Abstract
The survival rate for childhood craniopharyngioma has been improving, with more long-term survivors. Unfortunately it is rare for the patient to be normal, either from the disease itself or from the effects of treatment. Long-term survivors of childhood craniopharyngioma suffer a number of impairments, which include visual loss, endocrinopathy, hypothalamic dysfunction, cerebrovascular problems, neurologic and neurocognitive dysfunction. Pituitary insufficiency is present in almost 100%. Visual and hypothalamic dysfunction is common. There is a high risk of metabolic syndrome and increased risk of cerebrovascular disease, including stroke and Moyamoya syndrome. Cognitive, psychosocial, and emotional problems are prevalent. Finally, there is a higher risk of premature death among survivors of craniopharyngioma, and often this is not from tumor recurrence. It is important to consider craniopharyngioma as a chronic disease. There is no perfect treatment. The treatment has to be tailored to the individual patient to minimize dysfunction caused by tumor and treatments. So “cure” of the tumor does not mean a normal patient. The management of the patient and family needs multidisciplinary evaluation and should involve ophthalmology, endocrinology, neurosurgery, oncology, and psychology. Furthermore, it is also important to address emotional issues and social integration.
Keywords: craniopharyngioma, outcomes, endocrine, cardiovascular, behavioral
Introduction
The survival rate for childhood craniopharyngioma has been improving with more long-term survivors. For example, review of the German Childhood Cancer registry from 1980 to 2007 indicated an improvement in 5-year survival from 91% in the 1980s to 98% in the 1990s and an overall 10-year survival rate of 93%.1)
Unfortunately, it is rare for a patient to be normal, either because of the disease itself or because of the morbidity of the treatment. There are usually combinations of visual impairment, endocrinopathy, hypothalamic dysfunction, cerebrovascular disease, neurologic dysfunction, and neurocognitive dysfunction. This report reviews the current knowledge about the long-term status of patients treated for craniopharyngioma in childhood.
Visual Impairment
Visual acuity or visual field deficits are present in the long-term in approximately 50% to 80% of patients.2–4) For those patients who are diagnosed with craniopharyngioma earlier in childhood, at less than 10 years of age, visual problems are more common.2)
Endocrinopathy
Some form of pituitary insufficiency is present in the vast majority of long-term survivors.5) Panhypopituitarism, defined as absence of at least three anterior pituitary hormones, occurs in 75%–95% of patients treated for craniopharyngioma in childhood.2,3) For patients who are under 10 years of age at the time of diagnosis, panhypopituitarism tends to be present in all.2) Diabetes insipidus is common but depends to some extent on the type of treatment that has been used. For patients in whom a surgical resection of the tumor has been attempted, diabetes insipidus is present in between 70% and 90%, and is present in almost 100% of children who have been operated on for tumor resection at an age less than 10 years.2) When children have been treated solely with intracystic treatment the rate of diabetes insipidus tends to be less.
Physicians often underestimate the significance of the pituitary insufficiency, thinking that it is possible to normalize pituitary function simply by replacing the missing hormones. This is true to a large extent, but patients may not be truly normalized. Typically, in the long-term, patients have decreased fertility, decreased bone density, and an increased rate of metabolic syndrome, reflecting endocrinological dysfunction despite hormone replacement. Obesity and a poor lipid profile, with elevated triglycerides and lower high-density lipoprotein (HDL) cholesterol to total cholesterol ratio, are parts of the metabolic syndrome seen after childhood craniopharyngioma.6,7)
Obesity is present between 4% and 58% of patients at the time of diagnosis, but that increases up to 80% of patients after treatment, especially when the treatment has been with radical surgery.5,8,9) The major factor predicting obesity, both before and after treatment, is hypothalamic involvement by the tumor.8) As a result, based on the initial observations from the group in Paris10) recent protocols often advise against radical surgery when there is clearly hypothalamic invasion.8) In addition to the obesity which is often the most obvious feature of hypothalamic dysfunction and which is associated with hyperphagia, hypothalamic dysfunction may also be characterized by behavioural disturbances, outbursts of anger, apathy, and tiredness. In adults, diagnosed with craniopharngioma in childhood, metabolic syndrome is a very important issue, with a higher incidence of type 2 diabetes, dyslipidemia, obesity, and hypertension. There is an increased cardiovascular risk in adults with childhood onset craniopharyngioma.11) The highest risk of cardiovascular disease is in patients with tumors that were/are in the 3rd ventricle, probably reflecting the adverse impact of hypothalamic involvement.
Cerebrovascular Abnormalities
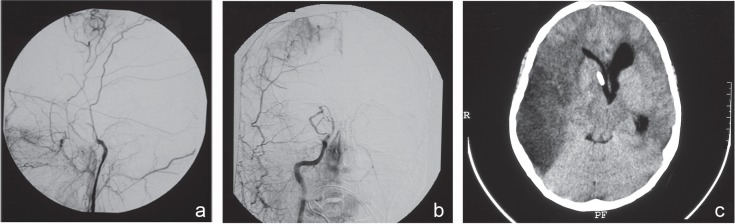
Cerebrovascular abnormalities in the long-term may be related to surgery for or to other treatments of craniopharyngioma, particularly if radiotherapy has been used. As a consequence of surgery for tumor that is adherent to the carotid artery, it is possible to develop a carotid pseudo aneurysm which may or may not require treatment. The long-term effects of radiotherapy for craniopharyngioma in a child include stenosis of the internal carotid artery, middle cerebral artery, anterior cerebral artery, Moyamoya syndrome, stroke, and cavernomas. In a series of 123 adult and pediatric patients with craniopharyngioma treated in Vancouver, Canada, 14 patients experienced a cardiovascular event. In 2, there was a perioperative stroke and in the remaining 12 the events occurred later (3 transient ischemic attacks and 9 strokes).3) In a study of 20 children followed for a median of 4 years, Liu et al. (2009) found 6 patients (30%) with vascular abnormalities.12) These comprised stenosis of the internal carotid or other cerebral arteries in three, carotid aneurysm in one, Moyamoya syndrome in one, and bilateral temporal cavernomas in one. When one looks at Moyamoya syndrome developing after radiotherapy for other tumors, the risk is approximately 0.5% for acute lymphoblastic leukemia and 3.5% for all brain tumors. The risk factors include radiation dose, young age at radiation, and the presence of associated neurofibromatosis type 1. Winkfield et al. (2011), while reporting the experience with childhood craniopharyngioma in Boston, identified Moyamoya syndrome in 4 of 43 patients who had received radiotherapy (9%).9) An example of Moyamoya syndrome in a child with craniopharyngioma is shown in Fig. 1.
Fig. 1.
Moyamoya syndrome. Right common carotid artery injection, lateral projection (a) and AP projection (b) in a 12-year-old child, who had received radiation therapy at 7 years of age for craniopharygioma after failure of intracystic bleomycin treatment. Total occlusion of the distal internal carotid artery is noted with collateral circulation from extracranial vessels going intracranially. This child suffered a severe stroke as shown in the CT scan (c). AP: anteroposterior, CT: computed tomography.
Seizure Disorder
The incidence of seizures in the long-term after management of childhood craniopharyngioma has not received much attention. There are two publications, one by Gautier et al. (2012)2) and another by Winkfield et al. (2011),9) in which seizure disorders are described. Gautier et al. noted 25% of 60 patients with childhood craniopharyngioma had a seizure disorder and Winkfield et al. noted that it was 11% of 79 patients in their series. Even with the lower incidence in the study by Winkfield et al., the incidence of seizures in the long-term is significant. In a combined series of adults and children [including 57 patients (46%) < 21 years], Lo et al. noted seizures in the long-term in 17%.3)
Neurocognitive Problems
Neurocognitive dysfunction in survivors of childhood craniopharyngioma has received significant attention.5,8,13,14) Many studies have indicated that in the long-term there is an absolute decrease in intelligence quotient (IQ) in children who have been treated for craniopharyngioma.14) The risk factors for this decline in IQ include radiation therapy at a young age, an attempted radical resection, and hypothalamic injury. Even in those patients who have a normal IQ, there may be abnormal cognitive function, with impairments of executive function, attention, processing speed, and memory.1,5,8,13–15) Mood disorders, mainly anxiety and depression have commonly been noted in survivors of childhood craniopharyngioma.14) Zada et al. conducted a systematic literature review of studies, in which neurobehavioral, social and emotional outcomes were assessed specifically in children diagnosed with craniopharyngioma.16) They identified 11 studies that met their inclusion criteria. Neurobehavioral abnormalities were present in 51 of 90 patients (57%); emotional dysfunction, primarily depression, in 58 of 146 patients (40%); and school dysfunction in 48 of 136 patients (35%).16)
Quality of Life (QOL)
In studies which have looked specifically at QOL in the long-term after treatment of craniopharyngioma, about 50% overall have a good QOL16) with about 90% having a good QOL when the only treatment has been intracystic treatment. It is interesting that even when the adult survivors of childhood diagnosed craniopharyngioma have significant endocrine and cognitive problems, they often report a normal QOL.13,14) QOL reporting by their proxies, usually parents, tends to be lower.14) Reduced QOL is more apparent in the psychosocial than in the physical dimensions.16) A number of factors are associated with decreased QOL. These include tumor progression or recurrence, multiple surgeries, intraoperative complications, retrochiasmatic tumor, hypothalamic involvement by the tumor, higher body mass index (BMI), a larger tumor, presence of hydrocephalus, and young age of onset.1,14,16,17) Gautier et al. (2012) compared the QOL of patients after treatment of craniopharyngioma with normals and also with patients who had other chronic conditions using the WHO-QOLBREF tool.2) In their physical health dimension, patients with craniopharyngioma function worse than normals, but are about the same as those with other chronic diseases. However, when it came to psychological health and social relationships, patients with prior childhood craniopharyngioma had a reduction in their scores relative not only to normals but to patients with other chronic diseases.
One of the issues that patients with childhood craniopharyngiomas face in later life is decreased sociability and loneliness. Zada et al. reported that social impairment, namely withdrawal and internalizing behavior, was present in 48 of 136 patients (35%) from their literature review.16) Approximately 11% to 25% are in marriage-like relationships and there appears to be decreased fertility in these adults.18,19)
Late mortality
In most of the reports of outcomes, the mortality is reported up to about 10 years, but there is a significant mortality of patients with craniopharyngioma even more than 10 years after diagnosis of the disease. This may be related to tumor recurrence or to a secondary neoplasm if radiotherapy had been used. The risk of a second neoplasm after radiotherapy is usually quoted at about 2% to 3% risk of malignant neoplasm in 20 years after therapy. In the experience in Boston with a median follow-up of 9 years (range 1–30 years), 4 of 43 (9%) of patients with radiotherapy had second neoplasms.9) One of these was a malignancy at 8 years and three were benign tumors all presenting at more than 10 years after treatment. In addition to neoplastic disease, there are a number of other reasons for late mortality that are not so obvious. Visser et al. (2010) reported on 17 patients with craniopharyngioma diagnosed in childhood, who were followed for more than 10 years.20) After 10 years there were 4 deaths among these 17 patients, and none of them were from tumor growth. Between 16 years and 25 years after diagnosis, death occurred because of uncontrolled diabetes insipidus in one, panhypopituitarism resulting in multi organ failure in one, liver failure in one, and a pontine infarct in one. Thus, there appears to be a significantly higher risk of death even after 10 years than the normal population.
Conclusion
In conclusion, craniopharyngioma behaves like and should be considered as a chronic disease. There is no perfect treatment and treatment should be tailored to the individual patient. The goal, as in any other chronic disease process, should be to minimize dysfunction, caused in this case by either the tumor or the treatments for tumor control. Cure of the tumor does not mean a normal patient. The survivors will be abnormal in all cases. Pituitary insufficiency is present in almost 100%. Visual and hypothalamic dysfunction is common. There is a high risk of metabolic syndrome, an increased risk of cerebrovascular disease, cognitive psychosocial and emotional problems, and a higher risk of death even when there is no tumor recurrence.
The management of the patients and their families with craniopharyngioma must be multidisciplinary. At a minimum, this should involve experts in ophthalmology, endocrinology, oncology, and psychology in addition to neurosurgery. It is also important that we start to address emotional issues and social integration in this population of patients.
References
- 1). Müller HL: Childhood craniopharyngioma. Pituitary 16: 56– 67, 2013. [DOI] [PubMed] [Google Scholar]
- 2). Gautier A, Godbout A, Grosheny C, Tejedor I, Coudert M, Courtillot C, Jublanc C, De Kerdanet M, Poirier JY, Riffaud L, Sainte-Rose C, Van Effenterre R, Brassier G, Bonnet F, Touraine P, Craniopharyngioma Study Group : Markers of recurrence and long-term morbidity in craniopharyngioma: a systematic analysis of 171 patients. J Clin Endocrinol Metab 97: 1258– 1267, 2012. [DOI] [PubMed] [Google Scholar]
- 3). Lo AC, Howard AF, Nichol A, Sidhu K, Abdulsatar F, Hasan H, Goddard K: Long-term outcomes and complications in patients with craniopharyngioma: the British Columbia Cancer Agency experience. Int J Radiat Oncol Biol Phys 88: 1011– 1018, 2014. [DOI] [PubMed] [Google Scholar]
- 4). Lin LL, El Naqa I, Leonard JR, Park TS, Hollander AS, Michalski JM, Mansur DB: Long-term outcome in children treated for craniopharyngioma with and without radiotherapy. J Neurosurg Pediatr 1: 126– 130, 2008. [DOI] [PubMed] [Google Scholar]
- 5). Müller HL: Consequences of craniopharyngioma surgery in children. J Clin Endocrinol Metab 96: 1981– 1991, 2011. [DOI] [PubMed] [Google Scholar]
- 6). Profka E, Giavoli C, Bergamaschi S, Ferrante E, Malchiodi E, Sala E, Verrua E, Rodari G, Filopanti M, Beck-Peccoz P, Spada A: Analysis of short- and long-term metabolic effects of growth hormone replacement therapy in adult patients with craniopharyngioma and non-functioning pituitary adenoma. J Endocrinol Invest 38: 413– 420, 2015. [DOI] [PubMed] [Google Scholar]
- 7). Srinivasan S, Ogle GD, Garnett SP, Briody JN, Lee JW, Cowell CT: Features of the metabolic syndrome after childhood craniopharyngioma. J Clin Endocrinol Metab 89: 81– 86, 2004. [DOI] [PubMed] [Google Scholar]
- 8). Puget S: Treatment strategies in childhood craniopharyngioma. Front Endocrinol (Lausanne) 3: 64, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9). Winkfield KM, Tsai HK, Yao X, Larson E, Neuberg D, Pomeroy SL, Ullrich NJ, Cohen LE, Kieran MW, Scott RM, Goumnerova LC, Marcus KJ: Long-term clinical outcomes following treatment of childhood craniopharyngioma. Pediatr Blood Cancer 56: 1120– 1126, 2011. [DOI] [PubMed] [Google Scholar]
- 10). Puget S, Garnett M, Wray A, Grill J, Habrand JL, Bodaert N, Zerah M, Bezerra M, Renier D, Pierre-Kahn A, Sainte-Rose C: Pediatric craniopharyngiomas: classification and treatment according to the degree of hypothalamic involvement. J Neurosurg 106: 3– 12, 2007. [DOI] [PubMed] [Google Scholar]
- 11). Holmer H, Popovic V, Ekman B, Follin C, Siversson AB, Erfurth EM: Hypothalamic involvement and insufficient sex steroid supplementation are associated with low bone mineral density in women with childhood onset craniopharyngioma. Eur J Endocrinol 165: 25– 31, 2011. [DOI] [PubMed] [Google Scholar]
- 12). Liu AK, Bagrosky B, Fenton LZ, Gaspar LE, Handler MH, McNatt SA, Foreman NK: Vascular abnormalities in pediatric craniopharyngioma patients treated with radiation therapy. Pediatr Blood Cancer 52: 227– 230, 2009. [DOI] [PubMed] [Google Scholar]
- 13). Fjalldal S, Holmer H, Rylander L, Elfving M, Ekman B, Osterberg K, Erfurth EM: Hypothalamic involvement predicts cognitive performance and psychosocial health in long-term survivors of childhood craniopharyngioma. J Clin Endocrinol Metab 98: 3253– 3262, 2013. [DOI] [PubMed] [Google Scholar]
- 14). Laffond C, Dellatolas G, Alapetite C, Puget S, Grill J, Habrand JL, Doz F, Chevignard M: Quality-of-life, mood and executive functioning after childhood craniopharyngioma treated with surgery and proton beam therapy. Brain Inj 26: 270– 281, 2012. [DOI] [PubMed] [Google Scholar]
- 15). Özyurt J, Thiel CM, Lorenzen A, Gebhardt U, Calaminus G, Warmuth-Metz M, Müller HL: Neuropsy-chological outcome in patients with childhood craniopharyngioma and hypothalamic involvement. J Pediatr 164: 876–881.e4, 2014. [DOI] [PubMed] [Google Scholar]
- 16). Zada G, Kintz N, Pulido M, Amezcua L: Prevalence of neurobehavioral, social, and emotional dysfunction in patients treated for childhood craniopharyngioma: a systematic literature review. PLoS ONE 8: e76562, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17). Kendall-Taylor P, Jönsson PJ, Abs R, Erfurth EM, Koltowska-Häggström M, Price DA, Verhelst J: The clinical, metabolic and endocrine features and the quality of life in adults with childhood-onset craniopharyngioma compared with adult-onset craniopharyngioma. Eur J Endocrinol 152: 557– 567, 2005. [DOI] [PubMed] [Google Scholar]
- 18). Sääf M, Thorén M, Bergstrand CG, Norén G, Rähn T, Tallstedt L, Backlund EO: Treatment of craniopharyngiomas—the stereotactic approach in a ten to twenty-three years’ perspective. II. Psychosocial situation and pituitary function. Acta Neurochir (Wien) 99: 97–103, 1989. [DOI] [PubMed] [Google Scholar]
- 19). Sterkenburg AS, Hoffmann A, Gebhardt U, Warmuth-Metz M, Daubenbuchel AM, Muller HL: Survival, hypothalamic obesity, and neuropsychological/psychosocial status after childhood-onset craniopharyngioma: newly reported long-term outcomes. Neuro Oncol 17: 1029– 38, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20). Visser J, Hukin J, Sargent M, Steinbok P, Goddard K, Fryer C: Late mortality in pediatric patients with craniopharyngioma. J Neurooncol 100: 105– 111, 2010. [DOI] [PubMed] [Google Scholar]