Abstract
Objectives. We explored the relationship between mental health and type 2 diabetes among women in New Delhi, India, in 2011.
Methods. We recruited a convenience sample of 184 diabetic women from 10 public and private clinics. They completed a finger-stick blood test and a questionnaire assessing demographic characteristics, depression and anxiety symptoms, and diabetes-related disabilities restricting their performance of daily tasks. A subsample of 30 women participated in follow-up qualitative interviews at their homes.
Results. More than one quarter of our sample of diabetic women reported high levels of anxiety symptoms, whereas 18% reported high levels of depression symptoms. Anxiety symptoms were patterned according to recency of diabetes diagnosis, with 40% of women diagnosed less than 2 years before their interview reporting high anxiety symptom levels, as opposed to 23% of women diagnosed more than 2 years in the past. Depression and anxiety scores differed with respect to their relationship to recency of diagnosis, number of children, blood glucose level, and functional disabilities restricting performance of daily tasks.
Conclusions. Screening for anxiety among people with diabetes has been overlooked in the past. Anxiety appears more prevalent than depression, especially during the first 2 years of the disease.
Chronic and noncommunicable diseases (CNCDs) are emerging as major research foci in tandem with their increasing global prevalence. In both developed and developing regions of the world, including South Asia, CNCDs are now leading causes of morbidity and mortality.1 With their complicated etiologies, long durations, frequent comorbidities, and lack of “cures,” CNCDs pose unique challenges for global health. In particular, CNCDs can have far-reaching personal and interpersonal effects that are difficult to capture in epidemiological and biomedical studies, yet are crucial to the trajectory of these illnesses. It is therefore necessary to adopt an analytic perspective that embraces the complex natural histories of chronic diseases as well as their potential comorbidities.
A particularly well-studied instance of comorbidity is the overlap between type 2 diabetes and depression. This comorbidity has been estimated to affect anywhere from 11% to 71% of individuals with diabetes, depending on the population studied and the diagnostic method used,2–4 and it is strongly associated with physical and mental morbidity and even mortality.2–6 Clinical and epidemiological studies have demonstrated the cyclical nature of diabetes–depression comorbidity,7 and medical social scientists have identified some of the social determinants linking the 2 conditions, including socioeconomic status (SES),8 the social significance of foods and activity patterns,9,10 and gendered social roles.11–13
The similarity between depression and anxiety symptoms, etiologies, and methods of diagnosis, as well as their common comorbidity,14 suggests that anxiety should be as great a concern in CNCD comorbidity as depression. Indeed, according to findings from the World Mental Health Survey, diabetes is roughly equally associated with depression and anxiety around the world.15 Yet, with one very recent exception,16 the potential impact of anxiety disorders on diabetes has received much less attention than diabetes–depression comorbidity.
Here we detail the findings of an exploratory mixed-method study of type 2 diabetes (hereafter diabetes) and mental health symptoms among women in New Delhi, India, with a special focus on symptoms of anxiety. India is home to the second-largest population of individuals with type 2 diabetes in the world.17 The limited existing evidence suggests that depression and anxiety are also common,18–20 although prevalence studies are few. Little is known about how diabetes and poor mental health co-occur in this setting or about what social determinants might shape their comorbidity.
On the basis of the observation that high levels of anxiety symptoms were significantly more prevalent than depression symptoms in our study, we believe that it is important to consider the causes and correlates of anxiety comorbid with diabetes. We propose a socially grounded interpretation of the patterns emerging from our preliminary data and offer suggestions for future research designed to assess the broader applicability of this interpretation for CNCD–anxiety comorbidity in other contexts.
METHODS
For this exploratory study, conducted in 2011, we recruited a convenience sample of 184 diabetic women from 10 hospitals and outpatient clinics catering to various socioeconomic groups in New Delhi, India. On random days, the first author and a research assistant visited each clinic and invited women to participate in an interview as they waited to see a physician.
The interviews involved a questionnaire that collected data on demographic characteristics, depression and anxiety symptoms, and disabilities restricting performance of daily tasks. SES was assessed indirectly with a scoring system comprising each woman’s self-reported educational level, caste, employment status (and, if working, type of job), and presence or absence of a maid in the household. Resulting scores were divided into low, middle, and high tertiles for analyses. We employed this type of assessment because women were generally unable or unwilling to report their household’s income.
We used the Hopkins Symptoms Checklist-25, previously validated for use in Hindi-speaking populations, to assess symptoms of depression and anxiety.12 Our scoring method produced a cutoff value of 1.3 or higher indicating clinically significant symptoms of anxiety or depression.13
The questionnaire also included a locally derived instrument designed to measure severity of disability resulting from diabetes in 18 gender-specific tasks that women deemed important; the instrument was developed from free-listing and domain analysis exercises conducted among this population during pilot research in 2009.12,21 The tasks assessed were generally domestic, involving family care and household maintenance,12 and women were asked to indicate whether their diabetes had affected their performance of each of these activities a lot, a little, or not at all. This ranking generated a simple summary score (with a possible range of 0–36) for each woman representing diabetes-related functional disability restricting performance of daily tasks.
Diabetes control was evaluated with finger-stick tests of random blood glucose and glycated hemoglobin (HbA1c). Glucose levels should fall between 70 and 180 milligrams per deciliter, depending on when the person last ate. HbA1c, which indicates blood sugar fluctuations over the past 2 to 3 months, ideally should not exceed 7%.22
We subsequently conducted follow-up qualitative interviews with 30 diabetic women from the initial sample. These women were chosen purposively from a subgroup of women willing to participate in a second interview to represent the widest possible range with respect to religion, caste, age, and number of years living with diabetes. These interviews were conducted at women’s homes in Hindi or English, based on respondent preference. They took about an hour and followed a modified version of Kleinman’s illness narrative interview protocol.23 This protocol focuses on eliciting women’s opinions about why they think they got diabetes and how they feel it has affected their lives. Interviews were recorded, translated, and transcribed for analysis.
We used SPSS version 19 (IBM, Somers, NY) to perform univariate and bivariate statistical analyses as well as linear regressions, via backward elimination, to identify significant predictors of anxiety. These multivariable analyses were stratified into 2 groups according to how long in the past (< 2 years vs ≥ 2 years) women had been diagnosed with diabetes because of the significant difference in anxiety levels between these 2 groups shown in the bivariate analysis, because the qualitative literature on chronic diseases predicts that time since diagnosis moderates illness experiences,24–26 and because we suspected that relationships between predictor variables and the outcome variable, anxiety, might differ between the 2 groups.
We used MaxQDA version 10 (VERBI GmbH, Berlin, Germany) to conduct qualitative analyses on the translated interview transcripts. Coding followed a grounded theory approach involving a multistep process of open coding, axial coding, and identification of relationships between emergent themes.27 The quotations included here, drawn from the coded materials, represent commonly mentioned sentiments.
RESULTS
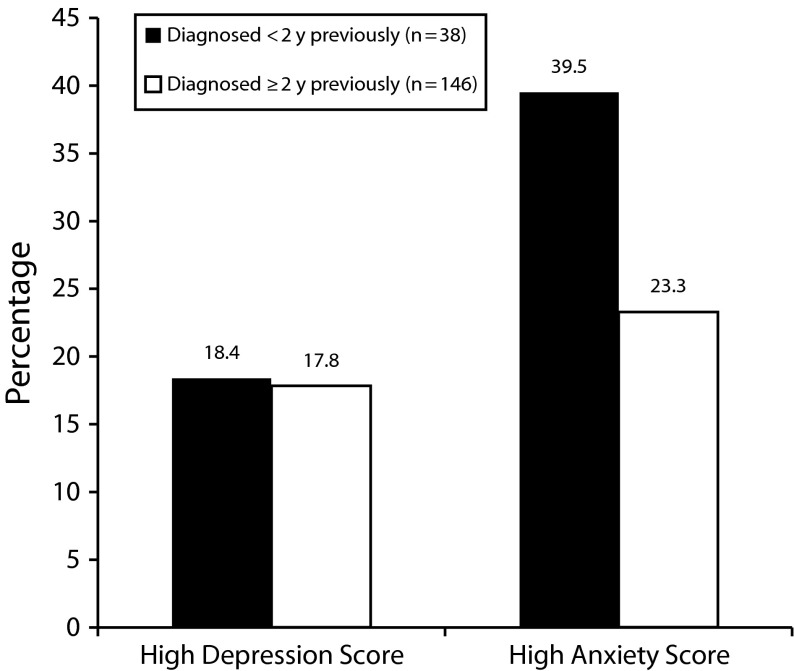
Although both depression and anxiety symptoms were common among the diabetic women in our sample, anxiety symptoms were more widespread. Nearly 19% of the 184 women with diabetes reported levels of depression symptoms suggesting clinically significant disorders, whereas 26.6% reported anxiety symptoms suggesting clinically significant disorders. Fourteen percent had potentially significant levels of both depression and anxiety symptoms. Preliminary analyses indicated that a remarkably higher proportion of women diagnosed more recently (< 2 years before their interview; n = 38) than longer in the past (≥ 2 years before their interview; n = 146) reported significant levels of anxiety symptoms, even though the “veteran” diabetic women tended to have poorer overall physical health (Table 1). In the more recently diagnosed group, 39.5% of women reported a high level of anxiety symptoms, as opposed to 23.3% of the veteran group (P = .047). There was no such difference between the diagnosis groups in depression symptoms (Figure 1).
TABLE 1—
Demographic Characteristics of Diabetic Women, by Time Since Diagnosis: India, 2011
| Characteristic | Diagnosed ≥ 2 Y Previously (n = 146) | Diagnosed < 2 Y Previously (n = 38) |
| Age,* y, mean (range = 27.0–78.0) | 55.3 | 47.8 |
| Completed secondary school, % | 54.4 | 44.7 |
| Joint family structure, % | 47.3 | 47.4 |
| No. of children, mean | 3.0 | 2.8 |
| Socioeconomic status, % | ||
| Low | 16.4 | 28.9 |
| Middle | 55.5 | 65.8 |
| High | 28.1 | 5.3 |
| Hindu, % | 83.6 | 73.7 |
| Body mass index, kg/m2, mean (range = 16.0–59.2) | 28.4 | 26.5 |
| % body fat, mean (range = 5.5–51.0) | 35.6 | 33.8 |
| Blood glucose level, mg/dL, mean (range = 0.0–468.0) | 158.2 | 173.3 |
| Glycated hemoglobin, mean % (range = 5.6–> 13.0) | 8.4 | 8.8 |
| Anxiety symptoms,* % | 23.3 | 39.5 |
| Depression symptoms, % | 17.8 | 18.4 |
| No. of stressful events in past year, mean (range = 0.0–11.0) | 3.0 | 2.9 |
| No. of disabilities restricting performance of tasks,* mean (range = 0.0–14.0) | 6.0 | 1.1 |
*P < .05 between groups.
FIGURE 1—
Comparison of the percentages of women with diabetes diagnosed < 2 years vs ≥ 2 years in the past with high levels of depression and anxiety symptoms: India, 2011.
In linear regression analyses, disabilities restricting performance of daily tasks predicted increased anxiety and depression scores for both the recently diagnosed and the veteran diabetic women; disabilities predicted depression more strongly across diabetes duration subgroups. Among women diagnosed less than 2 years previously, each additional child predicted a 0.282-point increase in anxiety score (P = .051) and a 0.348-point increase in depression score (P = .003; Table 2). Among veteran diabetic women, however, blood glucose (and not number of children) predicted anxiety, and blood glucose and HbA1c predicted depression. Although SES ranged widely in this sample, it did not predict women’s anxiety scores and predicted depression scores only among the veteran group (B = −0.170; P = .024).
TABLE 2—
Results of Linear Regression Analysis Predicting Anxiety and Depression Symptom Scores Among Diabetic Women, by Time Since Diagnosis: India, 2011
| Anxiety Score |
Depression Score |
|||
| Variable (Category)a | B | P | B | P |
|
Diagnosed < 2 y previously | ||||
| Disability (score) | 0.494 | .001 | 0.658 | < .001 |
| Children (continuous) | 0.282 | .051 | 0.348 | .003 |
| Adjusted R2 | 0.280 | 0.592 | ||
|
Diagnosed ≥ 2 y previously | ||||
| Disability (score) | 0.244 | .001 | 0.520 | < .001 |
| Glucose (continuous) | 0.386 | < .001 | 0.272 | .004 |
| Glycated hemoglobin (continuous) | −0.264 | .006 | ||
| SES (categorical) | −0.170 | .024 | ||
| Adjusted R2 | 0.193 | 0.333 | ||
Note. SES = socioeconomic status. Only statistically significant predictors are shown. Because the table reports adjusted estimates, there are no confidence intervals; thus, only the adjusted P values appear.
Other predictors entered into each backward elimination regression model were religion, body mass index, % body fat, waist-to-hip ratio, education, number of years married, family type (joint vs nuclear), SES, insulin dependency, stressful life events in the past year, the interaction between SES and disability, and the interaction between SES and stressful life events.
In qualitative interviews, women reported that stress, worry, or tension was the primary cause of their illness.12,13 Women connected the onset of their diabetes to recent stressful events such as the death of a spouse, as well as to the residual effects of stress accumulated over their lives. For some, diabetes management was a source of additional distress as well. One woman, for example, reported feeling so much anxiety about her blood sugar that she trembled whenever she checked it.
Many women talked about how their diagnosis came as a shock and required some “getting used to.” One woman, diagnosed only 6 months before her interview, connected the onset of her illness to the stress she endured when her husband lost his job because of dengue fever. At the time of her initial interview, she complained of the difficulties associated with diabetes control, especially because she had previously consumed many sweets. When we visited her house 5 months later for a follow-up interview, however, she had eliminated chai (a type of sweet milky tea usually consumed multiple times a day by the women in this study) from her diet and asserted, “I can do everything [housework-wise]. Sickness is all in the mind.” When asked if she found diabetes control difficult now, she said, “It’s become a habit.” Another woman explained in a follow-up interview, “You get sort of used to the idea [of having diabetes].”
When asked about how diabetes had affected their daily routines, many women said that they made minor modifications but still managed the same tasks. Comments such as “I can’t work as fast as I used to” and “I have to stop and rest, so things take longer” were common. Some women mentioned that they sat down when peeling vegetables instead of standing up or that they maintained responsibility for most household work but needed help with the most physically demanding tasks, such as mopping the floor. Many women had part- or full-time domestic help, which mitigated the disabilities they might have otherwise experienced with respect to performing household tasks.
DISCUSSION
This exploratory analysis of symptoms of depression and anxiety among diabetic women in New Delhi, India, was guided by the observation that anxiety has received little research attention as compared with depression, especially given its potential comorbidity with chronic diseases. Although high levels of depression symptoms were present in this group of diabetic women, high anxiety symptom levels were significantly more common. More than a quarter of the women in the study reported clinically significant levels of anxiety symptoms, and anxiety was predicted by recency of diabetes diagnosis, blood glucose level, disabilities restricting daily functioning, and level of household burden. Here we offer some socially grounded interpretations of the observed relationships.
The prevalence of high anxiety symptom levels among women diagnosed more recently suggests an initial period of increased vulnerability to anxiety that may wane over time as women become more accustomed to having diabetes. The qualitative data support the idea that women become accustomed both to the idea of “being diabetic” and to the everyday routines associated with diabetes management. Qualitative work among people suffering from other chronic diseases has demonstrated that these diagnoses often create profound disruptions in identity, social relationships, and life routines, and may precipitate periods of personal and interpersonal recalibration.24–26
Similarly, the anxiety observed among recently diagnosed women may reflect a period of increased distress as they adjust to their diabetes and learn to manage it along with other responsibilities. Although these disruptions may never entirely disappear, women may experience less day-to-day anxiety related to diabetes as time goes on. Our qualitative data also support this hypothesis; the case of the woman who initially felt “sad” about having to give up sweets but later felt that it had become “habit” illustrates this progression, and this was a common pattern. There was no similar association between depression symptoms and diabetes onset.
Regardless of how recently a woman was diagnosed with diabetes, disabilities restricting performance of daily tasks were consistent predictors of anxiety and depression symptoms. Limitations in daily function were a key factor linking diabetes with compromised mental health in this sample, and the effect seemed to be magnified among more recently diagnosed women. As Table 2 demonstrates, disabilities restricting daily tasks predicted approximately twice the increase in anxiety symptoms and a 20% greater increase in depression symptoms among recently diagnosed women relative to veteran diabetic women, despite the fact that veterans reported higher levels of actual disability on an everyday basis. This finding underscores the importance of screening diabetic women for mental health problems early in their illness trajectory and of developing interventions that can delay or prevent diabetes-related complications, not only for the sake of women’s physical well-being but for the sake of their mental health as well.
Higher blood glucose was related to anxiety and depression symptoms among veteran diabetic women; this is unsurprising, as an association between poor diabetes control and mental and physical health complications is well documented.2 It is, however, notable that among newly diagnosed women, number of children predicted anxiety and depression symptoms more strongly than did blood sugar level. This underscores the importance of family dynamics, and particularly of having a larger number of dependents, for diabetic women’s mental health early in their diagnosis, a finding corroborated in the ethnographic portions of this study14 and in other settings.12 Although number of children was strongly and negatively correlated with women’s educational levels and SES, neither of the latter 2 variables emerged as a consistent predictor of women’s mental health, suggesting that in this context household burdens may outweigh other common predictors of distress.
In this cultural context, patrilocal joint families (in which nearly half of the women lived) place young and middle-aged married women at the center of household duties, including intensive caregiving for parents-in-law, children, and spouses.28,29 Cultural and religious ideals that promote outward expressions of self-sacrifice as indications of women’s virtue create social norms that do not encourage women to engage in self-care behaviors.12,13 When a woman develops diabetes in this cultural context, the imperatives of self-care for the sake of one’s health may chafe against dominant social norms that emphasize women’s care of others.
It is noteworthy that SES, which ranged widely in this sample, did not emerge as a consistent predictor of the relationships between anxiety symptoms, depression symptoms, and diabetes. One might expect SES to be an important determinant of factors such as diabetes control and number of children and thus to be closely related to mental health symptoms in this setting. Instead, SES was significant only in predicting depression symptoms among veteran diabetic women, and even in this case it was minimally protective, conferring a statistically significant but small reduction of 0.17 points in depression score (which ranged from 0 to 2.73 in this sample) for each higher socioeconomic class. This result suggests that other predictors of mental well-being identified here, including number of children, recency of diagnosis, and blood glucose level, appear to be more important than SES in the relationship between diabetes and distress.
Cumulatively, our analyses suggest that anxiety may be a common source of comorbidity with type 2 diabetes. In addition, they suggest that diabetes may be linked to increased anxiety symptoms in this sample through culturally mediated mechanisms that include patrilocal family structures, burdens related to family responsibilities, and the degree to which diabetes impinges on women’s ability to fulfill domestic tasks linked directly to those responsibilities.
This scenario calls for 3 future directions. First, future studies among people with chronic diseases should include anxiety as well as depression assessments to determine whether anxiety is as common in other settings as it was in this one. At present, data on anxiety levels among people with chronic diseases are remarkably sparse, but it is entirely plausible that anxiety is as significant a problem as depression among people with chronic diseases. This could have important clinical, policy, and programmatic implications because anxiety calls for a somewhat different treatment path than depression.
Second, future studies should explore the social correlates of mental and physical health comorbidities, as those reported in this study might be context specific. For instance, diabetic women in societies where family responsibilities are less central to women’s identity might experience less anxiety related to disability than that observed here, and in nonpatrilocal societies anxiety might be less pronounced among newly diagnosed, younger women than it was here. Third, further research is needed to investigate whether the apparent increased vulnerability to anxiety shortly after diagnosis is a widespread aspect of chronic disease experiences and, if so, to assess the programmatic and clinical implications of this potentially important finding.
Limitations
Because of the small sample size and convenience sampling method used in this study, its results are not generalizable to North Indian women as a whole. This group of women was subject to potential selection bias during the initial clinical encounter as well as the follow-up stage. In addition, as a result of the cross-sectional design of our study, we cannot assess the relationship between diabetes and mental health longitudinally, although stratifying women by duration of their diabetes provided some insight into potential longer-term relationships between diabetes and anxiety disorders. Finally, the application of linear regression to a nonrepresentative sample means that the P values reported here represent the probability that a given statistic is a result of pure chance rather than representing the probability that associations exist in the larger population. Because of these limitations, our findings can be interpreted only as a potential launching point for larger, more robust studies that might explore relationships between chronic diseases and anxiety disorders.
Conclusions
In this study of mental health among diabetic women living in New Delhi, India, we found that high levels of anxiety disorder symptoms were common, affecting more than 25% of the total sample. Although women’s depression and anxiety symptoms were patterned somewhat similarly, there were some important differences. For example, anxiety symptoms were significantly more widespread than depression symptoms across the entire sample of diabetic women. Also, high anxiety symptom levels were more common among recently diagnosed diabetic women than among diabetic women diagnosed longer in the past, a trend that was not present for the depression data. These results suggest that it might be appropriate to time anxiety screening, treatment, and prevention differently than depression interventions for people with chronic diseases.
Our analyses identified several variables that predicted anxiety symptoms in this convenience sample, including blood sugar level, time since diagnosis, disabilities restricting performance of daily tasks, and number of children. Our qualitative data suggested that a key pathway linking diabetes with both anxiety and depression symptoms in this context appears to be the degree to which the illness interferes with women’s daily functioning in a particular set of gender-specific tasks relevant for women in this cultural context. These tasks largely involve the care of others and may thus conflict with the intensive self-care regimens typically prescribed for diabetes.
Anxiety disorders should receive more attention as a potential source of comorbidity with CNCDs. Our exploratory study showed high levels of anxiety symptoms among women with type 2 diabetes in New Delhi and also demonstrated higher anxiety scores among women diagnosed more recently with diabetes. If results are similar in future studies, this may indicate that anxiety and depression interact with CNCDs in distinct ways and at distinct times in the CNCD illness trajectory. This situation, in turn, could indicate a need for changes in detection and treatment of mental health problems that are comorbid with chronic diseases; for instance, detection of comorbid anxiety might be more effective if heightened during the first years of a chronic disease diagnosis. Such considerations may become increasingly important as age at onset of type 2 diabetes becomes younger around the world.
Acknowledgments
Funding for this study was provided by the National Science Foundation, the Fulbright-Hayes Foundation, the American Institute of Indian Studies, the Lemelson/SPA Fund, and Emory University.
We thank the member physicians of the Research Society for the Study of Diabetes in India, all of the research participants, and Sneha Sharma.
Human Participant Protection
This study was approved by the institutional review boards of Emory University and the University College of Medical Sciences (India). All participants provided verbal informed consent before taking part in the study.
References
- 1.Lozano R, Naghavi M, Foreman K et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ciechanowski P, Katon W, Russo J. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160(21):3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 3.de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta-analysis. Psychosom Med. 2001;63(4):619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. 2010;87(3):302–312. doi: 10.1016/j.diabres.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 5.Goldney RD, Phillips PJ, Fisher LJ, Wilson DH. Diabetes, depression, and quality of life. Diabetes Care. 2004;27(5):1066–1070. doi: 10.2337/diacare.27.5.1066. [DOI] [PubMed] [Google Scholar]
- 6.Katon WJ, Rutter C, Simon G et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28(11):2668–2672. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 7.Golden SH, Lazo M, Carnethon M et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299(23):2751–2759. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mendenhall E, Shivashankar R, Tandon N, Ali MK, Narayan KMV, Prabhakaran D. Stress and diabetes in socioeconomic context: a qualitative study of urban Indians. Soc Sci Med. 2012;75(12):2522–2529. doi: 10.1016/j.socscimed.2012.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rock M. Sweet blood and social suffering: rethinking cause-effect relationships in diabetes, distress, and duress. Med Anthropol. 2003;22(2):131–174. doi: 10.1080/01459740306764. [DOI] [PubMed] [Google Scholar]
- 10.Wiedman D. Native American embodiment of the chronicities of modernity: reservation food, diabetes and the metabolic syndrome among the Kiowa, Comanche and Apache. Med Anthropol Q. 2012;26(4):595–612. doi: 10.1111/maq.12009. [DOI] [PubMed] [Google Scholar]
- 11.Mendenhall E. Syndemic Suffering: Social Distress, Depression, and Diabetes Among Mexican Immigrant Women. Walnut Creek, CA: Left Coast; 2012. [Google Scholar]
- 12.Weaver LJ, Hadley C. Social pathways in the comorbidity between type 2 diabetes and mental health concerns in a pilot study of urban middle- and upper-class Indian women. Ethos. 2011;39(2):211–225. [Google Scholar]
- 13.Weaver LJ, Worthman CM, DeCaro JA, Madhu SV. The signs of stress: embodiments of social inequality among women in New Delhi, India. Soc Sci Med. 2015;131:122–130. doi: 10.1016/j.socscimed.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Sartorius N, Utsun TB, Lecrubier Y, Wittchen HU. Depression comorbid with anxiety: results from the WHO Study on Psychological Disorders in Primary Health Care. Br J Psychiatry Suppl. 1996;30:38–43. [PubMed] [Google Scholar]
- 15.Scott KM, Bruffaerts R, Tsang A et al. Depression-anxiety relationships with chronic physical conditions: results from the World Mental Health Surveys. J Affect Disord. 2007;103(1–3):113–120. doi: 10.1016/j.jad.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 16.Demmer RT, Gelb S, Suglia SF et al. Sex differences in the association between depression, anxiety, and type 2 diabetes mellitus. Psychosom Med. 2015;77(4):467–477. doi: 10.1097/PSY.0000000000000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diabetes Atlas, 5th Edition, 2012 Update. Brussels, Belgium: International Diabetes Federation; 2011. [Google Scholar]
- 18.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81(8):609–615. [PMC free article] [PubMed] [Google Scholar]
- 19.Patel V, Kirkwood BR, Pednekar S et al. Gender disadvantage and reproductive health risk factors for common mental disorders in women: a community survey in India. Arch Gen Psychiatry. 2006;63(4):404–413. doi: 10.1001/archpsyc.63.4.404. [DOI] [PubMed] [Google Scholar]
- 20.Poongothai S, Pradeepa R, Ganesan A, Mohan V. Prevalence of depression in a large urban South Indian population—the Chennai Urban Rural Epidemiology Study (Cures-70) PLoS One. 2009;4(9):e7185. doi: 10.1371/journal.pone.0007185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Borgatti S. Elicitation techniques for cultural domain analysis. In: Schensul JJ, editor. Enhanced Ethnographic Methods. Walnut Creek, CA: AltaMira Press; 1999. pp. 115–151. [Google Scholar]
- 22.American Diabetes Association. Standards of medical care in diabetes—2011. Diabetes Care. 2011;34(S1):S16–S27. doi: 10.2337/dc11-0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liburd L, Namageyo-Funa A, Jack L, Gregg E. Views from within and beyond: illness narratives of African American men with type 2 diabetes. Diabetes Spectr. 2004;17(4):219–224. [Google Scholar]
- 24.Charmaz K. Good Days, Bad Days: The Self and Chronic Illness in Time. New Brunswick, NJ: Rutgers University Press; 1991. [Google Scholar]
- 25.Greenhalgh S. Under the Medical Gaze: Facts and Fictions of Chronic Pain. Berkeley, CA: University of California Press; 2001. [Google Scholar]
- 26.Becker G. Disrupted Lives: How People Create Meaning in a Chaotic World. Berkeley, CA: University of California Press; 1997. [Google Scholar]
- 27.Strauss A, Corbin J. Grounded theory research: procedures, canons and evaluative criteria. Qual Sociol. 1990;13(1):3–21. [Google Scholar]
- 28.Donner H. Domestic Goddesses: Maternity, Globalization and Middle-Class Identity in Contemporary India. Burlington, VT: Ashgate Publishing; 2008. [Google Scholar]
- 29.Ray R, Qayum S. Cultures of Servitude: Modernity, Domesticity, and Class in India. Palo Alto, CA: Stanford University Press; 2009. [Google Scholar]