Abstract
This study estimates the percentage of health care expenditures in the non-institutionalized United States (U.S.) adult population associated with levels of physical activity inadequate to meet current guidelines. Leisure-time physical activity data from the National Health Interview Survey (2004–2010) were merged with health care expenditure data from the Medical Expenditure Panel Survey (2006–2011). Health care expenditures for inactive (i.e., no physical activity) and insufficiently active adults (i.e., some physical activity but not enough to meet guidelines) were compared with active adults (i.e., ≥150 minutes/week moderate-intensity equivalent activity) using an econometric model. Overall, 11.1% (95% CI: 7.3, 14.9) of aggregate health care expenditures were associated with inadequate physical activity (i.e., inactive and insufficiently active levels). When adults with any reported difficulty walking due to a health problem were excluded, 8.7% (95% CI: 5.2, 12.3) of aggregate health care expenditures were associated with inadequate physical activity. Increasing adults' physical activity to meet guidelines may reduce U.S. health care expenditures.
Keywords: Physical activity, Exercise, Health expenditures, Health care
Regular physical activity is associated with important health benefits, including reduced risk for premature death, cardiovascular disease, ischemic stroke, type 2 diabetes, colon and breast cancers, and depression.1 Current national guidelines for aerobic physical activity recommend for substantial health benefits, adults should participate weekly in at least 150 minutes of moderate-intensity aerobic activity, at least 75 minutes of vigorous-intensity aerobic activity, or an equivalent combination.2 Despite the health benefits, fewer than half of United States (U.S.) adults met the minimal guidelines for aerobic activity and almost one-third of adults were physically inactive in 2011.3
Population levels of physical activity inadequate to meet current guidelines can place a health burden on the U.S. population that results in higher health care expenditures. Many studies quantify this burden by estimating the percentage of health care costs associated with physical inactivity using a population-attributable fraction approach.4–9 This approach combines risk, prevalence, and aggregate cost estimates from unlinked sources.4–9 Costs calculated from unlinked sources can be biased if the characteristics of the source populations differ or if measures of physical inactivity differ across sources.
Studies using individual physical activity data linked to health care expenditure data overcome many of the limitations associated with estimates calculated using a population-attributable fraction approach.10–18 Studies using linked data show that an individual's physical activity level is associated with health care expenditures, but these studies have limitations, such as selected study populations,11–17 lack of adequate control for confounding characteristics,10,13,18 and measures of physical activity that do not match current guidelines.10–12,14–18 In addition, while these studies compare estimates of per person costs associated with different levels of physical activity, they do not provide estimates of the population level burden associated with inadequate physical activity. To our knowledge, no study uses linked individual data to estimate the percentage of health care expenditures associated with inadequate levels of aerobic physical activity defined using current guidelines criteria.
Studies have consistently shown that obese persons have higher health care expenditures than normal weight persons.11,13,19–21 One pathway by which physical activity may influence health care expenditures is through its role in weight management.1 Given this potential pathway, adjusting estimates of the association between physical activity and health care expenditures for an individual's obesity status may be overly conservative. Therefore, it is important to examine estimates of the percentage of health care expenditures associated with inadequate levels of physical activity with and without adjustment for obesity status.
Using linked individual data, this study examines the association of leisure-time aerobic physical activity (defined using current guidelines) and health care expenditures in a nationally representative sample of non-institutionalized U.S. adults with and without adjusting for obesity status. These results are then applied to estimate the percentage of overall health care expenditures associated with levels of physical activity inadequate to meet current guidelines.
Methods
Data
Data from the National Health Interview Survey (NHIS) (2004–2010) and the Medical Expenditure Panel Survey (MEPS) (2006–2011) were merged at the individual level. The NHIS is a multistage probability sample survey of U.S. households conducted annually. Data on physical activity are collected during the sample adult interview. The MEPS uses the same sampling frame as the NHIS. Respondents from the previous 2 years of NHIS are included in each MEPS year. MEPS response rates for study years range from 53.5% (2010) to 59.3% (2008). Additional information about the design of the NHIS and the MEPS are described elsewhere.22,23
There were 57 987 MEPS records for adults age 21 years or older with a linkable NHIS sample adult record. Adults missing data on covariates or physical activity were excluded (n = 3627). Adults who were pregnant during the MEPS year or at the NHIS interview (2141) or who reported being unable to do physical activity (1054) were excluded from all analyses.
Measures
Physical activity level
In the NHIS, adults were asked how often and, if applicable, the duration during leisure-time they participated for at least 10 minutes at a time, in 1) vigorous-intensity activities (i.e., heavy sweating or large increases in breathing or heart rate) and 2) light- or moderate-intensity activities (i.e., light sweating or slight to moderate increases in breathing or heart rate). To classify adults into levels of physical activity, minutes of moderate-intensity equivalent activity were calculated by counting 1 minute of vigorous-intensity activity as 2 minutes of light- or moderate-intensity activity.2 Respondents were then classified into three activity levels using current guidelines: 1) active, reporting at least 150 minutes/week of moderate-intensity equivalent physical activity; 2) insufficiently active, reporting some moderate-intensity equivalent physical activity but not enough to meet active definition; 3) inactive, reporting no moderate-intensity equivalent physical activity that lasted at least 10 minutes.2
Health care expenditures
A continuous variable of yearly total direct health care expenditures was calculated (includes expenditures for all services: inpatient, outpatient, emergency room, office-based, dental, vision, home health, prescription drug, and other). The Personal Health Care Expenditure Price Index was used to adjust all expenditures to 2012 dollars.24
Covariates
Covariate data from the MEPS dataset included: sex, age (in years: 21–29, 30–39, 40–49, 50–59, 60–69, 70–79, and 80 and older), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic other), marital status (married, widowed, divorced/separated, never married), census region (Northeast, Midwest, South, West), metropolitan statistical area (MSA, non-MSA), poverty level (household income as a percentage of federal poverty level: less than 100%, 100–199%, 200–399%, 400% or more), health insurance status (coverage for the year: any private coverage, Medicare and Medicaid, Medicare only, Medicaid only, uninsured), and MEPS year. Covariate data from the NHIS dataset included: education level (less than high school graduate, high school graduate, some college, college graduate), smoking status (current, former, never), and body mass index (BMI) category. BMI was calculated using self-reported weight and height and was categorized as underweight (<18.5 kg/m2), normal weight (18.5–25 kg/m2), overweight (25–<30 kg/m2), and obese (≥30 kg/m2).25
Statistical analysis
To capture the skewed nature of health care expenditure data, a four-part econometric model was used.20,26 In this four-part model, two probit models predicted the probability of having a positive health care expenditure and, among those with a positive health care expenditure, having a positive in-patient expenditure. Two generalized linear models with a log link and gamma distribution predicted total health care expenditures separately for adults with a positive health care expenditure but no in-patient expenditure and for adults with a positive in-patient expenditure. Modified Park's tests were used to determine the appropriate distribution specification for the generalized linear models.27,28 Predictions from each part of the four-part model were combined to generate predicted health care expenditures for each individual.
Inactive adults were compared to active adults by calculating the mean and percent difference in health care expenditures. To calculate the mean difference in health care expenditures for inactive adults compared to being active, the mean of predicted health care expenditures for inactive adults with the inactive variable set to 0 (i.e., “as if” the individual was active) was subtracted from the mean of predicted health care expenditures for inactive adults with the inactive variable set to 1 (i.e., “as is”).21,29 The percent difference was estimated by dividing the mean difference between health care expenditures for inactive adults compared to active adults by the mean predicted health care expenditure for inactive adults “as if” the individual was active.21 The percentage of aggregate health care expenditures associated with inactivity was calculated by dividing the sum of differences in health care expenditures for inactive adults compared to being active by the total predicted expenditures for all adults.21 This process was repeated for insufficiently active adults.
Two models were estimated to derive the above measures. Model 1 included physical activity level and covariates (i.e., sex, age group, race/ethnicity, census region, metropolitan statistical area status, marital status, education, poverty level, health insurance status, smoking status, and MEPS year). Model 2 included the same covariates and added BMI category.
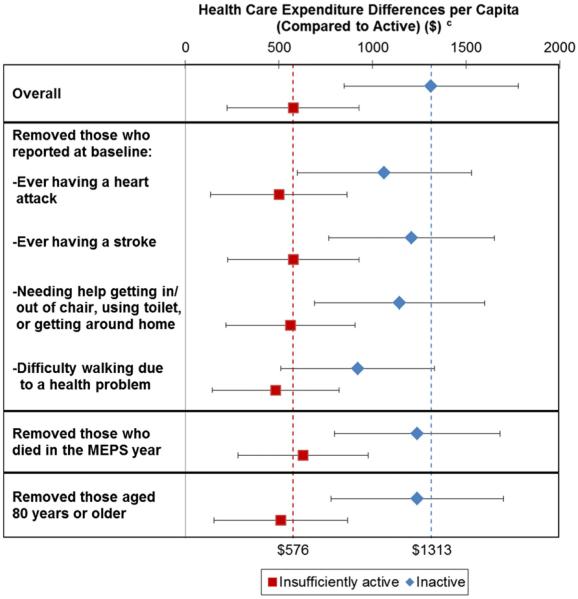
Though adults who reported being unable to do physical activity were excluded, to address the concern that inactive or insufficiently active adults might have health problems preventing them from participating in physical activity and increase their expenditures, multiple sensitivity analyses were conducted. Sensitivity analyses excluded subgroups such as adults who reported at the time of the NHIS interview (i.e., baseline) ever having had a heart attack; ever having had a stroke; needing help getting in/out of bed or chairs, using the toilet, or getting around the home; or having difficulty walking because of a health problem. In addition, adults who died during the MEPS year or who were greater than or equal to 80 years of age were excluded.
Statistical weights and balanced repeated replications methods were applied to produce estimates representative of the civilian, non-institutionalized U.S. population and to account for the complex sample design. In the NHIS, only one sampled adult per household is asked questions about physical activity and MEPS person-year weights were adjusted to account for this sampling.30 A raking procedure was used to adjust statistical weights for adults with complete NHIS and MEPS data to match population totals from the full MEPS sample (SAS, version 9.3).31 Stata, version 13.0, was used for the statistical analyses.
Results
The analytic sample included 51165 adults age 21 years or older and excluded those who were pregnant or who reported being unable to do physical activity. From 2006–2011, the average total annual health care expenditures per year was $1.05 trillion for this sample weighted to the U.S. population. The majority of the sample was white non-Hispanic, married, had some college education or was a college graduate, and had some private insurance coverage for the year (Table 1).
Table 1.
Distribution of select characteristics and prevalence of physical activity level by select characteristics - US adults, NHIS and MEPS 2006–2011a.
| Overall |
Prevalence of Physical Activity Levelb |
|||||||
|---|---|---|---|---|---|---|---|---|
| Sample size (%)c | Inactive |
Insufficiently Active |
Active |
|||||
| (N = 19 959) |
(N = 10 264) |
(N = 20 942) |
||||||
| Characteristic | % | (SE) | % | (SE) | % | (SE) | ||
| Overall | 51 165 | 34.2 | (0.6) | 20.2 | (0.4) | 45.5 | (0.5) | |
| Sex | ||||||||
| Male | 23 170 | (50.2) | 32.8 | (0.8) | 18.5 | (0.5) | 48.6 | (0.6) |
| Female | 27 995 | (49.8) | 35.6 | (0.7) | 22.0 | (0.5) | 42.4 | (0.6) |
| Age (years) | ||||||||
| 21–29 | 6741 | (16.2) | 27.6 | (1.1) | 17.5 | (1.0) | 54.9 | (1.3) |
| 30–39 | 9493 | (17.4) | 29.3 | (0.9) | 19.6 | (0.6) | 51.2 | (1.0) |
| 40–49 | 10 173 | (20.2) | 32.8 | (0.9) | 20.5 | (0.8) | 46.7 | (0.9) |
| 50–59 | 9650 | (19.7) | 34.2 | (1.0) | 21.3 | (0.7) | 44.4 | (0.9) |
| 60–69 | 7119 | (13.5) | 37.1 | (1.3) | 22.1 | (0.9) | 40.7 | (1.1) |
| 70–79 | 4691 | (7.8) | 42.8 | (1.4) | 20.8 | (1.0) | 36.4 | (1.3) |
| ≥80 | 3298 | (5.2) | 56.4 | (1.6) | 20.3 | (1.2) | 23.4 | (1.3) |
| Race/ethnicity | ||||||||
| White, non-Hispanic | 27 992 | (69.0) | 30.2 | (0.8) | 20.7 | (0.5) | 49.1 | (0.6) |
| Black, non-Hispanic | 9749 | (11.1) | 43.6 | (1.1) | 19.4 | (0.7) | 36.9 | (0.9) |
| Hispanic | 9638 | (13.3) | 46.6 | (1.1) | 18.4 | (0.7) | 35.0 | (1.0) |
| Other, non-Hispanic | 3786 | (6.6) | 35.2 | (1.4) | 20.5 | (1.3) | 44.2 | (1.6) |
| Education level | ||||||||
| Less than HS graduate | 10 291 | (13.9) | 56.9 | (1.2) | 18.0 | (0.8) | 25.1 | (0.9) |
| High school graduate | 13 687 | (26.6) | 44.0 | (1.1) | 19.8 | (0.6) | 36.2 | (0.9) |
| Some college | 14 517 | (29.9) | 29.3 | (0.8) | 21.9 | (0.6) | 48.8 | (0.8) |
| College graduate | 12 670 | (29.6) | 19.7 | (0.7) | 20.1 | (0.6) | 60.2 | (0.8) |
| Marital status | ||||||||
| Married | 23 435 | (56.2) | 32.5 | (0.8) | 21.2 | (0.5) | 46.2 | (0.6) |
| Widowed | 5255 | (7.0) | 52.6 | (1.4) | 21.1 | (1.1) | 26.4 | (1.2) |
| Divorced/separated | 10 431 | (14.6) | 37.6 | (0.9) | 19.8 | (0.8) | 42.6 | (0.9) |
| Never married | 12 044 | (22.2) | 30.6 | (0.9) | 17.8 | (0.6) | 51.7 | (1.0) |
| Census region | ||||||||
| Northeast | 7819 | (18.6) | 35.0 | (1.3) | 20.7 | (0.8) | 44.3 | (1.3) |
| Midwest | 11 149 | (21.8) | 29.0 | (1.2) | 24.2 | (0.8) | 46.8 | (1.0) |
| South | 19 793 | (36.5) | 39.4 | (1.3) | 18.4 | (0.7) | 42.2 | (0.9) |
| West | 12 404 | (23.1) | 30.3 | (1.0) | 19.1 | (0.6) | 50.6 | (1.1) |
| Metropolitan statistical area (MSA) | ||||||||
| MSA | 8275 | (15.9) | 40.8 | (1.5) | 20.1 | (0.8) | 39.1 | (1.5) |
| non-MSA | 42 890 | (84.1) | 33.0 | (0.7) | 20.3 | (0.4) | 46.7 | (0.6) |
| Poverty level (income as percentage of FPL) | ||||||||
| <100% FPL | 8954 | (10.7) | 48.7 | (1.1) | 18.1 | (0.7) | 33.3 | (0.9) |
| 100%–199% FPL | 11 309 | (17.3) | 45.9 | (0.9) | 19.5 | (0.6) | 34.6 | (0.8) |
| 200%–400% FPL | 15 141 | (30.6) | 36.1 | (0.8) | 20.7 | (0.6) | 43.2 | (0.8) |
| >400% FPL | 15 761 | (41.4) | 24.2 | (0.7) | 20.8 | (0.6) | 55.0 | (0.7) |
| Health insurance status d (coverage for the year) | ||||||||
| Any private coverage | 31 334 | (69.5) | 28.4 | (0.7) | 20.9 | (0.4) | 50.7 | (0.6) |
| Medicare and Medicaid | 2734 | (2.9) | 64.7 | (1.9) | 16.2 | (1.3) | 19.1 | (1.4) |
| Medicare only | 4527 | (7.5) | 47.8 | (1.3) | 21.5 | (1.0) | 30.7 | (1.2) |
| Medicaid only | 4006 | (5.0) | 49.5 | (1.5) | 19.0 | (1.1) | 31.5 | (1.5) |
| Uninsured | 8564 | (15.2) | 43.6 | (1.2) | 17.6 | (0.8) | 38.8 | (1.1) |
| Smoking | ||||||||
| Current | 10 845 | (20.6) | 41.7 | (1.1) | 18.2 | (0.6) | 40.1 | (1.0) |
| Former | 10 990 | (22.2) | 30.8 | (0.8) | 21.6 | (0.7) | 47.6 | (0.9) |
| Never | 29 330 | (57.2) | 32.9 | (0.7) | 20.4 | (0.5) | 46.7 | (0.6) |
| BMI categorye | ||||||||
| Underweight | 757 | (1.5) | 44.7 | (2.7) | 19.4 | (2.0) | 35.9 | (2.5) |
| Normal weight | 17 295 | (35.5) | 30.9 | (0.6) | 18.0 | (0.5) | 51.1 | (0.7) |
| Overweight | 18 225 | (35.8) | 33.4 | (0.9) | 19.6 | (0.5) | 47.0 | (0.8) |
| Obese | 14 888 | (27.2) | 39.1 | (1.0) | 24.2 | (0.7) | 36.8 | (0.8) |
| MEPS year | ||||||||
| 2006 | 8835 | (16.2) | 36.8 | (1.1) | 18.7 | (0.6) | 44.5 | (0.9) |
| 2007 | 7967 | (16.5) | 35.9 | (1.0) | 19.9 | (0.7) | 44.2 | (0.9) |
| 2008 | 8080 | (16.5) | 35.7 | (1.2) | 19.6 | (0.8) | 44.7 | (1.0) |
| 2009 | 8803 | (16.7) | 35.0 | (1.1) | 19.9 | (0.7) | 45.1 | (0.9) |
| 2010 | 8245 | (16.9) | 32.0 | (1.1) | 21.4 | (0.6) | 46.6 | (0.9) |
| 2011 | 9235 | (17.2) | 30.2 | (0.9) | 21.8 | (0.6) | 47.9 | (0.8) |
Abbreviations: BMI, body mass index; FPL, federal poverty level; MEPS, Medical Expenditure Panel Survey; NHIS, National Health Interview Survey; SE, standard error; %, percentage.
Note: Percentages may not add to 100% due to rounding.
Certain adults were excluded from the analysis: 2141 (weighted: 3.6%) who were pregnant during the MEPS year or at the NHIS interview and 1054 (weighted: 1.5%) who reported being unable to do physical activity.
Physical activity level is defined as active (≥150 minutes/week moderate-intensity equivalent activity), insufficiently active (some moderate-intensity equivalent activity but not enough to meet active definition), and inactive (no moderate-intensity equivalent activity that lasted at least 10 minutes).
Estimates of % are weighted. Weighted overall population estimate is approximately 207 million adults.
Adults with Tricare are classified as having private insurance. Adults reporting other public insurance are included with the Medicaid category.
BMI category is defined as underweight (BMI <18.5 kg/m2), normal weight (BMI 18.5–<25 kg/m2), overweight (BMI 25–< 30 kg/m2), and obese (BMI ≥30 kg/m2).
Over one-third of adults were inactive, 20.2% were insufficiently active, and 45.5% were physically active (Table 1). Physical activity varied significantly (adjusted Wald P-value < 0.01) by sex, age group, race/ethnicity, education level, marital status, census region, metropolitan statistical area status, poverty level, health insurance status, smoking status, BMI category, and year observed in the MEPS. Prevalence of physical activity was higher among males, younger age groups, non-Hispanic whites, adults with higher levels of education and household income, normal weight adults, and adults who were not current smokers.
After adjusting for the main covariates, the mean annual expenditure difference per capita for inactive adults compared to active adults was $1437 (percent difference: 29.9%) and for insufficiently active compared to active adults was $713 (15.4%) (Table 2). After including BMI category as a covariate, the means of annual expenditure and percent differences for inactive adults ($1313, 26.6%) and insufficiently active adults ($576, 12.1%) versus active adults decreased slightly but the differences remained significant.
Table 2.
Expenditure Differences, Percent Differences, and Percentage of Aggregate Health Care Expenditures of Inactive and Insufficiently Active Versus Active Physical Activity Levels—US Adults, NHIS and MEPS 2006–2011a.
| Health Care Expenditure Differences Per Capita (compared to active) |
Percent Difference Per Capita (compared to active) |
Percentage of Aggregate Health Care Expenditures |
||||
|---|---|---|---|---|---|---|
| Model and Physical Activity Levelb | Mean ($)c | (95% CI) | % | (95% CI) | % | (95% CI) |
| Model 1: Physical activity and covariatesd | ||||||
| Inactive | 1437 | (985, 1889) | 29.9 | (19.3, 40.4) | 9.6 | (6.6, 12.7) |
| Insufficiently active | 713 | (361, 1064) | 15.4 | (7.4, 23.3) | 2.8 | (1.5, 4.2) |
| Inactive and insufficiently active e | e | e | e | e | 12.5 | (8.8, 16.1) |
| Model 2: Physical activity, covariatesd and BMI category | ||||||
| Inactive | 1313 | (848, 1778) | 26.6 | (16.1, 37.1) | 8.8 | (5.7, 11.9) |
| Insufficiently active | 576 | (224, 927) | 12.1 | (4.4, 19.7) | 2.3 | (0.9, 3.7) |
| Inactive and insufficiently active e | e | e | e | e | 11.1 | (7.3, 14.9) |
Abbreviations: BMI, body mass index; CI, confidence interval; MEPS, Medical Expenditure Panel Survey; NHIS, National Health Interview Survey; %, percentage.
Excludes adults who were pregnant and those who reported being unable to do physical activity.
Physical activity level is defined as active (≥150 minutes/week moderate-intensity equivalent activity), insufficiently active (some moderate-intensity equivalent activity but not enough to meet active definition), and inactive (no moderate-intensity equivalent activity that lasted at least 10 minutes).
Expenditures adjusted to 2012 dollars using the Personal Health Care Expenditure Price Index.
Covariates include sex, age group, race/ethnicity, census region, metropolitan statistical area, marital status, education, poverty level, health insurance status, smoking status, and MEPS year.
Estimates of mean differences and percent differences are based on models including inactive and insufficiently active as distinct categories therefore these estimates are not provided for the combined group. Percentages for the inactive and sufficiently active may not add to total due to rounding.
The percentage of aggregate health care expenditures associated with inadequate levels of physical activity (i.e., inactive and insufficiently active) was 12.5% and remained significant at 11.1% after adjusting for BMI (Table 2). An estimated $131 billion (95% CI: $91 billion, $172 billion) before adjusting for BMI and $117 billion (95% CI: $76 billion, $158 billion) after adjusting for BMI of health care expenditures per year were associated with inadequate levels of physical activity.
Sensitivity analysis
Mean differences in expenditures for inactive and insufficiently active persons (compared to active) remained significant after excluding adults who reported at baseline ever having a heart attack; ever having a stroke; needing help getting in/out of bed or chairs, using the toilet, or getting around the home; difficulty walking because of a health problem; who died during the MEPS year; or who were aged 80 or over (Fig 1).
Fig 1.
Mean Expenditure Differences per Capita of Inactive and Insufficiently Active Versus Active Physical Activity Levels, after Selected Exclusions – US Adults, NHIS and MEPS 2006–2011a,b. Abbreviations: BMI, body mass index; CI, confidence interval; MEPS, Medical Expenditure Panel Survey; NHIS, National Health Interview Survey. aPhysical activity level is defined as active (≥150 minutes/week moderate-intensity equivalent activity), insufficiently active (some moderate-intensity equivalent activity but not enough to meet active definition), and inactive (no moderate-intensity equivalent activity that lasted at least 10 minutes). Models adjust for: sex, age group, race/ethnicity, census region, metropolitan statistical area, marital status, education, poverty level, health insurance status, smoking status, BMI category, and MEPS year. bExcludes adults who were pregnant and those who reported being unable to do physical activity. The number of adults excluded for each subanalysis was: 1861 reported ever having a heart attack at baseline (i.e., NHIS interview); 1544 reported ever having a stroke at baseline; 514 reported at baseline needing help getting in/out of bed or chairs, using toilet, or getting around the home; 3206 reported at baseline difficulty walking (without the use of equipment) because of a health problem; 520 died during MEPS survey year; or 3298 ≥ 80 years of age. cExpenditures adjusted to 2012 dollars using the Personal Health Care Expenditure Price Index. Upper and lower error bars represent upper and lower bounds of the 95% CI. Dashed vertical lines represent overall estimates.
The largest overall change in estimates was observed when adults with any reported difficulty walking because of a health problem were excluded; therefore, all estimates were recalculated after this exclusion (Table 3). This exclusion resulted in removing 4.5% of the population. About 28.0% of adults with reported difficulty walking were aged 80 years or older. The majority of adults (63.1%) with reported difficulty walking were inactive, 18.8% were insufficiently active, and 18.1% were active. After removing those with reported difficulty walking, the average total annual health care expenditure per year was $906 billion or 85.9% of aggregate health care expenditures for the overall population.
Table 3.
Expenditure differences, percent differences, and percentage of aggregate health care expenditures of inactive and insufficiently active versus active physical activity levels – US adults, excluding adults with reported difficulty walking, NHIS and MEPS 2006–2011a.
| Health Care Expenditure Differences Per Capita (compared to active) |
Percent Difference Per Capita (compared to active) |
Percentage of Aggregate Health Care Expenditures |
||||
|---|---|---|---|---|---|---|
| Model and Physical Activity Levelb | Mean ($)c | (95% CI) | % | (95% CI) | % | (95% CI) |
| Model 1: Physical activity and covariatesd | ||||||
| Inactive | 1015 | (614, 1416) | 23.6 | (13.6, 33.6) | 7.3 | (4.4, 10.1) |
| Insufficiently active | 603 | (258, 948) | 14.0 | (5.7, 22.2) | 2.7 | (1.2, 4.2) |
| Inactive and insufficiently active e | e | e | e | e | 9.9 | (6.5, 13.4) |
| Model 2: Physical activity, covariates,d and BMI category | ||||||
| Inactive | 920 | (509, 1332) | 20.9 | (10.9, 31.0) | 6.6 | (3.7, 9.5) |
| Insufficiently active | 482 | (142, 822) | 10.9 | (3.0, 18.7) | 2.1 | (0.7, 3.6) |
| Inactive and insufficiently active e | e | e | e | e | 8.7 | (5.2, 12.3) |
Abbreviations: BMI, body mass index; CI, confidence interval; MEPS, Medical Expenditure Panel Survey; NHIS, National Health Interview Survey; %, percentage.
Excludes adults who were pregnant and those who reported being unable to do physical activity. In addition, excludes 3206 adults (4.5%) with reported difficulty walking (without the use of equipment) because of a health problem.
Physical activity level is defined as active (≥150 minutes/week moderate-intensity equivalent activity), insufficiently active (some moderate-intensity equivalent activity but not enough to meet active definition), and inactive (no moderate-intensity equivalent activity that lasted at least 10 minutes).
Expenditures adjusted to 2012 dollars using the Personal Health Care Expenditure Price Index.
Covariates include sex, age group, race/ethnicity, census region, metropolitan statistical area, marital status, education, poverty level, health insurance status, smoking status, and MEPS year.
Estimates of mean difference and percent difference are based on models including inactive and insufficiently active as distinct categories therefore these estimates are not provided for the combined group. Percentages for the inactive and sufficiently active may not add to total due to rounding.
After these adults were excluded, all estimates decreased although differences between inactive and insufficiently active adults compared to those active remained significant (Table 3). Among adults with no reported difficulty walking, the percentage of health care expenditures associated with inadequate levels of physical activity was significant at an estimated 9.9%, resulting in about $90 billion (95% CI: $58 billion, $122 billion) of health care expenditures per year associated with inadequate levels of physical activity. Similar to findings for the overall population, the percentage of health care expenditures associated with inadequate levels of physical activity decreased slightly but remained significant after adjusting for BMI (8.7%, Table 3), resulting in about $79 billion (95% CI: $46 billion, $112 billion) of health care expenditures per year associated with inadequate levels of physical activity.
Discussion
The study findings show during 2006–2011, independent of BMI, inadequate levels of aerobic physical activity (after adjusting for BMI) were associated with an estimated 11.1% of aggregate health care expenditures. Excluding adults with any reported difficulty walking, inadequate levels of physical activity were associated with 8.7% of aggregate health care expenditures. The considerable financial burden associated with inadequate levels of physical activity in the U.S. could potentially be reduced by increasing adults' physical activity to levels consistent with current guidelines and Healthy People 2020 objectives.2,32
It is difficult to compare this study's findings with other studies linking physical activity and health care expenditures because of the numerous measures and methods that have been used.10–18 There are two studies whose findings can be roughly equated to this study's defined physical activity levels, and findings from these studies were similar. In this study, we found the percent difference in health care expenditures for an active adult compared to an inactive adult was 26.6% overall and 20.9% when limited to adults with no reported difficulty walking. In a study of Australian women age 50 to 55, the percent difference in costs for sedentary versus moderately-active (a level consistent with current guidelines) women was 26.3%.13 Among enrollees in a Minnesota health plan age 40 or older, each additional “active” day per week was associated with a 4.7% decrease in health care cost. Thus, 5 days of activity would represent about a 23.5% cost reduction compared with no days of physical activity.14
This study's estimate of the percentage of health care expenditures in the U.S. associated with physical inactivity is different from the one previous study providing this estimate. The previous study estimated that 2.4% of health care expenditures in the U.S. were associated with physical inactivity.5 When examining physical inactivity alone, we found that overall 8.8% of health care expenditures were associated with physical inactivity and 6.6% when adults with reported difficulty walking were excluded. There are a number of methodological differences between the two studies that may explain much of the difference.5 First, physical activity is related to numerous conditions1; however, the previous study5 limited costs to only coronary heart disease, hypertension, colon and breast cancer, diabetes, gallbladder disease, and osteoporotic fractures. Second, the previous study5 used a population attributable fraction approach to allot condition-specific costs to physical inactivity, while this study used a regression based approach to examine total health care expenditures. A study examining diabetes-attributable medical spending found estimates were 43% higher when comparing regression based and attributable fraction approaches, even when the attributable fraction approach considered a comprehensive list of conditions.33 A regression based approach may be higher because it incorporates not only the higher probability of a condition but also the costs of increased treatment intensity for adults with a condition.33 Future work may wish to examine the influence different methodologies have on estimates of the economic burden associated with inadequate levels of physical activity.
Reverse causality may be a concern. It could be argued that some persons who are not physically active have higher health care expenditures because previous health events limit their ability to be active while also increasing health care expenditures. This issue was addressed with two elements of the study design. First, there is a 1 to 2 year lag between the physical activity assessment and the time when health care expenditure data are collected; therefore, any new health events captured in the health care expenditure measure would not directly influence an individual's physical activity level. Second, adults who reported being unable to do physical activity were excluded from the analytic sample.
In addition, multiple sensitivity analyses that excluded certain individuals from the study population were conducted. When individuals who reported previous health events, limitations, and difficulty walking, or who died during the MEPS year were excluded, estimates of mean differences in health care expenditures for inactive adults compared to active adults decreased but were still significant. There are two plausible explanations for this decrease: 1) individuals were inactive because of poor health, confounding the association, and when individuals in poor health were removed the association decreased; or 2) the sensitivity analyses controlled for other ways physical activity might influence health care expenditures, and the association decreased as some of the influences were removed. For example, when adults with reported difficulty walking because of a health problem were excluded, the influence physical activity may have had on these individuals experiencing the health problem and their ability to maintain function after the health problem was removed. If someone had been active prior to the event and had later become inactive, to include the individual would overestimate the costs of inactivity; however, if the individual had been inactive prior to the health event and remained inactive, excluding that person would result in an underestimate. Given the data, it is not possible to determine which of these explanations was more likely. However, through the multiple sensitivity analyses findings were found to be robust to different sample specifications. Also, the more conservative estimates calculated when adults with any reported difficulty walking were excluded are provided.
Several limitations are noted. This study used observational data, which may have biased the observed associations by introducing confounding factors. To reduce such bias, models controlled for several factors; however, it was not possible to control for all potential confounding factors. For example, active adults may have had positive health behaviors related to diet, sleep, or participation in preventive care. Second, MEPS data rely on one household informant to report health care expenditures for all household members with a sample of expenditures further verified and supplemented with data from medical providers.34 Studies have shown that health care expenditures are underreported in MEPS.35,36 If underreporting is similar across demographic and behavioral characteristics, this underreporting would likely lead to underestimates of mean per capita and total health care expenditures associated with inadequate levels of physical activity. Third, NHIS physical activity data are derived from self-reported information, and studies have indicated that reporting bias can result in high estimates of physical activity.34 However, individuals overestimating their physical activity would likely lead to a more conservative estimate of the association between physical activity and health care expenditures. Finally, the physical activity measure is based only on leisure-time activity and this may have resulted in an underestimate of physical activity levels when individuals' occupations are considered.
This study has several important strengths. First, data from the NHIS and MEPS include a large, nationally representative sample, allowing for broad generalizability of findings to non-institutionalized U.S. adults. In addition, the NHIS and the MEPS contained relevant variables that allowed models to include many covariates and provided data to conduct multiple sensitivity analyses. Finally, the physical activity measure categorized individuals into levels consistent with current physical activity guidelines.2
Levels of physical activity inadequate to meet current guidelines are associated with a significant financial burden for the U.S. health care system. This study's estimates are limited to direct health care expenditures associated with inadequate physical activity in the non-institutionalized population. This study did not estimate indirect costs, which include lost productivity from premature death and disability associated with illness, nor does it address the costs in the institutionalized population that may be associated with inadequate levels of physical activity. Future studies that consider these additional costs may improve estimates of the economic burden of inadequate physical activity. Nevertheless, this study found that inadequate physical activity is associated with a significant percentage of health care expenditures in the U.S.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Abbreviations and Acronyms
- BMI
Body Mass Index
- MEPS
Medical Expenditure Panel Survey
- NHIS
National Health Interview Survey
- U.S.
United States
Footnotes
Statement of Conflict of Interest We have no conflicts of interest to report.
REFERENCES
- 1.Physical Activity Guidelines Advisory Committee . Physical activity guidelines advisory committee report, 2008. U.S. Department of Health and Human Services; Washington, DC: 2008. [DOI] [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services . 2008 physical activity guidelines for Americans. U.S. Department of Health and Human Services; Washington, DC: 2008. [Google Scholar]
- 3.Schiller JS, Lucas JW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2011. Vital Health Stat. 2012;10(11):97–102. [PubMed] [Google Scholar]
- 4.Allender S, Foster C, Scarborough P, Rayner M. The burden of physical activity-related ill health in the UK. J Epidemiol Community Health. 2007;61:344–348. doi: 10.1136/jech.2006.050807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colditz GA. Economic costs of obesity and inactivity. Med Sci Sports Exerc. 1999;31:S663–S667. doi: 10.1097/00005768-199911001-00026. [DOI] [PubMed] [Google Scholar]
- 6.Garrett NA, Brasure M, Schmitz KH, Schultz MM, Huber MR. Physical inactivity: direct cost to a health plan. Am J Prev Med. 2004;27:304–309. doi: 10.1016/j.amepre.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 7.Katzmarzyk P, Janssen I. The economic costs associated with physical inactivity and obesity in Canada: an update. Can J Appl Physiol. 2004;29:90–115. doi: 10.1139/h04-008. [DOI] [PubMed] [Google Scholar]
- 8.Katzmarzyk PT, Gledhill N, Shephard RJ. The economic burden of physical inactivity in Canada. CMAJ. 2000;163:1435–1440. [PMC free article] [PubMed] [Google Scholar]
- 9.Popkin BM, Kim S, Rusev ER, Du S, Zizza C. Measuring the full economic costs of diet, physical activity and obesity-related chronic diseases. Obes Rev. 2006;7:271–293. doi: 10.1111/j.1467-789X.2006.00230.x. [DOI] [PubMed] [Google Scholar]
- 10.Pratt M, Macera CA, Wang G. Higher direct medical costs associated with physical inactivity. Phys Sportsmed. 2000;28:63–70. doi: 10.3810/psm.2000.10.1237. [DOI] [PubMed] [Google Scholar]
- 11.Anderson LH, Martinson BC, Crain AL, Pronk NP, Whitebird RR, O'Connor PJ, et al. Health care charges associated with physical inactivity, overweight, and obesity. Prev Chronic Dis. 2005;2:A09. [PMC free article] [PubMed] [Google Scholar]
- 12.Bland PC, An L, Foldes SS, Garrett N, Alesci NL. Modifiable health behaviors and short-term medical costs among health plan members. Am J Health Promot. 2009;23:265–273. doi: 10.4278/ajhp.08042842. [DOI] [PubMed] [Google Scholar]
- 13.Brown WJ, Hockey R, Dobson AJ. Physical activity, Body Mass Index and health care costs in mid-age Australian women. Aust N Z J Public Health. 2008;32:150–155. doi: 10.1111/j.1753-6405.2008.00192.x. [DOI] [PubMed] [Google Scholar]
- 14.Pronk NP, Goodman MJ, O'Connor PJ, Martinson BC. Relationship between modifiable health risks and short-term health care charges. JAMA. 1999;282:2235–2239. doi: 10.1001/jama.282.23.2235. [DOI] [PubMed] [Google Scholar]
- 15.Wang F, McDonald T, Reffitt B, Edington DW. BMI, physical activity, and health care utilization/costs among Medicare retirees. Obes Res. 2005;13:1450–1457. doi: 10.1038/oby.2005.175. [DOI] [PubMed] [Google Scholar]
- 16.Yang G, Niu K, Fujita K, Hozawa A, Ohmori-Matsuda K, Kuriyama S, et al. Impact of physical activity and performance on medical care costs among the Japanese elderly. Geriatr Gerontol Int. 2011;11:157–165. doi: 10.1111/j.1447-0594.2010.00651.x. [DOI] [PubMed] [Google Scholar]
- 17.Wang F, McDonald T, Champagne LJ, Edington DW. Relationship of body mass index and physical activity to health care costs among employees. J Occup Environ Med. 2004;46:428–436. doi: 10.1097/01.jom.0000126022.25149.bf. [DOI] [PubMed] [Google Scholar]
- 18.Wang G, Pratt M, Macera CA, Zheng ZJ, Heath G. Physical activity, cardiovascular disease, and medical expenditures in U.S. adults. Ann Behav Med. 2004;28:88–94. doi: 10.1207/s15324796abm2802_3. [DOI] [PubMed] [Google Scholar]
- 19.Bell JF, Zimmerman FJ, Arterburn DE, Maciejewski ML. Health-care expenditures of overweight and obese males and females in the medical expenditures panel survey by age cohort. Obesity (Silver Spring) 2011;19:228–232. doi: 10.1038/oby.2010.104. [DOI] [PubMed] [Google Scholar]
- 20.Finkelstein EA, Fiebelkorn IC, Wang G. National medical spending attributable to overweight and obesity: how much, and who's paying? Health Aff (Millwood) 2003:W3219–W3226. doi: 10.1377/hlthaff.w3.219. Suppl. Web Exclusives: W3-219-W3-226. [DOI] [PubMed] [Google Scholar]
- 21.Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood) 2009;28:w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 22.National Center for Health Statistics (NCHS) [Date Accessed: 2013 November 3];National Health Interview Survey (NHIS) Available from: http://www.cdc.gov/nchs/nhis.htm.
- 23.Agency for Healthcare Research and Quality (AHRQ) [Date Accessed: 2013 November 3];Medical Expenditure Panel Survey (MEPS) Available from: http://www.meps.ahrq.gov/mepsweb/
- 24.Agency for Healthcare Research and Quality (AHRQ) [Date Accessed: 2014 April 19];Using appropriate price indices for analyses of health care expenditues or income across multiple years. Available from: http://meps.ahrq.gov/mepsweb/about_meps/Price_Index.shtml.
- 25.National Heart, Lung, and Blood Institute . Clinical guidelines on the identification, evaluation, and treatment of over-weight and obesity in adults: the evidence report. U.S. Department of Health and Human Services, National Institutes of Health; Bethesda, MD: 1998. [Google Scholar]
- 26.Manning WG, Newhouse JP, Duan N, Keeler EB, Leibowitz A, Marquis MS. Health insurance and the demand for medical care: evidence from a randomized experiment. Am Econ Rev. 1987;77:251–277. [PubMed] [Google Scholar]
- 27.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20:461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- 28.Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. 2004;23:525–542. doi: 10.1016/j.jhealeco.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 29.Adams EK, Melvin CL, Raskind-Hood C, Joski PJ, Galactionova E. Infant delivery costs related to maternal smoking: an update. Nicotine Tob Res. 2011;13:627–637. doi: 10.1093/ntr/ntr042. [DOI] [PubMed] [Google Scholar]
- 30.Cohen SB. An estimation methodology to permit longitudinal cohort analyses based on the National Health Interview Survey and Medical Expenditure Panel Survey, Agency for Healthcare Research and Quality Working Paper No. 11002. Agency for Healthcare Research and Quality (AHRQ); Rockville, MD: 2010. [Google Scholar]
- 31.Izrael D, Hoaglin DC, Battaglia MP. Proceedings of the Twenty-Fifth Annual SAS Users Group International Conference. 2000. A SAS macro for balancing a weighted sample. [Google Scholar]
- 32.U.S. Department of Health and Human Services [Date Accessed: 2012 December 1];Healthy people 2020. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/default.aspx.
- 33.Honeycutt AA, Segel JE, Hoerger TJ, Finkelstein EA. Comparing cost-of-illness estimates from alternative approaches: an application to diabetes. Health Serv Res. 2009;44:303–320. doi: 10.1111/j.1475-6773.2008.00909.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sallis JF, Saelens BE. Assessment of physical activity by self-report: status, limitations, and future directions. Res Q Exerc Sport. 2000;71:S1–S14. [PubMed] [Google Scholar]
- 35.Zuvekas SH, Olin GL. Validating household reports of health care use in the medical expenditure panel survey. Health Serv Res. 2009;44:1679–1700. doi: 10.1111/j.1475-6773.2009.00995.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zuvekas SH, Olin GL. Accuracy of Medicare expenditures in the medical expenditure panel survey. Inquiry. 2009;46:92–108. doi: 10.5034/inquiryjrnl_46.01.92. [DOI] [PubMed] [Google Scholar]