Abstract
Objective: A comprehensive bibliometric analysis was conducted on publications for yoga therapy research in clinical populations.
Methods: Major electronic databases were searched for articles in all languages published between 1967 and 2013. Databases included PubMed, PsychInfo, MEDLINE, IndMed, Indian Citation Index, Index Medicus for South-East Asia Region, Web of Knowledge, Embase, EBSCO, and Google Scholar. Nonindexed journals were searched manually. Key search words included yoga, yoga therapy, pranayama, asana. All studies met the definition of a clinical trial. All styles of yoga were included. The authors extracted the data.
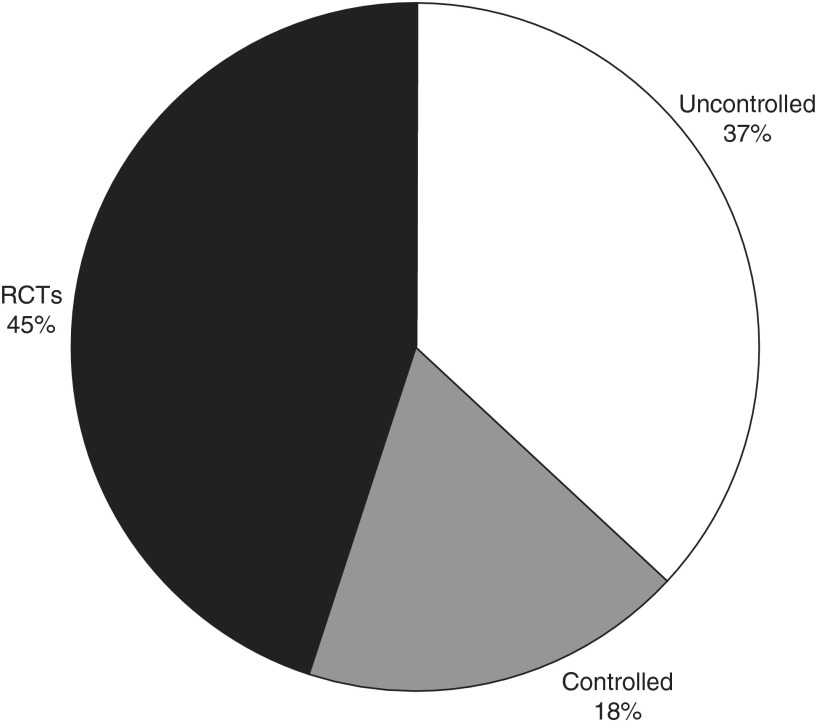
Results: A total of 486 articles met the inclusion criteria and were published in 217 different peer-reviewed journals from 29 different countries on 28,080 study participants. The primary result observed is the three-fold increase in number of publications seen in the last 10 years, inclusive of all study designs. Overall, 45% of the studies published were randomized controlled trials, 18% were controlled studies, and 37% were uncontrolled studies. Most publications originated from India (n=258), followed by the United States (n=122) and Canada (n=13). The top three disorders addressed by yoga interventions were mental health, cardiovascular disease, and respiratory disease.
Conclusion: A surge in publications on yoga to mitigate disease-related symptoms in clinical populations has occurred despite challenges facing the field of yoga research, which include standardization and limitations in funding, time, and resources. The population at large has observed a parallel surge in the use of yoga outside of clinical practice. The use of yoga as a complementary therapy in clinical practice may lead to health benefits beyond traditional treatment alone; however, to effect changes in health care policy, more high-quality, evidence-based research is needed.
Introduction
Yoga originated in India thousands of years ago as a philosophical or spiritual discipline to deliver practitioners from suffering, or dis-ease (duhkha).1 The practice of yoga unifies the mind and body through coordinated breathing (pranayama), movement (asana), and meditation (dhyana), which has been known to promote well-being and reduce stress. Stress has been defined as the disruption of a person's “biological, psychological and social dimensions” as a result of environmental challenges or perceived threat.2 It is estimated that between 60% and 90% of visits to the doctor are stress-related, due to the aggravating effects of stress on such conditions as cardiovascular disease, mental health, chronic pain, and sleep disorders.3,4 Chronic stress results in a maladaptive activation of the hypothalamic-pituitary-adrenal axis and the autonomic nervous system.5 The autonomic nervous system regulates the parasympathetic (ie, rest and digest) and sympathetic (ie, fight or flight) systems and influences functions such as digestion, heart rate, and respiratory rate as a compulsory stabilizing response to stress and other environmental challenges (ie, the stress response).5 Proper functioning of the hypthothalamic-pituitary-adrenal axis regulates metabolism, the immune system, normal growth and development, thyroid function, and reproduction.5 Numerous yoga studies have demonstrated the positive healing effects on a broad spectrum of health domains, such as physiologic factors as well as psychological well-being (e.g., depression, anxiety),6–8 including the stress response.9 The intentional practice of yogic principles triggers the relaxation response10 and counters the effects of the involuntary physiologic or stress responses, thus restoring balance in the nervous system. Therefore, the holistic application of yoga as an adjuvant therapy in clinical practice may lead to health benefits beyond traditional treatment alone.
In India, yoga has a history of therapeutic benefits as documented and edited by Sri Kuvalayananda in the first journal dedicated to yoga research, called Yoga Mimamsa, launched in 1924. Influenced by studies conducted in India,11,12 the first randomized controlled trial (RCT) was conducted in the West by Chandra Patel,13,14 on the efficacy of yoga for hypertension. With the success of these studies, the Indian Council of Medical research funded a major undertaking to examine neurophysiologic changes with yoga to be conducted by the National Institute of Mental Health and Neuroscience (Bangaluru, India). Additional studies on the benefits of yoga, such as for bronchial asthma,15 were conducted at the Swami Vivekananda Yoga Research Foundation (SVYASA, Bengaluru, India; www.svyasa.org) followed by an increase in public awareness on the Indian subcontinent through the teachings of Swami Ramdev.16 To strengthen and encourage yoga research in India, the government has actively funded projects and established the Central Council for Research in Yoga and Naturopathy.
In the last several decades, the millions of practitioners and the rise of yoga studios have popularized yoga in the West as a holistic wellness approach. A recent report by the U.S. Department of Health and Human Services indicates a doubling of yoga use among adults between 2002 and 2012.17 Concurrently, the field of yoga and yoga therapy research has emerged as a compelling option within integrative medicine in the United States. In 1998, the National Institutes of Health in the United States established the National Center for Complementary and Integrative Health (www.nccih.nih.gov) to determine the role and safety of alternative therapies, such as yoga, for improving the nation's health.18 Symposia and conferences, such as the International Association of Yoga Therapists' Symposium on Yoga Research (www.iayt.org/?page=ConferenceLanding), have emerged for the purpose of sharing ongoing research and networking among yoga researchers around the world. The Academic Consortium for Integrative Medicine & Health (www.imconsortium.org/), a group currently composed of almost 60 academic medical centers, has been established in response to the growing demand for integrative medicine in health care delivery, such as yoga for symptomatic treatment of clinical conditions. Finally, mind-body practices, including yoga, are cost-effective by reducing unnecessary procedures and the number of hospital visits.19
In light of the growing interest in the therapeutic benefits and cost-effectiveness of yoga for prevention and alleviation of symptoms related to disease, the need for more evidence has never been more pressing.20 Primary obstacles for conducting yoga research include the lack of funding and investigator training and methodologic challenges specific to yoga study design. Thus, the evidence for yoga efficacy and effectiveness is in its infancy. RCTs provide the highest standard in research design because of their rigorous internal validity and safeguards to minimize bias; however RCTs are resource intensive, may be beyond the means of the study team, and are not without limitations.2 Other study designs are important to consider, such as nonrandomized controlled or uncontrolled studies (i.e., single group), even though these are ranked lower on the hierarchy of evidence.2 These study designs are important because they provide preliminary data, help determine sample size, and help generate hypotheses for larger, future studies. Considering the early stage of yoga research, it is necessary to examine the field as a whole for available evidence.
This bibliometric review expands upon the previously published 2004 review21 by one coauthor (SBK) to showcase the growth of the field of yoga research around the world in the last decade. We focus on clinical populations to highlight the prevalence of yoga studies to alleviate disease-related symptoms. If the goal is to affect policy or change health care, this is a necessary step. Much yoga research has been published, primarily in yoga specialty journals from India, such as Yoga Mimamsa. However, because of the growing acceptance of yoga in Western medicine, the number of conventional journals and more general alternative health journal publications (i.e., those on complementary and alternative medicine) have been included. Finally, evaluating the number of studies conducted as RCTs, controlled studies, and uncontrolled studies provides an overview of the general quality of the field to date.
Methods
Data sources
A comprehensive review of major electronic databases was conducted for articles published between 1967 and 2013. Indexed online journals were searched via computerized bibliographic databases and included PubMed, PsychInfo, MEDLINE, IndMed, Indian Citation Index, Index Medicus for South-East Asia Region, Web of Knowledge, Embase, EBSCO, and Google Scholar. Nonindexed journals were searched manually, including Yoga Mimamsa and journal collections located at the National Library of Medicine (Bethesda, MD). Reference lists from relevant articles and published reviews were manually searched for additional studies. The key search words included yoga, yoga therapy, pranayama, and asana. For example, a search in PubMed used the following Mesh terms to identify relevant articles: “Yoga”[MeSH]) AND “Clinical Trial” [publication type]. In another example, key search words were searched independently in IMSEAR and IndMed by topic. The search strategies were kept broad to capture as many relevant articles as possible and then acquired abstracts were manually evaluated according to the inclusion and exclusion criteria.
Inclusion and exclusion criteria
The studies included in this bibliometric review met the definition of a clinical trial. A clinical trial is a research study designed to answer specific questions about the efficacy and effectiveness of behavioral interventions on humans with a clinical diagnosis. Study methods include quantitative, qualitative, and mixed-methods approaches. Only peer-reviewed journals where publication reprints were available were included. All languages, clinical diagnoses or symptoms related to clinical diagnoses were considered. For studies addressing a symptom related to a specific disease (e.g., insomnia in breast cancer survivors), the study was categorized under the primary disease condition. Abstracts, dissertation reports, conference proceedings, book chapters, case reports, case series, and treatment programs with minimal reported outcomes were excluded.
Types of intervention
Interventions included yoga or yoga-based techniques. All styles of yoga were included, and no distinction was made between styles. Yoga as it is expressed in India is largely based on Patanjali or Hatha yoga, which is the umbrella term for the many newly formed styles since the adoption of yoga in the West. Therefore, yoga is defined traditionally as a combination of asana, pranayama, and meditation. Studies with multimodal interventions that combine yoga plus another active treatment (e.g., cognitive-behavior therapy) were included if most of the intervention consisted of yoga. Mindfulness-based stress reduction interventions, Transcendental Meditation, Vipassana, or other meditation-only studies were not included in this review because they have been extensively reviewed elsewhere.22 Breathing exercises belonging to specific pranayama practices were included, whereas breathing exercises for visualization or relaxation were not.
Data extraction
Two authors extracted data (P.J., J.S.). Study type, journal type, country, sample size, and disease were characterized. Study type was subdivided into RCTs, nonrandomized controlled studies, and uncontrolled studies. Journal type was subdivided into yoga specialty, CAM, and traditional. Yoga specialty journals are those that specifically publish yoga articles. CAM journals publish studies on a wide range of holistic practices, including yoga. “Traditional” is reserved for journals that publish mainstream clinical research in the medical community (e.g., Journal of the American Medical Association). Total sample size was determined for all study completers in all groups. In cases where study teams published multiple articles based on the same study population (e.g., published on a subset of the data or data on the waitlist control), publications were excluded and are noted in the corresponding figures and results. The country in which the study was conducted determined the study location, or region. For example, for Indian researchers in an Indian journal conducting the study in Iran, the country classification would be Iran. Any gray area categorizations were reviewed individually, paper by paper, and categorized by consensus.
Results
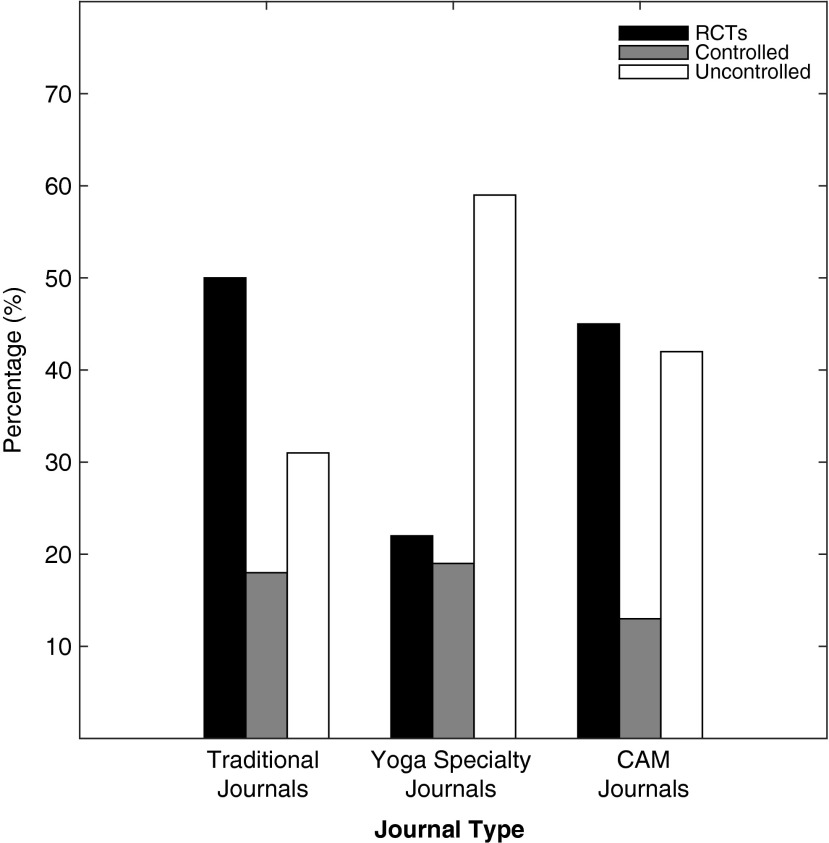
A total of 486 articles met the inclusion criteria and were published in 217 different peer-reviewed journals from 29 different countries on 28,080 study participants. A bibliography of these publications is provided in the Supplementary Appendix (Supplementary materials are available online at http://www.liebertpub.com/acm). A total of 80 articles were published in yoga specialty journals, 86 articles were published in CAM journals, and 320 were published in traditional journals. Overall, 45% of the studies published were RCTs, 18% were controlled studies, and 37% were uncontrolled studies (Fig. 1). Figure 2 depicts the type of study design published for each journal type. Publications were excluded for duplicated study designs by the same study team on the same dataset (n=27). In the traditional journals, 50% of the publications were RCTs, 31% were uncontrolled studies, and 18% were controlled studies (Fig. 2). Yoga specialty journals published more uncontrolled studies (59%) than RCTs (22%) or controlled studies (19%). In CAM journals, 45% were RCTs, 13% were controlled, and 42% were uncontrolled.
FIG. 1.
The pie chart shows the proportion of all publications (n=486) reporting randomized controlled trials (RCTs), nonrandomized controlled studies, and uncontrolled studies (i.e., no control group).
FIG. 2.
The bar chart shows the percentage of publications by journal type and study design. Duplications by study design were excluded (n=27). CAM, complementary and alternative medicine.
Total sample size was determined as all study completers (regardless of group assignment) for each study design and plotted in a histogram (bin size=25) in Figure 3. Studies that published multiple articles based on the same study group (e.g., publications for follow-up data or with separate outcomes) were not included in the distribution (n=59). Sample sizes ranged from 4 to 621 in 427 studies, with the exception of 1 study with 2522 participants, which was excluded from the graphical representation. A rightward-skewed distribution was observed wherein 65% of studies (276 of 427) included a sample size of 50 participants or fewer (Fig. 3). The median value in the sample was 40. Few studies (13%) were published with sample sizes of 100 or more.
FIG. 3.
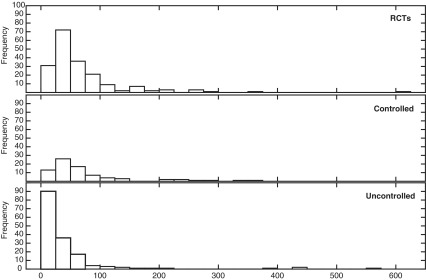
Histogram of sample size by study design. Total sample size for each publication is plotted (bin size=25). Publications with duplicate sample size were excluded (n=59).
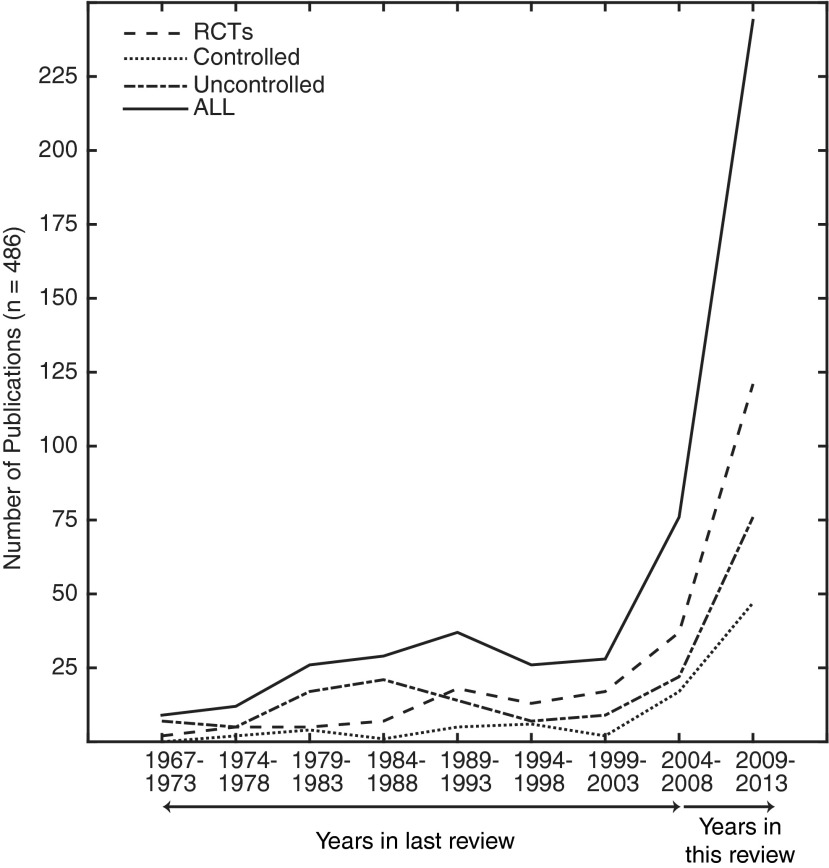
Publication years span from 1967 to 2013 and are plotted in Figure 4 in increments of 5 years (with the exception of 1967–1973). The total number of publications increased slowly until the turn of the century, when the number publications increased from 28 total publications between 1999 and 2003 to 76 total publications between 2004 and 2008, followed by a sharp increase (almost triple) in the total number of publications to 243 between 2009 and 2013. Most total publications during this last time interval were RCTs.
FIG. 4.
Number of publications for every 5-year increment (with the exception of 1967–1973) for all journals and for each study design.
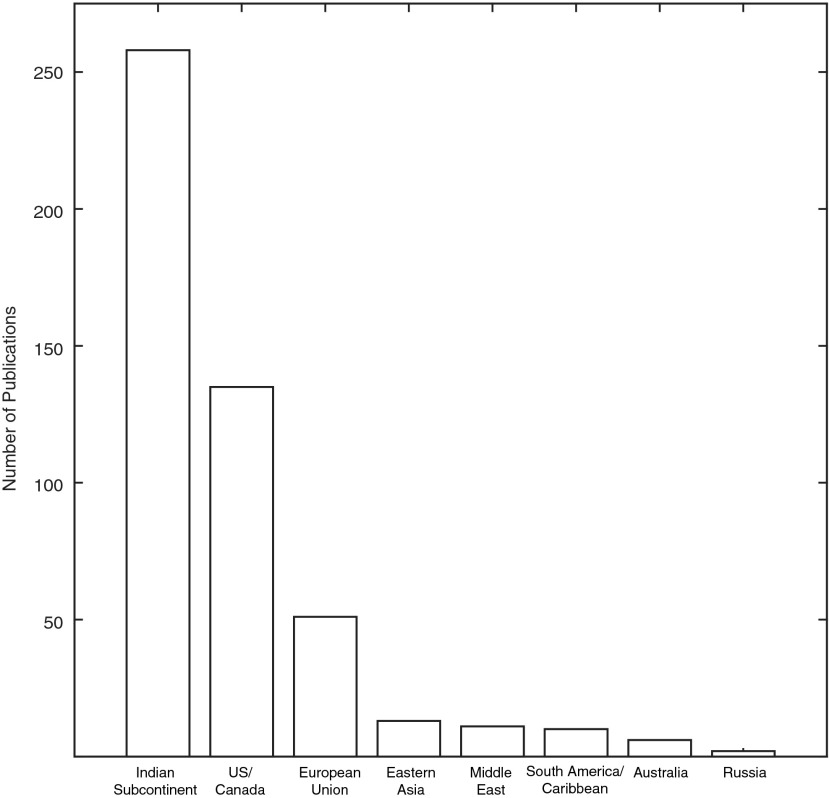
Investigators from India produced a total of 258 publications on yoga as a therapeutic intervention between 1967 and 2013, followed by 135 publications from the United States (122) and Canada (13) and 51 publications from the European Union (22 in the United Kingdom and 10 from Germany) (Fig. 5). The remainder of the publications (42 of 486) spanned the globe from eastern Asia (13), the Middle East (11), South America/Caribbean (10), Australia (6), and Russia (2) (Fig. 5).
FIG. 5.
Number of publications by region.
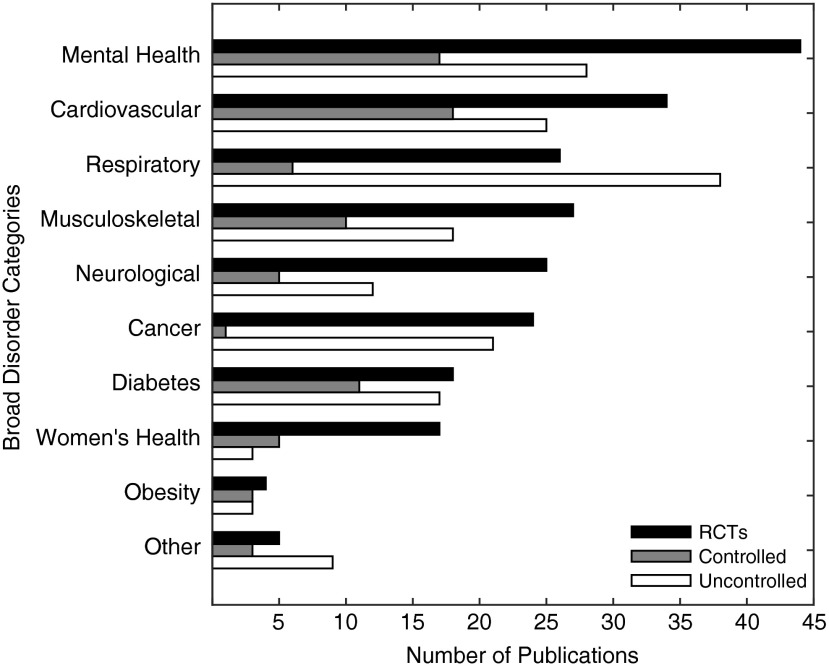
Individual disease type from each study was assigned to a broad disorder category, shown in Figure 6. Studies reporting on multiple diseases in their single study cohort were excluded (n=9). The top three disorders addressed by yoga interventions were mental health, cardiovascular disease, and respiratory disease. Yoga for mental health disorders makes up the majority of publications. Mental health disorders include anxiety, depression, post-traumatic stress disorder, schizophrenia, and addiction, among other psychopathologic diseases. Hypertension and heart disease were the main conditions studied in the cardiovascular category. Of all respiratory studies, 79% of the studies dealt with asthma. Musculoskeletal disorders ranked fourth, with 38% of the studies dedicated to arthritis-related conditions and 22% addressing chronic low back pain (only 2% of the total 487 studies).
FIG. 6.
Number of publications categorized into broad disorders by study design. Publications with multiple disorders were excluded (n=9).
Discussion
In this updated bibliometric review, the available publications on yoga research were assembled for clinical populations between 1967 and 2013. A total of 486 publications, inclusive of the initial bibliometric review from 2004,21 were identified from various sources and from several regions worldwide. The primary result in the current review is the three-fold increase in number of publications seen in the last decade, signaling that yoga research is a field undergoing substantial growth and interest. The distribution of publications by study design, region, and journal type were qualitatively similar to that reported in the 2004 paper.21 The surge in publications has occurred in parallel with an increase in healthy U.S. adults practicing yoga (approximately 21 million) according to the 2012 National Health Interview Survey.17
The hierarchy of evidence ranks RCTs above controlled studies, followed by uncontrolled designs as determined by methodologic constraints and bias-minimization procedures.2 In this review, 45% of all publications were RCTs; 37% were uncontrolled studies. Thus, the quality of the research as determined by this simplified categorization is limited in scope. However, it is worthwhile noting that approximately 50% of RCTs and publications were published in traditional journals, suggesting that the mainstream medical literature is beginning to explore the plausibility of complementary and integrative therapies in practice. In contrast, yoga studies in yoga specialty journals were mostly uncontrolled designs (i.e., single-group trials) (59%) and thus are limited in validity. This finding is consistent with reports showing that studies not published in major databases and in certain countries correlate with poorer methodologic quality23 and have shown evidence of publication bias.24
Studies conducted in India accounted for almost 50% (n=258) of the publications to date, while the studies in the United States and Canada accounted for almost a third (n=135) of the publications in this review. A similar bibliometric analysis that analyzed yoga RCTs in all populations reported 170 publications from India and 98 from the United States.25 The disparity is likely due to differences in the inclusion and exclusion criteria: only diseased participants in this study versus both diseased and healthy populations in that study. In addition, journal publications from India are more difficult to access because many are not indexed. This review was able to include prominent but less well internationally known Indian journals, such as Yoga Mimamsa, which are not easily accessible to the western research community. Without a systematic review and meta-analysis, it is difficult to determine the overall validity and bias in these publications. It is possible that earlier studies did not adhere to more recent reporting standards set forth by the Consolidated Standards of Reporting Trials (CONSORT),26 further limiting our interpretation of publications reported.
Determining the appropriate sample size is essential for all clinical trials. Conducting a study with the appropriate sample size affords confidence that the study is powered to detect a significant result.27 Most studies in this review (65%) included a sample of 50 participants or fewer (not including duplicate studies). While many factors, such as significance level, power, and treatment-specific effect size, determine the sample size for a given study, RCTs generally require more than 50 participants to determine a clinically relevant difference.28 One common constraint in yoga research studies is the limitations in funding, time, and additional resources that restrict the number of participants in a study. It is important to consider all the variables in determining the value of the information provided from a study.
The number of good-quality studies adds to the repository of evidence that determine the therapeutic benefits of yoga on symptomatic treatment of clinical conditions. Summary findings, such as systematic reviews and meta-analyses, rely on the available literature in a given field. Most publications were dedicated to mental health and cardiovascular disease. Coincidentally, an overview of systematic reviews for any medical condition identified unanimous positive evidence for depression and cardiovascular risk reduction29 and mixed results for other conditions. It's possible that the total number of publications in the other conditions in the review were not sufficient to provide a good synthesis of the evidence to draw any definitive conclusions. A separate review concluded that yoga may be a beneficial complementary therapy to many mental and physical health conditions, although more good-quality evidence is needed.30
The third major category of yoga publications was dedicated to respiratory conditions, in particular asthma, and similarly a separate systematic review suggested that yoga might be an ancillary intervention for asthma in conjunction with usual care.31 The fourth major category in the broad disorders involved musculoskeletal disorders. Considering the attention yoga is gaining for chronic low back pain in the United States,32 it is surprising that only 2% of the total number of studies were dedicated to this disorder. Finally, the use of yoga to mitigate symptoms related to cancer treatment (primarily in breast cancer survivors) has surged recently, with most publications published in only the last 10–15 years.33
This review is not without limitations. Even though a thorough literature search was conducted to the best of the authors' ability, it is likely that not all publications were acquired. The journals that were not obtained are unlikely to have studies with rigorous research design,with validated outcome measures, and that conform to the expected norms for acceptable research. This is a bibliometric review and therefore did not assess bias and validity. Minimally, the “quality” can be surveyed on the basis of a simple characterization of study design. Different styles of yoga were not distinguished because all yoga practices are rooted from a single system and differ only in delivery, not their components (i.e., breathing, posture, meditation). In so much as a “yoga prescription” is delivered, it may be important to consider the condition and thus determine the best approach. For example, patients with restricted range of motion (e.g., stroke) may benefit from yoga that focuses on alignment and slow movements by using props (e.g., chair) wherein students may only do a few poses at a time, holding each for an extended period. Alternatively, patients with cardiovascular or mental health issues may benefit from a more dynamic yoga practice.
Despite the promising increase in yoga publications in the last decade, the research field faces a formidable challenge. Good study design dictates the use of a standardized yoga protocol for the treatment arm in an RCT to determine efficacy/effectiveness and in most cases is applied to a homogenous study population, limiting generalizability to the population at large. However, in clinical practice, yoga “therapy” is tailored to the individual need as determined by the heterogeneous presentation of symptoms and severity of disease. Determining what kind of yoga to administer for a specific condition or patient remains an open question and major challenge for evidence-based integrative medicine.
In conclusion, publications on yoga to mitigate disease-related symptoms in clinical populations have surged despite challenges facing the field of yoga research, which include standardization and limitations in funding, time, and resources. The population at large has observed a parallel surge in the use of yoga outside of clinical practice. The use of yoga as a complementary therapy in clinical practice may lead to health benefits beyond traditional treatment alone. However, to effect changes in health care policy, more good-quality, evidence-based research is needed.
Supplementary Material
Acknowledgments
The authors are indebted to Shirley Telles (Patanjali Research Foundation, Haridwar, India) for coordinating assistance in the project. This study was funded in part by Mr. Shekhar Agrawal, president of the Patanjali Yogpeeth Trust (PYP USA).
Author Disclosure Statement
No personal or financial interests exist, but all the authors are involved in both yoga practice and yoga research.
References
- 1.Iyengar BKS. Light on Yoga. New York: Schocken, 1995 [Google Scholar]
- 2.Lewith GT, Jonas WB, Walach H, eds. Clinical Research in Complementary Therapies: Principles, Problems and Solutions. London: Churchill Livingston, 2012 [Google Scholar]
- 3.Cummings NA, VandenBos GR. The twenty years Kaiser-Permanente experience with psychotherapy and medical utilization: Implications for national health policy and national health insurance. Health Policy Q 1981;1:159–175 [PubMed] [Google Scholar]
- 4.Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care - incidence, evaluation, therapy, and outcome. Am J Med 1989;86:262–266 [DOI] [PubMed] [Google Scholar]
- 5.Charmandari E, Tsigos C, Chrousos G. Endocrinology of the stress response. Annu Rev Physiol 2005;67:259–284 [DOI] [PubMed] [Google Scholar]
- 6.Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K. Yoga for anxiety: a systematic review of the research evidence. Br J Sports Med 2005;39:884–891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pilkington K, Kirkwood G, Rampes H, Richardson J. Yoga for depression: the research evidence. J Affect Disord 2005;89:13–24 [DOI] [PubMed] [Google Scholar]
- 8.Cramer H, Lauche R, Langhorst J, Dobos G. Yoga for depression: a systematic review and meta-analysis. Depress Anxiety 2013;30:1068–1083 [DOI] [PubMed] [Google Scholar]
- 9.Riley KE, Park CL. How does yoga reduce stress? A systematic review of mechanisms of change and guide to future inquiry. Health Psychol Rev 2015;April 15:1-18 [DOI] [PubMed] [Google Scholar]
- 10.Benson H. The Relaxation Response. New York: Morrow, 1975 [Google Scholar]
- 11.Anand BK, Chhina GS, Singh B. Studies on Shri Ramanand yogi during his stay in an air-tight box. Ind J Med Res 1961;49:82–89 [PubMed] [Google Scholar]
- 12.Wenger MA, Bagchi BK, Anand BK. Experiments in India on ‘voluntary’ control of the heart and pulse. Circulation 1961;24:1319–1325 [DOI] [PubMed] [Google Scholar]
- 13.Patel C. Randomised controlled trial of yoga and biofeedback in management of hypertension. Lancet 1975;2:93–95 [DOI] [PubMed] [Google Scholar]
- 14.Patel C. 12-month follow-up of yoga and bio-feedback in the management of hypertension. Lancet 1975;1:62–64 [DOI] [PubMed] [Google Scholar]
- 15.Singh V, Wisniewski A, Britton J, Tattersfield A. Effect of yoga breathing exercises (pranayama) on airway reactivity in subjects with asthma. Lancet 1990;335:1381–1383 [DOI] [PubMed] [Google Scholar]
- 16.Anand AC. Swami Ramdev and scientific medicine: losing is fine, but the lesson should not be lost! Natl Med J Ind 2007;20:256–259 [PubMed] [Google Scholar]
- 17.Clarke TC, Black LI, Stussman B J, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl Health Stat Rep 2015;1–16 [PMC free article] [PubMed] [Google Scholar]
- 18.National Center for Complementary and Integrative Health. NCCIH at a Glance. Online document at: https://nccih.nih.gov/about/ataglance, accessed July14, 2015
- 19.Sobel DS. The cost-effectiveness of mind-body medicine interventions. Prog Brain Res 2000;122:393–412 [PubMed] [Google Scholar]
- 20.Khalsa SBS. Why do yoga research: who cares and what good is it? Int J Yoga Ther 2007;17:19–20 [Google Scholar]
- 21.Khalsa SBS. Yoga as a therapeutic intervention: a bibliometric analysis of published research studies. Ind J Physiol Pharmacol 2004;48:269–285 [PubMed] [Google Scholar]
- 22.Goyal M. Singh S, Sibinga EMS, et al. . Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med 2014;174:357–368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Linde K, Jonas WB, Melchart D, Willich S. The methodological quality of randomized controlled trials of homeopathy, herbal medicines and acupuncture. Int J Epidemiol 2001;30:526–531 [DOI] [PubMed] [Google Scholar]
- 24.Vickers A, Goyal N, Harland R, Rees R. Do certain countries produce only positive results? A systematic review of controlled trials. Control Clin Trials 1998;19:159–166 [DOI] [PubMed] [Google Scholar]
- 25.Cramer H, Lauche R, Dobos G. Characteristics of randomized controlled trials of yoga: a bibliometric analysis. BMC Complement Alternat Med 2014;14:1–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moher D, Hopewell S, Schulz KF, et al. . CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c869–c869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Noordzij M, Tripepi G, Dekker FW, Zoccali C, Tanck MW, Jager KJ. Sample size calculations: basic principles and common pitfalls. Nephrol Dial Transplant 2010;25:1388–1393 [DOI] [PubMed] [Google Scholar]
- 28.Whitley E, Bal J. Statistics review 4: sample size calculations. Crit Care 2002;6:335–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ernst E, Lee MS. How effective is yoga? A concise overview of systematic reviews. Focus Alternat Complement Ther 2010;15:274–279 [Google Scholar]
- 30.Bussing A, Michalsen A, Khalsa SBS, Telles S, Sherman KJ. Effects of Yoga on mental and physical health: a short summary of reviews. Evidence Based Complement Alternat Med 2012. doi: 10.1155/2012/165410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cramer H, Posadzki P, Dobos G, Langhorst J. Yoga for asthma: a systematic review and meta-analysis. Ann Allergy Asthma Immunol. 2014;112:503–510 [DOI] [PubMed] [Google Scholar]
- 32.National Center for Complementary and Alternative Medicine. Yoga for health. Online document at: http://nccih.nih.gov/health/yoga/introduction.htm#hed3, accessed July14, 2015
- 33.Smith KB, Pukall CF. An evidence-based review of yoga as a complementary intervention for patients with cancer. Psycho-oncology 2009;18:465–475 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.