This article is the first in the series “International Perspectives on Pharmacy Practice”. For general information about the series, see the article elsewhere in this issue: Raman-Wilms L, Moles RJ. Widening our horizons: pharmacy practice from a global perspective. Can J Hosp Pharm. 2015;68(5):417.
WHO Region: The Western Pacific
Country: Australia
INTRODUCTION
The Commonwealth of Australia is one of the wealthiest countries in the Western Pacific region, with a population estimated at over 23 million in 2013.1 About 27% of the population were born overseas, predominantly in the United Kingdom, New Zealand, China, and India,2 and 3% of the population are Indigenous Australians.3 Despite the country’s geographic size, Australia’s population is substantially lower than that of other regions of similar size4 because of a large, uninhabitable central desert. Australia is divided into 6 states and 2 major mainland territories (Figure 1); in most respects, the 2 territories function as states.
Figure 1.
Map of Australia, showing states and territories.
According to the Australian Bureau of Statistics, life expectancy is among the highest in the world and 25 years longer than a century ago. A baby boy born between 2010 and 2012 can expect to live to 79.9 years of age and a baby girl to 84.3 years;3 however, life expectancy for the Indigenous population is 10.6 years less for boys and 9.5 years less for girls. Like most developed nations, Australia has experienced a drop in birth rate and infant mortality. More specifically, infant mortality rates have fallen from 65.7 to 3.3 deaths per 1000 live births over the past 85 years.5,6 Decreased birth rates coupled with increased life expectancy mean that Australia exemplifies global trends, with an expanding older population.
As in most developed countries, chronic conditions such as cardiovascular disease, cancer, chronic obstructive pulmonary disease, and diabetes mellitus are the leading causes of illness and health burden in Australia.3 Unsurprisingly, the leading cause of death in both men and women is coronary artery disease, which accounts for about 15% of all deaths, followed by stroke, dementia, and lung cancer.5
The multicultural nature of Australia’s population, the aging population, and the burden of chronic conditions present unique challenges to the Australian health sector. These challenges have opened new practice opportunities for pharmacists, discussed later in this article.
HEALTH SYSTEM LEADERSHIP/GOVERNANCE AND HEALTH CARE FINANCING
Australia has both public and private health care systems, which operate side by side. Public sector health services are provided by all levels of government (local, state or territorial, national) and include public hospitals, visits to clinics, and visits to general practitioners. Private sector health service providers include private hospitals, medical practices, and community pharmacies.
With respect to patient information, the public and private sectors currently function as stand-alone operations. Unlike some other countries, Australia has yet to successfully implement a national electronic patient record system.7 Nonetheless, in the community setting most prescribing is now electronic, and patient records are kept electronically (although cannot be accessed by health care professionals outside of the particular practice), with hospitals starting to follow suit. Electronic medication charts are slowly being phased in, with intensive care units being the first to introduce this technology.
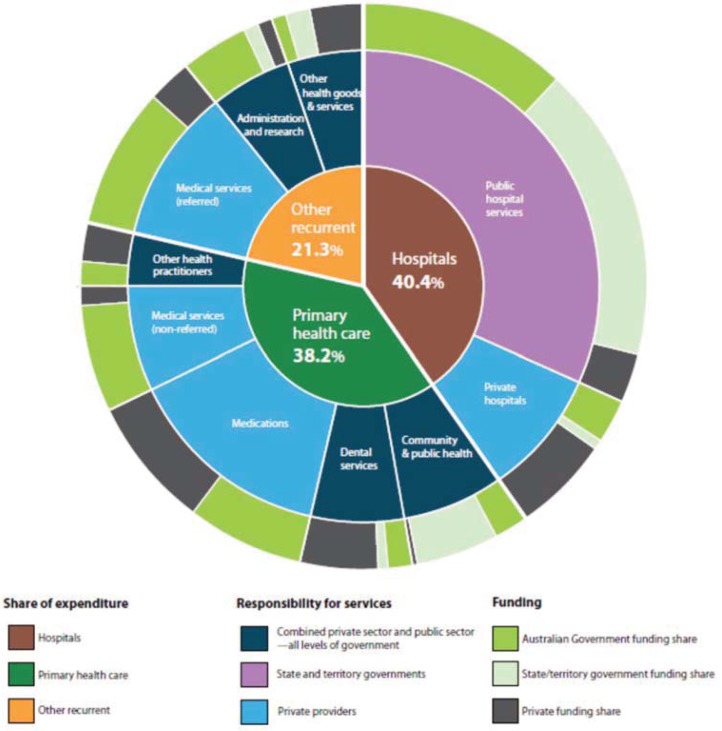
The Australian health care funding systems aim to provide timely and affordable access to quality health care and medications but are by no means simple. Figure 2 illustrates the complexity of the health funding systems in Australia.3
Figure 2:
Health services and funding in Australia.3 Source: Australian Institute of Health and Welfare.
PHARMACEUTICAL BENEFITS SCHEME, MEDICARE, AND OTHER FUNDS
The main sources of health care funding in Australia are the Pharmaceutical Benefits Scheme (PBS), Medicare, private health insurance, the Department of Veterans’ Affairs, individual finances, and “other” sources.8 The amount that each contributes to care depends on the patient type (pensioners, war veterans, general patients) and the services provided.8
In 2011/12, health care spending in Australia was estimated at $140.2 billion AUD, or 9.5% of gross domestic product.3 This amount was 1.7 times higher than in 2001/02, with health care expenditures growing faster than the population.3 Almost 70% of total health care expenditure during 2011/12 was funded by federal, state, or territorial governments, with the federal government contributing 42% and the state and territorial governments 27%. The remaining 30% ($42.4 billion AUD) was paid for by patients (17%), private health insurers (8%), and accident compensation schemes (5%).3
Australia has 2 federally funded schemes that help to ensure timely and affordable access to health care and medications for all residents eligible for a Medicare card: the PBS and Medicare. People eligible to receive this funding for health include Australian citizens, those with a permanent visa, those working in Australia, and those with a proven relationship to an Australian citizen.9 The PBS helps to achieve Australia’s National Medicines Policy, a collective effort to bring about better access to and improved use of medications through 4 central objectives10:
Citizens have timely access to the medicines they need, at a cost that individuals and the community can afford.
Medicines meet appropriate standards of quality, safety, and efficacy.
Medicines are selected wisely, are used only when necessary, and are used safely and effectively.
Australia maintains a responsible and viable medicines industry.
The PBS was established in 1948 to provide free medications to pensioners and aims to meet objective 1 of the National Medicines Policy. The PBS began as a list of 139 “life-saving and disease-preventing medicines that were available to the Australian community”.11 Today, the PBS schedule has expanded to contain over 800 medicines,12 and the scheme provides subsidized medicines to any person who has a valid Medicare card or is from a country with which Australia has a reciprocal health care agreement.11 In 2015, the copayment prices for prescriptions were $37.70 AUD for a general patient and $6.10 AUD for a patient with a concession (usually low-income earners), a pension, or a Department of Veterans’ Affairs card. Therefore, for example, if the actual price of a medicine is $100 AUD, a general patient pays $37.70, with the remainder covered by the government. If a medicine is not listed in the PBS schedule, the consumer must pay the full price as a private prescription.
Medicare is a separate publicly funded scheme for universal health care that was introduced in 1975. It is nominally funded by an income tax surcharge, the Medicare levy, currently set at 2%.13 Patients with a valid Medicare card have access to subsidized primary health care and free treatment in public hospitals.14 Those with a valid Medicare card are also entitled to subsidized treatment from medical practitioners, eligible midwives, nurse practitioners, and allied health professionals who have a Medicare provider number.
For Australia’s Indigenous population, further incentives are offered to assist with managing chronic disease. For example, the Closing the Gap (CTG) PBS copayment measure improves access to PBS medicines for eligible Indigenous peoples who are living with, or at risk of, chronic disease.15 If a prescriber from a general practice or an Indigenous health service believes the patient could experience setbacks in the prevention or ongoing management of their chronic disease or is unlikely to adhere to the medicines regimen without assistance, then the prescriber annotates the prescription with “CTG” to alert the pharmacist that the prescription is to be dispensed with copayment relief.15 CTG prescriptions for PBS medicines attract a lower (or nil) patient copayment. That is, general (nonconcessional) patients who present a CTG prescription will be charged the current concessional rate ($6.10) for each PBS item on the prescription, and concessional patients who present a CTG prescription do not pay the patient copayment for any PBS item on the prescription.15
Private health insurance plays a small role in overall health funding and comes as “hospital” or “general” coverage.16 In an attempt to combat the increasing costs of the health care system in Australia, the government introduced the Medicare levy in 1997. This additional tax is paid by those without private hospital coverage, with the amount paid being dependent on the person’s marital or family status and income.17 Depending on the type of private health insurance purchased, patients may be able to access other services not otherwise subsidized through Medicare or the PBS.16 Patients are predominantly responsible for making claims to their insurer after receiving a health service or medication, although some health care providers are able to make the claim on the patient’s behalf. Unlike the situation in other countries such as the United States, Australian pharmacies do not have any contact with insurers when dispensing medications that are not subsidized within the PBS.
FEDERAL, STATE, AND TERRITORIAL CONTROL AND CONTRIBUTIONS
The Australian government and the state and territorial governments fund and deliver a range of other health services, including population health programs, community health services, health and medical research, Indigenous health services, mental health services, and health care infrastructure. In addition, the various levels of government also fund tertiary health care. Outpatient services attached to public hospitals are funded by the state, territorial, and national governments but are managed by state and territorial governments only, whereas private hospitals are owned and operated by the private sector.
Patients receiving care in a public hospital can opt to be treated as public or private patients. For example, a patient admitted to a public hospital is treated as an “inpatient”. If the person chooses to be treated as a public inpatient, the hospital services provided are funded by Medicare and state or territorial funds, whereas medications are fully subsidized and are usually funded through the state or territory. If the person opts to be treated as a private inpatient, the person’s insurance will reimburse the public hospital for some of the costs incurred. A patient who is treated in a public hospital without being admitted is treated as an “outpatient”, with the services and medications received being subsidized by Medicare and PBS, respectively. On the other hand, patients who receive care at a private hospital must be treated as private patients, with the cost of their stay subsidized by their insurance and the cost of medications being subsidized by the PBS. About 3%–4% of public hospital funding comes from private health insurance and the individual, whereas in private hospitals this figure is about 55%–58%.8,18
HEALTH WORKFORCE AND THE ROLE OF PHARMACISTS: MEDICATION SUPPLY AND BEYOND
Australia has a large, diverse health workforce that includes medical practitioners (physicians), nurses, midwives, psychologists, physiotherapists, dentists and related professionals, medical radiation practitioners, chiropractors, optometrists, podiatrists, osteopaths, Indigenous health practitioners, Chinese medicine practitioners, and pharmacists. In 2013, there were 591 503 registered health care practitioners. Over half of these were nurses and midwives, and more than 100 000 were medical practitioners.19
In Australia, only authorized practitioners—those with the appropriate formal training and registration—are allowed to supply medications to the public. Most frequently, “authorized practitioners” are registered pharmacists supplying medications to a patient according to a prescription or medical order. Although other professionals such as medical practitioners, dentists, nurse practitioners, midwives, optometrists, and podiatrists can obtain authorization to supply medications directly to patients, generally speaking patients will obtain their medications from a pharmacy, and the pharmacies will obtain medications from wholesalers.
By law, anyone with a pecuniary interest in a pharmacy must hold a pharmacy registration, and a pharmacist must be in charge of and supervise the operations of every pharmacy business. In addition, the number of pharmacies in which a person can have a pecuniary interest depends on state legislation. For example, in New South Wales and Victoria, a pharmacist can have a pecuniary interest in up to 5 pharmacies.
As of June 2014, there were more than 25 000 pharmacists in Australia,20 over 21 000 of whom were working in the pharmacy sector. The majority of these pharmacists had completed a pharmacy degree from 1 of the 17 accredited pharmacy schools in the country.21 Together, these schools graduate close to 2000 students per year.
To become a registered pharmacist, students must complete a degree program that has been accredited by the Australian Pharmacy Council (APC)—either a 4-year Bachelor of Pharmacy or a 2-year Master of Pharmacy—followed by 1 year of supervised practice in an approved practice setting.22 A number of professional organizations represent pharmacists and various aspects of pharmacy and pharmacy practice (see Table 1). Akin to the situation within Australia’s health care system as a whole, the influence of these organizations on the profession and its structure is complex, and jurisdictions often overlap.
Table 1.
Major Professional Pharmacy Organizations in Australia
| Organization | Abbreviation | Description |
|---|---|---|
| Australian Association of Consultant Pharmacy* | AACP | Deals primarily with sourcing new professional or consultant services for pharmacists and accreditation of pharmacists to provide these services |
| Australian College of Pharmacy* | ACP | Develops and provides education, training, and research programs to further the pharmacy profession; able to accredit and also provide continuing professional development activities, as well as nationally recognized qualifications relevant to pharmacy practice |
| Australian Health Practitioner Regulation Agency | AHPRA | National health professional regulation authority; contains several health professional boards, including the PBA |
| Australian Pharmacy Council | APC | Ensures the educational standards of potential pharmacists by accrediting pharmacy schools and their programs, intern training programs, and providers of continuing professional development; also conducts written examinations in conjunction with the PBA and assesses international students who have completed an Australian degree and overseas-trained pharmacists for eligibility to commence the registration process in Australia |
| Pharmaceutical Defence Limited* | PDL | Provides professional indemnity insurance to pharmacists (including students and interns), advice when errors are made, and legal advice related to pharmacy practice |
| Pharmaceutical Society of Australia* | PSA | Professional organization that provides tools to enable excellence in the practice of pharmacy, such as educational (continuing professional development) sessions, practice guidelines, and codes of ethics; claims to represent all pharmacists, but with the bulk of pharmacists practising in the community, most PSA tools are tailored to that sector |
| Pharmacy Board of Australia* | PBA | One of several health professional boards within the AHPRA; oversees pharmacist registration and provides registration standards, codes, and guidelines for professional practice |
| Pharmacy Guild of Australia* | PGA | Registered under the Fair Work Act as an employers’ association; acts as a union representing community pharmacy owners; also provides workplace relations advice and support to pharmacy owners |
| Professional Pharmacists Australia* | PPA | Union of non-owner community pharmacists |
| Society of Hospital Pharmacists of Australia* | SHPA | Akin to the Canadian Society of Hospital Pharmacists; provides pharmacy education, practice guidelines and standards, and other resources predominantly tailored to those working in the hospital setting |
Members of the Pharmacy Practitioner Development Committee (formerly the Advanced Pharmacy Practice Framework Steering Committee).
The APC oversees the quality of pharmacy training and is responsible for the accreditation of pharmacy schools, pharmacy programs, and intern training programs. The APC also administers written examinations that interns must pass before they undertake a final oral exam administered by the Pharmacy Board of Australia (PBA). On successful completion of both the written and the oral examinations, the graduate can apply for registration with the Australian Health Practitioner Regulation Agency (AHPRA). To maintain registration, a pharmacist must complete and record at least 40 continuing professional development credits annually. Mandatory continuing professional development was introduced in 2010.
Overseas-qualified pharmacists (from countries other than New Zealand, as pharmacists in Australia and New Zealand have equivalent status) seeking general registration in Australia are required to pass an examination conducted under the auspices of the APC. Those who pass this exam are then required to complete a period of supervised practice as assigned by the PBA. Conversely, pharmacists with an Australian pharmacy degree must generally complete a period of supervised practice (and sometimes additional study period) before being allowed to practise independently in overseas countries other than New Zealand.
To support the pharmacist’s role, pharmacy technicians and assistants provide various services in community and hospital pharmacies. In the community setting, support staff may also dispense medicines, supply some over-the-counter medicines, and undertake other administrative tasks such as refilling stock. In the hospital setting, technicians assist with dispensing the supply of ward stock, manufacturing, aseptic compounding, and administration duties.
Although ancillary staff members are not required by legislation to hold any formal educational qualification or registration requirements, PBA guidelines recommend that all dispensing technicians and assistants undertake and complete recognized training courses relevant to their role.23 A 2007 hospital pharmacy survey24 revealed that 52% of hospital pharmacy technicians held a qualification, with the majority of these holding what is called a certificate 3 or 4 (essentially a non-university diploma) from a tertiary technical college. The Society of Hospital Pharmacists of Australia (SHPA) has suggested that 1 support staff should be employed for every 1.5 pharmacists,24 although the PBA allows up to 2 dispensing technicians for every pharmacist.23
The scope of practice for pharmacists working in Australia is extremely broad. The National Competency Standards Framework for Pharmacists in Australia25 states the following:
Pharmacists use their expertise in medicines to optimise health outcomes and minimise medication misadventure. They apply their knowledge of poisons to promote their safe use and avoid harm to users and others in the community. The practice of pharmacy includes the custody, preparation, dispensing and provision of medicines, together with systems and information to assure quality of use. As readily accessible health professionals, pharmacists provide primary health care including education and advice to promote good health and to reduce the incidence of illness. A sound pharmaceutical knowledge base, effective problem-solving, organisational, communication and interpersonal skills, together with an ethical and professional attitude, are essential to the practice of pharmacy.
Registered pharmacists work in many areas of the health care sector. The majority (63%) work in the community pharmacy setting, whereas results from the 2014 health workforce survey showed that about 18% of the pharmacist population works in a hospital.21 Outside of the community and hospital settings, pharmacists are employed in universities, government departments of health, and the pharmaceutical industry. Because Australia has a relatively small population, there are currently few resources to support a large amount of manufacturing in the country. Multinational drug companies have offices in Australia and employ a range of pharmacists in various areas such as regulatory affairs, drug information, and medical training, but according to the 2014 workforce survey, only 1.7% of pharmacists are in this sector of the profession.21
COMMUNITY PHARMACY PRACTICE
Traditional pharmacist roles in community practice involve dispensing prescriptions and providing advice and primary care. These roles are reflected in the current product-oriented remuneration model in Australia; that is, the pharmacy earns money from dispensing and sale of products. Unfortunately, this model does not promote patient-centred care, despite most pharmacists having a positive attitude toward patient-centred concepts. The government pays the pharmacy (not the individual pharmacist) for the number of PBS prescriptions dispensed. Additional income is generated from selling other nonprescription products or from price mark-up on non-PBS prescriptions. This money is then used to pay for business costs, including wages. The hourly wage in a community pharmacy setting is between $22 and $50 AUD depending on days of the week and times of day that the person works and location of the pharmacy (with pharmacists who practise in a regional or remote setting earning considerably more than those practising in more urban settings).
Despite the current remuneration model, Australia has embarked on some unique remuneration models for services provided from this community setting. The Pharmacy Guild of Australia, which acts as a union of pharmacy owners, is a powerful lobby group that traditionally negotiates funding agreements with the Commonwealth government on a 5-year cycle. The current agreement (known as the “sixth community pharmacy agreement”) allows for a pharmacy to receive practice incentive payments in 6 priority areas:
dose administration aids (i.e., the pharmacy receives some government funding for repacking patients’ medicines in multiple-dose packaging)
clinical interventions (with pharmacists documenting any interventions performed to improve the quality use of medicines), which do not necessarily involve communication directly with a physician but can be any activity that improves the quality use of medications
staged supply, whereby, for medications like benzodiazepines, analgesics, and antidepressants, patients are given a certain number of days’ worth of medication at a time (requires a substantial amount of documentation)
primary health care, including screening and risk assessment, as well as follow-up for some common chronic conditions
community services support, including needle exchange and opioid substitution dispensing
working with others (i.e., pharmacists receive an annual incentive if they document collaborative practice with at least 2 nonpharmacist health care professionals)
These incentives are divided among the number of claiming pharmacies on a pro rata basis for the activity documented. Most of these services are routinely provided in the pharmacy, but having incentives to encourage these services is seen as beneficial to ensuring that pharmacists continue to provide high standards of care to the Australian public. The other services that are remunerated through the sixth (i.e. current) community pharmacy agreement include MedsChecks, Home Medicines Reviews, and Residential Medication Management Reviews. These services are described as “cognitive pharmacy services” and require comprehensive review of a patient’s medicines, as described below.
The MedsChecks service, which is conducted in the pharmacy, focuses on education and self-management. Remuneration of $62.18 AUD is given to a pharmacy after it has completed a patient’s medication check. A higher fee, $93.27 AUD, is received when the pharmacy conducts a diabetes medication check for a patient with a recent diagnosis of type 2 diabetes or a patient with poorly controlled diabetes who is unable to access a diabetes educator.
Medication review services take considerably more time and are often conducted in stages. Each review must be requested by a medical doctor. The pharmacist interviews the patient or care-giver regarding the person’s medicines and health and then writes a comprehensive report that includes the pharmacist’s findings and recommendations for the doctor, patient, and other health care professionals to consider. The review programs require cooperation between the general practitioner, the pharmacist, and the patient. Pharmacists are remunerated $208.22 AUD for each Home Medicines Review and $105.29 AUD for each Residential Medication Management Review. Only accredited pharmacists are authorized to provide review services. These accredited pharmacists have undertaken additional training and assessment before being deemed competent to perform reviews; to maintain their accreditation they must complete and record at least 20 additional continuing professional development credits annually.
Australia provides free vaccinations against 16 diseases through the national vaccination program, available only to Australian citizens. As of the end of December 2012, 92% of Australian children were assessed as fully vaccinated.3 Because of this national program, a large number of previously common vaccine-preventable diseases are now eradicated or very rare, with no cases of diphtheria or poliomyelitis recorded in recent years.3 Influenza vaccines are free for people aged 65 years and over, and Australia has one of the highest uptakes of patients seeking yearly flu vaccinations. In 2014, after a pilot trial in Queensland, the provision of vaccinations was reported to be within the scope of pharmacists. Since then, training courses for pharmacists are being established with the aim that administration of vaccinations by pharmacists will become ubiquitous in the community pharmacy setting.
HOSPITAL PRACTICE
Unlike some other countries, Australia currently has no defined residency training program for pharmacy graduates wanting to work in the hospital sector. About 200 (10%) of each year’s graduates are offered intern training in a hospital setting,24 and others find positions in hospital pharmacy after registration. The current hourly wage for hospital pharmacists is between $40 AUD and $50 AUD, depending on the state/territory in which they are employed and their level of practice.
Hospital pharmacists in Australia can have generalist roles or can practise within a very narrow field. The 2007 hospital pharmacy survey reported that on average pharmacists spent 47% of their time providing clinical services, drug information services, and training and education; 38% of their time acquiring, manufacturing, and dispensing medicines; and 15% of their time managing the medicines and personal resources of the pharmacy service and performing hospital-wide activities such as institutional drug policy management.24
In a large public teaching hospital, it is common to find a team of 30 or more pharmacists in the department, with the majority working in multidisciplinary teams. Although members of the SHPA have advocated, on Facebook and Twitter feeds, that pharmacy services should be provided 24 hours a day, 7 days a week, most hospitals in the country provide pharmacy services during regular business hours and an on-call service overnight. Some hospitals have skeleton staff on weekends, providing mainly distribution services, although after-hours services are increasing.
MOVE TOWARD THE “CLINICAL PHARMACIST”
Clinical pharmacy in Australia has been guided through the development and update of the Standards of Practice for Clinical Pharmacy, published in 2013.26 These standards state that pharmacists undertake clinical pharmacy activities for individual patients to minimize the inherent risk associated with the use of medicines. Clinical pharmacy activities support a collaborative approach (with patients, caregivers, prescribers, and other health care professionals) to medication management. The following clinical pharmacy activities are described in these standards:
performing medication reconciliation
assessing current medication management
performing clinical review, therapeutic drug monitoring, and adverse drug reaction management
contributing to the medicines management pathway
providing medicines information
facilitating continuity of medication management on discharge or transfer
participating in interdisciplinary ward rounds and meetings
training and education
participating in research
performing quality improvement activities and peer review
Importantly, these standards provide guidance on the staffing levels required to provide optimal services, as well as information on how to assess one’s own practice or the practice of peers through the use of ClinCAT, a clinical competency assessment tool aimed at motivating and guiding professional development. Given that these resources were created under the auspices of SHPA, it is unsurprising that these roles are predominantly delivered in hospital, although community pharmacists are increasingly becoming involved. Many pharmacists would claim to practise pharmaceutical care; however, the term is not commonly used in Australia, and other terms such as “medication management services” are more common.
A large proportion of a clinical pharmacist’s time is spent performing the clinical roles described above. In addition, some pharmacists specialize in other services, such as compounding, sterile manufacturing, provision of medicines information, drug-use evaluation, and administration of investigational drug trials.
FUTURE DIRECTIONS
The “Advanced Level” Pharmacist
Currently, there is only one recognized level of practice in Australia; however, practitioners acknowledge that some pharmacists are indeed practising at an “advanced level”.27 Advanced practice is said to be “practice that is so significantly different from that achieved at initial registration that it warrants recognition by professional peers and the public of the expertise of the practitioner and the education, training and experience from which that capability was derived”.28 Representatives from a number of Australian pharmacy associations and organizations (Table 1), together known as the Pharmacy Practitioner Development Committee (formerly the Advanced Pharmacy Practice Framework Steering Committee), have developed a framework for recognition of advanced pharmacy practice in Australia. A credentialing system was piloted in 2015, and the first “advanced practitioners” will soon be formally recognized.
Policy-makers in Australia have been careful to ensure that the title for these practitioners will use the word “advanced” rather than “specialist”. The National Competency Standards Framework25 considers the following:
It is well recognised within and beyond the pharmacy sector that the scope of practice of pharmacists has changed considerably over recent years. Associated with that change in scope has been an increasing tendency for pharmacists to choose to focus on particular areas of practice such as management, compounding or medication management. In limiting their scope of practice pharmacists afford themselves the opportunity to increase their expertise and improve their performance. This is probably the reason that a narrowing in scope of practice or ‘specialisation’ in practice is often seen as being synonymous with ‘advanced’ practice. This is reinforced by the medical model where ‘specialisation’ is synonymous with enhanced expertise through advanced training. However, ‘specialisation’ refers only to scope of practice rather than level of performance. Also, ‘specialisation’ of itself does not confer additional expertise. It therefore follows that ‘specialisation’ can occur without any associated enhancement in performance. To avoid confusion it is therefore considered preferable to discuss professional practice in terms of scope of practice and performance level.
Advanced practice pharmacists are considered to be those who influence practice, mentor and guide others, and are acknowledged as leaders in their field of practice.27 While many pharmacists are already practising at this advanced level, implementation of this new credential will formally recognize these pharmacists. Advanced practice areas are based on the National Competency Standards Framework and range from broad areas such as patient care, education, and medication review to narrower fields such as oncology and compounding.
The Prescribing Pharmacist
There is currently no legislation in Australia that grants prescribing rights to pharmacists. Pharmacists in the community setting can recommend over-the-counter medicines, which are divided into 2 schedules. Schedule 2 medicines (“pharmacy medicines”) are only available in a pharmacy and must be sold under the supervision of a pharmacist. A pharmacy assistant may hand such medicines to customers, but this must be done in the presence of a registered pharmacist. Schedule 3 medicines (“pharmacist only medicines”) must be handed out by pharmacists themselves. As such, it could be said that pharmacists do prescribe from this limited list of medicines. Pharmacist prescribing of “prescription only medicines” (schedules 4 and 8) is not currently allowed; however, there has been much talk about widening prescribing rights to many health care professionals other than medical doctors. Health care professionals other than medical doctors who already have prescribing rights include nurse practitioners, midwives, dentists, optometrists, and podiatrists. Prescribing rights for pharmacists in Australia may be granted in the near future, as there are prescribing pharmacists in the United Kingdom and New Zealand.
CONCLUSION
Australian pharmacists have an integral role in maintaining quality use of medications and upholding the objectives of the National Medicines Policy. Pharmacists have a number of opportunities to showcase their skills in community and hospital settings, as well as other sectors, such as industry, education, and government. In the near future, new opportunities, including vaccination, advanced practice, and possibly pharmacist prescribing, will further pharmacists’ contribution to the health and well-being of the Australian people. These new service-oriented practice areas demonstrate a strong acknowledgment of the high-level clinical skills of pharmacists; however, for these skills to be sustainable and cost-effective, a robust service-based remuneration model needs to be implemented, especially for those practising in community.
Footnotes
Competing interests: None declared.
References
- 1.Countries: Australia [map, statistics] Geneva (Switzerland): World Health Organization; 2015. [cited 2015 Jul 3]. Available from: www.who.int/countries/aus/en/ [Google Scholar]
- 2.3412.0 - migration, Australia, 2013–14. Canberra (Australia): Australian Bureau of Statistics; 2015. Jan 29, Also available from: www.abs.gov.au/AUSSTATS/abs@.nsf/ProductsbyCatalogue/66CDB63F615CF0A2CA257C4400190026?OpenDocument. [Google Scholar]
- 3.Australia’s health 2014. Canberra (Australia): Australian Institute of Health and Welfare; 2014. Aust Health Ser no. 14. Cat. no. AUS 178. Also available from: www.aihw.gov.au/publication-detail/?id=60129547205. [Google Scholar]
- 4. Countries in the world (ranked by 2014 population). Worldometers; 2014 [cited 2015 Aug 28]. Available from: www.worldometers.info/world-population/population-by-country/
- 5.3303.0 - causes of death, Australia, 2013. Canberra (Australia): Australian Bureau of Statistics; 2015. Mar 31, [cited 2015 Jun 24]. Available from: www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/3303.0~2013~Main%20Features~Leading%20Causes%20of%20Death~10001. [Google Scholar]
- 6.3302.0 - deaths, Australia, 2013. Canberra (Australia): Australian Bureau of Statistics; 2014. Nov 6, [cited 2015 Aug 30]. Available from: www.abs.gov.au/ausstats/abs@.nsf/Latestproducts/3302.0Main%20Features52013?opendocument&tabname=Summary&prodno=3302.0&issue=2013&num=&view= [Google Scholar]
- 7.Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res. 2010;10:231. doi: 10.1186/1472-6963-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Australia’s hospitals 2011–12 at a glance. Canberra (Australia): Australian Institute of Health and Welfare; 2013. Health Serv Ser no. 49. Cat. no. HSE 133. Also available from: www.aihw.gov.au/publication-detail/?id=60129543134. [Google Scholar]
- 9.Eligibility for Medicare card. Canberra (Australia): Commonwealth of Australia, Department of Human Services; [cited 2015 Jun 24]. Available from: www.humanservices.gov.au/customer/enablers/medicare/medicare-card/eligibility-for-medicare-card. [Google Scholar]
- 10.National Medicines Policy 2000. Commonwealth of Australia, Department of Health and Ageing; 1999. [cited 2015 Sep]. Available from: www.health.gov.au/internet/main/publishing.nsf/Content/B2FFBF72029EEAC8CA257BF0001BAF3F/$File/NMP2000.pdf. [Google Scholar]
- 11.The Pharmaceutical Benefits Scheme: About the PBS. Canberra (Australia): Commonwealth of Australia, Department of Health; [cited 2015 Aug 29]. Available from: www.pbs.gov.au/info/about-the-pbs. [Google Scholar]
- 12.Sweeny K. Medicine prices in Australia: an international comparison. Pharm Ind Project Work Pap Ser. [Victoria University, Melbourne, Australia] 2005:29. [Google Scholar]
- 13.Medicare levy. Canberra (Australia): Commonwealth of Australia, Australian Taxation Office; 2015. [cited 2015 Jun 29]. Available from: https://www.ato.gov.au/Individuals/Medicare-levy/ [Google Scholar]
- 14.Wikipedia, the free encyclopedia. Wikipedia Foundation Inc; Medicare (Australia) modified 2015 Jul 25[cited 2015 Jul 27]. Available from: http://en.wikipedia.org/wiki/Medicare_%28Australia%29. [Google Scholar]
- 15.Closing the gap - PBS co-payment measure. Canberra (Australia): Commonwealth of Australia, Department of Human Services; updated 2015 Jun 24 [cited 2015 Jul 3]. Available from: www.humanservices.gov.au/health-professionals/services/pbs-closing-the-gap-co-payment-measure/ [Google Scholar]
- 16.Private health insurance - frequently asked questions. Canberra (Australia): Commonwealth of Australia, Department of Health; updated 2013 Oct 4 [cited 2015 Jul 3 ]. Available from: www.health.gov.au/internet/main/publishing.nsf/Content/Frequently+Asked+Questions-1#what. [Google Scholar]
- 17.Medicare levy surcharge. Canberra (Australia): Commonwealth of Australia, Private Health Insurance Ombudsman; [cited 2015 Aug 30 ]. Available from: www.privatehealth.gov.au/healthinsurance/incentivessurcharges/mls.htm. [Google Scholar]
- 18.Australia’s hospitals at a glance 2012–13. Canberra (Australia): Australian Institute of Health and Welfare; 2013. Health Serv Ser no. 55. Cat. no. HSE 146. Also available from: www.aihw.gov.au/australias-hospitals-at-a-glance-2012-13/ [Google Scholar]
- 19.Workforce: health workforce. Canberra (Australia): Australian Institute of Health and Welfare; reviewed 2015 Mar [cited 2015 Aug 30 ]. Available from: www.aihw.gov.au/workforce/ [Google Scholar]
- 20.Pharmacy registrant data: June 2014. Canberra (Australia): Pharmacy Board of Australia; 2014. Jul, Also available from: www.pharmacyboard.gov.au/About/Statistics.aspx. [Google Scholar]
- 21.Australia’s health workforce series: pharmacists in focus. Adelaide (Australia): Health Workforce Australia; 2014. Mar, Also available from: https://www.hwa.gov.au/sites/default/files/HWA_Australia-Health-Workforce-Series_Pharmacists%20in%20focus_vF_LR.pdf. [Google Scholar]
- 22.Australian Pharmacy Council [website] Canberra (Australia): Australian Pharmacy Council; [cited 2015 Jun 24 ]. Available from: http://pharmacycouncil.org.au/content/ [Google Scholar]
- 23.Guidelines for dispensing of medicines. Canberra (Australia): Pharmacy Board of Australia; 2015. Also available from: www.pharmacyboard.gov.au/Codes-Guidelines.aspx. [Google Scholar]
- 24.O’Leary KM, Allinson YM. Snapshot of the Australian public hospital pharmacy workforce in 2007. J Pharm Pract Res. 2009;39(1):28–33. doi: 10.1002/j.2055-2335.2009.tb00700.x. [DOI] [Google Scholar]
- 25.National competency standards framework for pharmacists in Australia 2010. Deakin (Australia): Pharmaceutical Society of Australia; 2010. Also available from: https://www.psa.org.au/download/standards/competency-standards-complete.pdf. [Google Scholar]
- 26.Society of Hospital Pharmacists of Australia Standards of practice for clinical pharmacy services. J Pharm Pract Res. 2013;43(2 Suppl) [Google Scholar]
- 27.An advanced pharmacy practice framework for Australia. Deakin (Australia): Advanced Pharmacy Practice Framework Steering Committee; 2012. Oct, [Google Scholar]
- 28.What is advanced pharmacy practice? Canberra (Australia): Australian Pharmacy Council; [cited 2015 Jan 19 ]. Available from: https://www.pharmacycouncil.org.au/pharmacists/australian-nz-pharmacists/what-is-advanced-pharmacy-practice/ [Google Scholar]