Abstract
Objectives. We investigated the perspectives of people using a wheelchair and their difficulties in accessing dental services.
Methods. Our participatory research was on the basis of a partnership between people using a wheelchair, dental professionals, and academic researchers. Partners were involved in a committee that provided advice at all stages of the project. Our team adopted a qualitative descriptive design. Between October 2011 and October 2012 we conducted semistructured individual interviews with 13 adults who lived in Montreal, Québec, Canada, and used a wheelchair full time. We audio-recorded and transcribed verbatim interviews, and we interpreted data using an inductive thematic analysis.
Results. Oral health is of heightened importance to this group of people, who tend to use their mouth as a “third hand.” We identified successive challenges in accessing dental services: finding a dentist and being accepted, organizing transportation, entering the building and circulating inside, interacting with the dental staff, transferring and overcoming discomfort on the dental chair, and paying for the treatments.
Conclusions. Governments, dental professional bodies, dental schools, and researchers should work with groups representing wheelchair users to improve access to dental services.
People with physical disabilities generally experience poor oral health and have more untreated dental problems than does the rest of the population.1 One reason for this disadvantage is that systemic diseases underlying disabilities, and associated medications, can negatively affect or be affected by oral health. For instance, immunosuppressive agents used in the treatment of rheumatoid arthritis cause gingival hyperplasia and antispasmodics, anti-Parkinsonism, and muscle relaxant medications cause xerostomia.2 Cerebral palsy patients may experience severe bruxism, temporomandibular joint problems, and tooth wear. Furthermore, poor oral health may be detrimental to general health, especially for people with disabilities. Notably, the association of periodontal disease with heart disease, stroke, and diabetes is now well established.3,4
Access to dental services may be difficult for those with physical disabilities.5 Among the “4.4 million persons with disabilities in Canada, dental care remains one of the most required health services yet it is also the hardest to find.”6(p9) Despite great health needs, people with disabilities experience major obstacles in accessing primary care.7 This is the case in Québec, Canada, for instance, where one fifth of this population reports being unable to access the health care they require.8 The number of wheelchair users is steadily increasing as the elderly population increases; there are 6 times more wheelchair users today than there were 30 years ago.3,9 According to Statistics Canada, approximately half of current wheelchair users belong to the rapidly expanding elderly population.10
Despite these problems, very little is known about the dental care pathways of people using a wheelchair, including the challenges encountered in accessing dental services. We addressed this lack of knowledge by seeking to identify obstacles and better understand their implications. The social model of disability suggests that wheelchair use is impeded by society’s failure to take into account impairments and accessibility when creating physical and social environments.11 We explored this failure, and we have proposed solutions to facilitate this population’s access to quality dental services.
METHODS
Adopting a participatory approach, we developed a partnership linking 3 groups of constituents12—people with disabilities, dental professionals, and researchers—who collaborated through an advisory committee during all stages of the research. Each group contributed expertise, through either scientific knowledge or lived experience.
Design and Sampling
Our qualitative descriptive design was well suited to exploring phenomena that we knew little about.13 Semistructured interviews allowed the collection of in-depth information about complex issues, such as perceptions, emotions, and behaviors.14
We brought together a group of participants who were diverse along various sociodemographic and health measures, type of wheelchair (electric or manual) used, and type of dental coverage using a purposeful sampling strategy known as “maximum variation.”15 To be included, participants had to (1) be permanent wheelchair users, (2) be aged 18 to 65 years, (3) be able to speak English, and (4) have consulted a dentist or searched for dental services in the previous 2 years.
Data Collection and Analysis
With the help of our community partners, we recruited 13 people in Montreal, Québec, Canada, and interviewed them between October 2011 and October 2012. Participants chose where the interviews took place, such as their home or workplace. Before starting, the interviewer (F. R.) explained her background and the objectives of the project and answered participants’ questions. Then each participant signed a consent form approved by an academic institutional review board. The discussion lasted about 1 hour, with a follow-up interview when necessary. We audio-recorded all interviews and transcribed them verbatim. The interviewer adopted an open-ended conversational style and used an interview guide that was designed to aid recall of oral health–related experiences. During the fieldwork, the interviewer used introspective and intersubjective approaches; after each interview, a debriefing session with another team member (C. B.) allowed her to reflect on interview dynamics.
We used inductive thematic analysis, “a process of coding the data without trying to fit it into a pre-existing coding frame, or the researcher’s analytic preconceptions,”16(p12) during which all codes emerged.17 We then examined the codes and their corresponding passages through an iterative process, regrouped them into larger themes, and established links between these. Finally, we built matrices to display and summarize the data.18 These matrices helped us interpret the data. The results were discussed with 2 study participants, who elaborated on certain issues that had not been sufficiently explored in the interviews.
RESULTS
Participants included 9 women and 4 men who permanently used a wheelchair. Their need for a wheelchair was the consequence of an accident affecting their spinal cord or the result of 1 of the following: cerebral palsy, rheumatoid arthritis, spinal meningitis, or a degenerative neuromuscular disorder. In some cases, these diseases affected people’s ability to masticate or swallow. Only 4 participants had private dental insurance from paid employment; the other 9 received social assistance and thus benefited from public dental insurance (Table1).
TABLE 1—
Wheelchair Users (n = 13) Accessing Dental Services: Montreal, Québec, Canada, 2011–2012
| Characteristic | No. Participants |
| Gender | |
| Women | 9 |
| Men | 4 |
| Age, y | |
| 18–29 | 1 |
| 30–49 | 6 |
| 50–65 | 6 |
| Occupation or income source | |
| Employed full time | 3 |
| Employed part time or casually | 2 |
| Unemployed or on social assistance | 8 |
| Reason for disability | |
| Accident or spinal cord injury | 4 |
| Cerebral palsy | 3 |
| Arthritis | 2 |
| Spinal meningitis | 2 |
| Neuromuscular diseases | 2 |
| Type of wheelchair | |
| Manual | 3 |
| Electric | 10 |
| Time in wheelchair, y | |
| < 10 | 2 |
| 10–20 | 3 |
| 21–30 | 6 |
| 31–40 | 1 |
| > 40 | 1 |
| Type of dental insurance | |
| Private | 4 |
| Public (e.g., welfare) | 9 |
Participants highly valued oral health and oral health care. They underlined the role of their teeth for aesthetics and, most importantly, emphasized their mouth’s crucial function as a “third hand.” They described using their mouths in their daily lives as a replacement for, or in addition to, their hands. They used their mouths to help them carry objects and in various other circumstances:
I put everything in my mouth now, and I do everything with my mouth now. Because it’s like my third hand, because I don’t have the usage of my right hand; it’s all paralyzed. My left hand is working a bit but not my right, so I do a lot of things with my teeth, you know. I’m grabbing things; I’m holding things, so it’s very important that I take very good care of my teeth. (interviewee 2)
Use of their mouths as a third hand raised concerns among participants about damage to their teeth and the need for professional dental care:
To have good teeth for me is essential because I need my mouth to actually do everything, so I’m trying to keep as many [teeth] as possible in my mouth! (interviewee 8)
Yet participants reported tremendous difficulties accessing dental services. Figure 1 depicts the numerous challenges, each of which, singly or in combination with others, could delay or even interrupt participants’ dental care pathway:
finding a dentist and being accepted,
organizing transportation,
entering the building and circulating inside,
interacting with the dental staff,
transferring into the dental chair,
overcoming discomfort on the dental chair, and
paying for treatment.
FIGURE 1—
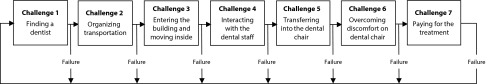
Challenges faced by wheelchair users in their dental care pathway: Montreal, Québec, Canada, 2011–2012.
Each of these challenges could delay or even interrupt participants’ dental care pathway. Participants did not face all these challenges each time they consulted; for instance, some had secured professional dental care and thus no longer encountered the challenges of finding a dentist and negotiating interaction with the staff.
Challenge 1, Finding an Accessible Dental Clinic
Finding a dentist was typically a difficult and frustrating process. Participants used numerous strategies, including word of mouth and searching out accessible clinics in person or through telephone inquiries. Unsuccessful after several years, certain participants had suspended their search or even given up. Consequently, some decided to stay with a dentist despite being dissatisfied, whereas others simply remained without a dentist. Participants deplored the lack of reliable information:
That’s the hardest part: nowhere you can ask or go on the Internet to see a directory of dentists, let’s say in Montreal, and, say, with the specification “wheelchair accessible.” (interviewee 8)
An erroneous understanding of accessibility caused dental staff to mislead several participants. For instance, after having a discussion with a dental secretary and obtaining an appointment, a participant discovered that the clinic was not accessible:
When I got there, I couldn’t get into the office. There were steps. As I remember there were 5 or 6 steps or something like that. (interviewee 4)
Some dental staff refused participants over the telephone or even once they arrived at the clinic, despite having booked an appointment. These hurtful and discriminatory situations were compounded in the case of wheelchair users on social assistance, who felt that they faced the “double challenge” (interviewee 8) that disability and welfare pose, as each can constitute a reason for refusal by a dentist.
Challenge 2, Transportation Issues
Participants who had to rely on public adapted transportation faced many logistical difficulties. They deplored the lack of punctuality of the transportation services, forcing them to anticipate delays to avoid being late or miss dental appointments.
That was a problem because the first time I went to my regular dentist, I booked for an hour and it took like 2 and a half hours [to be treated at the dental office]. So I had to kind of make arrangements so that they pick me up later. And then the second one . . . took like 20 minutes and I was out. So again I had to call and make arrangements. (interviewee 5)
Adapted transport made a mistake in the time of appointment. So I called them [the dental office] and said, “Excuse me.” When the receptionist called me she said, “You have cancelled 3 times.” When I went there I said, “. . . sometimes there is no choice but cancelling.” (interviewee 10)
Challenge 3, Clinic Access and Circulation
Even though some buildings seemed accessible at first glance, numerous obstacles became apparent upon entry:
If the door is too heavy, I don’t know, I could call the secretary: “I’m here, can you please come and open the door?” Something like that, yeah. I have to have a backup plan. (interviewee 5)
That was like an old building and I just barely fit with my chair. So someone had to push me because the doors were just standard doors [not wide enough for wheelchair users].
Most spaces were small or cluttered, making circulation a difficult and sometimes impossible endeavor, especially for those using electric wheelchairs, which are more cumbersome than are manual wheelchairs. In certain cases, the waiting rooms could not accommodate a wheelchair:
I don’t have any space, so I cannot even be in the waiting room. I have to go out [of the clinic] or I have to go in [the examination room]; so it’s not pleasant. (interviewee 2)
It’s a big dental office so there are a lot of offices . . . when someone is coming, they go back because there is no room for 2 of us: I’m on the chair and they are walking and there is no room. (interviewee 7)
Accessibility of clinic washrooms was particularly important, as participants were away from home for lengthy periods. But most washrooms were not adapted to their needs, a very stressful situation (interviewee 7).
Because of lack of space, the dental staff sometimes had to move the furniture to permit circulation. This applied to the examination room, which was generally tight and rendered the transfer into the dental chair particularly challenging:
[It is not easy to maneuver] to go in and, you know, try to get in the space because they have to take out . . . everything, and often there are extra machines; they have to push that out. So I can, you know, go backwards so I can transfer. (interviewee 2)
Afraid of hitting and damaging furniture or walls, participants expressed their embarrassment at being a potential source of disturbance for the staff (interviewee 4).
Challenge 4, Interacting With Dental Staff
The reception countertop, which was usually higher than the participant’s head, constituted the first barrier in interaction with dental staff. In addition, this design complicated the paperwork, notably when, as is typical, the counter and credit card terminal were inaccessible (interviewee 2).
Of course, participants described positive interactions with dental professionals, many of whom were “patient,” “positive,” “helpful,” or “understanding.” But other encounters felt discriminatory, such as being ignored at times:
When I’m accompanied . . ., you know, they are talking to the person standing up rather than looking at me first. (interviewee 12)
Challenge 5, Transferring Into the Dental Chair
Participants found it difficult to transfer into the dental chair and to remain immobile for long stretches of time (interviewee 8). They preferred to stay in their wheelchair during the dental treatment, but dental professionals were reportedly reluctant, invoking practical reasons and lack of comfort, even in the case of electric wheelchairs that allowed people to lie in a horizontal position.
The process of transferring was arduous because of the chair design but also the dental staff’s lack of appropriate skills and equipment (Table 2). The situation was especially acute for participants suffering from generalized paralysis, as they could not actively participate in the transfer. Many apprehended pain and even feared falling. Moreover, the dental staff was so uncomfortable with this procedure that they generally refused to undertake a transfer on their own. Consequently, a friend, family member, or personal attendant was required to accompany and assist at the dental clinic (interviewee 5).
TABLE 2—
Wheelchair Users’ Difficulties Transferring Into a Dental Chair: Montreal, Québec, Canada, 2011–2012
| Issues | Participant Quotations |
| Excessive height of the dental chair. The lowest level of the chair was still too high and made participants’ transfer difficult. | “I found their chairs could [should] move up and down a bit lower because even with the manual chair, you still need help for transfer . . . from what I can remember you have to stand because it’s still a couple of inches you have to get bumped [lifted] up there.” (interviewee 8) |
| “Coming back on the wheelchair was more challenging, because it’s lower and the position of the feet is . . . in an angle, so all those factors made it more difficult to get back on the chair.” (interviewee 7) | |
| Obtrusive position of the dental chair arm. The arms of some dental chairs did not slide and impeded participants’ installation. | “The arm couldn’t come off, so they had to lift me, help me transfer.” (interviewee 1) |
| Lack of supportive devices. The dental chairs lacked bars and handles to facilitate transfer. | “On the chair of the dentist you don’t have support; you don’t have anchors, guiding bars.” (interviewee 9) |
| Chair covering. Participants could not install themselves in the chair because of fabrics not conducive to transfers, such as sticky leather. | “Sometimes it’s all leather and leather doesn’t slide, so it’s very difficult to go from my chair to the leather that is very sticky.” (interviewee 2) |
| Dental staff lack of skills. The staff lacked skills on lifting techniques, manual transfer of the participants, and removing the electric wheelchair from the examination room once the transfer was done. | “As much as the dentist that I have is really, really nice and really accommodating, they definitely don’t know anything about people with disabilities. They do their best; they’re very open-minded, but they obviously never had any training or any real understanding of the real situation, so they have to ask many questions.” (interviewee 5) |
| “We need to transfer me with 2 people and so they wanted me to bring somebody to do the top so that’s the heaviest part to lift and just have to transfer.” (interviewee 5) | |
| “They try to take the chair out of the space, but they can’t because they don’t know how to. . . . They are not used to working with the chair, so it’s not easy. It’s not easy for them; it’s not easy for me.” (interviewee 2) |
Challenge 6, Discomfort During Treatment Sessions
Lying in the dental chair was uncomfortable for most participants and was a source of back, neck, and shoulder pain, especially during long sessions. The dental chairs were poorly adapted to their needs: they lacked cushion support, the plastic covers could be slippery and cause a fall, and the lower part of the chair was not adjustable:
She set me on this chair, adjusted me to get flat completely . . . so I was like at an angle and this is really torture. (interviewee 9)
Numerous specific medical conditions caused further difficulty or concern; for instance, participants who used a urinary catheter and drainage bag were particularly uncomfortable in a horizontal position (interviewee 2).
Participants with arthritis and muscular dystrophy reported difficulties in opening and closing their mouths, which complicated treatment sessions:
I go for my fillings there and the last 2 that I got were in the back and I cannot open my mouth very wide. And she complained the whole intervention that “oh, if you have another one that’s this far I won’t be able to do it.” . . . She made me feel bad about my mouth not opening . . . of course I’m like enduring a lot of pain because when she says, “Open!” it hurts so much. (interviewee 5)
Challenge 7, Payment
Despite some form of insurance coverage, whether private or public, financial barriers remained. People with private insurance complained that the benefits were insufficient to cover all dental expenses (interviewee 9).
Those on social assistance benefited from public dental insurance, which meant they were eligible for only basic treatments and 1 annual dental check-up. For other treatments or additional check-ups, participants had to pay out of pocket (interviewee 8). Financial considerations forced some participants to reduce the frequency of their check-ups or choose cheaper treatment options. Others tried to pay in installments, borrow money, or occasionally consult a school of dental hygiene (interviewees 4, 5, and 7).
DISCUSSION
We found that oral health is of heightened importance to people using a wheelchair for whom the mouth functions as a third hand and therefore is of added functional importance. People with disabilities encounter tremendous obstacles in their dental care pathways to the point of exclusion from dental services. Such exclusion from basic health care contradicts the United Nations Convention on the Rights of Persons with Disabilities, according to which “persons with disabilities have the right to the enjoyment of the highest attainable standard of health without discrimination on the basis of disability.”19 It is, furthermore, the role of the state to “take all appropriate measures to ensure access for persons with disabilities to health services.”19 The right to health care is undeniable, and it is partially available through public dental insurance. Yet substantial flaws in coverage amount to greatly reduced services and even a lack of services for vulnerable segments of the population.
Limitations
We conducted this study in Montreal, Canada, and so our results should be considered in social, political, and cultural context. The challenges that we described may nevertheless occur to varying degrees in other countries, especially if they share some of the characteristics of the Quebec health care system and its regulations. It is important to note that we interviewed wheelchair users with specific medical conditions (Table 1); people with different types of impairment may thus experience other kinds of barriers in accessing dental services.
In addition, all participants had consulted or searched for dental services in the previous 2 years. We thus excluded people who, not having consulted for a long time, may have faced particular barriers we have not documented. The sample of 13 people may appear to be a limitation by some standards but is appropriate considering that we used saturation to guide sample size.20
Conclusions
To our knowledge, this study is the first to voice the experiences of wheelchair users concerning access to dental services. The challenges that we described refer to all dimensions of access as defined by Penchansky and Tomas21: availability, accessibility, affordability, accommodation, and even acceptability. With respect to acceptability, it is important to note that certain participants felt that dental professionals overlooked them because of their physical condition.
Some of these challenges have been documented in the medical field,22,23 including structural problems in physical environments, transportation, financial issues, and personal factors. Our research adds to this literature by describing challenges that are specific to dentistry. We explored new territories by richly documenting issues such as challenges in transferring to and sitting in dental chairs during treatment sessions. Our research also provides insight into the specific relevance of oral health to some of the participants’ physical conditions, such as limitations in opening their mouths. The use of the mouth to transport objects and compensate for limb paralysis lends particular significance to their dental needs.
According to the World Health Organization’s biopsychosocial model of disability,24 it is the responsibility of society to increase the access of people with different needs by removing social and physical obstacles. As illustrated in Figure 2, we urge governments, dental professional bodies, dental schools, and researchers to work in partnership with groups representing people using a wheelchair to take concrete measures to improve access to dental services. Situating people with physical disabilities in the center of Figure 2 emphasizes their central role and involvement in the production of knowledge and the implementation of change.
FIGURE 2—
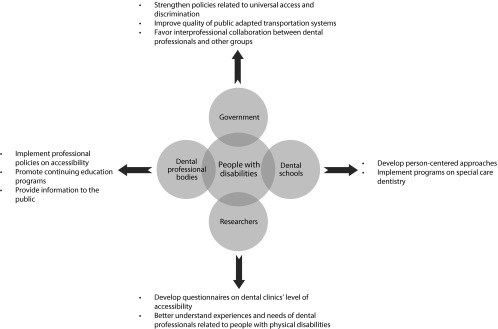
Recommendations for stakeholders to improve wheelchair users’ access to dental services: Montreal, Québec, Canada, 2011–2012.
We provide suggestions appropriate for Canada but likely to apply in many other countries. First, we recommend that the degree of accessibility of dental clinics be systematically evaluated in Quebec (Figure 2). From this perspective, existing questionnaires on universal access, such as the Access Audit Checklist (National Health Service in Scotland), could be adapted for dental clinics and enriched with specific questions inspired by our study. The results should then be made widely available to the population, which lacks crucial information on clinic accessibility.
Second, professional bodies, dental schools, and governmental institutions should carefully examine the results of this evaluation and, in partnership with people with disabilities, identify actions to be undertaken. Figure 2 provides examples of interventions and policies. For instance, dental schools could promote patient-centered approaches25,26 and, as Dolan recommends, develop undergraduate as well as graduate special care dentistry programs to allow future dentists to better respond to the needs of people with disabilities.27 Governmental and professional bodies should further strengthen antidiscrimination policies and favor interprofessional collaboration: social workers, occupational therapists, nurses, and family doctors could play a key role in connecting people with disabilities and dental professionals.
Dentistry is not well enough organized to fulfill the needs of wheelchair users, who, as a consequence, face discrimination. The deficiencies of the dental care system in accommodating this growing sector of the population are felt in several ways, including inaccessible buildings, negative attitudes and lack of knowledge on the part of dental professionals and staff, high costs of dental services, and inadequate insurance plans. These factors complicate the process of dental treatment and intersect to create a hostile environment for people using wheelchairs. It is up to the political and professional bodies, in partnership with people with physical disabilities, to remove the barriers, thereby providing affordable, accessible, and high-quality dental care for all.
Acknowledgments
F. R.-K. was the recipient of a master of science fellowship from the Centre de recherche de Montréal sur les inégalités sociales, les discriminations et les pratiques alternatives de citoyenneté and received financial support from the Canadian Institutes of Health Research. B. N. holds a Canada Research Chair in Life Course Oral Epidemiology. C. B. holds a salary award from Fonds de recherche du Québec—Santé.
This study’s data have been published in a master’s thesis; we also presented abstracts at the following conferences: 80e Congres de l’ACFAS (Association Francophone pour le Savoir), Montreal, May 2012; 18th Qualitative Health Research Conference (QHR), Montreal, October 2012; and 16èmes JASP (Journées Annuelles de Santé Publique), Montreal, November 2012.
We thank the people who participated in the qualitative interviews for their time and willingness to share their experiences. We are very grateful to the members of the advisory committee: Isabelle Ducharme, Linda Gauthier, Martine Lévesque, Nathalie Morin, Laurent Morissette, Laurence Parent, and Claire Savage. We also thank Alissa Levine for her substantial editorial contributions.
Human Participant Protection
This study received approval from McGill University Faculty of Medicine’s institutional review board. All participants gave written informed consent.
References
- 1.Glassman P, Miller CE. Preventing dental disease for people with special needs: the need for practical preventive protocols for use in community settings. Spec Care Dentist. 2003;23(5):165–167. doi: 10.1111/j.1754-4505.2003.tb00305.x. [DOI] [PubMed] [Google Scholar]
- 2.Sreebny LM, Schwartz SS. A reference guide to drugs and dry mouth. Gerodontology. 1986;5(2):75–99. doi: 10.1111/j.1741-2358.1986.tb00055.x. [DOI] [PubMed] [Google Scholar]
- 3.Stiefel DJ. Dental care considerations for disabled adults. Spec Care Dentist. 2002;22(3 suppl):26S–39S. [PubMed] [Google Scholar]
- 4.Wu T, Trevisan M, Genco RJ, Dorn JP, Falkner KL, Sempos CT. Periodontal disease and risk of cerebrovascular disease: the first national health and nutrition examination survey and its follow-up study. Arch Intern Med. 2000;160(18):2749–2755. doi: 10.1001/archinte.160.18.2749. [DOI] [PubMed] [Google Scholar]
- 5.Sigal A. Time to improve access to oral health care for persons with special needs. J Can Dent Assoc. 2009;75(7):517–519. [PubMed] [Google Scholar]
- 6.Sandhu H, Mock D. Dental schools are committed to increasing access to care. J Can Dent Assoc. 2010;76 a5. [PubMed] [Google Scholar]
- 7.Kroll T, Beatty PW, Bingham S. Primary care satisfaction among adults with physical disabilities: the role of patient-provider communication. Manag Care Q. 2003;11(1):11–19. [PubMed] [Google Scholar]
- 8.Camirand J. Vivre avec une incapacité au Québec: Un portrait statistique à partir de l’enquête sur la participation et les limitations d’activités de 2001–2006. Montreal, Québec: Institut de la statistique du Québec; 2011. [Google Scholar]
- 9. LaPlante MP; Disability Statistics Center. Demographics of wheeled mobility device users. Presented at the Conference on Space Requirements for Wheeled Mobility; October 9–11, 2003; Buffalo, NY.
- 10.Shields M. Use of wheelchairs and other mobility support devices. Health Rep. 2004;15(3):37–41. [PubMed] [Google Scholar]
- 11.Nagi S. Some conceptual issues in disability and rehabilitation. In: Sussman MB, editor. Sociology and Rehabilitation. Washington, DC: American Sociological Association in Cooperation with the Vocational Rehabilitation Administration, US Department of Health, Education and Welfare; 1965. pp. 100–113. [Google Scholar]
- 12.Green LW, George MA, Daniel M . Study of Participatory Research in Health Promotion: Review and Recommendations for Development of Participatory Research in Health Promotion in Canada. Ottowa, Ontario: Royal Society of Canada; 1995. [Google Scholar]
- 13.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23(4):334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 14.Bedos C, Pluye P, Loignon C, Levine A. Qualitative research. In: Lesaffre E, Feine J, Leroux B, Declerck D, editors. Statistical and Methodological Aspects of Oral Health Research. Chichester, UK: John Wiley; 2009. pp. 113–130. [Google Scholar]
- 15.Patton MQ. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- 16.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 17.Corbin JM, Strauss AL. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newburry Park, CA: Sage; 1990. [Google Scholar]
- 18.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 19.United Nations Enable. Convention on the Rights of Persons with Disabilities. 2006. Available at: http://www.un.org/disabilities/convention/conventionfull.shtml. Accessed April 14, 2015.
- 20.Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82. [Google Scholar]
- 21.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–140. doi: 10.1097/00005650-198102000-00001. [DOI] [PubMed] [Google Scholar]
- 22.Dejong G, Palsbo SE, Beatty PW, Jones GC, Knoll T, Neri MT. The organization and financing of health services for persons with disabilities. Milbank Q. 2002;80(2):261–301. doi: 10.1111/1468-0009.t01-1-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iezzoni LI, O’Day B. More Than Ramps: A Guide to Improving Health Care Quality and Access for People With Disabilities. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- 24.International Classification of Functioning, Disability and Health: ICF. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 25.US Department of Justice. ADA standards for accessible design. 2010. Available at: http://www.ada.gov/regs2010/2010ADAStandards/2010ADAstandards.htm. Accessed August 11, 2014.
- 26.Apelian N, Vergnes J-N, Bedos C. Humanizing clinical dentistry through a person-centered model. International Journal of Whole Person Care. 2014;1(2):30–50. [Google Scholar]
- 27.Dolan TA. Professional education to meet the oral health needs of older adults and persons with disabilities. Spec Care Dentist. 2013;33(4):190–197. doi: 10.1111/scd.12013. [DOI] [PubMed] [Google Scholar]


