need to realize the importance of careful titration to avoid significant side effects such as dizziness, drowsiness, dysphoria, or hypotonia . In the context of MS or any other neurological state there may be a risk of falls.
The best immediate treatment for an excessive dose of cannabinoid is to lie down and rest and symptoms will usually resolve in 2–3 h. A subsequent dose reduction of about 10–25 % is advised and physician guidance may be needed.
Assessing Outcomes
For most patients starting to use cannabinoids for the symptoms of a chronic neurological disease, an assessment of outcomes should occur between 2 and 4 weeks [40]. By this time, a clear indication as to whether the patient is benefitting from this therapy can normally be established. For responders, further “fine tuning” may be necessary to determine the optimum pattern in terms of dosing and timing across a 24-h period. For nabiximols, this may include increasing the number of uses of the spray at other times of day to establish a suitable maintenance regimen.
Those who fail to get any useful benefit should discontinue and no withdrawal phenomena would be expected. Sometimes a patient discovers after discontinuation that they were indeed getting benefit and these may be different to the original therapeutic targets. A retrial of therapy with different assessment parameters is indicated.
The principal scientific studies have focused on showing effectiveness for a single parameter (e.g., spasticity, pain. etc.). However, in practice, there are often improvements across a range of different symptoms many of which may be of significant value to the patient (Fig. 1). Therefore, the assessment needs to be customized to the individual.
Some have suggested that a patient should only continue with nabiximols if a 20 % improvement in spasticity has been obtained. However, it can be difficult to quantify the improvement in spasticity clinically over a period with the same degree of accuracy achieved in clinical trials. The effect of other benefits such as a reduction in the number of spasms, an improvement in sleep, and a benefit to the husband or wife in a reduction of their work load in caring for the patient, should all be included [16].
However, a recent study on the use of nabilone use in the UK showed a poor standard of evaluation of ongoing dosing, benefit. and side effects [20]. Therefore, a schedule of parameters to guide the physician/nurse evaluating the patient using a cannabinoid can be developed to reflect a varied range of information being collected in ordinary clinical practice (Table 1).
Table 1.
Cannabinoid assessment areas
| a) Pattern of dosing |
| b) Target symptoms evaluation |
| c) Side effect assessment |
| d) Patient’s activities of daily living |
| e) Carer’s activities of daily living |
| f) Changes to other medications |
Whether one uses a numeric rating score, widely used in the formal studies of effectiveness for spasticity and pain, or simple verbal rating scores or patient and carer descriptions of change, scores may vary according to the circumstances of cannabinoid use. To note that a patient stops screaming out in pain from spasms whenever she or he was being washed was a suitable parameter to measure (patient of the author).
Long-term Use of Cannabinoids
The long-term studies on nabiximols and the clinical experience from patients using medicinal cannabinoids for several years have indicated that the dose of cannabinoid remains relatively stable once an optimum dose has been established. Therefore, any reasons for increasing the dose need to be carefully evaluated.
So far there is no evidence of long term side effects emerging from studies of the use of prescribed cannabinoid medicines (e.g., dependency, tolerance, and mental health effects). Therefore, careful assessment of any apparent new problem is essential to determine etiology. It should be remembered that new CNS symptoms may not be caused by the patient’s cannabinoid therapy but by the underlying disease or its complications.
The same reassurances cannot be made for those using unregulated sources of cannabis of indeterminate quality and constituents. Many users may be taking quantities more often seen amongst recreational users than those in a formal clinical setting. Long-term studies of recreational users have largely focused on the psychiatric and the cognitive effects. The presence or absence of CBD may be a critical factor in the development of such problems, as it has antipsychotic properties.
Nabiximols has been evaluated as an add-on therapy for intractable symptoms, uncontrollable by established therapies. Therefore, once the overall benefit is established, the value of any other medicines needs to be reviewed to ensure optimum management of symptoms.
Economics
Like most new medicines, nabiximols is expensive, having gone through extensive research for current regulatory purposes. The other available cannabinoids (nabilone, dronabinol) did not have this level of scrutiny before their introduction 20–30 years ago.
Nabiximols has undergone economic evaluation with a very wide range of results, making it very difficult to assess the economics in everyday management [2, 49–51]. However, when compared with the disease-modifying drugs used in MS, all cannabinoids costs are much lower, on average.
Discontinuation of Cannabinoids
Patients who have been using cannabinoids on a long-term basis may wish or need to discontinue their cannabinoid either permanently or temporarily. In general, a short downward titration period of a few days would seem reasonable, although cannabinoids may take several weeks to be completely eliminated from the body. Patients may experience a return of their symptoms but a withdrawal syndrome is very unlikely, although sleep and mood may be upset temporarily [15].
There are a number of reasons for discontinuation. First, assessing symptom control after an initial titration period often helps to define the benefit gained. Second, a patient may develop an unrelated emergency condition or need elective surgery. So far, experience suggests that it is acceptable to continue with cannabinoid treatment unless there is an absolute contraindication. However, this needs to be assessed on an individual basis. If the cannabinoid is stopped then the symptoms of spasticity or pain may rapidly get worse, thereby adding to the burden of the disease process. Pain from an injury or another disease should be treated in the normal way, using conventional pain-management strategies. Finally, if patients wish to travel abroad, they will need advice on the regulations for carrying cannabinoids into another country, especially outside Europe. An embassy should be able to provide information about the local regulations and the legality. In the UK, a Home Office license is not needed for users when leaving the country. Patients should always carry a letter detailing their travel arrangements, medical condition, and the medicines they will be carrying. A contact telephone number for the patient’s ordinary doctor is also useful.
Conclusion
Although the use of cannabis as a medicine has a long history, its formal use in modern medicine is still in its infancy. Whilst there is still very little research into this therapeutic area in comparison with other established medicines, the safety profile is impressive. The development of medicinal grade products has allowed high-quality research, particularly in the field of MS. This has led to a higher quality of research when set against, for example, previous studies on medicines for spasticity [52].
As with any new class of medicine, it takes time to establish a widespread clinical experience. This needs to start with an understanding of the basic science but, sadly, teaching on the ECS is still minimal, despite 20 years of knowledge of the system.
Undoubtedly, there will be more to learn on the practical use of medicinal cannabinoids as new therapeutic areas emerge and as confidence in their use as medicines grows.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(PDF 1224 kb)
Acknowledgments
Conflicts of Interest
The author has participated on a number of research studies on nabiximols and nabilone. He has participated in advisory boards and undertaken teaching sessions on cannabinoids for a number of pharmaceutical companies.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Scotter EL, Abood ME, Glass M. The endocannabinoid system as a target for the treatment of neurodegenerative disease. Br J Pharmacol. 2010;160:480–498. doi: 10.1111/j.1476-5381.2010.00735.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute for Health and Care Excellence. Multiple sclerosis. Management of multiple sclerosis in primary and secondary care. NICE clinical guideline 186. Available at: http://guidance.nice.org.uk/cg186. Accessed 17 Aug 2015. [PubMed]
- 3.Pertwee RG. Targeting the endocannabinoid system with cannabinoid receptor agonists: pharmacological strategies and therapeutic possibilities. Philos Trans R Soc Lond B Biol Sci. 2012;367:3353–3363. doi: 10.1098/rstb.2011.0381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skaper RD, Di Marzo V. Why do cannabinoid receptors have more than one endogenous ligand? Philos Trans R Soc Lond B Biol Sci. 2012;367:3216–3228. doi: 10.1098/rstb.2011.0382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Notcutt W, Clarke E. Cannabinoids in clinical practice: A UK perspective. In: Pertwee R (ed.) Handbook of cannabis, Oxford University Press, Oxford, 2014; p. 415-432
- 6.Wade DT, Collin C, Stott C, Duncombe P. Meta-analysis of the efficacy and safety of Sativex (nabiximols), on spasticity in people with multiple sclerosis. Mult Scler. 2010;16:707–714. doi: 10.1177/1352458510367462. [DOI] [PubMed] [Google Scholar]
- 7.Novotna A, Mares J, Ratcliffe S, et al. A randomized, double-blind, placebo-controlled, parallel-group, enriched-design study of nabiximols (Sativex), as add-on therapy, in subjects with refractory spasticity caused by multiple sclerosis. Eur J Neurol. 2011;18:1122–1131. doi: 10.1111/j.1468-1331.2010.03328.x. [DOI] [PubMed] [Google Scholar]
- 8.Vermersch P. Sativex® (Tetrahydrocannabinol + Cannabidiol), an endocannabinoid system modulator: basic features and main clinical data. Exp Rev Neurother. 2011;11:15–19. doi: 10.1586/ern.11.27. [DOI] [PubMed] [Google Scholar]
- 9.Collin C, Ehler E, Waberzinek G, et al. A double-blind, randomized, placebo controlled, parallel-group study of Sativex, in subjects with symptoms of spasticity due to multiple sclerosis. Neurol Res. 2010;32:451–459. doi: 10.1179/016164109X12590518685660. [DOI] [PubMed] [Google Scholar]
- 10.Rog DJ, Nurmikko TJ, Friede T, Young CA. Randomized, controlled trial of cannabis based medicine in central pain in multiple sclerosis. Neurology. 2005;65:812–819. doi: 10.1212/01.wnl.0000176753.45410.8b. [DOI] [PubMed] [Google Scholar]
- 11.Brady CM, DasGupta R, Dalton C, et al. An open-label pilot study of cannabis-based extracts for bladder dysfunction in advanced multiple sclerosis. Mult Scler. 2004;10:425–433. doi: 10.1191/1352458504ms1063oa. [DOI] [PubMed] [Google Scholar]
- 12.Zajicek J, Fox P, Sanders H, et al. Cannabinoids for treatment of spasticity and other symptoms related to multiple sclerosis (CAMS study): multicentre randomised placebo-controlled trial. Lancet. 2003;362:1517–1526. doi: 10.1016/S0140-6736(03)14738-1. [DOI] [PubMed] [Google Scholar]
- 13.Zajicek JP, Hobart JC, Slade A, Barnes D, Mattison PG. Multiple sclerosis and extract of cannabis: results of the MUSEC trial. J Neurol Neurosurg Psychiatry. 2012;83:1125–1132. doi: 10.1136/jnnp-2012-302468. [DOI] [PubMed] [Google Scholar]
- 14.Serpell M, Notcutt W, Collin C. Sativex long-term use: an open-label trial in patients with spasticity due to multiple sclerosis. J Neurol. 2013;260:285–295. doi: 10.1007/s00415-012-6634-z. [DOI] [PubMed] [Google Scholar]
- 15.Notcutt W, Langford R, Davies P, Ratcliffe S, Potts R. A placebo-controlled, parallel-group, randomized withdrawal study of subjects with symptoms of spasticity due to multiple sclerosis who are receiving long-term Sativex® (nabiximols) Mult Scler. 2012;18:219–228. doi: 10.1177/1352458511419700. [DOI] [PubMed] [Google Scholar]
- 16.Notcutt WG. A questionnaire survey of patients and carers of patients prescribed Sativex as an unlicensed medicine. Prim Health Care Res Dev. 2012;12:1–8. doi: 10.1017/S1463423612000333. [DOI] [PubMed] [Google Scholar]
- 17.Nurmikko TJ, Serpell MG, Hoggart B, et al. Sativex successfully treats neuropathic pain characterised by allodynia: a randomised, double-blind, placebo-controlled clinical trial. Pain. 2007;133:210–220. doi: 10.1016/j.pain.2007.08.028. [DOI] [PubMed] [Google Scholar]
- 18.Abrams DI, Jay CA, Shade SB, et al. Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trial. Neurology. 2007;68:515–521. doi: 10.1212/01.wnl.0000253187.66183.9c. [DOI] [PubMed] [Google Scholar]
- 19.Ellis RJ, Toperoff W, Vaida F, et al. Smoked medicinal cannabis for neuropathic pain in HIV: a randomized, crossover clinical trial. Neuropsychopharmacology. 2009;34:672–680. doi: 10.1038/npp.2008.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lynch ME, Campbell F. Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials. Br J Clin Pharmacol. 2011;72:735–744. doi: 10.1111/j.1365-2125.2011.03970.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cichewicz DL, Martin ZL, Smith FL, Welch SP. Enhancement mu opioid antinociception by oral delta9-tetrahydrocannabinol: dose-response analysis and receptor identification. J Pharmacol Exp Ther. 1999;289:859–867. [PubMed] [Google Scholar]
- 22.Karst M, Wippermann S, Ahrens J. Role of cannabinoids in the treatment of pain and (painful) spasticity. Drugs. 2010;70:2409–2438. doi: 10.2165/11585260-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 23.Russo E. Clinical endocannabinoid deficiency (CECD): can this concept explain therapeutic benefits of cannabis in migraine, fibromyalgia, irritable bowel syndrome and other treatment-resistant conditions? Neuroendocrinol Lett. 2004;25:31–39. [PubMed] [Google Scholar]
- 24.Devinsky O, Cilio M, Cross H, et al. Cannabidiol: Pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders. Epilepsia. 2014;55:791–802. doi: 10.1111/epi.12631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ware MA, Fitzcharles MA, Joseph L, Shir Y. The effects of nabilone on sleep in fibromyalgia: results of a randomized controlled trial. Anesth Analg 2010;110(2):604-10. [DOI] [PubMed]
- 26.Hall W. The respiratory risks of cannabis smoking. Addiction. 1998;93:1461–1463. doi: 10.1080/09652149834586. [DOI] [PubMed] [Google Scholar]
- 27.Henry JA, Oldfield WLG, Kon OM. Comparing cannabis with tobacco. BMJ. 2003;326:942–943. doi: 10.1136/bmj.326.7396.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnson C. Shared care guideline: Nabilone in the management of chronic neuropathic pain that has failed to respond to other first and second line treatments. NHS Lincolnshire in Association with United Lincolnshire Hospitals Trust, 2013. https://www.google.co.uk/?gws_rd=ssl#q=nabilone+licensed+indications.
- 29.Flynn J, Hanif N. Nabilone for the management of intractable nausea and vomiting in terminally staged AIDS. J Palliat Care. 1992;8:46–47. [PubMed] [Google Scholar]
- 30.Notcutt W, Phillip C, Hughe J, LacouX P, Vijayakulasingam V, Baldock L. A retrospective description of the use of nabilone in uk clinical practice – extension study. British Pain Society Annual Scientific Meeting 2015, Glasgow: Poster Presentation; 2015.
- 31.Russo E, Guy GW. A tale of two cannabinoids: the therapeutic rationale for combining tetrahydrocannabinol and Cannaidiol. Med Hypotheses. 2006;66:234–246. doi: 10.1016/j.mehy.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 32.Notcutt W, Price M, Chapman G. Clinical experience with nabilone for chronic pain. Pharm Sci. 1997;3:551–555. [Google Scholar]
- 33.GW Pharmaceuticals. Sativex—summary of product characteristics. Available at: http://www.gwpharm.com/. Accessed 17 Aug 2015.
- 34.Johnson JR, Burnell-Nugent M, Lossignol D, et al. Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC: CBD extract and THC extract in patients with intractable cancer-related pain. J Pain Symptom Manag. 2010;39:167–179. doi: 10.1016/j.jpainsymman.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 35.Strasser F, Luftner D, Possinger K, et al. Comparison of orally administered cannabis extract and delta-9-tetrahydrocannabinol in treating patients with cancer-related anorexia-cachexia syndrome: a multicenter, phase III, randomized, double-blind, placebo-controlled clinical trial from the Cannabis-In-Cachexia-Study-Group. J Clin Oncol. 2006;24:3394–3400. doi: 10.1200/JCO.2005.05.1847. [DOI] [PubMed] [Google Scholar]
- 36.Nutt DJ, King LA, Phillips LD. Independent Scientific Committee on Drugs. Drug harms in the UK: a multicriteria decision analysis. Lancet. 2010;376:1558–1565. doi: 10.1016/S0140-6736(10)61462-6. [DOI] [PubMed] [Google Scholar]
- 37.Schoedel KA, Chen N, Hilliard A, et al. A randomized, double blind, placebo controlled, crossover study to evaluate the subjective abuse potential and cognitive effects of nabiximols oromucosal spray in subjects with a history of recreational cannabis use. Hum Psychopharmacol. 2011;26:224–236. doi: 10.1002/hup.1196. [DOI] [PubMed] [Google Scholar]
- 38.Calhoun SR, Galloway GP, Smith DE. Abuse potential of dronabinol (Marinol) J Psychoactive Drugs. 1998;30:187–196. doi: 10.1080/02791072.1998.10399689. [DOI] [PubMed] [Google Scholar]
- 39.Ware MA, St A-TE. The abuse potential of the synthetic cannabinoid nabilone. Addiction. 2010;105:494–503. doi: 10.1111/j.1360-0443.2009.02776.x. [DOI] [PubMed] [Google Scholar]
- 40.Wade D. Evaluation of the safety and tolerability profile of Sativex: is it reassuring enough? Exp Rev Neurother. 2012;12:9–14. doi: 10.1586/ern.12.12. [DOI] [PubMed] [Google Scholar]
- 41.Robson P. Abuse potential and psychoactive effects of d-9-tetrahydrocannabinol and Cannabidiol oromucosal spray (Sativex), a new cannabinoid medicine. Exp Opin Drug Saf. 2011;10:675–685. doi: 10.1517/14740338.2011.575778. [DOI] [PubMed] [Google Scholar]
- 42.Henquet C, Krabbendam L, Spauwen J, et al. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ. 2005;330:11. doi: 10.1136/bmj.38267.664086.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Degenhardt L, Hall W. Cannabis and psychosis. Curr Psychiatry Rep. 2002;4:191–196. doi: 10.1007/s11920-002-0026-5. [DOI] [PubMed] [Google Scholar]
- 44.Aragona M, Onesti E, Tomassini V, et al. Psychopathological and cognitive effects of therapeutic cannabinoids in multiple sclerosis: a double-blind, placebo controlled, crossover study. Clin Neuropharmacol. 2009;32:41–47. doi: 10.1097/WNF.0B013E3181633497. [DOI] [PubMed] [Google Scholar]
- 45.Johns A. Pyschiatric effects of cannabis. Br J Psychiatry. 2001;178:116–122. doi: 10.1192/bjp.178.2.116. [DOI] [PubMed] [Google Scholar]
- 46.Sexton BF, Tunbridge RJ, Brook-Carter N, et al. The influence of cannbis on driving. UK Transport Research Laboratory, Report 477, 2000. Available at: http://www.erowid.org/plants/cannabis/cannabis_driving6.pdf. Accessed 17 Aug 2015.
- 47.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344 doi: 10.1136/bmj.e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Englehart K, Sexton BF, Tunbridge RJ, et al. The influence of cannabis on driving. Available at: http://www.erowid.org/plants/cannabis/cannabis_driving6.pdf. Accessed 17 Aug 2015.
- 49.Slof J, Gras A. Sativex® in multiple sclerosis spasticity: a cost-effectiveness model. Expert Rev Pharmacoecon Outcomes Res. 2012;12:525–538. doi: 10.1586/erp.12.40. [DOI] [PubMed] [Google Scholar]
- 50.Flachenecker P. A new multiple sclerosis spasticity treatment option: effect in everyday clinical practice and cost-effectiveness in Germany. Exp Rev Neurother. 2013;13(3 Suppl. 1):15–19. doi: 10.1586/ern.13.1. [DOI] [PubMed] [Google Scholar]
- 51.AWMSG Secretariat Assessment Report. Delta-9-tetrahydrocannabinol/ Cannabidiol (Sativex®). All Wales Therapeutics and Toxicology Centre. Reference number: 644. July 2014.
- 52.Shakespeare DT, Boggild M, Young C. Anti-spasticity agents for multiple sclerosis. Cochrane Database Syst Rev. 2003;4:CD001332. doi: 10.1002/14651858.CD001332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)