Abstract
Background:
Granulomatous amebic encephalitis (GAE) is rare, but often fatal. The infection has been documented predominantly among the immunocompromised population or among those with chronic disease. To date, however, there have only been eight cases regarding the infection following hematopoietic stem cell transplantation (HSCT).
Case Description:
A 62-year-old female with a history of relapsed diffuse large B-cell lymphoma, recently underwent peripheral blood autologous stem cell transplant after BEAM conditioning (day 0). On day +15, she began to exhibit worsening fatigue, generalized weakness, and fever. Symptoms progressed to nausea, emesis, somnolence, confusion, and frontal headaches over the next few days. Imaging demonstrated multifocal ill-defined vasogenic edema with patchy enhancement. The patient was started on broad antibiotics, antifungals, and seizure prophylaxis. Evaluation for bacterial, fungal, mycobacterial, and viral etiologies was fruitless. Her mental status progressively deteriorated. On day +22, she exhibited severe lethargy and went into pulseless electrical activity arrest, requiring chest compressions. The episode lasted <2 min and her pulse was restored. She was taken to the operating room for a brain biopsy. Postoperatively, her right pupil began to dilate compared to the left; she demonstrated extensor posturing in her upper extremities and withdrawal in her lower extremities. Repeat computed tomography demonstrated progressive edema. Given poor prognosis and poor neurological examination, the family opted for withdrawal of care. Final pathology was consistent with Acanthamoeba GAE.
Conclusion:
The authors report the third case of GAE after autologous stem cell transplant, and the ninth case overall after HSCT. This case is unusual due to its rapid clinical presentation after HSCT compared to prior literature. The case highlights the need for high suspicion of Acanthamoeba infection in this patient population.
Keywords: Acanthamoeba, encephalitis, stem cell transplantation
INTRODUCTION
Encephalitis is defined by acute inflammation of the brain, which may be attributed to an immunological or infectious process.[17,18] In particular, virus and bacteria predominantly constitute the infectious etiologies, being the culprit for up to 90% of cases; on the other hand, ameba rarely causes infectious encephalitis.[7] Free-living ameba may induce 2 different forms of encephalitis: Primary amebic meningoencephalitis and granulomatous amebic encephalitis (GAE).[19] The former, characteristically caused by Naegleria fowleri, follows an acute, severe, and rapid clinical deterioration to coma, and death in several days.[19] The latter, generally associated with Acanthamoeba spp., Balamuthia mandrillaris, or Sappinia pedata, exhibits a subacute or chronic decline, ultimately also leading to death.[12] Accurate diagnosis demands high clinical vigilance and proper laboratory testing.[12] Radiology studies tend to produce nonspecific findings such as necrosis, multifocal lesions, pseudotumoral masses, hemorrhagic infarcts, and variable enhancement.[16]
GAE has been documented predominantly among the immunocompromised population or among those with chronic disease.[5] On the other hand, there have only been eight cases regarding the infection following hematopoietic stem cell transplantation (HSCT).[1,2,3,4,5,9,13] We report another patient who succumbed to the infection following peripheral blood autologous stem cell transplantation. The symptoms began 15 days after transplantation, which was significantly earlier compared to prior literature (69–215 days);[1,2,3,4,5,9,13] this short time frame after transplantation highlights the need for high clinical suspicion of this pathology in this patient population for accurate diagnosis and timely treatment.
CASE PRESENTATION
Patient is a 62-year-old female with history of relapsed diffuse large B-cell lymphoma (initially diagnosed 4 years ago s/p 6 cycles of R-CHOP followed by remission, with relapse 4 months ago s/p 3 cycles of RICE) who had recently underwent peripheral blood autologous stem cell transplant after BEAM conditioning (BiCNU, etoposide, Ara-c, melphalan). This was complicated by a neutropenic fever and hypotension, requiring Intensive Care Unit observation. An infectious work-up was negative, and the patient was discharged on day +11 with evidence of peripheral count engraftment.
On day +15, she began to exhibit worsening fatigue, generalized weakness, and fever up to 100.9F. She was evaluated in the emergency department (ED), where subsequent chest X-ray, blood cultures, and urinalysis did not show any evidence of infection. Symptoms progressed to nausea, emesis, somnolence, confusion, and frontal headaches over the next few days. On day +18, the patient returned to the ED. The patient denied changes with vision, slurred speech, focal weakness, paresthesias, photo/phonophobia, or neck stiffness. A computed tomography (CT) head showed ill-defined hypodense areas with surrounding vasogenic edema in the right frontal lobe with subtle mass effect and effacement of the right frontal horn with similar ill-defined hypoattenuation in the left peri-atrial region and right temporal horn [Figure 1a]. Magnetic resonance imaging of the brain with or without contrast was performed revealing multiple ill-defined lesions concerning for infectious etiology, inflammatory reaction, fungal disease, or neoplasm [Figure 2a–d]. Cerebrospinal fluid was remarkable for the markedly elevated white blood cell count with neutrophil predominance, high protein, and normal glucose.
Figure 1.
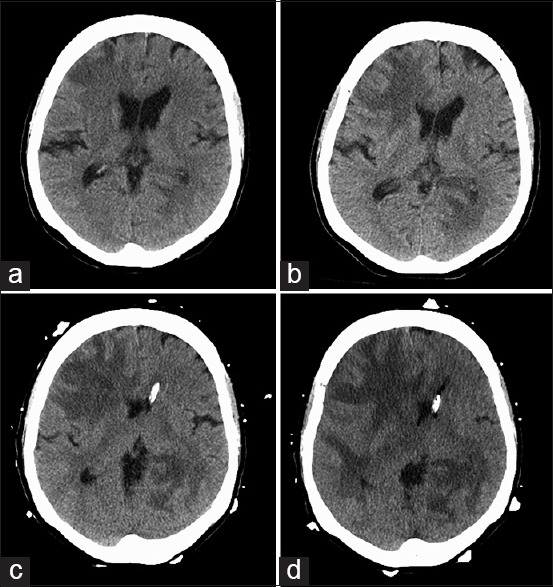
(a-d) Serial computed tomography demonstrates progressive cerebral edema
Figure 2.
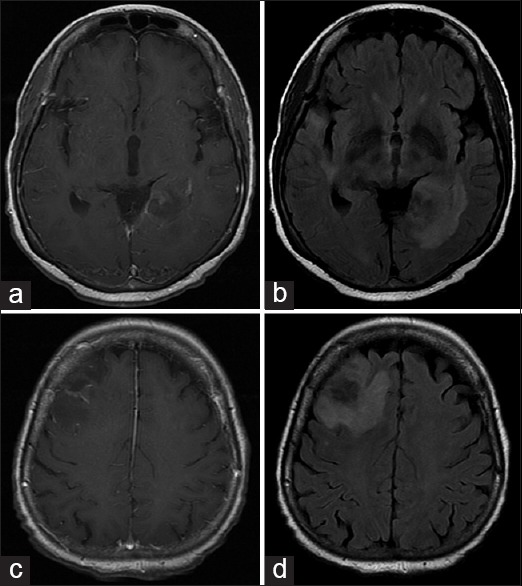
Magnetic resonance imaging brain T1 with contrast (a and c) and fluid-attenuated inversion recovery (b and d) demonstrates multifocal, patchy enhancing lesions at right frontal and left periatrial regions
The patient was started on broad antibiotics, antifungals, and seizure prophylaxis. Evaluation for bacterial, fungal, mycobacterial, and viral etiologies was fruitless. Her mental status progressively deteriorated, but she was able to follow simple commands with effort. On day +22, she exhibited severe lethargy followed by pulseless electrical activity arrest, requiring chest compressions. The episode lasted <2 min and her pulse was restored. Two hours later, she exhibited seizure-like activity, which ultimately required emergent intubation for airway protection. A repeat CT head was stable [Figure 1b]. Given the dramatic clinical decline and the possibility of elevated intracranial pressures, an external ventricular drain was placed and the opening pressure was 7 cm of water. Subsequently, she was taken to the operating room for brain biopsy, where a postoperative CT head demonstrates persistent edema [Figure 1c]. Postoperatively, her right pupil began to dilate compared to the left; she demonstrated extensor posturing in her upper extremities and withdrawal in her lower extremities. Repeat CT head revealed increased edema from the right frontal and temporal lesions [Figure 1d]. Given poor prognosis and poor neurological exam, the family opted for withdrawal of care. Final pathology revealed a damaged vessel within necrotic brain parenchyma with occasional amebic organisms identified among polymorphonuclear leukocytes [Figure 3a and b] consistent with GAE. Samples submitted to Centers for Disease Control and Prevention were positive for Acanthamoeba on indirect immunofluorescence and real-time polymerase chain reaction.
Figure 3.
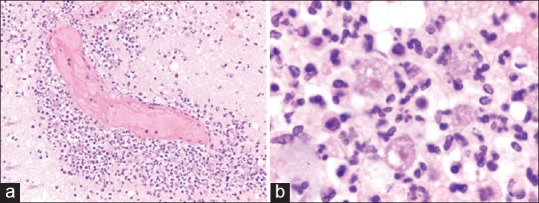
(a) A damaged vessel within necrotic brain parenchyma with occasional amebic trophozoites identified among polymorphonuclear leukocytes (b) high magnification demonstrates amebic trophozoites
DISCUSSION
Acanthamoeba is a type of free-living ameba that often resides in soil, air, or water environments.[10] Most people have encountered this ameba through daily living, as many asymptomatic, healthy people possess serum antibodies against Acanthamoeba.[10] For immunocompetent individuals, Acanthamoeba is typically associated with keratitis after contact lens use or after minor corneal trauma.[11] For immunocompromised individuals, the ameba can impose a disseminated infection, spreading to the skin, sinuses, and lungs.[11] Furthermore, Acanthamoeba may involve the central nervous system, manifesting as GAE, which proceeds along a subacute or chronic timeline.[11] Prior reported patients had various associated conditions, including AIDS, systemic lupus erythematous disease, steroid use, malnutrition, liver disease, renal disease, connective tissue disorder, tuberculosis, history of radiation therapy, and history of chemotherapy.[5] Despite its subtle onset, GAE is predominantly lethal and frequently diagnosed postmortem.[14] For rare occasions with premortem diagnosis, early treatments have resulted in good outcomes.[6,8,11,15]
Including this case, there have been nine reported patients with GAE following HSCT, six allogeneic HSCT recipients, and three autologous HSCT recipients.[1,2,3,4,5,9,13] Such a quantity is too small for significant analysis. In general, allogeneic recipients are more susceptible to infection; the higher number may partly be explained by this reasoning. In their extensive review of the eight prior patients, Akpek et al.[2] noted that seven out of eight patients underwent a prolonged course of steroids, while seven out of eight patients exhibited prior respiratory tract infections (including sinusitis, chronic rhinitis, and pneumonia); consequently, the authors believed that the nasal mucosa may be the most common route for infection. Onset of symptoms has ranged between 69 and 215 days while time to death after the most recent admission has ranged between 7 days and 6 weeks.[2] Our patient exhibited general fatigue and fever, but did not have any respiratory complaints. More dramatically, she exhibited symptoms only 15 days after HSCT and died after 8 days of hospitalization. Given the short time frame from transplantation to infection, significantly compared to prior cases, there is a possibility that she may have harbored the organism at the time of transplantation.
CONCLUSION
The authors reported the third case of GAE after autologous stem cell transplant, and the ninth case overall after HSCT. This case is unusual due to its rapid clinical presentation after HSCT compared to prior literature. The case highlights the need for high suspicion of Acanthamoeba infection in this patient population, especially with the common prevalence of the organism in the environment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Ninh Doan, Email: ndoan@mcw.edu.
Gregory Rozansky, Email: grozansky@mcw.edu.
Ha Son Nguyen, Email: hsnguyen@mcw.edu.
Michael Gelsomino, Email: mgelsomino@mcw.edu.
Saman Shabani, Email: sshabani@mcw.edu.
Wade Mueller, Email: wmueller@mcw.edu.
Vijay Johnson, Email: vijohnson@mcw.edu.
REFERENCES
- 1.Abd H, Saeed A, Jalal S, Bekassy AN, Sandström G. Ante mortem diagnosis of amoebic encephalitis in a haematopoietic stem cell transplanted patient. Scand J Infect Dis. 2009;41:619–22. doi: 10.1080/00365540903015117. [DOI] [PubMed] [Google Scholar]
- 2.Akpek G, Uslu A, Huebner T, Taner A, Rapoport AP, Gojo I, et al. Granulomatous amebic encephalitis: An under-recognized cause of infectious mortality after hematopoietic stem cell transplantation. Transpl Infect Dis. 2011;13:366–73. doi: 10.1111/j.1399-3062.2011.00612.x. [DOI] [PubMed] [Google Scholar]
- 3.Anderlini P, Przepiorka D, Luna M, Langford L, Andreeff M, Claxton D, et al. Acanthamoeba meningoencephalitis after bone marrow transplantation. Bone Marrow Transplant. 1994;14:459–61. [PubMed] [Google Scholar]
- 4.Castellano-Sanchez A, Popp AC, Nolte FS, Visvesvara GS, Thigpen M, Redei I, et al. Acanthamoeba castellani encephalitis following partially mismatched related donor peripheral stem cell transplantation. Transpl Infect Dis. 2003;5:191–4. doi: 10.1111/j.1399-3062.2003.00029.x. [DOI] [PubMed] [Google Scholar]
- 5.Feingold JM, Abraham J, Bilgrami S, Ngo N, Visvesara GS, Edwards RL, et al. Acanthamoeba meningoencephalitis following autologous peripheral stem cell transplantation. Bone Marrow Transplant. 1998;22:297–300. doi: 10.1038/sj.bmt.1701320. [DOI] [PubMed] [Google Scholar]
- 6.Fung KT, Dhillon AP, McLaughlin JE, Lucas SB, Davidson B, Rolles K, et al. Cure of Acanthamoeba cerebral abscess in a liver transplant patient. Liver Transpl. 2008;14:308–12. doi: 10.1002/lt.21409. [DOI] [PubMed] [Google Scholar]
- 7.Glaser CA, Honarmand S, Anderson LJ, Schnurr DP, Forghani B, Cossen CK, et al. Beyond viruses: Clinical profiles and etiologies associated with encephalitis. Clin Infect Dis. 2006;43:1565–77. doi: 10.1086/509330. [DOI] [PubMed] [Google Scholar]
- 8.Gupta D, Panda GS, Bakhshi S. Successful treatment of Acanthamoeba meningoencephalitis during induction therapy of childhood acute lymphoblastic leukemia. Pediatr Blood Cancer. 2008;50:1292–3. doi: 10.1002/pbc.21477. [DOI] [PubMed] [Google Scholar]
- 9.Kaul DR, Lowe L, Visvesvara GS, Farmen S, Khaled YA, Yanik GA. Acanthamoeba infection in a patient with chronic graft-versus-host disease occurring during treatment with voriconazole. Transpl Infect Dis. 2008;10:437–41. doi: 10.1111/j.1399-3062.2008.00335.x. [DOI] [PubMed] [Google Scholar]
- 10.Marciano-Cabral F, Cabral G. Acanthamoeba spp. as agents of disease in humans. Clin Microbiol Rev. 2003;16:273–307. doi: 10.1128/CMR.16.2.273-307.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maritschnegg P, Sovinz P, Lackner H, Benesch M, Nebl A, Schwinger W, et al. Granulomatous amebic encephalitis in a child with acute lymphoblastic leukemia successfully treated with multimodal antimicrobial therapy and hyperbaric oxygen. J Clin Microbiol. 2011;49:446–8. doi: 10.1128/JCM.01456-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parija SC, Dinoop K, Venugopal H. Management of granulomatous amebic encephalitis: Laboratory diagnosis and treatment. Trop Parasitol. 2015;5:23–8. doi: 10.4103/2229-5070.149889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pemán J, Jarque I, Frasquet J, Alberola C, Salavert M, Sanz J, et al. Unexpected postmortem diagnosis of Acanthamoeba meningoencephalitis following allogeneic peripheral blood stem cell transplantation. Am J Transplant. 2008;8:1562–6. doi: 10.1111/j.1600-6143.2008.02270.x. [DOI] [PubMed] [Google Scholar]
- 14.Satlin MJ, Graham JK, Visvesvara GS, Mena H, Marks KM, Saal SD, et al. Fulminant and fatal encephalitis caused by Acanthamoeba in a kidney transplant recipient: Case report and literature review. Transpl Infect Dis. 2013;15:619–26. doi: 10.1111/tid.12131. [DOI] [PubMed] [Google Scholar]
- 15.Seijo Martinez M, Gonzalez-Mediero G, Santiago P, Rodriguez De Lope A, Diz J, Conde C, et al. Granulomatous amebic encephalitis in a patient with AIDS: Isolation of Acanthamoeba sp. Group II from brain tissue and successful treatment with sulfadiazine and fluconazole. J Clin Microbiol. 2000;38:3892–5. doi: 10.1128/jcm.38.10.3892-3895.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh P, Kochhar R, Vashishta RK, Khandelwal N, Prabhakar S, Mohindra S, et al. Amebic meningoencephalitis: Spectrum of imaging findings. AJNR Am J Neuroradiol. 2006;27:1217–21. [PMC free article] [PubMed] [Google Scholar]
- 17.Stahl JP, Mailles A. What is new about epidemiology of acute infectious encephalitis? Curr Opin Neurol. 2014;27:337–41. doi: 10.1097/WCO.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 18.Venkatesan A, Benavides DR. Autoimmune encephalitis and its relation to infection. Curr Neurol Neurosci Rep. 2015;15:3. doi: 10.1007/s11910-015-0529-1. [DOI] [PubMed] [Google Scholar]
- 19.Visvesvara GS. Infections with free-living amebae. Handb Clin Neurol. 2013;114:153–68. doi: 10.1016/B978-0-444-53490-3.00010-8. [DOI] [PubMed] [Google Scholar]


