Abstract
Objective
The goal of this study was to evaluate the pregnancy potential of immature (metaphase I or germinal vesicle stage) oocytes retrieved in intracytoplasmic sperm injection (ICSI) cycles.
Methods
A total of 1,871 couples with infertility underwent 2,984 ICSI cycles. Cycles in which three or fewer oocytes were retrieved were included in this study in order to evaluate the pregnancy potential of immature oocytes. Cycles were divided into five groups (group I-V), according to the maturation status of the oocytes at the time of cumulus cell removal and ICSI. The fertilization and pregnancy rates after ICSI were analyzed and compared among the study groups based on the maturation status of the retrieved oocytes.
Results
The retrieval of only immature oocytes was associated with a significant decrease in the fertilization rate (76.1%±37.3% vs. 49.0%±49.1%, 66.7%±48.7%; group I vs. group II, group III, respectively) and the average number of transferred embryos (1.5±0.7 vs. 1.1±0.4, 1.1±0.6). The cycle cancellation rate was significantly higher when only immature oocytes were retrieved. The clinical pregnancy rate decreased significantly when the transferred embryos had originated from immature oocytes (16.9% vs. 10.3%, 1.2%).
Conclusion
In ICSI cycles, the fertilization potential and pregnancy potential of the immature oocytes retrieved in ICSI cycles were inferior to those of mature oocytes. Therefore, increasing the number of injectable oocytes and transferrable embryos by using immature oocytes after their spontaneous in vitro maturation does not necessarily improve pregnancy outcomes.
Keywords: Fertilization, In vitro maturation, Intracytoplasmic sperm injection, Mature oocyte, Pregnancy
Introduction
Controlled ovarian hyperstimulation has typically been performed using exogenous gonadotropin as part of in vitro fertilization (IVF) and embryo transfer programs in order to retrieve a large number of oocytes. Retrieved oocytes exist in one of three maturation stages: mature metaphase II (MII), immature metaphase I (MI), and immature germinal vesicle (GV) oocytes. Moreover, the maturation profiles of retrieved oocytes varies among patients. Immature oocytes are generally discarded in intracytoplasmic sperm injection (ICSI) cycles if the majority of the retrieved oocytes are mature. However, immature oocytes also are potential sources of embryos, which is an especially relevant consideration when all or most of the retrieved oocytes are immature. Moreover, several studies have confirmed that both normal pregnancies and live births have been achieved from embryos originating from immature oocytes [1,2,3,4,5].
According to recent studies, immature oocytes constitute between 15% and 20% of the total population of retrieved oocytes in stimulated cycles [6,7]. It is not yet known why some retrieved oocytes are immature. Two potential explanations have been proposed: first, heterogeneous follicles at different developmental stages at the starting time of ovarian hyperstimulation lead to different stages of oocyte maturation [8]; second, aspiration of the small antral follicle during oocyte retrieval can obtain oocytes in different stages of maturation [9,10]. Most immature oocytes undergo nuclear maturation spontaneously within 24 hours after oocyte retrieval and reach the final stage of nuclear maturation, metaphase II [11]. This process of spontaneous in vitro maturation (IVM) can take place rapidly. Therefore, oocytes that have matured in vitro can be injected with sperm to increase the number of transferrable embryos in ICSI when a low number of mature oocytes have been retrieved. Moreover, immature oocytes that do not mature on the day of oocyte retrieval can also undergo maturation overnight. When all or most of the injected oocytes are not fertilized, ICSI can be performed on these oocytes that have matured in vitro. However, in vitro-matured oocytes have been shown to exhibit a lower fertilization rate, abnormal embryonic development, frequent developmental blocks, retarded development, and lower implantation rates than in vivo-matured oocytes [4,5,12,13,14,15,16,17,18,19,20,21]. Moreover, in addition to showing lower developmental potential, in vitro-matured oocytes also show a lower potential for pregnancy. Therefore, the spontaneous abortion rate has been shown to be high in pregnancies achieved from embryos originating from immature oocytes obtained from stimulated cycles [4,5]. The low developmental and pregnancy potential of in vitro-matured oocytes remains a major hurdle to be overcome in the human oocyte IVM field. The low developmental and pregnancy potential of immature oocytes retrieved from stimulated cycles appears to result from suboptimal culture conditions that fail to support the cytoplasmic maturation of the oocytes [11].
Although immature oocytes retrieved together with mature oocytes in stimulated cycles have been shown to have low developmental and pregnancy potential, the clinical use of these immature oocytes may still be worthwhile. This is because the numbers of injectable oocytes can be increased at the time of ICSI, especially when only a low number of mature oocytes are retrieved. However, no evidence appears to indicate that increasing the number of injectable oocytes using immature oocytes retrieved from stimulated cycles actually increases pregnancy rates. Therefore, the present study evaluated the fertilization rate and pregnancy potential of immature oocytes retrieved from ICSI cycles in which a low number of oocytes were retrieved. Furthermore, this study evaluated whether the clinical use of immature oocytes, along with mature oocytes, increases pregnancy rates.
Methods
1. Patients
This study was approved by the institutional review board of Cheil General Hospital and Women's Healthcare Center. A preliminary study analyzed the percentage of ISCI cycles performed between 2011 and 2013 in which only immature oocytes were retrieved. A total of 4,332 cycles were analyzed, and only immature oocytes were retrieved in 127 cycles (2.9%) at the time of cumulus cell removal. Immature oocytes were retrieved along with mature oocytes in 4,205 cycles (97.1%) and the immature oocytes had not matured at the time of ICSI in 3,141 cycles (72.5%). The proportion of cycles in which immature oocytes were retrieved was again analyzed based on the number of retrieved oocytes. Only immature oocytes were retrieved in 0.4% of cycles (10 cycles) in which four or more oocytes (2,728 cycles) were retrieved and in 7.3% of cycles (117 cycles) in which three or fewer oocytes (1,604 cycles) were retrieved. Moreover, in cycles in which four or more oocytes were retrieved, only embryos originating from mature oocytes were transferred, while in cycles in which three or fewer oocytes were retrieved, embryos obtained from immature oocytes were transferred along with embryos originating from mature oocytes. Cycles in which four or more oocytes were retrieved, but only embryos originating from immature oocytes were transferred, were rare. Therefore, those cycles were excluded from this study, and only cycles in which three or fewer oocytes were retrieved were analyzed to evaluate the fertilization and pregnancy potential of embryos originating from oocytes that were immature at the time of oocyte retrieval. The inclusion criteria included couples who underwent an ICSI cycle from January 2003 to October 2013, in which three or fewer oocytes were retrieved. Couples were divided into five groups, according to the maturation status of the oocytes at the time of cumulus cell removal and ICSI. Group I included cycles in which immature oocytes coexisted with mature oocytes at the time of cumulus cell removal, but the immature oocytes had not yet matured at the time of ICSI (2,558 cycles). Group II included cycles in which only immature oocytes were retrieved at the time of cumulus cell removal, and some of these immature oocytes had matured at the time of ICSI (84 cycles). Group III included cycles in which only immature oocytes existed at the time of cumulus cell removal and ICSI, and some of these oocytes had matured 1 day after oocyte retrieval (103 cycles). Group IV included cycles in which immature oocytes coexisted with mature oocytes at the time of cumulus cell removal, and some of these immature oocytes had matured at the time of ICSI (119 cycles). Group V included cycles in which immature oocytes coexisted with mature oocytes at the time of cumulus cell removal, and some of these immature oocytes had matured 1 day after oocyte retrieval (120 cycles).
2. Controlled ovarian stimulation
Pituitary blockage was performed using either a gonadotropin-releasing hormone agonist or antagonist. Controlled ovarian stimulation was achieved with a daily dose of human menopausal gonadotropin or urinary or recombinant follicle-stimulating hormone, starting on the third day of the menstrual cycle. Follicular growth was monitored by transvaginal ultrasound examination, beginning on the fourth day of gonadotropin administration. When adequate follicular growth and serum E2 levels were observed, urinary or recombinant human chorionic gonadotropin was administered. Oocytes were then retrieved transvaginally under ultrasound guidance 36 hours after human chorionic gonadotropin administration.
3. Preparation of oocytes
Cumulus cells were removed approximately 2 hours after oocyte retrieval. During this time, oocytes were maintained in fertilization medium (Vitrolife, Göteborg, Sweden) supplemented with 10% recombinant human serum albumin (Vitrolife) or fertilization medium (Sage, Trumbull, CT, USA) supplemented with 5% human serum albumin (Sage) and covered with paraffin oil (Sage). Cumulus cells were removed after a short exposure to Hyase (Vitrolife), which contained hyaluronidase (80 IU/mL). The remaining cumulus cells were mechanically removed by gentle pipetting with a hand-drawn pipette.
The maturation status of each oocyte was evaluated using an inverted microscope (Nikon, Tokyo, Japan) and recorded. Mature MII-stage oocytes were separated from immature MI- and GV-stage oocytes and maintained independently. The maturation status of the immature oocytes was assessed again just before ICSI (4 hours after oocyte retrieval) on an inverted microscope. Immature oocytes were maintained in G1 medium (Vitrolife) supplemented with 5% recombinant human serum albumin or cleavage medium (Sage) supplemented with 10% serum protein substitute (Sage), and covered with paraffin oil. Oocytes were cultured overnight at 37℃ in a humidified atmosphere with 6% CO2. The maturation status of the immature oocytes that did not mature on the day of oocyte retrieval was assessed again on the day after oocyte retrieval, and ICSI was performed on mature oocytes observed on that day if all or most of the oocytes that had been injected with sperm on the day of oocyte retrieval had not been fertilized.
4. Intracytoplasmic sperm injection
ICSI was performed on the heated stage of an inverted microscope in a microinjection dish (Thermo Scientific, New York, NY, USA), prepared with droplets of Gamete medium (Vitrolife) and covered with paraffin oil. Approximately 16 hours after ICSI, fertilization was confirmed by the presence of two pronuclei and the extrusion of the second polar body. Embryos were maintained in a 50-µL drop of G1 medium (Vitrolife) or cleavage medium (Sage), supplemented with a 5% to 10% protein supplement, and covered with paraffin oil. Embryos were incubated in a humidified atmosphere with 6% CO2 at 37℃. Replacement of the embryos was carried out between the second day and the fourth day. Embryo quality was assessed on the morning of the day of embryo replacement. Embryos with even or slightly uneven blastomeres and ≤10% cytoplasmic fragmentation were classified as good embryos. Good embryos were also required to be ≥4-cells, ≥7-cells, and having reached at least the compaction stage on day 2, day 3, and day 4 replacement, respectively. In groups IV and V, embryos originating from mature oocytes were transferred when in vitro-matured oocytes had not been fertilized. Contrastingly, embryos derived from immature oocytes were transferred when mature oocytes had not been fertilized. In some cases, embryos originating from both mature and immature oocytes were transferred simultaneously. Clinical pregnancy was ascertained by confirming the fetal heartbeat using ultrasonography at 6 or 7 weeks of gestation. Miscarriage was defined as a clinical pregnancy that showed no fetal heartbeat, or the loss of the fetal heartbeat, before 12 weeks of gestation.
5. Statistical analysis
Results were expressed as mean±standard deviation. Statistical analysis was performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). One-way analysis of variance, the Kruskal-Wallis rank test, or Fisher's exact test was performed to analyze the whether the differences between groups were significant. The p-values less than 0.05 were considered to indicate a statistically significant difference.
Results
1. Retrieved oocytes and maturation rates in the study groups
The average age of the female partner (p=0.904) and basal follicle-stimulating hormone levels (p=0.165) were not significantly different among the study groups (Table 1). Infertility factors were not significantly different (p=0.374), using the classification of infertility as female-factor, male-factor, combined-factor, and unexplained-factor infertility. However, the numbers of retrieved oocytes were significantly different among the study groups (p<0.001). On average, significantly more oocytes were retrieved from groups IV (2.6±0.5) and V (2.5±0.5) than from groups I (1.9±0.8), II (1.3±0.6), and III (1.3±0.6). Moreover, on average, significantly more oocytes were retrieved from group I than from groups II and III. At the time of cumulus cell removal, the numbers of mature oocytes were significantly different between the groups (p<0.001). The average maturation rate of the oocytes retrieved from group I (1.7±0.7, 91.4%±18.2%) was significantly higher than the maturation rates of the oocytes retrieved from groups II (0, 0%), III (0, 0%), IV (1.3±0.5, 52.2%±13.2%), and V (1.2±0.4, 49.6%±11.3%). The numbers of injected oocytes were also significantly different among the study groups (p<0.001). The average numbers of injected oocytes in groups IV (2.4±0.5) and V (2.3±0.5) were significantly higher than those in groups I (1.7±0.7), II (1.1±0.4), and III (1.2±0.4). Moreover, the average number of injected oocytes in group I was significantly higher than in groups II and III. However, the maturation rates of each group were not significantly different at the time of ICSI (p=0.07) (Table 1).
Table 1. Numbers of retrieved oocytes and their maturation rates by group.
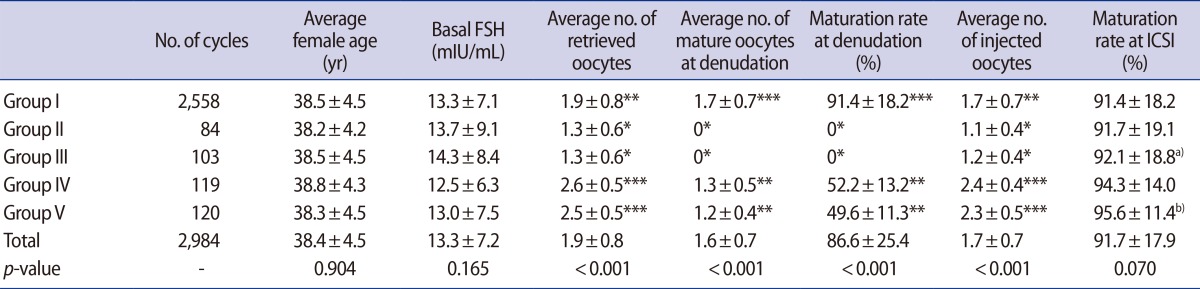
Values are presented as number or mean±standard deviation.
FSH, follicle-stimulating hormone; ICSI, intracytoplasmic sperm injection.
a)Rate of mature oocytes on the day after oocyte retrieval divided by the number of total retrieved oocytes; b)Rate the number of mature oocytes on the day of oocyte retrieval and the day after oocyte retrieval divided by the total number of retrieved oocytes; Superscript letters (*, **, ***) within the same column designate significant differences.
2. Fertilization rates and numbers of transferred embryos
The fertilization rate was calculated by dividing the number of oocytes with two pronuclei and a second polar body by the total number of injected oocytes. The fertilization rate of group II (49.0%±49.1%) was significantly lower than the rates of the other groups (p<0.001), whereas the fertilization rates of groups I, III, IV, and V were not significantly different (Table 2). Moreover, the numbers of transferred embryos were significantly smaller in groups II (1.1±0.4) and III (1.1±0.6) than in groups I (1.5±0.7), IV (1.6±0.8), and V (1.5±0.7) (p<0.001) (Table 2).
Table 2. Fertilization rates, numbers of transferred embryos, and clinical pregnancy rates by group.
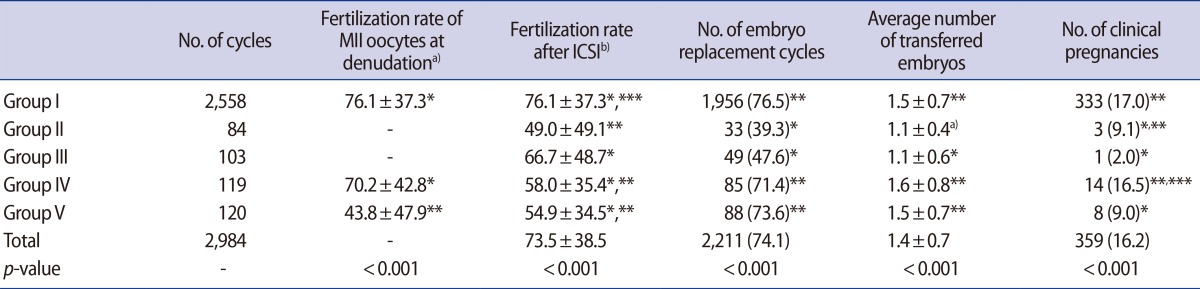
Values are presented as number (%) or mean±standard deviation.
MII, mature metaphase II; ICSI, intracytoplasmic sperm injection.
a)The fertilization rate of oocytes that were mature when cumulus cells were removed; b)The fertilization rate of all injected oocytes (oocytes that matured on the day of oocyte retrieval or the day after oocyte retrieval); Superscript letters (*, **, ***) within the same column designate significant differences.
The rates of cycle cancellation were significantly higher in groups II and III (60.7% and 52.4%, respectively) than in groups I, IV, and V (23.5%, 28.6%, and 26.4%, respectively; p<0.001) (Table 3). In some cases, embryos were frozen because the total number of embryos was small. However, the rate of cycle cancellation due to cryopreservation did not differ among the study groups. The rate of cycle cancellation due to fertilization failure (62.7%) was significantly higher in group II than in all other groups (p<0.05) (Table 3). The rate of cycle cancellation due to developmental arrest of the embryo was significantly higher (18.5%) in group III than in the other groups (p<0.01).
Table 3. Causes of cycle cancellation by group.
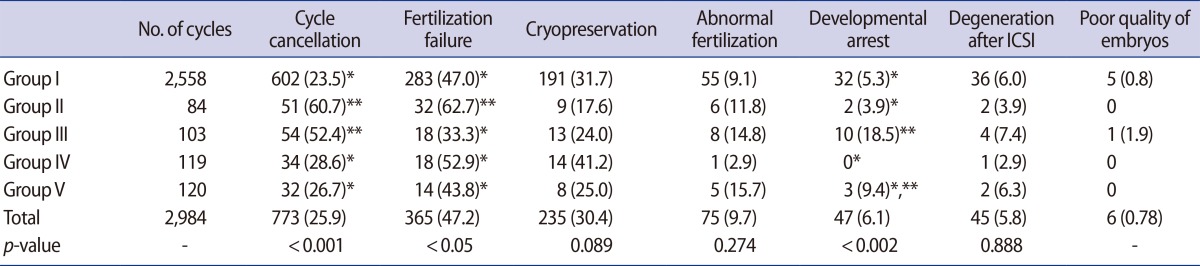
Values are presented as number (%).
Superscript letters (*, **) within the same column designate significant differences.
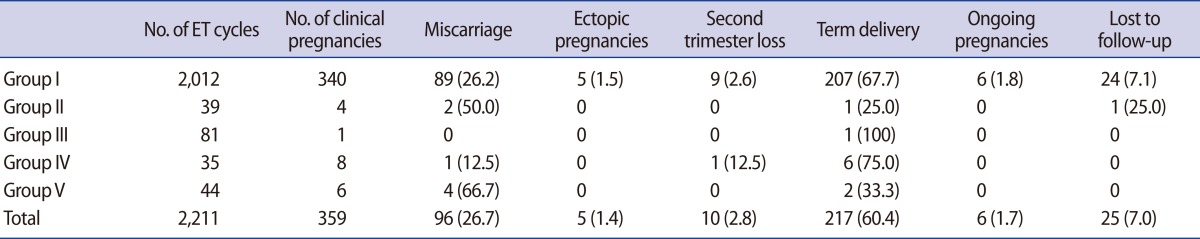
3. Pregnancy outcomes
On average, 1.5±0.7 embryos were transferred in each of the 2,211 cycles ultimately analyzed in this study. A total of 359 clinical pregnancies were established (16.2%). These clinical pregnancies resulted in 96 miscarriages, five ectopic pregnancies, 10 second trimester losses, and 217 deliveries. Six pregnancies were ongoing at the time of the data analysis, and 25 pregnancies were lost to follow up. Of the 217 deliveries, 20 were twin pregnancies and 197 were singleton pregnancies. Of the babies, 118 were female, and 115 were male, and the sex of the remaining four babies could not be ascertained.
The clinical pregnancy rates were significantly different among the study groups (p<0.001). The clinical pregnancy rate was significantly higher in group I than in all other groups, and the clinical pregnancy rate was significantly lower in group III than in other groups (Table 2). Clinical pregnancy rates were also reanalyzed according to the origin of the transferred embryos, since only embryos originating from mature or immature oocytes were transferred for some patients in groups IV and V, whereas both types of embryos were transferred simultaneously in other patients. The average age of the female partner was still not significantly different between the groups (p=0.214) when the groups were reclassified according to the origin of the transferred embryos (Table 4). However, the average numbers of transferred embryos were significantly different between the groups (p<0.001). For instance, the average numbers of transferred embryos in groups IV (2.3±0.5) and V (2.1±0.4) were significantly higher than those in groups I (1.5±0.7), II (1.1±0.4), and III (1.2±0.4). Similarly, the quality of the embryos was significantly different between the groups (p<0.001). The embryo quality in groups I and IV (rates of good embryos in transferred embryos, 25.0%±39.4% and 21.4%±23.1%, respectively) was significantly better (p<0.001) than in groups II, III, and V (5.1%±22.3%, 4.3%±19.7%, and 8.3%±18.2%, respectively). However, the average clinical pregnancy rate was significantly lower in group III than in other groups (p<0.005). In group I, 340 clinical pregnancies were established. Of these pregnancies, 96 aborted spontaneously within the first trimester, nine were lost within the second trimester, and 217 pregnancies resulted in the delivery of 227 babies. Of the remaining pregnancies, six were ongoing at the time of the study, five were ectopic, and 24 were lost to follow up. Of the 227 babies who were delivered, 116 were female, 107 were male, and the sex of the remaining four were not ascertained. In group II, one female baby was delivered, two pregnancies were aborted spontaneously within the first trimester, and one pregnancy was lost to follow up. One male baby was delivered in group III, whereas six male babies were delivered in group IV. In group IV, one pregnancy was aborted spontaneously within the first trimester and one was lost within the second trimester. One male and one female baby were delivered in group V, whereas four pregnancies aborted spontaneously within the first trimester (Table 5).
Table 4. Clinical pregnancy rates by group according to the origin of transferred embryos.
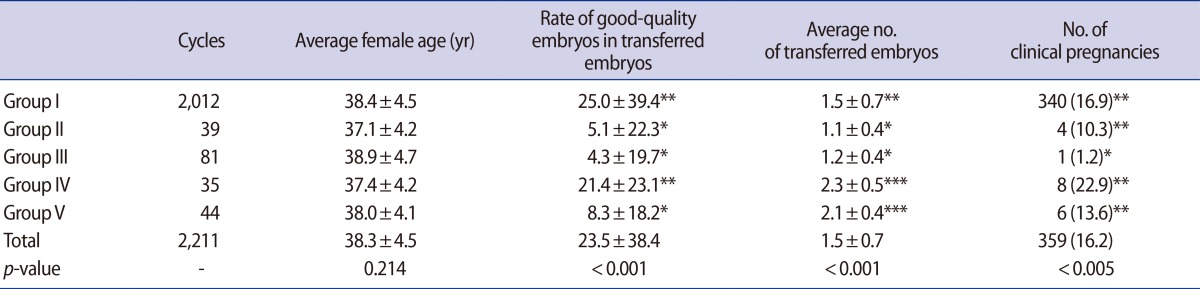
Values are presented as number (%) or mean±standard deviation.
Superscript letters (*, **, ***) within the same column designate significant differences.
Table 5. Delivery outcomes by group.
Values are presented as number (%).
ET, embryo transfer.
Discussion
In this study, we analyzed the fertilization rates of immature oocytes retrieved in ICSI cycles. The analysis of groups II and III provided information about the fertilization rates and pregnancy potential of immature oocytes that spontaneously underwent IVM, without confounding by the concurrent transfer of embryos originating from immature oocytes along with embryos originating from mature oocytes. The analysis of groups IV and V shed light on whether performing ICSI on in vitro-matured oocytes, thereby increasing the number of injectable oocytes, could improve pregnancy outcomes, because in groups IV and V, embryos originating from immature oocytes were transferred along with embryos originating from mature oocytes.
The fertilization rate decreased when all (groups II and III) or some (groups IV and V) of the retrieved oocytes were immature. The fertilization rate also decreased when ICSI was performed on some of the immature oocytes after spontaneous IVM on the day of oocyte retrieval (groups II and IV), or on the day after oocyte retrieval (groups III and V), compared with when ICSI was performed only on mature oocytes on the day of oocyte retrieval (group I). Several studies have reported decreased fertilization rates when ICSI was performed on immature oocytes after spontaneous maturation [5,14,17,20,21]. The cytoplasmic immaturity of in vitro-matured oocytes has been suggested as one possible explanation for this decreased fertilization rate [22,23,24]. Immature oocytes undergo nuclear maturation shortly after oocyte retrieval in current culture systems, although immature oocytes are not cultured in IVM medium. However, current culture systems seem to be insufficient for producing developmentally competent oocytes [6,23,24]. In this study, IVM medium was not used. Therefore, the cytoplasmic maturation of in vitro-matured oocytes in this study may have been inferior to that of in vitro-matured oocytes that were cultured in IVM medium in other studies. Another possible cause for the decreased fertilization rate could have been that one or more components necessary for cytoplasmic maturation were deficient in the in vitro-matured oocytes. Several metaphase deficiencies were observed in the in vitro-matured oocytes; it has been shown that these deficiencies indicate that the oocytes failed to mature in vivo under standard ovarian stimulation conditions [11].
The numbers of injectable oocytes and transferrable embryos decreased significantly when all of the retrieved oocytes were immature (groups II and III). Moreover, the rates of cycle cancellation because embryos could not be transferred were significantly higher in groups II and III, and the pregnancy rates were lower. The numbers of injectable oocytes were significantly increased when some of the retrieved oocytes were immature and ICSI was performed on some of these immature oocytes after their spontaneous IVM (groups IV and V). Moreover, the number of transferrable embryos was increased by performing ICSI on both in vitro-matured and in vivo-matured oocytes, yielding more embryos than were obtained when only in vivo matured-oocytes were used (group I). The rates of cycle cancellation of groups IV and V were also similar to that of group I. However, the pregnancy rates were not improved, even though the numbers of injectable oocytes and transferrable embryos were higher in groups IV and V. The pregnancy rates were also reanalyzed according to the origins of the transferred embryos. In groups IV and V, only embryos originating from mature oocytes were transferred when immature oocytes were unfertilized, whereas only embryos originating from immature oocytes were transferred when mature oocytes were unfertilized. When the data were reanalyzed according to the origin of the transferred embryos, the numbers of transferred embryos were higher in cycles in which embryos originating from both immature and mature oocytes were transferred. Moreover, the clinical pregnancy rates of cycles in which only embryos originating from immature oocytes were transferred (groups II and III) were lower than those in cycles in which only embryos originating from mature oocytes were transferred (group I). However, the clinical pregnancy rates of cycles in which embryos originating from both immature and mature oocytes were transferred (groups IV and V) were comparable to those of cycles in which only embryos originating from mature oocytes were transferred (group I). These results indicate that in groups IV and V, most pregnancies were achieved from embryos originating from mature oocytes, not from embryos originating from immature oocytes. Moreover, the pregnancy rates of groups III and V were lower than those of the other groups; these low pregnancy rates were likely a consequence of the poor quality of the embryos that were transferred in these groups. In group III, ICSI was performed on in vitro-matured oocytes since only immature oocytes were retrieved. However, in group V, ICSI was performed on in vitro-matured oocytes to avoid cycle cancellation due to the fertilization failure of mature oocytes, or to increase the number of transferrable embryos even if the retrieved mature oocytes were fertilized. The fertilization rate of mature oocytes in group IV (70.2%±42.8%) was comparable to that of group I (76.1%±37.3%), but the fertilization rate of mature oocytes in group V was significantly lower than that of group I (43.8%±47.9%, p<0.001). Since the mature oocytes exhibited a low fertilization rate, and the transferred embryos were generally of poor quality, the cytoplasmic maturation of the mature oocytes in group V appeared to be inadequate. Since oocyte maturation occurs relatively quickly in vitro [11,20], and the cumulus cells were removed a few hours after oocyte retrieval, some of the mature oocytes might have been immature at the time of oocyte retrieval and therefore may have undergone nuclear maturation between oocyte retrieval and the removal of cumulus cells. Several studies have investigated why embryos originating from 1-day-old oocytes result in low pregnancy rates. Asynchrony between embryo development and the endometrium [25], as well as embryonic chromosomal abnormalities [26], have been suggested to be possible causes for the low pregnancy rates obtained with embryos derived from 1-day-old oocytes. Moreover, the pregnancy rates obtained from embryos originating from 1-day-old oocytes have been shown to vary according to the particular fertility clinic [25,27,28]. Therefore, more research is clearly needed to increase the pregnancy rate from embryos originating from 1-day-old oocytes. Studies on optimal culture conditions could prove particularly insightful in this regard.
In conclusion, this study found that immature oocytes can be fertilized using ICSI after IVM. However, the fertilization rate of these immature oocytes and the quality of the embryos originating from these immature oocytes were significantly lower than the corresponding parameters in embryos that originated from mature oocytes. Moreover, pregnancy rates were not improved, even though the numbers of injectable oocytes and transferrable embryos can be increased by performing ICSI on immature oocytes after their IVM. Moderate pregnancy rates could be achieved by replacing only embryos derived from mature oocytes. Therefore, performing ICSI on immature oocytes after their IVM is likely unnecessary if mature oocytes are retrieved and if embryo replacement is possible using embryos derived from these mature oocytes. Thus, the clinical use of immature oocytes should only be deliberately considered when only immature oocytes are retrieved. The replacement of embryos derived from immature oocytes could be carried out in the same way as for embryos derived from mature oocytes if the retrieved immature oocytes then mature on the day of oocyte retrieval; however, we found that the pregnancy rate in this scenario was still lower than that of embryos derived from mature oocytes. If a fertility clinic intends to use immature oocytes clinically, the timing of ICSI should be determined with care, since extended culture periods after polar body extrusion might lead to aging of the oocytes. The optimal time for ICSI can be determined without frequent microscopic observation if recently developed technology, such as a time-lapse system, is used. The cryopreservation of embryos derived from immature oocytes might be desirable in cases where the retrieved immature oocytes mature on the day after oocyte retrieval and ICSI are performed, because asynchrony between embryo development and the endometrium are thought to reduce the chance of successful pregnancy. If the range of problems mentioned above, such as the timing of ICSI and asynchrony between embryo development and the endometrium, are solved, IVM of immature oocytes may be a valuable method in patients from whom a low number of oocytes are retrieved or when only immature oocytes are retrieved unexpectedly.
In order to ensure successful pregnancies, ovarian stimulation should first be performed, so that a large number of mature oocytes are retrieved. Ovarian stimulation is particularly important for patients from whom only a small number of oocytes are expected to be retrieved, such as patients with old age, poor response, premature ovarian failure, and similar conditions; moreover, stimulation should be performed extremely carefully in such cases.
Acknowledgments
We thank the medical and laboratory staff at the Center for Reproductive Medicine and Infertility, Cheil General Hospital.
Footnotes
Conflict of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Nagy ZP, Cecile J, Liu J, Loccufier A, Devroey P, Van Steirteghem A. Pregnancy and birth after intracytoplasmic sperm injection of in vitro matured germinal-vesicle stage oocytes: case report. Fertil Steril. 1996;65:1047–1050. doi: 10.1016/s0015-0282(16)58285-5. [DOI] [PubMed] [Google Scholar]
- 2.Edirisinghe WR, Junk SM, Matson PL, Yovich JL. Birth from cryopreserved embryos following in-vitro maturation of oocytes and intracytoplasmic sperm injection. Hum Reprod. 1997;12:1056–1058. doi: 10.1093/humrep/12.5.1056. [DOI] [PubMed] [Google Scholar]
- 3.Liu J, Lu G, Qian Y, Mao Y, Ding W. Pregnancies and births achieved from in vitro matured oocytes retrieved from poor responders undergoing stimulation in in vitro fertilization cycles. Fertil Steril. 2003;80:447–449. doi: 10.1016/s0015-0282(03)00665-4. [DOI] [PubMed] [Google Scholar]
- 4.Shu Y, Gebhardt J, Watt J, Lyon J, Dasig D, Behr B. Fertilization, embryo development, and clinical outcome of immature oocytes from stimulated intracytoplasmic sperm injection cycles. Fertil Steril. 2007;87:1022–1027. doi: 10.1016/j.fertnstert.2006.08.110. [DOI] [PubMed] [Google Scholar]
- 5.Alvarez C, Garcia-Garrido C, Taronger R, Gonzalez de Merlo G. In vitro maturation, fertilization, embryo development & clinical outcome of human metaphase-I oocytes retrieved from stimulated intracytoplasmic sperm injection cycles. Indian J Med Res. 2013;137:331–338. [PMC free article] [PubMed] [Google Scholar]
- 6.Cha KY, Chian RC. Maturation in vitro of immature human oocytes for clinical use. Hum Reprod Update. 1998;4:103–120. doi: 10.1093/humupd/4.2.103. [DOI] [PubMed] [Google Scholar]
- 7.Smitz J, Nogueira D, Vanhoutte L, de Matos DG, Cortvrindt R. Oocyte in vitro maturation. In: Gardner DK, Weissman A, Howles CM, Shoham Z, editors. extbook of assisted reproductive techniques: laboratory and clinical perspectives. 2nd ed. London: Taylor & Francis; 2004. pp. 125–161. [Google Scholar]
- 8.Stouffer RL, Zelinski-Wooten MB. Overriding follicle selection in controlled ovarian stimulation protocols: quality vs quantity. Reprod Biol Endocrinol. 2004;2:32. doi: 10.1186/1477-7827-2-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ectors FJ, Vanderzwalmen P, Van Hoeck J, Nijs M, Verhaegen G, Delvigne A, et al. Relationship of human follicular diameter with oocyte fertilization and development after in-vitro fertilization or intracytoplasmic sperm injection. Hum Reprod. 1997;12:2002–2005. doi: 10.1093/humrep/12.9.2002. [DOI] [PubMed] [Google Scholar]
- 10.Triwitayakorn A, Suwajanakorn S, Pruksananonda K, Sereepapong W, Ahnonkitpanit V. Correlation between human follicular diameter and oocyte outcomes in an ICSI program. J Assist Reprod Genet. 2003;20:143–147. doi: 10.1023/A:1022977002954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Combelles CM, Cekleniak NA, Racowsky C, Albertini DF. Assessment of nuclear and cytoplasmic maturation in in-vitro matured human oocytes. Hum Reprod. 2002;17:1006–1016. doi: 10.1093/humrep/17.4.1006. [DOI] [PubMed] [Google Scholar]
- 12.Lanzendorf SE, Zelinski-Wooten MB, Stouffer RL, Wolf DP. Maturity at collection and the developmental potential of rhesus monkey oocytes. Biol Reprod. 1990;42:703–711. doi: 10.1095/biolreprod42.4.703. [DOI] [PubMed] [Google Scholar]
- 13.Meng L, Wolf DP. Sperm-induced oocyte activation in the rhesus monkey: nuclear and cytoplasmic changes following intracytoplasmic sperm injection. Hum Reprod. 1997;12:1062–1068. doi: 10.1093/humrep/12.5.1062. [DOI] [PubMed] [Google Scholar]
- 14.De Vos A, Van de Velde H, Joris H, Van Steirteghem A. In-vitro matured metaphase-I oocytes have a lower fertilization rate but similar embryo quality as mature metaphase-II oocytes after intracytoplasmic sperm injection. Hum Reprod. 1999;14:1859–1863. doi: 10.1093/humrep/14.7.1859. [DOI] [PubMed] [Google Scholar]
- 15.Huang FJ, Chang SY, Tsai MY, Lin YC, Kung FT, Wu JF, et al. Relationship of the human cumulus-free oocyte maturational profile with in vitro outcome parameters after intracytoplasmic sperm injection. J Assist Reprod Genet. 1999;16:483–487. doi: 10.1023/A:1020551000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen SU, Chen HF, Lien YR, Ho HN, Chang HC, Yang YS. Schedule to inject in vitro matured oocytes may increase pregnancy after intracytoplasmic sperm injection. Arch Androl. 2000;44:197–205. doi: 10.1080/014850100262173. [DOI] [PubMed] [Google Scholar]
- 17.Kim BK, Lee SC, Kim KJ, Han CH, Kim JH. In vitro maturation, fertilization, and development of human germinal vesicle oocytes collected from stimulated cycles. Fertil Steril. 2000;74:1153–1158. doi: 10.1016/s0015-0282(00)01617-4. [DOI] [PubMed] [Google Scholar]
- 18.Bonu MA, Papaioannidou PG, Garetti S, Sciajno R, Serrao L, Preti S, et al. P-195 Twin pregnancy after in-vitro maturation of oocytes: case report. Hum Reprod. 2001;16(suppl 1):176–177. [Google Scholar]
- 19.Balakier H, Sojecki A, Motamedi G, Librach C. Time-dependent capability of human oocytes for activation and pronuclear formation during metaphase II arrest. Hum Reprod. 2004;19:982–987. doi: 10.1093/humrep/deh158. [DOI] [PubMed] [Google Scholar]
- 20.Strassburger D, Friedler S, Raziel A, Kasterstein E, Schachter M, Ron-El R. The outcome of ICSI of immature MI oocytes and rescued in vitro matured MII oocytes. Hum Reprod. 2004;19:1587–1590. doi: 10.1093/humrep/deh236. [DOI] [PubMed] [Google Scholar]
- 21.Vanhoutte L, De Sutter P, Van der Elst J, Dhont M. Clinical benefit of metaphase I oocytes. Reprod Biol Endocrinol. 2005;3:71. doi: 10.1186/1477-7827-3-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goud PT, Goud AP, Qian C, Laverge H, Van der Elst J, De Sutter P, et al. In-vitro maturation of human germinal vesicle stage oocytes: role of cumulus cells and epidermal growth factor in the culture medium. Hum Reprod. 1998;13:1638–1644. doi: 10.1093/humrep/13.6.1638. [DOI] [PubMed] [Google Scholar]
- 23.Russell JB. Immature oocyte retrieval with in-vitro oocyte maturation. Curr Opin Obstet Gynecol. 1999;11:289–296. doi: 10.1097/00001703-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 24.Trounson A, Anderiesz C, Jones G. Maturation of human oocytes in vitro and their developmental competence. Reproduction. 2001;121:51–75. doi: 10.1530/rep.0.1210051. [DOI] [PubMed] [Google Scholar]
- 25.Ming L, Liu P, Qiao J, Lian Y, Zheng X, Ren X, et al. Synchronization between embryo development and endometrium is a contributing factor for rescue ICSI outcome. Reprod Biomed Online. 2012;24:527–531. doi: 10.1016/j.rbmo.2012.02.001. [DOI] [PubMed] [Google Scholar]
- 26.Pehlivan T, Rubio C, Ruiz A, Navarro J, Remohi J, Pellicer A, et al. Embryonic chromosomal abnormalities obtained after rescue intracytoplasmic sperm injection of 1-day-old unfertilized oocytes. J Assist Reprod Genet. 2004;21:55–57. doi: 10.1023/B:JARG.0000025939.26834.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lundin K, Sjogren A, Hamberger L. Reinsemination of one-day-old oocytes by use of intracytoplasmic sperm injection. Fertil Steril. 1996;66:118–121. [PubMed] [Google Scholar]
- 28.Morton PC, Yoder CS, Tucker MJ, Wright G, Brockman WD, Kort HI. Reinsemination by intracytoplasmic sperm injection of 1-day-old oocytes after complete conventional fertilization failure. Fertil Steril. 1997;68:488–491. doi: 10.1016/s0015-0282(97)00223-9. [DOI] [PubMed] [Google Scholar]


