Abstract
The goal of modern diabetes treatment is to a large extent focused on self-management to achieve and maintain a healthy, low HbA1c. Despite all new technical diabetes tools and support, including advanced blood glucose meters and insulin delivery systems, diabetes patients still struggle to achieve international treatment goals, that is, HbA1c < 7.5 in children and adolescents. In this study we developed and tested a mobile-phone-based tool to capture and visualize adolescents’ food intake. Our aim was to affect understanding of carbohydrate counting and also to facilitate doctor–adolescent communication with regard to daily treatment. Furthermore, we wanted to evaluate the effect of the designed tool with regard to empowerment, self-efficacy, and self-treatment. The study concludes that implementing a visualization tool is an important contribution for young people to understand the basics of diabetes and to empower young people to define their treatment challenges. By capturing a picture of their own food, the person’s own feeling of being in charge can be affected and better self-treatment achieved.
Keywords: diabetes, empowerment, self-care, M-health
Diabetes treatment is challenging to adults, but even more so to young people. There is often a gap between the goal of treatment suggested by health care workers and official recommendations, versus young people’s own goals. Often the priority of young people is to assimilate and be similar to their peers, this often leads to neglecting the disease and treatment recommendations.1-3 Young people’s lack of advanced cognitive function due to late maturation of the frontal lobes in the brain is a limiting factor highly underestimated by health professionals.4 Self-care is dependent on a high level of perceived efficacy with integration of lots of information mixed with practical skills and competence. When cognitive functions are limited we need to develop systems that ease the understanding of diabetes and execution of self-treatment. Thus, pediatric and adolescent care need to be tailored to the target group to a much larger degree than practiced today.
Diabetes care and education are typically based on building competence based on theoretical and practical aspects of diabetes treatment. A lot of this theory is complex, and one needs an advanced cognitive function to be able to understand and utilize this into practical self-treatment. Magnetic resonance imaging studies demonstrate that motor and sensory brain areas mature first, the primary visual cortex matures early, while areas involved in executive functions mature later. This development pattern might facilitate the use of modern technology making use of visual imaging in this particular patient group.5
The authors performed a study utilizing the camera in a mobile phone as an add-on to a digital diabetes diary, to create a visual-based diabetes diary and a patient–doctor consultation tool. Some results from this study have been published elsewhere.4 This article focuses on the results regarding specific user experiences related to patient empowerment and prospective nutrition-based mobile systems that may ease daily self-care.
Food and Insulin
Understanding the amount of carbohydrates in the diet and how this affects blood glucose is 1 of the cornerstones of diabetes treatment. The total quantity of carbohydrates in food need to be calculated and the amount of insulin to be given needs to be adapted to this. We know that the insulin-carbohydrate ratio is different for each individual, the need for patients and caregivers to learn from each individual’s experience and reflect on this are therefore important. However, we know that the prevalence of disturbed eating behavior is high among young people with diabetes.6 It is suggested that a strong focus on rations and carbohydrates can partly contribute to an unhealthy relation to food and diet.7
Many patients struggle to find the right insulin dose to avoid low or high blood glucose and often look on this as a very demanding part of treatment. Parents and health care workers often suggest doses and give advice based on assumptions of amount and types of food consumed. A lot of work is performed to ease the calculation of carbohydrate in food and the amount of insulin needed. However, often patients and their carers base the use of advanced tools such as bolus calculators and each patient’s own insulin-carbohydrate ratio on best guess rather than facts. If insulin doses given are based on false assumptions of carbohydrate amounts, there is no surprise that treatment goals are difficult to achieve. Patients and caregivers therefore need to share a platform where food actually consumed is presented. Therefore, capturing and presenting pictures of food eaten is a way to improve common understanding of carbohydrate amounts between patients, parents, and health care workers. Such images can therefore affect the success rate of self-treatment, and through this we may be able to affect the feeling of empowerment in young patients.
Empowerment
Empowerment in relation to people’s own life and health is to a large extent based on Antonovsky’s concepts of sense of coherence (SOC) and general resistance resources (GRRs), claiming that people’s life orientations will have an impact on health. The SOC consists of at least 3 dimensions: comprehensibility, manageability, and meaningfulness.8 Patient empowerment focuses on the patient as taking an active role in her or his own disease management, or as being a contributing member of the medical decision team. This includes participation in and respect for patient advocacy, self-determination, health care consumerism, and patient safety.9 Empowerment is described in various ways and may be generalized as this: “A generic term for encouraging the active participation of patients and caregivers in choosing management options. It can be seen as a philosophy focusing on patients as active participants, not passive recipients, in the caring process, and thus they should be well informed about all aspects of their health, ‘wellness status’ and disease state, to gain maximum health benefit within the context of their social demands.”10 Funnell et al state that “patients are empowered when they have knowledge and skills, attitudes and self-awareness, necessary to influence their own behavior and that of others to improve the quality of their treatment and life.”11
It is hypothesized that to manage diabetes in different social settings we need to build more on mastery, vicarious experiences provided by social models, and social persuasiveness.12
Information and Communication Technology
During recent decades there has been a rapid development in information and communication technology (ICT). In health care we may see an ease in the flow of information between providers and their patients.13-15 These technologies include the Internet, email, and mobile phone applications (apps), and are often referred to as electronic health or “eHealth.”16 Studies of the use of mobile-phone-based tools among adolescents are few. The most important reasons for utilizing mobile phone apps in health care are the widespread use of mobile phones as well as their potential to integrate information from different types of wearable computers and sensors. In many ways we seem to approach what some has called a “mobile health revolution.”17,18 Examples of tools within diabetes is the “My Diabetes” app where user can choose either the mobile phone to enter self-management data or external sensors such as the Medtronic CareLink to import continuous glucose monitoring (CGM) system.19 In Norway, 94% of children and adolescents (9-16) have daily access to a mobile phone and 83% to a smartphone.20 Some wearable computers like wrist bands and smart watches communicate with mobile phone apps and diabetes self-care tools. In the future the aim is to develop a convenient and easy method to include multiple lifestyle information from different devices into applications that will ease the daily treatment of diabetes. Our study is part of an ongoing search for better tools in diabetes care, thus integrating useful functions in mobile phones at this stage may be an important feature of approaching future diabetes self-care.
Method
We performed and recorded interviews with each of the informants. Some of the results have been published elsewhere.4
Intervention
The intervention period was 3 months and has been described in detail earlier.4 The participants were introduced to a smartphone (HTC Touch 2), and 2 diabetes software applications. A mobile-phone-based diabetes diary called DiaMob and the diabetes message system (DMS), a short message system based on the Secure Health Dialogue SMS.21 Generally, participants could use the DiaMob application as much as they wanted but at least 2 full 3-day registration periods were mandatory. Participants came for a consultation with the research team (midway) to discuss the usage and have a “reflection in action” talk about the mandatory 3-day recordings in the DiaMob application. At the end of the 3-month period, the informants met with the research team for a semistructured interview. The interviews lasted between 30 minutes and 1 hour.
Smartphone Applications
Application 1: DiaMob
A smartphone camera was used to capture the actual diet of the patients in the DiaMob application and targets carbohydrate evaluation and insulin dosages. To start the process they had to choose 1 out of 4 pictograms describing the actual physical activity they planned to participate in or already had been involved in.22 Actual insulin dosage suitable for the food they planned to eat was entered and the app then started the camera function in the mobile phone and the portion was pictured. The phone and glucometer communicated via Bluetooth technology to automatically transfer the measured blood glucose values.
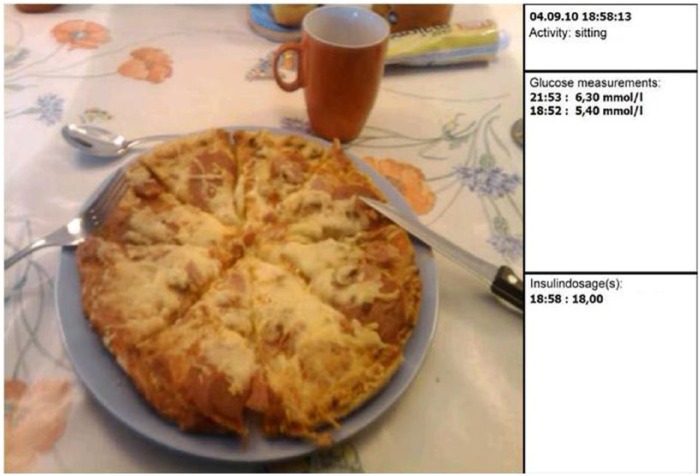
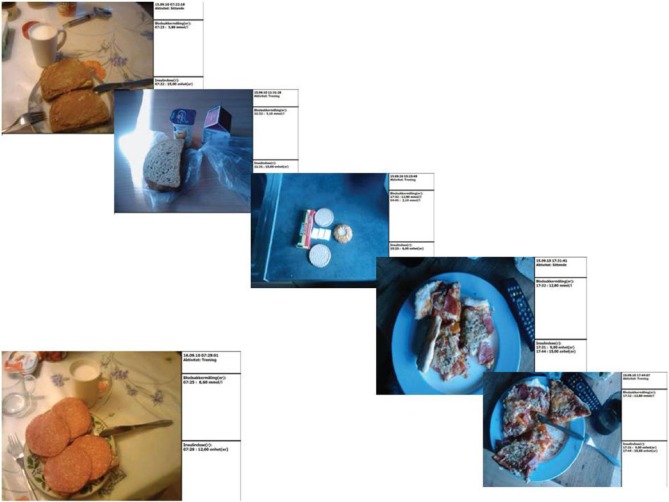
The picture produced by the DiaMob application incorporated relevant pre- and postprandial blood glucose values, insulin dosage given, and information of their physical activity (Figure 1), and could be displayed both on the user’s mobile phone and transferred to the clinician’s PC during consultation. A 24-hour diabetes diary has been created demonstrating the application (Figure 2).
Figure 1.
Example of picture produced by the DiaMob App. Pictures were available to the users to browse through on phone and could also be uploaded to computers and used during consultation.
Figure 2.
Example of a 24-hour period of food pictures used to discuss the eating habits, carbohydrate amounts, and insulin dosages at a consultation.
Application 2: Diabetes Message System
Due to strict Norwegian laws regarding health communication, a functional Internet-based encrypted short message system based on Secure Health Dialog System was created.21 This SMS system is referred to as the DMS. The participants were invited to use this application to send SMS messages to their providers.
Sample
We recruited a convenience sample of adolescents aged between 13 and 19 years in Eastern Norway. The participants were diagnosed with Type 1 diabetes at least 1 year prior to the start of the study, and with a current HbA1c of less than 10.0%. Twelve participants were enlisted, 7 girls and 5 boys. Of the 12 interviewees, 1 withdrew from the use of the applications halfway through the intervention due to personal reasons. All 12 participants were interviewed at the end.
Interviews
A semistructured interview guide was developed to elicit topics described in the aims of the study. The interviews were conducted in a meeting room at 2 outpatient clinics in Innlandet Hospital Trust Norway, each lasting between 45 and 90 minutes. Recordings were later transcribed; nonverbal aspects of the communication, such as pauses and laughter, were included. To analyze the interviews with regard to empowerment, we decided to use a deductive approach based on empowerment theory.11,23-26 Theory on empowerment in regard to diabetes were assessed and through discussions in the research team a few predefined factors thought to be important to empowerment and daily care, were enlisted. To evaluate changes with regard to empowerment among the adolescents we wanted to shed light on these predefined factors (Table 1). Some results from this study have already been reported elsewhere.4
Table 1.
Empowerment Factors Results From Analyses and Final Themes.
| Predefined empowerment factors | Results from analyses of interviews | Final theme |
|---|---|---|
| • If the disease was perceived as comprehensive and manageable. | Told that they understood diabetes theory before start of the study. However, reported that the picture app changed their understanding of cornerstones of treatment. | Improved comprehension and increased feeling of managing the self-treatment. |
| This was reported as giving them an increased feeling of being able to manage the disease. | ||
| • The sense of influence over and feeling of meaning in their own life. | Most adolescents in the study felt in charge of their own life, however they talked about acceptance as an important factor. Acceptance of own disease and treatment and also acceptance from important others like friends to treatment while in different social settings. | Social settings change action readiness with regard to acceptance of disease and self-treatment. |
| DiaMob increased social acceptance | ||
| • Feeling of being recognized with regard to self-treatment and self-medication. | Positive response from people who know the disease is important to feel empowered. The SMS application increased the possibility for response directly from their health care professional. The direct contact with those they trust was reported as important. To know that they got an answer back, gave a feeling of acceptance and to be paid attention to. | Positive feedback leads to mastery and increases empowerment. |
| Negative feedback leads to opposition. | ||
| SMS solutions lower the threshold for contact and give adolescents a sense of “being in charge.” | ||
| • The adolescents’ experience of coping—including access to and the ability to exploit knowledge, social resources, or equipment. | The most important factor for coping was seen as control of improved daily glucose values. DiaMob was reported as giving them better insight into what causes changes in glucose measurements. They reported better coping and not least increased motivation to succeed. | To see and reflect using pictures improves understanding and knowledge and affects self-treatment. |
| • Changes in any desire to improve their own situation. | DiaMob gave them a visual and tangible understanding of how physical activity, food intake, and insulin dosage, interact and affect postprandial glucose measurements. This gave them a new start to change the direction of their own treatment. | Patients are empowered and can change their own lives when they are able to integrate knowledge and resources to take rational decisions. Through experience they are further able to evaluate the effectiveness of their decisions.11 |
| SMS solution gave them a feeling of being in charge and closer to the health care practitioners. |
Questions with regard to empowerment were asked at the end of each interview to ensure that the predefined factors for empowerment were illuminated.
We also wanted to assess the way the young people evaluated their own food and the amount of carbohydrates they ate.
Ethical Considerations
The adolescents and their parents gave written consent for the study according to Norwegian requirements. The study was approved by the Regional Committee on Medical Research Ethics (Ref: 2009/773b).
Results
The participants were asked to commit to complete 2 sets of diabetes diary records, each covering a continuous period of 3 days, during the intervention. This would yield approximately 24 pictures for each participant (288 pictures). During the study, 691 pictures were downloaded (mean 50, minimum 25, maximum 94).
The overall results from the data analysis demonstrated that adolescents found both mobile applications useful as support for their diabetes self-management. These data were supported by scores on the System Usability Scale (SUS).4 Furthermore, glycemic control, as measured by HbA1c, improved in 7 out of 11 participants completing the study.4 With regard to the empowerment criteria, our findings suggest that the use of ICT in this setting improves factors thought to be important for these young people to feel empowered and take care of their diabetes self-treatment. To use the camera to picture the actual food the diabetes patients ate, incorporating pre and postprandial glucose measurements in the final pictures, increases the possibilities for both caregivers and patients to share a common platform to find the right insulin-carbohydrate ratio. Implementing all 4 cornerstones of diabetes treatment in the picture of actual food intake seems to increase comprehensibility, manageability, and meaningfulness (Table 1), and should therefore be utilized in diabetes care to a larger extent.
Food, Carbohydrates, and Visualization
The adolescents stated that to see their own food made them reflect on their unhealthy habits of food intake. Even the participating health care practitioners were surprised by the amount of carbohydrates actually eaten by the Type 1 diabetes patients. Generally, the patients ate more carbohydrates than expected, and initially they underestimated the amount of insulin needed to match their daily diet. The application made it possible for caregivers and patients to evaluate amounts of carbohydrate more exact.
Discussion
The main result of this study was that the 2 applications were found useful by the participants. They reported a better understanding of the relationship between food (carbohydrates), the amount of insulin and how this affected the blood glucose levels. An increased understanding of these important cornerstones of treatment seems to improve self-treatment and the feeling of success. Succeeding in better and tighter glucose control will improve HbA1c, and we also know that this is closely linked to improved health-related quality of life.4,27 Success and optimism are important in influencing young people’s confidence and self-efficacy in diabetes self-care and through this improved treatment results,28,29 especially during the adolescent period, when we know that the feeling of shortcoming can be detrimental. To facilitate success in daily treatment, through better understanding of important cornerstones, is therefore crucial. DiaMob and DMS were useful in this aspect.
Reports on HbA1c results and the SUS have been reported elsewhere,4 however, it is important to keep in mind that these outcomes were used to ensure a triangulation of the study results, and despite not being the focus of this article we highlight these findings as an additional strength of our study results. Results on the predefined areas focusing on empowerment changes (Table 1) are also favorable to the mobile phone applications.
The adolescents felt that DiaMob improved comprehension of the disease and increased the teenagers’ feelings of being able to manage self-treatment. Furthermore, the adolescents reported that DiaMob increased the social acceptance of the disease. Antonovsky states that feelings of comprehensibility, manageability, and meaningfulness are essential for people to take charge of their own tasks in life.8 This has been linked to empowerment and self-efficacy and is important for taking care of a disease 24 hours, 7 days a week. The adolescents reported improved knowledge and skills, attitudes and self-awareness. These are claimed by Funnell et al as necessary for empowerment.11 One of the results reported earlier4 on facilitated and increased understanding and knowledge of diabetes treatment is thought to be caused by pictures being processed by parts of the brain that mature early in life. The future of diabetes care in children and adolescents probably should include picture-based material rather than traditional theoretical education.
Health care practitioners have a role in engendering optimism, in maintaining enthusiasm, and facilitating and encouraging maintenance of health behaviors.29 It is interesting that the adolescents reported that the 2 mobile apps actually contributed to a feeling of increased support from their health care providers. Positive feedback was obtained through discussions when their own food pictures with results of glucose measurements, amount of carbohydrates, and insulin doses were discussed. The adolescents reported that to see these pictures, both on a mobile and on a clinician’s PC during consultation, increased reflection, improved understanding and knowledge, and they reported better coping and increased motivation to succeed in self-treatment.
The possibility of using DMS to get in contact with their caregivers was perceived as a tool enabling them to take action and be in charge. The health care system needs to listen to this message and we need to adapt to the rapid developments in ICT and the young generation’s motivation to use such tools in chronic diseases.
Empowerment has been important in diabetes care for more than 30 years. Young people actually report, in line with empowerment theory, that they feel empowered and can change their own lives when they are able to integrate knowledge and resources to take rational decisions.11 Visualization of food and the presentation, together with pre- and postglucose measurements, insulin doses, and physical activity, gives health care providers and patients a common platform and tool to improve knowledge and enhance rational decisions. Through discussions this enables young patients to improve future self-treatment.
Food, Carbohydrates, and Visualization
Both patients and their caregivers were often surprised by the large amount of carbohydrates and unhealthy eating habits of the diabetes patients. Patients reflected on their own diet and the visualization gave caregivers and their patients a common platform based on a real world situation. A paper-based diabetes diary does not specify portions. Some pictures, like the one in Figure 1, point out that patients actually ate a huge amount of pizza twice in less than 15 minutes. Most health care practitioners would not know the actual quantity of pizza eaten if this was reported in a traditional paper diary. DiaMob was therefore a tool that increased the possibilities to make advice on insulin doses a lot more specific and easier to understand for patients and their helpers.
Future Use
Our DiaMob app is still not available on the market. The adolescents suggested improvements for the next generation to be developed. The future direction of development should optimally incorporate technology from pumps and pods as well as the new innovative glucose meters and wearable microcomputers to better improve the accuracy of what is going on in the body in real-time. An integration of all these variables within a dynamic algorithm, acting as close as possible to an artificial pancreas, may help to enhance daily diabetes care. We believe that the time for such tools is just around the corner and our study shows that this will support young people in their self-care.
Conclusion
Mobile applications based on visualization seem to be an important way to support young people with diabetes to understand the basics of their disease and to empower them to define and cope with their treatment challenges. The person’s own feeling of being in charge can be affected and better self-treatment achieved. Future diabetes care needs to implement ICT based on mobile phone applications, and/or other wearable computing applications such as smart watches and wearable sensors (eg, improved CGM systems). The prospect of applications using algorithms that integrate real-time automatically recorded activities, heart rate, blood pressure, and so on, with camera recognition to automatically analyze the amount of carbohydrates, and that communicates directly with modern CGM systems as well as pumps and pods, is no longer science fiction. Approaching prototypes and studies involving these technologies will help us enhance diabetes care and contribute to the aim of designing an artificial pancreas system.
Supplementary Materials
The original sound tracks from interviews and their transcripts are stored in the university college’s personal computer. The material can be accessed through contact with the first author.
Acknowledgments
The authors wish to express their gratitude to the teenagers participating in the study, and to the diabetes nurses and doctors at the participating centers. Furthermore, we are grateful for the support from the system development team at NST and to WTW for valuable help, and to master’s student Anett Helen Westerbø who performed interviews and helped out analyzing some of the results.
Footnotes
Abbreviations: CGM, continuous glucose monitoring; DMS, Diabetes Message System; eHealth, electronic health; GRRs, general resistance resources; HbA1c, hemoglobin A1c; ICT, information and communication technology; NST, Norwegian Centre for Integrated Care and Telemedicine; SOC, sense of coherence.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a grant from Novo Nordic in Norway and the Norwegian Diabetes Association. We also appreciate the financial support from Professor Knut Dahl-Jorgensen’s research group in the developmental process.
References
- 1. Viner RM, Ozer EM, Denny S, et al. Adolescence and the social determinants of health. Lancet. 2012;379(9826):1641-1652. [DOI] [PubMed] [Google Scholar]
- 2. Jaccard J, Blant H, Dodge T. Peer influences on risk behavior: an analysis of the effects of a close friend. Dev Psychol. 2005;41(1):135-147. [DOI] [PubMed] [Google Scholar]
- 3. La Greca AM, Auslander WF, Greco P, Spetter D, Fisher EB, Santiago JV. I get by with a little help from my family and friends: adolescents’ support for diabetes care. J Pediatr Psychol. 1995;20(4):449-476. [DOI] [PubMed] [Google Scholar]
- 4. Frøisland DH, Årsand E, Skarderud F. Improving diabetes care for young people with type 1 diabetes through visual learning on mobile phones. J Med Internet Res. 2012;14(4):e111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gogtay N, Giedd JN, Lusk L, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci USA. 2004;101(21):8174-8179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wisting L, Frøisland DH, Skrivarhaug T, Dahl-Jørgensen K, Ro Ø. Disturbed eating behavior and omission of insulin in adolescents receiving intensified insulin treatment: a nationwide population-based study. Diabetes Care. 2013;36(20):3382-3387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jones JM, Lawson ML, Daneman D, Olmsted MP, Rodin G. Eating disorders in adolescent females with and without type 1 diabetes: cross sectional study. BMJ. 2000;320(7249):1563-1566. [PMC free article] [PubMed] [Google Scholar]
- 8. Eriksson M, Lindstrom B. Antonovsky’s sense of coherence scale and its relation with quality of life: a systematic review. J Epidemiol Community Health. 2007;61(11):938-944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Torrey T. The history of the patient empowerment movement. Available at: http://patients.about.com/od/patientempowermentissues/a/history_patemp.htm.
- 10. Empowerment, patients. Available at: http://medical-dictionary.thefreedictionary.com.
- 11. Funnell MM, Anderson RM, Arnold MS, et al. Empowerment: an idea whose time has come in diabetes education. Diabetes Educ. 1991;17(1):37-41. [DOI] [PubMed] [Google Scholar]
- 12. Bandura A. Self-efficacy mechanism in human agency. Am Psychol. 1982;37(2):122-147. [Google Scholar]
- 13. Avison D, Young T. Time to rethink health care and ICT? Comm ACM. 2007;50(6):69-74. [Google Scholar]
- 14. Jackson CL, Bolen S, Brancati FL, Batts-Turner ML, Gary TL. A systematic review of interactive computer-assisted technology in diabetes care. J Gen Int Med. 2006;21(2):105-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Blake H. Innovation in practice: mobile phone technology in patient care. Brit J Comm Nurs. 2008;13(4):160-165. [DOI] [PubMed] [Google Scholar]
- 16. Pagliari C, Sloan D, Gregor P, et al. What is eHealth (4): a scoping exercise to map the field. J Med Internet Res. 2005;7(1):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eng DS, Lee JM. Mobile health applications for diabetes and endocrinology: promise and peril? Pediatr Diabetes. 2013;14(4):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Arnhold M, Quade M, Kirch W. Mobile applications for diabetics: a systematic review and expert-based usability evaluation considering the special requirements of diabetes patients age 50 years or older. J Med Internet Res. 2014;16(4):e104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Varbanov R. My diabetes. Available at: https://sites.google.com/site/mydiabetesapp/home. Accessed October 14, 2014.
- 20. Medietilsynet. Barn og medier. Barn og unges (9-16) bruk og opplevelser av medier. Available at: http://www.medietilsynet.no/documents/barn%20og%20medier-undersøkelsene/rapport_barnogmedier_2014.pdf.
- 21. WTW. HelseRespons. Available at: http://helserespons.no.
- 22. Årsand E, Frøisland DH, Skrøvseth SO, et al. Mobile health applications to assist patients with diabetes: lessons learned and design implications. J Diabetes Sci Technol. 2012;6(5):1197-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Antonovsky A. The sense of coherence—an historical and future perspective. Israel J Med Sci. 1996;32(3-4):170-178. [PubMed] [Google Scholar]
- 24. Lindstrom B, Eriksson M. Salutogenesis. J Epidemiol Comm Health. 2005;59(6):440-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Funnell MM, Weiss MA. Empowering patients with diabetes. Nursing. 2009;39(3):34-37. [DOI] [PubMed] [Google Scholar]
- 26. Anderson RM, Funnell MM. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Educ Counseling. 2005;57(2):153-157. [DOI] [PubMed] [Google Scholar]
- 27. Frøisland DH, Graue M, Markestad T, Skrivarhaug T, Wentzel-Larsen T, Dahl-Jørgensen K. Health-related quality of life among Norwegian children and adolescents with type 1 diabetes on intensive insulin treatment: a population-based study. Acta Paediatrica. 2013;102(9):889-895. [DOI] [PubMed] [Google Scholar]
- 28. van der Ven NCW, Weinger K, Yi J, et al. The Confidence in Diabetes Self-Care Scale: psychometric properties of a new measure of diabetes-specific self-efficacy in Dutch and U.S. patients with type 1 diabetes. Diabetes Care. 2003;26(3):713-718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lo R. Correlates of expected success at adherence to health regimen of people with IDDM. J Adv Nurs. 1999;30(2):418-424. [DOI] [PubMed] [Google Scholar]