Supplemental Digital Content is available in the text.
Keywords: diagnosis, tuberculosis, culture, children, symptoms
Abstract
Background:
Childhood tuberculosis (TB) is usually Mycobacterium tuberculosis (MTB) culture negative. Furthermore, clinical presentation may be altered by active case finding, isoniazid prophylaxis and early treatment. We aimed to establish the value of presenting symptoms for intrathoracic TB case diagnosis among young children.
Methods:
Healthy, HIV-uninfected, South African infants in an efficacy trial of a novel TB vaccine (MVA85A) were followed for 2 years for suspected TB. When suspected, investigation followed a standardized algorithm comprising symptom history, QuantiFERON Gold-in-Tube, chest radiography (CXR), MTB culture and Xpert MTB/RIF from paired gastric lavage and induced sputa. Adjusted odds ratios and 95% confidence intervals describe the associations between symptoms and positive MTB culture or Xpert MTB/RIF, and CXR compatible with intrathoracic TB.
Results:
Persistent cough was present in 172/1017 (16.9%) of the children investigated for TB. MTB culture/Xpert MTB/RIF was positive in 38/1017 children (3.7%); and CXR was positive, that is, compatible with intrathoracic TB, in 131/1017 children (12.9%). Children with persistent cough had more than triple the odds of a positive MTB culture/Xpert MTB/RIF (adjusted odds ratios: 3.3, 95% confidence interval: 1.5–7.0) and positive CXR (adjusted odds ratios: 3.5, 95% confidence interval: 2.2–5.5). Persistent cough was the only symptom that differentiated children with severe (56.5%) from nonsevere intrathoracic TB disease (28.2%; P = 0.001).
Conclusion:
Persistent cough was the cardinal diagnostic symptom associated with microbiologic and radiologic evidence, and disease severity, of intrathoracic TB. Symptom-based definitions of TB disease for diagnostic, preventive and therapeutic studies should prioritize persistent cough above other symptoms compatible with childhood TB.
Globally, an estimated half a million children develop tuberculosis (TB) annually, contributing approximately 6%–10% of all TB cases. About 80,000 of these children die every year, making TB one of the major causes of mortality in children younger than 5 years.1,2 Clinical trials of new TB vaccines in infants are planned to coincide with peak childhood TB incidence, and highest risk of severe morbidity and mortality, as these occur during the first 2 years of life.3,4 For this reason, accurate diagnosis of TB in these very young children is critical for diagnostic, preventive and therapeutic studies.
Childhood TB lacks definitive diagnostic criteria.5 The diagnosis of childhood TB is particularly difficult because TB disease in young children is pauci-bacillary and usually culture negative.6 A recent expert consensus statement recommends the following clinical case definitions for confirmed, probable and possible intrathoracic TB in clinical research to evaluate diagnostic assays: signs and symptoms suggestive of TB plus microbiologic confirmation for confirmed TB; signs and symptoms suggestive of TB plus a positive CXR, in addition to either (1) a positive response to anti-TB treatment or (2) documented exposure to Mycobacterium tuberculosis (MTB) or (3) immunologic evidence of MTB infection, for probable TB; and signs and symptoms suggestive of TB with either (1) a positive CXR or (2) a positive response to anti-TB treatment or (3) documented exposure to MTB or (4) immunologic evidence of MTB infection, for possible TB.7 However, in TB-endemic countries, symptoms associated with TB frequently occur in association with other common childhood illnesses, and this lack of specificity may limit their diagnostic usefulness.8,9 In addition, in children younger than 3 years of age, rapid progression of disease to severe forms, such as miliary TB or TB meningitis, may shorten the period for detection of classic respiratory symptoms, and thus limit the opportunity for respiratory symptom-based diagnosis.8 We have previously shown that clinical response to treatment may have limited value as a diagnostic criterion for pediatric trials of TB diagnostics and vaccines,10 and chest radiographic features of intrathoracic TB may be difficult to interpret.11 The diagnosis of childhood TB in the setting of clinical trials is further complicated by active TB disease surveillance, isoniazid preventive therapy, and effective short-course chemotherapy.12 Therefore, the phenotype of TB cases in such research settings is likely to represent early, mild disease that is associated with higher diagnostic uncertainty,11,12 and might not reflect the typical phenotype of TB disease occurring in communities where routine health service interventions are less efficient.6,11,13 In particular, the symptom profile of TB cases is likely to be affected, along with altered radiologic disease severity and sputum bacillary burden.6
Our hypothesis was that classic respiratory symptoms, including persistent cough and wheeze, are not useful for diagnosis of the mild TB disease phenotype that would be observed most often in a clinical trial setting. Detailed understanding of the relationship between individual symptoms, including cough and wheeze, and both culture confirmation of MTB (the current diagnostic gold standard) and radiologic evidence of intrathoracic TB, will be key to design of diagnostic endpoints for accurate diagnosis of pediatric childhood TB in future trials. We present an analysis of the relationships between individual symptoms and these microbiologic and radiologic diagnostic criteria; we examine the usefulness of individual symptoms for diagnosis of TB disease and for differentiating between severe and nonsevere intrathoracic TB disease, in the setting of a clinical trial.
MATERIALS AND METHODS
This analysis is based on diagnostic data from a Phase 2b, double-blind, randomized, controlled trial for evaluation of safety, immunogenicity, and prevention of TB with the novel TB vaccine MVA85A, in BCG-vaccinated, HIV-negative infants.14 The clinical trial was approved by the University of Cape Town Faculty Of Health Sciences Human Research Ethics Committee, and registered with the South African National Clinical Trials Register (DOH-27-0109-2654) as well as with ClinicalTrials.gov (NCT00953927). Written informed consent was obtained from mothers for infant participation. The study was conducted from July 2009 to October 2012, in the Western Cape Province of South Africa, where the incidence of TB disease in children younger than 2 years is estimated at 3000 per 100,000.15,16 The methodology and main results have been reported previously.14 In brief, healthy, BCG-vaccinated, HIV-uninfected infants were randomized at age 18–22 weeks to receive either the candidate TB vaccine MVA85A or placebo. Thereafter, infants were actively followed up for incident TB disease for a median of 24 months. Infants were assessed and weighed at study days 0, 7, 28, 84, and every 84 days thereafter. A QuantiFERON Gold-in-Tube (QFT; Cellestis, Melbourne, Australia) test was done at screening, again on study day 336 and on the last scheduled visit for each infant. Infants with a cohabiting household member with a new TB diagnosis; or weight loss, or failure to thrive (crossing growth chart centiles) in the last 2 months; or persistent cough for longer than 2 weeks; or known conversion to a positive QFT or TST were actively investigated.
The 1017 children admitted to a TB case verification ward for standardized evaluation of suspected TB disease during the period July 2009 to October 2012 are included in this analysis, for which additional approval was granted by the University of Cape Town Faculty Of Health Sciences Human Research Ethics Committee (UCT HREC Reference 563/2013). Standardized investigation included TB contact and symptom history, liquid mycobacterial culture (MGIT, Becton-Dickinson, USA) and Xpert MTB/RIF (Cepheid, Franklin Lakes, NJ), 2 paired induced sputum and gastric lavage samples, TB infection status (QFT) and chest radiography. Chest radiographs (CXR) were reviewed by 3 independent pediatric radiologists blinded to the clinical data, for radiographic features compatible with a diagnosis of intrathoracic TB. Concordance between at least 2 reviewers classified the radiological diagnosis as either CXR positive (compatible with TB) or CXR negative (not compatible with TB). A positive CXR was defined as having any one of the following features: airway compression, Ghon focus, mediastinal lymphadenopathy, pleural effusion, airspace opacification, nodular picture (bilateral miliary nodules), cavitation observed in the same anatomical position by 2 or more expert radiology reviewers. For the purposes of this analysis, the composite microbiological TB disease endpoint included either a positive MGIT culture or positive Xpert MTB/RIF. Severe intrathoracic TB disease was defined, according to Wiseman et al,17 as a positive CXR with any 1 of the following features: airway compression, multilobar airspace opacification, nodular picture (bilateral miliary nodules) or cavitation. Nonsevere intrathoracic TB disease included all other positive CXR cases, including any combination of the following features: Ghon focus, isolated hilar lymphadenopathy or pleural effusion.17
Statistical analyses were performed using Stata/IC 11 (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX: StataCorp LP). Univariate logistic regression models were used to quantify the associations between each of the risk factors and the dependent variables, culture and CXR. Separate multivariate logistic regression models were built to identify symptoms with the strongest independent association with positive culture and CXR, after adjusting for other covariates. To compare the differences in symptoms (and other covariates) between children with severe and nonsevere intrathoracic TB disease, and between children with and without persistent cough, we calculated the 95% confidence interval for the difference between 2 population proportions. We calculated sensitivity, specificity and positive and negative predictive values of individual symptoms for positive culture and CXR-dependent variables.
RESULTS
A total of 2797 infants were enrolled in the parent trial, of which 1017 (36.4%), who were investigated for incident TB over a median of 24 months follow-up, form the basis of this analysis. The mean age at investigation was 19.2 months (standard deviation ± 7.4) and mean weight-for-age Z score −0.9 (standard deviation ± 1.2).
Of the 1017 children investigated for incident TB, 476 children (46.8%) were male; 38 children (3.7%) had a positive culture for MTB or positive Xpert MTB/RIF, and 131 children (12.9%) had a chest radiograph suggestive of intrathoracic TB. Six hundred and fifty-five (64.4%) children presented with at least 1 symptom (ie, were classified as symptomatic), of which the most common symptom was failure to thrive (508 children; 50%). Other symptoms included a persistent nonremitting cough in 172 children (16.9%), loss of appetite in 181 (17.8%), wheezing in 128 (12.6%), loss of weight in 32 (3.1%), fever in 21 (2.1%) and lethargy in 12 (1.2%) of the investigated children. Conversion to positive QFT was observed in 228 children (22.4%) and a household TB contact was reported in 329 children (32.6%).
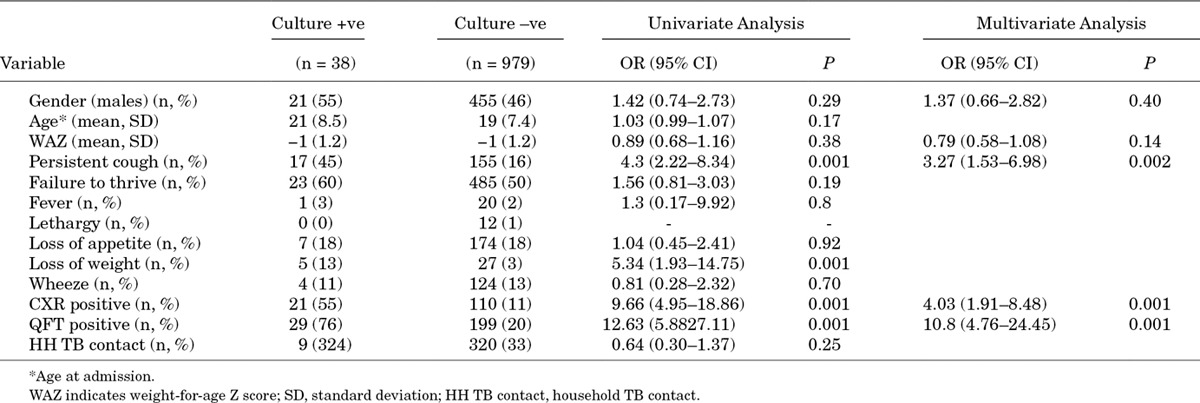
Children with positive MTB culture/Xpert MTB/RIF were more likely to have had a persistent cough (AOR: 3.3), a positive QFT result (AOR: 10.8) and a CXR compatible with intrathoracic TB (AOR: 4.0) compared with those children without positive MTB culture. Other symptoms, including persistent wheeze, fever, failure to thrive, loss of weight, lethargy and loss of appetite, were not independently associated with positive MTB culture (Table 1).
TABLE 1.
Univariate and Multivariate Models of Demographic, Symptom, and Other Diagnostic Variables Associated with Mycobacterium Tuberculosis (MTB) Culture-positive Intrathoracic TB
Of the 38 children with a positive culture for MTB or Xpert MTB/RIF, 1 child (2.6%) had only CXR compatible with severe intrathoracic TB, 4 children (10.5%) had symptoms only and 6 children (15.8%) were TB exposed only (ie, QFT positive or household contact); and 1 child (2.6%) was asymptomatic and unexposed. There were 3 children (7.9%) with TB exposure and a CXR compatible with nonsevere TB, 2 children (5.3%) with symptoms and a CXR compatible with severe TB, 6 children (15.8%) with symptoms and TB exposure, 5 children (13.2%) with symptoms, exposure and a CXR compatible with severe TB and 10 (26.3%) children with symptoms, TB exposure and a CXR compatible with nonsevere TB.
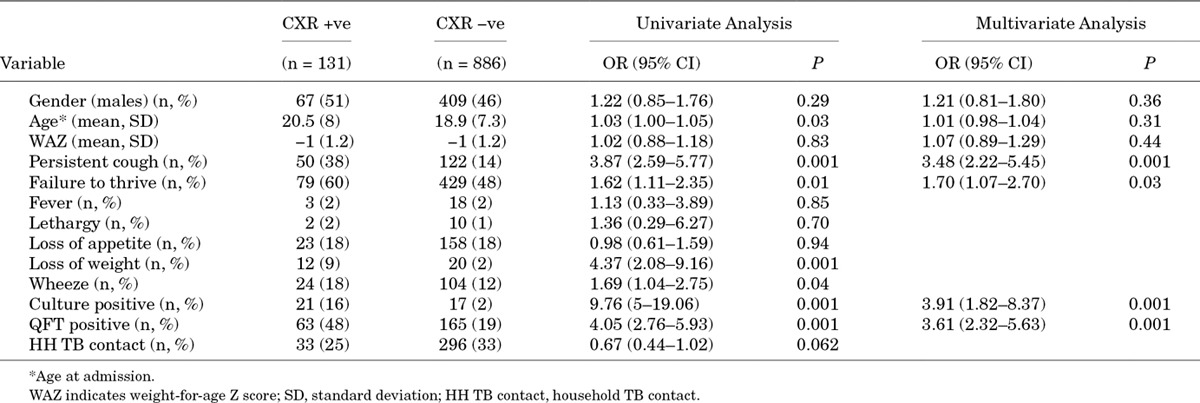
Children with a CXR compatible with intrathoracic TB were more likely to have had persistent cough (AOR: 3.5) and failure to thrive (AOR: 1.7), as well as positive QFT result (AOR: 3.6) and positive MTB culture (AOR: 3.9), compared with children without a CXR compatible with intrathoracic TB (Table 2).
TABLE 2.
Univariate and Multivariate Models of Demographic, Symptom, and Other Diagnostic Variables Associated with a CXR Compatible with Intrathoracic TB
Of the 131 children with a CXR compatible with intrathoracic TB, 7 children (5.4%) were asymptomatic and TB unexposed, 3 children had a CXR (2.3%) compatible with severe TB and 4 children had a CXR (3.1%) compatible with nonsevere TB. Eighteen children (13.8%) were TB exposed only, with 4 (3.1%) and 14 (10.7%) children with CXRs compatible with severe and nonsevere TB, respectively. Forty-three children (32.8%) were symptomatic only, with 13 children (9.9%) having a CXR compatible with severe TB and 30 children (22.9%) having a CXR compatible with nonsevere TB. Forty-two of the 131 children (32.1%) were both symptomatic and TB exposed, with 13.7% (n = 18) and 18.3% (n = 24) having a CXR compatible with severe and nonsevere TB, respectively. There were 21 children (16.0%) with a positive CXR and a positive culture for MTB, of which 1 child (0.8%) had severe TB on CXR, but was neither symptomatic nor TB exposed; 3 children (2.3%) were TB exposed only with nonsevere TB on CXR; 2 children (1.5%) were symptomatic only with severe TB on CXR; 5 children (3.8%) were both symptomatic and TB exposed with severe TB on CXR; and the remaining 10 children (7.6%) were both symptomatic and TB exposed with nonsevere TB on CXR (Fig., Supplemental Digital Content 1, http://links.lww.com/INF/C217).
Persistent cough was the only diagnostic variable that distinguished severity of TB disease, being twice as common in severe TB compared with nonsevere intrathoracic TB (56.5% vs. 28.2%; P = 0.001). The demographic features, symptom profile and other diagnostic variables for children with and without severe intrathoracic TB disease, as per the classification of Wiseman et al (2012), are shown in Table, Supplemental Digital Content 2, http://links.lww.com/INF/C218.
Children with and without persistent cough are compared in Table 3. Other common symptoms of childhood TB disease, as well as radiographic and microbiological evidence of TB, were more common in children with persistent cough than among those without persistent cough.
TABLE 3.
Comparison of Demographic, Clinical and Microbiological Features Between Children With and Without Persistent Cough
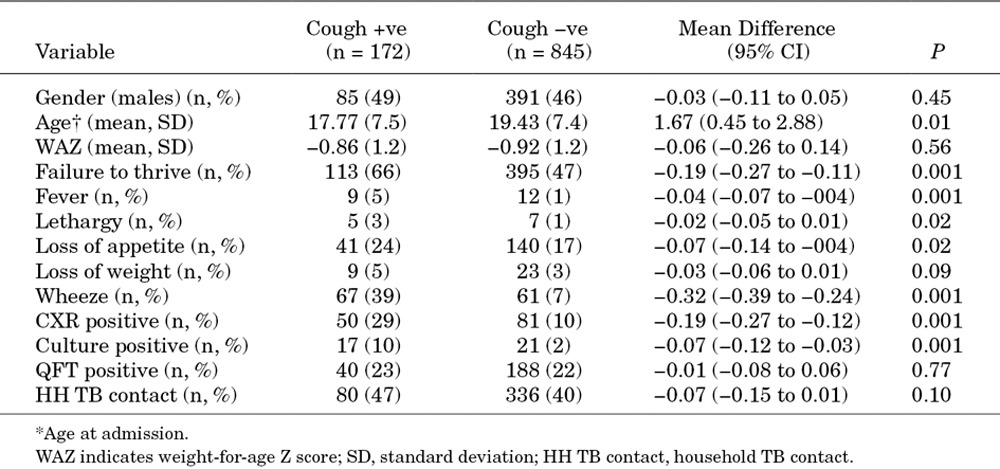
Figure 1A shows the diagnostic sensitivity and specificity of the individual typical TB symptoms for MTB culture/Xpert MTB/RIF—the current gold standard for diagnosis of TB. Persistent cough had relatively good diagnostic sensitivity and specificity compared with other symptoms. Figure 1B presents the sensitivity and specificity of cough, QFT, CXR and their various combinations for positive MTB culture. The clinical triad of cough, QFT and CXR was highly specific, but poorly sensitive.
FIGURE 1.
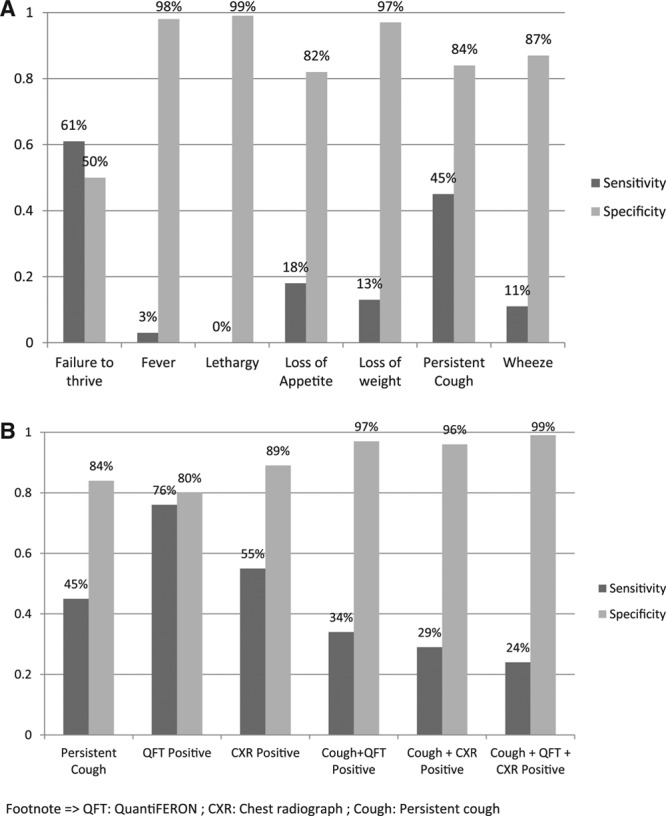
Sensitivity and specificity of (A) individual symptoms for positive MTB culture (B) persistent cough, quantiFERON and chest x-ray for positive MTB culture.
DISCUSSION
We have shown that in a cohort of young, HIV uninfected, BCG vaccinated, South African children who were actively followed for incident TB disease and investigated under standardized research conditions (1) persistent cough was the only symptom independently associated with both microbiological and radiological evidence of intrathoracic TB, (2) persistent cough differentiated children with severe intrathoracic TB from those with nonsevere intrathoracic TB disease, yet (3) if persistent cough were used as a screening test, more than half of MGIT culture-confirmed intrathoracic TB cases would have been missed; and furthermore, if combined with QFT and CXR to improve diagnostic specificity, more than 3 quarters of TB cases would have been missed.
Despite these considerable shortcomings, persistent cough was the most useful of several possible symptoms for inclusion in the diagnostic approach to childhood TB. Children with persistent cough had more than 3 times the odds of a positive MTB culture or a CXR consistent with intrathoracic TB. Furthermore, in the model of positive MTB culture, persistent cough was the only symptom independently associated with microbiological confirmation of disease. This finding contrasts with earlier reports among young children in a TB vaccine trial setting,18,19 in which persistent cough was not associated with microbiological evidence of TB. This difference may be attributed to the fact that children in these earlier studies were younger (median age 11 months and 13 months), compared with the children reported here (median age 18 months). It is also possible that cough was better characterized in these older children; or alternatively, the symptom of persistent cough in very young children is less specific for intrathoracic TB due to the high burden of other respiratory illnesses in infancy.
We also showed that persistent cough and failure to thrive were independently associated with radiographic evidence of intrathoracic TB. However, the presence of persistent cough was the only symptom that differentiated intrathoracic disease severity, being twice as common in children with severe TB compared to those with nonsevere TB disease. Finally, children with persistent cough were more likely to demonstrate the spectrum of other clinical features consistent with the typical presentation of childhood TB, namely weight loss, failure to thrive, fever, lethargy, wheezing and a positive QFT, indicative of MTB infection.
Collectively, these findings confirm the pivotal importance of persistent cough for the diagnosis of childhood TB, even in very young children with early mild disease, as recommended by Graham et al and Marais et al.7–9 It is clear that persistent cough is the cardinal symptom that should be included, in preference to other symptoms, in the clinical triad for a composite TB endpoint in future clinical trials of new TB vaccines, diagnostics and drugs in this study population.
We had originally hypothesized, based on previous study in children, that symptoms, including persistent cough, would have limited diagnostic value in this study population.18,19 Indeed, we confirmed that persistent cough has poor sensitivity for positive MTB culture, although superior to other classical diagnostic symptoms, and would not be useful as an isolated screening test. However, when combined with positive QFT and chest radiography, a high specificity of 99% could be achieved, suggesting that almost all children without culture-positive TB could be excluded by the composite endpoint, based on the clinical triad of cough, QFT and chest radiography. However, this highly specific clinical endpoint could only be achieved at the expense of dramatic loss in sensitivity, as we have observed in a recent infant TB vaccine trial,14 in which clinically diagnosed TB cases were outnumbered by MTB culture-confirmed cases.
It is worth noting that children without persistent cough who had radiological evidence of intrathoracic TB were more likely to have nonsevere (mediastinal) disease. It is possible that the clinical consequences of delayed diagnosis in these children would be less severe than for children with more advanced disease. By contrast, the majority of children with severe intrathoracic TB disease demonstrated multilobar airspace opacification, a combination of airway compression and lymphadenopathy, or a combination of airway compression, lymphadenopathy and multilobar airspace opacification. Compressive intrathoracic lymph node disease, which might be expected to have a lower bacillary burden, might explain the low rate of positive MTB cultures observed among children with severe intrathoracic TB (Fig., Supplemental Digital Content 3, http://links.lww.com/INF/C219). It is also noteworthy that in asymptomatic children referred for investigation as a result of either a household TB contact or conversion to positive QFT (n = 202), a positive culture for MTB was observed in 5 children (2.5%), a CXR compatible with TB was observed in 16 children (7.9%) and both a positive culture and a CXR compatible with TB was observed in 3 children (1.5%). This finding reinforces the need to investigate asymptomatic children with known TB exposure (Fig., Supplemental Digital Content 1, http://links.lww.com/INF/C217).
Interpretation of our data is limited by the fact that this study was conducted only in young HIV uninfected children who were under active surveillance for suspected intrathoracic TB. These findings may not apply to older age groups, HIV infected children, or sicker, hospitalized children. This analysis does not include a formal diagnostic classification of TB cases, such as that proposed by Graham et al.7 Rather, we categorized only radiological and microbiological evidence of disease, since inclusion of symptoms, including persistent cough, in the clinical TB case classification would result in a circular, self-referential argument. Finally, we speculate that associations between classical symptoms and TB disease might be stronger in resource-limited settings in high TB burden countries, where health services are less efficient and children present later with more severe disease.
These data support the inclusion of persistent cough, in preference to other symptoms, in the clinical endpoint definition for future diagnostic, vaccine and therapeutic trials. However, it should be noted that although the diagnostic triad of persistent cough, positive QFT and chest radiograph is highly specific for culture-confirmed TB disease, application of this composite endpoint would result in significant under estimation of the total number of TB cases in this study population.
ACKNOWLEDGMENTS
The authors thank the SATVI MVA85A 020 trial study team.
Supplementary Material
Footnotes
Study was funded by Aeras.
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (www.pidj.com).
REFERENCES
- 1.CDC. TB in children (global perspective) 2014. Available at: http://www.cdc.gov/tb/topic/populations/TBinChildren/global.htm. Accessed November 10, 2014. [Google Scholar]
- 2.WHO. Global tuberculosis report 2014. 2014.. Available from: http://www.who.int/tb/publications/factsheet_global.pdf. Accessed November 12, 2014. [Google Scholar]
- 3.Marais BJ, Gie RP, Schaaf HS, et al. The natural history of childhood intra-thoracic tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004;8:392–402. [PubMed] [Google Scholar]
- 4.Marais BJ, Gie RP, Schaaf HS, et al. The clinical epidemiology of childhood pulmonary tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004;8:278–285. [PubMed] [Google Scholar]
- 5.Osborne CM. The challenge of diagnosing childhood tuberculosis in a developing country. Arch Dis Child. 1995;72:369–374. doi: 10.1136/adc.72.4.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mulenga H, Moyo S, Workman L, et al. Phenotypic variability in childhood TB: implications for diagnostic endpoints in tuberculosis vaccine trials. Vaccine. 2011;29:4316–4321. doi: 10.1016/j.vaccine.2011.04.020. [DOI] [PubMed] [Google Scholar]
- 7.Graham SM, Ahmed T, Amanullah F, et al. Evaluation of tuberculosis diagnostics in children: 1. Proposed clinical case definitions for classification of intrathoracic tuberculosis disease. Consensus from an expert panel. J Infect Dis. 2012;205(Suppl 2):S199–S208. doi: 10.1093/infdis/jis008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marais BJ, Gie RP, Hesseling AC, et al. A refined symptom-based approach to diagnose pulmonary tuberculosis in children. Pediatrics. 2006;118:e1350–e1359. doi: 10.1542/peds.2006-0519. [DOI] [PubMed] [Google Scholar]
- 9.Marais BJ, Gie RP, Obihara CC, et al. Well defined symptoms are of value in the diagnosis of childhood pulmonary tuberculosis. Arch Dis Child. 2005;90:1162–1165. doi: 10.1136/adc.2004.070797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mpofu N, Moyo S, Mulenga H, et al. Time to symptom resolution in young children treated for intrathoracic tuberculosis. Pediatr Infect Dis J. 2014;33:1226–1230. doi: 10.1097/INF.0000000000000523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatherill M, Hanslo M, Hawkridge T, et al. Structured approaches for the screening and diagnosis of childhood tuberculosis in a high prevalence region of South Africa. Bull World Health Organ. 2010;88:312–320. doi: 10.2471/BLT.09.062893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hawkridge A, Hatherill M, Little F, et al. South African BCG trial team. Efficacy of percutaneous versus intradermal BCG in the prevention of tuberculosis in South African infants: randomised trial. BMJ. 2008;337:a2052. doi: 10.1136/bmj.a2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hatherill M, Verver S, Mahomed H Taskforce on Clinical Research Issues, Stop TB Partnership Working Group on TB Vaccines. Consensus statement on diagnostic end points for infant tuberculosis vaccine trials. Clin Infect Dis. 2012;54:493–501. doi: 10.1093/cid/cir823. [DOI] [PubMed] [Google Scholar]
- 14.Tameris MD, Hatherill M, Landry BS, et al. MVA85A 020 Trial Study Team. Safety and efficacy of MVA85A, a new tuberculosis vaccine, in infants previously vaccinated with BCG: a randomised, placebo-controlled phase 2b trial. Lancet. 2013;381:1021–1028. doi: 10.1016/S0140-6736(13)60177-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.English R. Boland/Overberg region, annual health status report 2007/08. Available at: http://www.westerncape.gov.za/Text/2009/12/boland_overberg_region_07_08.pdf. Accessed June 15, 2013. [Google Scholar]
- 16.Adams S. Cape winelands &Overberg districts, annual health status report 2008/09. Available at: http://sun025.sun.ac.za/portal/page/portal/Health_Sciences/English/Centres/Rural_Clinical_School/annual_health_report/Annual_Health_Status_Report_2008-2009%20final.pdf. Accessed June 20, 2013. [Google Scholar]
- 17.Wiseman CA, Gie RP, Starke JR, et al. A proposed comprehensive classification of tuberculosis disease severity in children. Pediatr Infect Dis J. 2012;31:347–352. doi: 10.1097/INF.0b013e318243e27b. [DOI] [PubMed] [Google Scholar]
- 18.Luabeya KK, Mulenga H, Moyo S, et al. Diagnostic features associated with culture of Mycobacterium tuberculosis among young children in a vaccine trial setting. Pediatr Infect Dis J. 2012;31:42–46. doi: 10.1097/INF.0b013e31823eeaf9. [DOI] [PubMed] [Google Scholar]
- 19.Hatherill M, Hawkridge T, Zar HJ, et al. Induced sputum or gastric lavage for community-based diagnosis of childhood pulmonary tuberculosis? Arch Dis Child. 2009;94:195–201. doi: 10.1136/adc.2007.136929. [DOI] [PubMed] [Google Scholar]


