Abstract
We present a pilot study of 12 veterans diagnosed with combat-related PTSD and treated with prolonged exposure therapy (PE) via telehealth technology. A reference sample of 35 combat veterans treated with in-person PE in the same clinic is also included for a comparison. Feasibility and clinical outcomes of interest include: technical performance and practicality of the telehealth equipment, patient safety, treatment completion rates, number of sessions required for termination, and clinical outcomes. Results indicated large statistically significant decreases in self-reported pathology for veterans treated with PE via telehealth technology. Preliminary results support the feasibility and safety of the modality. Suggestions for the implementation of PE via telehealth technology are discussed.
The United States has deployed more than 1.5 million troops to Iraq or Afghanistan as part of Operations Iraqi Freedom and Enduring Freedom (OIF/OEF; Rand, 2008). Exposure to combat and long periods of sustained threat associated with OEF/OIF deployment increase risk for mental health problems, including posttraumatic stress disorder (PTSD; Hoge, Castro, Messer, McGurk, Cotting, & Koffman, 2004). Whereas a majority of troops are resilient and adjust well to post-deployment civilian life, a significant number of troops are returning with serious mental health service needs. Given the overall scale of OEF/OIF deployments, even applying the most conservative estimates for OEF-OIF-related PTSD (4-8%; Smith, Ryan, Wingard, Slymen, Sallis, Kritz-Silverstein, et al., 2008) translates into tens of thousands of troops returning with post-deployment PTSD and associated functional impairment. The Department of Veterans Affairs (VA) has been hiring additional mental health professionals and increasing emphasis on evidence-based practices in an attempt to meet the mental health needs of returning OEF/OIF personnel (U.S. House Committee on Oversight and Government Reform, 2007).
The VA is currently engaged in a nationwide effort to disseminate prolonged exposure (PE; Foa, Hembree & Rothbaum, 2007), a manualized treatment for PTSD, to VA clinicians throughout the country (U.S. Department of Veterans Affairs, 2007). Exposure-oriented therapies are effective in treating PTSD (Bradley, Greene, Russ, Dutra, & Westen, 2005; Foa, Davidson & Frances, 1999; Institute of Medicine, 2007) and support for PE has been found across a variety of settings (Foa, Hembree, Cahill, Rauch, Riggs, Feeny, et al., 2005; Foa & Rauch, 2004; Schnurr, Friedman, Engel, Foa, Shea, Chow, et al., 2007). Preliminary results and case studies of PE with OEF/OIF veterans at VA Medical Centers (VAMCs) are promising (Rauch, Defever, Favorite, Duroe, Garrity, Martis, Liberzon, 2009; Tuerk, Brady, Grubaugh, in press; Tuerk, Grubaugh, Hamner, & Foa, 2009). However, veterans living in rural areas are less likely to receive appropriate mental health interventions at their local VA community-based outpatient clinics (CBOCs) because the availability of fully trained PTSD treatment providers is limited. Accordingly, there is a compelling justification for creativity and flexibility in the delivery of PE and other evidence-based interventions.
Research indicates 60-75% of OEF/OIF veterans with mental health disorders do not seek mental health care (Hoge et al., 2004). Hoge and colleagues broadly categorize barriers to mental health care as person-based barriers, centered on a tendency to avoid perceived stigma, and geographically-based barriers, related to the proximity and availability of services. Barriers such as lack of transportation and time to travel to appointments decrease service usage. Moreover, rural veterans who can and do access mental health services in their communities often have access to fewer options (Beachler, Holloman, & Herman, 2003; New Freedom Commission on Mental Health, 2003).
To address these barriers, application of non-conventional models of service delivery to military populations has been advocated (e.g., Frueh, Monnier, Yim, Grubaugh, Hammner, & Knapp, 2007). One such method proposed is telemedicine or telehealth, which involves the use of telecommunication technology for providing assessment and treatment to patients. Psychotherapy provided via video teleconferencing, as described in the current study, is one example of telehealth. VHA has made significant investments in establishing a telehealth infrastructure and making telehealth modalities available to patients living in rural areas of the country. As a result of these efforts, demand for the modality by clinicians and patients has increased and the Committee on Veterans’ Affairs, United States House of Representatives has endorsed further development of telehealth modalities within the VA (U.S. House Committee on Veterans Affairs, 2005).
Telehealth offers a number of potential benefits as an alternative to in-person treatment (Jerome & Zaylor, 2000; Perednia & Allen, 1995). One potential benefit is lower cost without sacrificing quality of care (Morland, Frueh, Pierce, & Miyahira, 2003). Moreover, several studies demonstrate that telehealth can be applied in a cost-effective manner within VA settings (Fortney, Steffick, Burgess, Maciejewski, & Peterson, 2005). Patients also benefit from decreases in transportation costs, travel time, and lost employment (Bose, McLauren, Riley, & Mohammedali, 2001; Elford, White, Bowering, Ghandi, Maddiggan, & St.John, 2000).
The delivery of various interventions via telehealth has recently accumulated significant research support. Telehealth has now been used in the delivery of behavioral treatments, psychological assessments, social skills group treatment, and session evaluations (Alessi, 2002; Cowain, 2001; Deitsch, et al., 2000; Hilty, Sison, Nesbit, & Hales, 2000; Hyler & Gangure, 2003; Monnier et al., 2007). Telehealth has been successfully employed for individuals in rural areas (Brown, 1998; Ermer, 1999; Nesbitt et al., 2000), and for difficult-to-treat patient populations, such as the elderly (Poon et al., 2005), patients with thought disorders (Zarate, Weinstock, Cukor, Morabito, Leahy, Burns, & Baer, 1997), and avoidant/reluctant patients (Brodey, Claypoole, Motto, Arias, & Goss, 2000; Zaylor, Whitten, & Kingsley, 2000). However, to our knowledge, no studies have investigated the delivery of PE via telehealth technology.
Method
The current investigation is a proof-of-concept pilot study of PE delivered via telehealth technology, i.e., via one-on-one video conferencing (telehealth PE). For a comparison, a reference group of patients receiving traditional treatment (in-person PE) at the same clinic is also included. The sample consists of veterans diagnosed with combat-related PTSD at a VAMC in the Southeast United States. All veterans were offered in-person PE; additionally, optional access to telehealth PE was made available for patients living in rural areas, or otherwise far from the VAMC. Outcomes of interest include technical and pragmatic feasibility, patient safety, treatment completion rates, number of sessions to treatment termination, and clinical outcomes related to self-reported symptoms of PTSD and depression.
Participants
The telehealth PE and in-person PE samples consist of 47 combat veterans: 72% OEF/OIF veterans; 6% Female; 34% Black, 64% White; mean age, 39 years (SD = 16). Treatment seeking patients were identified by referrals from mental health providers and case managers to the PTSD clinical team. A PTSD diagnosis via the Structured Clinical Interview for the DSM-IV (SCID-IV; First, Spitzer, Gibbon & Williams, 1996) was established by an in-person interview with a psychiatrist before assignment to PE. Veterans living outside the VAMC metropolitan area were given the option of selecting PE (n = 12) delivered at a VA-CBOC closer to, or in, their community. All 12 veterans who were offered telehealth PE accepted it. Accordingly, no one self-selected out of the telehealth condition. Selection appeared to be based on patient preference (i.e., veterans did not choose telehealth PE to avoid long wait times for in-person appointments, as same-week appointments were offered to all veterans regardless of treatment medium). Patients receiving care at the main medical center were not offered telehealth PE, and are included here as a broad comparison group for the telehealth PE pilot study. Thirty-nine veterans were assessed and met criteria for in-person treatment at the VAMC, of which 4 (10%) were lost to follow up or otherwise did not respond to the invitation for treatment. The remaining 35 came to at least one in-person PE session. Table 1 presents patient characteristics for the telehealth PE and in-person PE samples. All patients were treated by the two primary authors (PT & MY), who are both clinical psychologists with specialized training in trauma work and PE.
Table 1.
Sample Demographics and Characteristics by Treatment Context
| PE Live n = 35 n (%) | PE via telehealth n = 12 n (%) | Total sample N = 47 n (%) | |
|---|---|---|---|
| Female | 3 (9) | 0 (0) | 3 (6) |
| Race/ethnicity | |||
| Black | 14 (40) | 2 (17) | 16 (34) |
| Hispanic | 1 (3) | 0 (0) | 1 (2) |
| White | 20 (57) | 10 (83) | 30 (64) |
| Combat theater | |||
| Desert Storm | 1 (3) | 0 (0) | 1 (2) |
| OEF/OIF | 25 (71) | 9 (75) | 34 (72) |
| Vietnam | 8 (23) | 3 (25) | 11 (24) |
| WW-II | 1 (3) | 0 (0) | 1 (2) |
| M | SD | M | SD | M | SD | |
|---|---|---|---|---|---|---|
| Age | 38.0 | 15.93 | 39.3 | 15.62 | 39.0 | 15.69 |
| Baseline | ||||||
| PCL | 60.69 | 9.54 | 61.00 | 10.58 | 60.76 | 9.64 |
| BDI | 27.79 | 9.30 | 27.33 | 12.48 | 27.68 | 9.96 |
Note. PE = Prolonged exposure therapy; PCL = PTSD Checklist; BDI = Beck Depression Inventory.
Measures
Feasibility and clinical outcomes include: the technical performance and practicality of the telehealth equipment, patient safety, treatment completion rates, number of sessions required for termination, and clinical outcomes on repeated measures of PTSD and depression given every two weeks during treatment. The measures were administered at the beginning of each odd-numbered session and on the last day of treatment. The PTSD Checklist – Military Version (PCL; Weathers, Huska, & Keane 1991) is a 17-item self-report measure of symptoms based on DSM-IV criteria. Scores range from 17 to 85 with higher scores reflecting greater PTSD severity. The instrument has good diagnostic efficiency (> .70), and robust psychometric properties (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996).
The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) is a 21- item self-report measure that assesses behavioral and affective symptoms of depression. The BDI-II demonstrates adequate convergent validity, discriminant validity, and test-retest reliability (r = .93), as well as good internal consistency (α > .92; Beck et al.; Steer & Clark, 1997).
Procedures
PE Treatment
PE (Foa et al., 2007) is a manualized treatment protocol usually delivered in 8 to 15 weekly 90-minute sessions. PE includes the following major components: (a) psychoeducation; (b) detailed rationale for exposure-oriented treatment; (c) repeated in vivo exposure to safe situations avoided due to distress; (d) repeated, prolonged imaginal exposure to traumatic memories, and (e) processing or discussion of the memories, events, and imaginal exposures. Imaginal exposure consists of patients imagining and providing a verbal description of the traumatic event/s with their eyes closed. Patients practice in vivo exposures and listen to the audio-recorded sessions as “homework” between weekly appointments.
PE Treatment via Telehealth
Telehealth patients presented to their local VA-CBOC for weekly, 90-min PE sessions conducted in a dedicated room for videoconferencing with the VAMC. Telehealth was conducted using a Tanburg 1000 MXP. The treatment regimen followed the PE protocol described above. The telehealth aspect of treatment did not appear to interfere with the clinicians' basic ability to follow the PE protocol; however there were some logistical and clinical issues that arose from the telehealth context.
First, our primary concern in delivering telehealth PE was patient safety. Pre-treatment site visits to the CBOCs were used to survey the physical premises and build relationships that would later serve to facilitate good communication between treating clinicians and CBOC staff. During each session of PE, clinicians had contact information readily available for CBOC support staff. All appointments took place during regular hours of operation; accordingly, the CBOCs were staffed with on-site mental health professionals and security personnel in case of emergencies. Notably, there were no instances in which staff needed to be contacted due to patient safety concerns.
One logistical variation in delivering PE via telehealth was the use of fax machines to convey homework, information forms, and pen and paper measures of psychopathology. Forms were faxed to support staff prior to appointments and given to patients in the waiting room. Patients then returned the self-report measures to staff at the end of the session to be faxed back to providers. During the treatment sessions, patients were asked about their responses to the assessments to track progress, since a visual inspection of the results was not available to the provider until after the session. Another pragmatic variation was the use of overnight mail to send imaginal exposure audio recordings to patients each week to be listened to as homework. In some cases, this procedural difference resulted in a delay in starting audio exposure homework for the telehealth sample relative to the in-person sample. A third logistical variation consisted of using online shared calendars to facilitate scheduling of the telehealth room between PE providers and providers of other services at the CBOC.
One clinical difference between in-person PE and telehealth PE was how resistance to in-vivo exposure exercises was handled. When encountered in traditional exposure settings, it is often helpful for the clinician to accompany a resistant patient to practice exposure within the clinic or hospital setting (Foa, Hembree, & Rothbaum, 2007); for example, by visiting the hospital cafeteria, standing in line at the gift shop, or sitting in public with the patient's back to the door. This was not possible for the telehealth group. Accordingly, in some cases, when patients had difficulty beginning in-vivo exercises on their own, it was helpful for the patients to complete the exercise while talking to the clinician on a cell phone.
Data Analysis
Qualitative description and descriptive statistics are used to describe feasibility outcomes while inferential statistics are used to investigate pre-post clinical outcomes. Pre/post clinical outcomes for the in-person PE reference sample are also provided. Potential differences between the groups are not modeled, as the study is not powered appropriately for non-inferiority analyses. The reference group is included to provide a rough comparison of telehealth treatment to traditional treatment provided by the same clinicians over the same time period. Repeated measures, dependent means t-tests are used to compare pre/post treatment effects (d-type effect sizes) for patients who attended at least five sessions of telehealth PE or in-person PE. Descriptive and clinical information about patients who did not complete at least five sessions is provided.
Results
Technical Performance of the Telehealth Equipment
There were few technical problems with the telehealth equipment. Occasionally, CBOC staff, who were using the telehealth room for multiple purposes, unplugged and moved the machine. This led to a delay in starting sessions and in some cases difficulty reconnecting. Additionally, the telehealth video feed occasionally became pixilated for 2 to 10 seconds during high traffic times. However, such interruptions did not significantly impact the flow of communication. Overall, the telehealth equipment worked properly and produced clear audio and video signals with little audio delay. Coordination between clinicians and remote staff started well and improved as working relationships developed. For example, as relationships developed, the remote staff began looking for and expecting the pre-session assessment faxes, direct phone extensions to reach treating clinicians during times of technical difficulty were memorized to facilitate more rapid communication, and the remote staff became more vigilant about making sure the telehealth equipment was not unplugged between sessions. The use of online shared calendars and readily accessible phone communication between sites was invaluable for problem solving.
Safety Issues
As noted, there were no instances in the PE telehealth condition where on-site staff had to be contacted for patient safety. Titrating of emotional reactions and patient engagement in traumatic memories, normally including anxiety, increased psychomotor activity, crying, and reexperiencing symptoms, were all handled adequately with the same protocol and clinical skills employed for in-person PE. There were no instances of patients leaving the room or otherwise inappropriately disengaging from the therapeutic communication. However, there was one instance of a patient insisting on leaving the telehealth room door open during the first five sessions due to extreme hypervigilance. The same patient also felt more comfortable leaving his eyes open during the imaginal exposures to keep a watch on his surroundings. Both of these manifestations of hypervigilance may have been more effectively assuaged with in-person interactions. However, they did not represent a threat to patient safety.
Treatment Completion & Number of Sessions
Table 1 presents baseline descriptive statistics for all patients in both samples who began treatment. The treatment completion rate for the in-person PE sample was 83% and the treatment completion rate for the telehealth PE sample was 75%. Six veterans in the in-person PE sample and 3 veterans in the telehealth-PE sample did not complete at least 5 sessions and had 2 or fewer points of measurement, and thus were labeled as non-completers. All of the patients in both samples who did not complete treatment were OEF/OIF veterans. In-person PE non-completers (n = 6) had a mean PCL baseline score of 65.3 (SD = 9.4) and a mean BDI-II baseline score of 30.0 (SD = 8.9), were 50% White, 50% Black and had a mean age of 31 (SD = 7) years. Telehealth PE non-completers (n = 3) had a mean PCL baseline score of 58.3 (SD = 11.6) and a mean BDI-II baseline score of 34.3 (SD = 12.0), were 100% White, and had a mean age of 33 (7) years.
The mean number of sessions for treatment completers was 10.1 (SD = 3.8) for the in-person PE group and 10.0 (SD = 6.3) for the telehealth PE group. The range of sessions in both groups was 1 to 21. Two patients in the in-person PE sample and 1 patient in the telehealth PE sample required more than 15 sessions to sufficiently address symptoms (additional sessions for patients with particularly long or severe trauma/s is standard clinical practice, though not the usual course of treatment).
Clinical Outcomes
As reflected in the descriptive statistics provided in Table 1, preliminary independent means t-tests revealed no clinically or statically significant differences in baseline symptom severity between the in-person PE group and the telehealth PE group. Mean pre- and post-treatment PCL scores for the in-person PE group were 60.7 (SD = 9.5) and 27.7 (SD = 6.0) respectively. This difference is clinically and statistically significant, t(28)= 16.9, p < .001, d = 4.2.. Mean pre- and post-treatment PCL scores for the telehealth PE group were 61.0 (SD = 10.6) and 34.9 (SD = 7.6). This difference is also clinically and statistically significant, t(8) = 12.3, p < .001, d = 2.9. Figure 1 displays the pre/post PCL means for both samples with 95% confidence intervals reflecting the results of the repeated measure pre/post t-tests.
Figure 1.
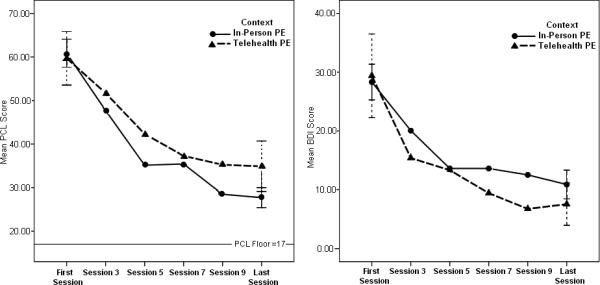
PTSD Checklist (PCL) and Beck Depression Inventory (BDI-II) outcomes by prolonged exposure (PE) treatment condition, with 95% Confidence Intervals for first and last session measurements (in-person PE, n = 29; telehealth PE, n = 9).
Mean pre- and post-treatment BDI-II scores for the in-person PE group were 27.8 (SD = 9.3) and 10.9 (SD = 6.4). This difference is clinically and statistically significant, t(28) = 8.7, p < .001, d = 2.2. Mean pre- and post-treatment BDI-II scores for the telehealth PE group were 27.3 (SD = 12.5) and 7.6 (SD = 4.7). This difference is also clinically and statistically significant, t(8) = 5.5, p < .001, d = 2.3. Figure 1 displays the pre/post BDI-II means for both samples with 95% confidence intervals reflecting the results of the repeated measure pre/post t-tests.
Discussion
PE treatment via telehealth technology was associated with large reductions in symptoms of PTSD and depression for veterans diagnosed with combat-related PTSD. In the current sample, telehealth PE treatment was safe and pragmatically viable. Treatment non-completion rates, although higher than average for our clinic, were in the acceptable range. Overall, the results of this study support the need for a large-scale randomized controlled trial.
The high acceptance rate (12 out of 12) of telehealth PE suggests that some aspects of telehealth services may be especially well suited for and attractive to veterans with PTSD. Although one of the points of treatment is to facilitate a patient's return to normal functioning, early on in the treatment process patients with PTSD may be particularly uncomfortable around crowds in waiting rooms or hospital lobbies. Accordingly, telehealth services may obviate the need for patients to overcome such anxiety on their own before having had effective treatment for it. Additionally, many veterans from the wars in Iraq and Afghanistan feel uncomfortable traveling long distances by car due to lingering fears of improvised explosive devices on the roads. Receiving services locally may increase their willingness to engage in treatment. Finally, many veterans with PTSD spend significant time and energy avoiding reminders of their trauma and war; large VA medical centers contain many trauma-related cues, e.g., uniforms, evidence of injury, war-related art work, and other veterans. Consequently, receiving services at smaller, local CBOCs may be more appealing to such veterans. At this point it is unclear if these concerns contributed to the 100% initial acceptance rate of telehealth services in the current pilot study.
Although outcomes across both samples appear roughly similar, there are at least three potentially important areas in need of further investigation. First, as noted, non-completion rates were slightly higher in the telehealth PE sample. Second, non-completers in the in-person PE sample, though not in the telehealth PE sample, self-reported relatively more PTSD-related distress at baseline. Lastly, although confidence intervals for PCL scores overlap at post-treatment for both samples, there is a notable variation in effects sizes between the samples (in-person PE, d = 4.25; telehealth PE, d = 2.88). This variation may be of note even though both effect sizes are considered large by accepted standards (Cohen, 1988). In the current samples, variation between the two effect sizes is in part influenced by higher standard deviations in the telehealth sample as compared to the in-person sample. Although the observed difference in effect sizes cannot solely be attributed to differences in standard deviations, it is unclear if the smaller effect size in the telehealth condition is a reliable finding or clinically significant. The current study is not powered appropriately for non-inferiority analyses and therefore conclusions cannot be made regarding the observed differences in effect sizes. Moreover, all three distinctions highlighted above are difficult to interpret given the small sample size of the telehealth pilot sample. However, regardless of descriptive comparisons between in-person and telehealth PE, the current study did reveal that veterans who received PE via telehealth showed large clinically and statistically significant reductions in self-reported PTSD pathology over the course of their treatment, with most subjects scoring within or near the normal range on the two primary measures at post-treatment. The pilot study also revealed that telehealth delivered PE can be conducted safely by properly trained clinicians.
The current study noted both logistical and clinical distinctions between delivering in-person PE and telehealth PE. These distinctions include the use of fax machines and mail to facilitate the exchange of materials, shared online calendars for scheduling, and the use of cell phones for patient support. Another difference was how severe clinical presentations were handled across both treatment contexts. For example, the PE protocol calls for patients to close their eyes while engaged in imaginal exposure to foster a vivid revisiting of the traumatic event/s. Occasionally, hypervigilant patients express unwillingness to close their eyes, in order to stay alert and on guard at all times. In live contexts, PE providers can encourage such patients by providing a reminder that they are also in the room and can watch out for any potential threats (however unlikely) during imaginal exposure. This option, and others like it, are not available in a telehealth context and call for clinical flexibility, strong rapport-building skills, and creativity. Additionally, practicing in vivo exposures in the medical center milieu during sessions with patients who are reticent or confused about how to start in vivo exposures was done via cell phones within the telehealth context. Such clinical variations are only relevant for patients with more severe symptom expression. The PE protocol sufficiently addresses modest resistance via reiteration of the treatment rationale, which is provided easily over the telehealth medium. At this point, it is unclear whether these variations are significant enough to merit the development and validation of a modified PE protocol specifically designed for telehealth.
The current pilot study did not randomize subjects to treatment condition; patients were allowed to choose the telehealth condition within the natural ecology of their treatment. Another limitation is that sessions were not coded for treatment fidelity. However this limitation is somewhat mitigated because the primary author is a designated consultant for PE in the VA dissemination effort, has completed training in the supervision of PE, and participates in bimonthly supervision with the developers of PE regarding training and adherence to the PE treatment model. A third limitation is that self-report instruments, rather than standardized clinical interviews, were used to assess clinical outcomes. However, the large effect sizes reported here (d = 2.15 - 4.25) and highly significant p-values (p < .001), as well as the pattern of change over time, increase confidence that improvement in symptoms was being conveyed by patients over the course of treatment. Moreover, the self-report measures used have good reliability and correlate well with clinical interviews.
Our experience in piloting telehealth PE leads us to offer the following suggestions to researchers interested in studying the modality: (a) Given appropriate safety precautions there appears to be little justified reason to fear harming patients in a large-scale RCT of telehealth PE, while at the same time, there appears to be much potential benefit for patients; accordingly, inclusion criteria need not be overly stringent or exclusionary; (b) Appropriate safety precautions include available on-site mental health providers and security staff who can be contacted at the patient end if needed, clinician access to direct phone numbers for such staff, and ongoing assessment of self harm, and suicidal and homicidal ideation; (c) Patients who present with more severe symptoms or extreme hypervigilance may be harder to treat via telehealth and researchers should consider this question when designing studies and evaluating outcomes; (d) When recruiting patients, clinicians should present the modality in positive terms, such as “cutting edge,” stressing the convenience and innovation of the modality, rather than as a second-class alternative to in-person treatment; (e) Taking the time to visit and develop working relationships with support staff at CBOCs or other satellite clinics is invaluable to obtaining their necessary assistance, as the modality will likely require more work from them and can be unintentionally sabotaged by overworked support staff with little “buy-in;” (f) PE offers much opportunity for rapport building, warmth, instilling of hope, and the development of teamwork; these “non-specific” factors of treatment are essential in helping patients engage with the active components of treatment and should be at the forefront of telehealth services and clinical supervision.
It is likely that the current increasing demand for mental health services in VA and Department of Defense settings will require the implementation of treatments that have not been adequately investigated. Or, as in the current study, that treatments with adequate empirical support will be modified or otherwise flexibly implemented in an attempt to meet the needs of veterans. While the scale of the current situation poses challenges to both service providers and veterans, it also presents unprecedented opportunities for scientific investigation and the continued development of evidence based interventions for PTSD.
Acknowledgments
Dr. Tuerk is supported by an SCTR K12 Career Development Award. Drs. Acierno and Ruggiero are supported by Department of Defense grant W81XWH-07-PTSD-IIRA (PI: Acierno). Dr. Acierno is also supported by VA HSR&D Merit grant IIR-04-421 (PI: Egede). Dr. Ruggiero is also supported by a VA (VISN-7) research career development award. Views in this article do not represent those of the funding agencies.
References
- Alessi NE. Telepsychiatric care for a depressed adolescent. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:894–895. doi: 10.1097/00004583-200208000-00004. [DOI] [PubMed] [Google Scholar]
- Beachler M, Holloman C, Herman J. Southern rural access program: An overview. Journal of Rural Health. 2003;19:301–307. doi: 10.1111/j.1748-0361.2003.tb01048.x. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer R, Brown G. Manual for Beck Depression Inventory-II. Psychological Corporation; San Antonio, Tex: 1996. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL). Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bose U, McLauren P, Riley A, Mohammedali A. The use of telepsychiatry in the brief counseling of non-psychotic patients from an inner London general practice. Journal of Telemedicine & Telecare. 2001;7:S8–S10. doi: 10.1177/1357633X010070S103. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta- analysis of psychotherapy for PTSD. American Journal of Psychiatry. 2005;162:214–227. doi: 10.1176/appi.ajp.162.2.214. [DOI] [PubMed] [Google Scholar]
- Brodey BB, Claypoole KH, Motto J, Arias RG, Goss R. Satisfaction of forensic psychiatric patients with remote telepsychiatric evaluation. Psychiatric Services. 2000;51:1305–1307. doi: 10.1176/appi.ps.51.10.1305. [DOI] [PubMed] [Google Scholar]
- Brown FW. Rural telepsychiatry. Psychiatric Services. 1998;49:963–964. doi: 10.1176/ps.49.7.963. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Lawrence Erlbaum Associates; New Jersey: 1988. [Google Scholar]
- Cowain T. Cognitive-behavioural therapy via videoconferencing to a rural area. Australian & New Zealand Journal of Psychiatry. 2001;35:62–64. doi: 10.1046/j.1440-1614.2001.00853.x. [DOI] [PubMed] [Google Scholar]
- Deitsch S, Frueh B, Santos A. Telepsychiatry for post-traumatic stress disorder. Journal of Telemedicine & Telecare. 2000;6:184–186. doi: 10.1258/1357633001935194. [DOI] [PubMed] [Google Scholar]
- Elford R, White H, Bowering R, Ghandi A, Maddiggan B, St.John K. A randomized control study of child psychiatric assessments conducted using videoconferencing. Journal of Telemedicine & Telecare. 2000;6:73–82. doi: 10.1258/1357633001935086. [DOI] [PubMed] [Google Scholar]
- Ermer D. Experience with a rural telepsychiatry clinic for children and adolescents. Psychiatric Services. 1999;50:260–261. doi: 10.1176/ps.50.2.260. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I disorders. Biometrics Research Department, New York State Psychiatric Institute; New York: 1996. [Google Scholar]
- Foa EB, Davidson JRT, Frances A. The expert consensus series: Treatment of posttraumatic stress disorder. Journal of Clinical Psychiatry. 1999;60:4–76. [Google Scholar]
- Foa EB, Hembree EA, Rothbaum BO. Prolonged exposure therapy for PTSD: Emotional processing of traumatic experiences, Therapist Guide. Oxford University Press; New York, NY: 2007. [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SA, Riggs DS, Feeny NC, et al. Randomized study of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Rauch SA. Cognitive changes during prolonged exposure versus prolonged exposure plus cognitive restructuring in female assault survivors with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2004;72:879–884. doi: 10.1037/0022-006X.72.5.879. [DOI] [PubMed] [Google Scholar]
- Fortney J, Steffick D, Burgess J, Jr, Maciejewski M, Peterson L. Are primary care services a substitute or complement for specialty & inpatient services? Health Services Research. 2005;40:1422–1442. doi: 10.1111/j.1475-6773.2005.00424.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frueh BC. PTSD and Vietnam veterans. Science. 2007;315:184–187. [PubMed] [Google Scholar]
- Frueh BC, Monnier J, Yim E, Grubaugh AL, Hamner MB, Knapp RG. A randomized study of telepsychiatry for post-traumatic stress disorder. Journal of Telemedicine & Telecare. 2007;13:142–147. doi: 10.1258/135763307780677604. [DOI] [PubMed] [Google Scholar]
- Hilty D, Sison J, Nesbitt T, Hales R. Telepsychiatric consultation for ADHD in the primary care setting. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:15–16. doi: 10.1097/00004583-200001000-00009. [DOI] [PubMed] [Google Scholar]
- Hoge C, Castro C, Messer S, McGurk D, Cotting D, Koffman R. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hyler S, Gangure D. A review of the costs of telepsychiatry. Psychiatric Services. 2003;54:976–980. doi: 10.1176/appi.ps.54.7.976. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . Treatment of posttraumatic stress disorder: An assessment of the evidence. National Academy of Sciences. Retrieved March; Washington, DC: 2007. 2009 from the World Wide Web: http://books.nap.edu/catalog.php?record_id=11955#toc. [Google Scholar]
- Jerome L, Zaylor C. Cyberspace: Creating a therapeutic environment for telehealth applications. Professional Psychology Research and Practice. 2000;31:478–483. [Google Scholar]
- Morland L, Frueh B, Pierce K, Miyahira S. PTSD & telemental health: Updates & future directions. National Center for PTSD Clinical Quarterly. 2003;12:1–5. [Google Scholar]
- Nesbitt T, Hilty D, Kuenneth C, Siefkin A. Development of a telemedicine program: A review of 1,000 videoconferencing consultations. Western Journal of Medicine. 2000;173:169–174. doi: 10.1136/ewjm.173.3.169-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New Freedom Commission on Mental Health . Achieving the promise: Transforming mental health care in America. Final report. Rockville, MD: US.: 2003. DHHS Pub. No.SMA-03-3832. [Google Scholar]
- Perednia DA, Allen A. Telemedicine technology & clinical applications. Journal of the American Medical Association. 1995;27:483–488. [PubMed] [Google Scholar]
- Poon P, Hui E, Dai D, Kwok T, Woo J. Cognitive intervention for community-dwelling older persons with memory problems: Telemedicine versus face-to-face treatment. International Journal of Geriatric Psychiatry. 2005;20:285–286. doi: 10.1002/gps.1282. [DOI] [PubMed] [Google Scholar]
- Rand Center for Military Health Policy . Invisible wounds of war: Summary and recommendations for addressing psychological and cognitive injuries. Arlington, VA: U.S.: 2008. Document Number: MG-720/1-CCF; ISBN/EAN: 9780833044532. [Google Scholar]
- Rauch SAM, Defever E, Favorite T, Duroe A, Garrity C, Martis B, Liberzon I. Prolonged exposure for PTSD in a Veterans Health Administration PTSD Clinic. Journal of Traumatic Stress. 2009;22(1):60–64. doi: 10.1002/jts.20380. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, et al. Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled study. Journal of the American Medical Association. 2007;297:820–830. doi: 10.1001/jama.297.8.820. [DOI] [PubMed] [Google Scholar]
- Smith T, Ryan M, Wingard D, Slymen D, Sallis J, Kritz-Silverstein D, Millennium Cohort Study Team New onset and persistent symptoms of post-traumatic stress disorder self reported after deployment and combat exposures: Prospective population based US military cohort study. British Medical Journal. 2008;336:366–71. doi: 10.1136/bmj.39430.638241.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steer RA, Clark DS. Psychometric properties of the Beck Depression Inventory-II with college students. Measurement and Evaluation in Counseling and Development. 1997;30:128–136. [Google Scholar]
- Tuerk PW, Brady KT, Grubaugh AL. Clinical case discussion: PTSD and alcohol dependence. Journal of Addiction Medicine. doi: 10.1097/ADM.0b013e3181a9d276. in press. [DOI] [PubMed] [Google Scholar]
- Tuerk PW, Grubaugh A, Hamner MB, Foa EB. Diagnosis and treatment of PTSD-related compulsive checking behaviors in veterans of the Iraq war: The influence of military context on the expression of PTSD symptoms. American Journal of Psychiatry. 2009;166:762–767. doi: 10.1176/appi.ajp.2009.08091315. [DOI] [PubMed] [Google Scholar]
- [January 5, 2009];U.S. Department of Veterans Affairs, Research and Development Press Release. 2007 from the World Wide Web: http://www.research.va.gov/resdev/news/press_releases/ptsd-101807.cfm.
- U.S. House Committee on Oversight and Government Reform . Statement of Antonette Zeiss. Deputy Chief Consultant, Office of Mental Health ervices, Department of Veterans affairs; May 24, 2007. [January 5, 2009]. from the World Wide Web: http://www.va.gov/OCA/testimony/hgrc/070524AZ.asp. [Google Scholar]
- U.S. House Committee on Veterans’ Affairs, United States House of Representatives [March 20, 2009];Veteran's Health Care: E-Health and Telemedicine. 2005 May 18; from the World Wide Web: http://www.house.gov/sites/comms/veterans_dem/health/ehealtele.html.
- Weathers F, Huska J, Keane T. The PTSD Checklist Military Version (PCL-M) National Center for PTSD; Boston, MA: 1991. [Google Scholar]
- Zarate C, Jr, Weinstock L, Cukor P, Morabito C, Leahy L, Burns C, et al. Applicability of telemedicine for assessing patients with schizophrenia: Acceptance and reliability. Journal of Clinical Psychiatry. 1997;58:22–25. doi: 10.4088/jcp.v58n0104. [DOI] [PubMed] [Google Scholar]
- Zaylor C, Whitten P, Kingsley C. Telemedicine services to a county jail. Journal of Telemedicine & Telecare. 2000;6:S93–S95. doi: 10.1258/1357633001934294. [DOI] [PubMed] [Google Scholar]


