Abstract
Background
Despite the historically low smoking prevalence among Chinese women, there is a trend of future increase.
Purpose
We systematically reviewed the correlates of smoking among Chinese girls and women.
Method
We conducted a systematic review of literature on correlates of smoking among Chinese women using Medline and China Academic Journals databases. Following the PRISMA statement, two investigators independently searched for literature, identified and reviewed papers, assessed the quality of the papers, and extracted information. The characteristics of studies and correlates of smoking were synthesized separately for youth and adults.
Results
A total of 15 articles (11 on adults, 4 on youth) met the inclusion criteria. Based on these studies, peer smoking was the most consistent correlate of smoking among Chinese girls. Among Chinese women, partner smoking, job-related stress, and exposure to cigarettes made for women were consistent correlates of smoking. Knowledge of harms and negative attitudes towards smoking were found to be negatively associated with smoking.
Conclusion
Overall, the evidence base for smoking among Chinese women is limited. Although smoking among Chinese women is still at an early stage, it is becoming more prevalent among specific population subgroups, such as rural-to-urban migrant workers. Although further research is needed, findings from the current study provide a roadmap for research and policy on prevention of smoking among Chinese girls and women.
Keywords: Smoking, China, Women, Correlates, Prevention, Epidemiology, Public health
Introduction
China is the world’s largest tobacco producer and consumer with more than 300 million smokers [1]. Based on the 2010 China Global Adult Tobacco Survey, about 53 % of men and 2.4 % of women aged 15 years and older currently smoke [2]. Smoking has contributed to an enormous disease burden in China, posing great challenges to public health and well-being [3]. It has been estimated that if the current smoking prevalence continues, one in three Chinese men will eventually die from tobacco-related diseases [4].
Although smoking prevalence among Chinese women has traditionally been very low [5], there are concerns about future increases in susceptibility, targeted marketing, and disease burden among women in China and elsewhere in Asia [6]. Worldwide, the spread of the cigarette epidemic has followed the “diffusion of innovations” theory [7] wherein cigarette smoking was adopted by males in high-income nations before it was adopted by women and people in middle- and low-income countries [8]. Subsequently, in many countries, smoking rates among men are on the decline, signifying a late-stage epidemic, but rates among women are still rising, indicating an early-stage epidemic [9,10]. Currently, women’s smoking rates in low- to middle-income countries, such as China, are much lower compared to high-income countries [11]. Using country-level data, Hitchman and Fong found that higher gross national income and gender empowerment were independently associated with higher female-to-male smoking prevalence ratios [12]. Therefore, a plausible and worrisome projection is that with the increasing spending power and weakening cultural and social constraints of women in emerging economies, such as China, there may be an expanding epidemic of smoking among women with subsequent impacts on overall mortality, morbidity, and economic systems [9].
China is an important case study for the diffusion of smoking among women in low- to middle-income countries. The currently low smoking prevalence among Chinese women is largely due to traditional gender roles and social expectations [13]. Such gender-specific smoking patterns in mainland China have also been observed in Hong Kong [14], Taiwan [15], and other Asian countries with which China shares cultural similarities [16,17]. There is evidence of an increase in smoking rates among women in Japan and Korea as a result of westernization and promotional campaigns of the tobacco industry targeting women and girls [17–19]. Results from the China National Tobacco Survey have shown a slight increase in smoking prevalence among women, particularly young women, from 1996 to 2010 [2]. Between 1993 and 2008, the age for smoking initiation among Chinese women has decreased significantly, and the percentage of heavy smokers (≥20 cigarettes/day) has increased dramatically [2]. A recent survey reported an alarmingly high ever smoking prevalence of 20 % among Chinese adolescent girls and young women aged 14–24 years [20]. With a huge population and a historically low smoking rate among women, China is an almost limitless potential market for the tobacco industry [21,22].
Although the smoking epidemic among Chinese women is still at an early stage, proactive actions are necessary in order to prevent further growth of the epidemic. Successful public health and behavioral medicine interventions should be based on in-depth knowledge about smoking susceptibility among young Chinese women and girls and particularly about the population distribution and correlates of smoking. To consolidate information about smoking among Chinese women, we conducted a systematic review on correlates reported in peer-reviewed and gray literature. The ultimate aim of this review is to inform further research and public health interventions to prevent the growing epidemic of smoking among Chinese women.
Methods
Literature Search
We conducted a systematic literature review on correlates of smoking among Chinese women. The review methodology followed the PRISMA statement (http://www.prisma-statement.org/) [23]. Medline and China Academic Journals (CAJ) databases were used for searching for English and Chinese journal articles that were published, in print or online until January 2013. OAIster was used to search for gray literature. In Medline and OAIster, terms for women and girls (woman, women, female, females, girl, girls, gender) were used in AND-combination with terms for smoking (smoking, smoke, smoker, smokers, cigarette, cigarettes, tobacco) and in AND-combination with terms for China (including special administrative regions such as Hong Kong and Taiwan). Medical Subject Headings (MeSH), subheadings, and terms were used when available. In CAJ, thesaurus terms for “women/girls” and “smoking” (in Chinese) were used in AND-combination. Additional manual searches were conducted by checking articles cited in reference lists of included papers and by searching in the authors’ own archives.
Inclusion/Exclusion Criteria
To be included, studies were required to (1) focus on women or girls (gender-stratified studies were included); (2) examine correlates of smoking; and (3) have been conducted in mainland China, Hong Kong, Macau, or Taiwan. Exclusion criteria were as follows: (1) descriptive studies without formal statistical analyses, (2) passive smoking or combined active and passive smoking as outcome variable, (3) non-cigarette smoking (e.g., water pipe) as the main focus, and (4) studies with poor quality (see “Quality Assessment and Data Extraction”). Only full-text papers were considered for review. Papers written in either English or Chinese were eligible. Initial screening was conducted by two independent investigators (DD and KG for English literature and DD and XZ for Chinese literature) scanning the titles and abstracts of identified papers. This process was followed by independent reviews of full texts of all potentially relevant papers. Disagreement between the two investigators was discussed, and a final consensus was reached.
Quality Assessment and Data Extraction
Information on the study population, measurement, and analyses (both adjusted and unadjusted) was extracted for each paper. The methodological quality of each study was independently assessed by two investigators (DD and KG) using a quality checklist adapted from previous reviews of observational studies [24,25]. The checklist included ten criteria with yes (1) and no/not clear (0) responses. To ensure the quality of studies included in the review, papers with a quality score of 5 or lower were excluded from the synthesis of the results.
We summarized the characteristics of each paper reviewed (Table 1) and tabulated the results in descending order by the quality scores of the studies separately for youth (Table 2) and adults (Table 3). We used “+”, “−”, and “0” to notify positive, inverse, and no associations. If a study reported multiple models for the same variable, we assessed the consistency of associations within a study and assigned “+” or “−” when over 60 % of the results across models were significant in the same direction. In the situation of multiple papers from the same study [26,27] reporting the same association (e.g., age), we only reported findings from the article with a higher quality score.
Table 1.
Characteristics of primary studies reviewed (n =15)
| Author | Study population | Location | Age (years) | Random sample | Response rate | Questionnaire administration | Sample size | Smoking rate | Validity score |
|---|---|---|---|---|---|---|---|---|---|
| Youths | |||||||||
| Zhang [31] | Secondary school students | Henan, China | 10–19 | Yes | 97 %a | Self | 1,720 | ES, 5.4 % | 9 |
| Huang [34] | Elementary school students | Taiwan | Mean=11 | Yes | 94 %a | Self | 1,137 | ES, 9.2 % | 7 |
| Ma [29] | 9th grade students | 7 cities in China | Mean=15 | Yes | Not stated | Self | 1,768 | Not stated | 7 |
| Wen [30] | High school students | Taiwan | 15–18 | Not stated | Not stated | Self | 22,821 | CS, 5.1 % | 6 |
| Adults | |||||||||
| Chuang [32] | General | Taiwan | 20+ | Yes | 67 %a | Interviewer | Not stated | ES, 5 % | 10 |
| Shin [26] | Rural-to-urban migrants | 10 provincial capital cities in China | 18–30 | No | 99 % | Interviewer | 1,697 RHW, 532 SW | ES: 18.4 % (RHW), 58.3 % (SW) CS: 3.2 % (RHW), 41.9 % (SW) | 9 |
| Wan [27] | Same as Shin [26] | – | – | – | – | – | – | – | 8 |
| Yang [38] | Aborigines | Taiwan | 17–50 | Yes | 89 % | Interviewer | 300 | CS, 11.6 % | 8 |
| Chen [28] | Rural-to-urban migrants | Beijing, China | 18–30 | Not stated | Not stated | Self | 866 | CS, 10.9 % | 7 |
| Finch [18] | Rural-to-urban migrants | Beijing, China | 18–30 | No | Not stated | Interviewer | 165 RHW, 72SW | ES: 16.1 % (RHW), 54.9 % (SW) CS: 6.5 % (RHW), 33.3 % (SW) | 7 |
| Ho [20] | High school and college students | 6 provincial capital cities in China | 14–24 | No | 95 % | Self | 11,095 | ES: 20.1 % (urban), 22.0 % (rural) CS: 4.2 % (urban), 1.9 % (rural) | 7 |
| Lau [35] | General | Hong Kong | 18+ | Yes | 75 % (smokers), 77 % (non-smokers) | Telephone | 2,024 | ES, 3.4 % CS, 2.7 % | 7 |
| Tsai [37] | General | Taiwan | 18+ | Yes | 48 %a | Interviewer | 90 | CS, 4.8 % | 6 |
| Lin [36] | Employees of microelectronics companies | Taiwan | 16–57 | No | 73 % | Self | 1,950 | ES, 11.6 % CS, 9.3 % | 6 |
| Cai [33] | General | 31 provinces in China | 15+ | Yes | Not stated | Interviewer | 74,236 | CS: 2.8 (urban), 2.6 (rural) | 6 |
ES ever smoker, CS current smoker, RHW restaurant hotel workers, SW sex workers
Response rate of female/male combined samples, no female-specific response rate was reported
Table 2.
Correlates of smoking in Chinese girls (n =4)
| Author
|
|||||
|---|---|---|---|---|---|
| Zhang [31] | Huang [34] | Ma [29] | Wen [30] | ||
| Demographics | Age/grade | + | |||
| Living in rural areas | 0 | − | |||
| Individual | Social belief | + | |||
| Subjective norms | 0 | 0 | |||
| Low refusal efficacy | + | ||||
| Knowledge of harms | 0 | ||||
| Social | Parents smoking | + | 0 | 0 | + |
| Peer smoking | + | + | + | ||
| Teacher smoking | + | ||||
| Tender, loving, and caring parents | − | ||||
| Anti-smoking curricula | − | ||||
ES ever smoking, CS current smoking
Table 3.
Correlates of smoking among Chinese women (n =11)
| Author (year)
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chuang [32] | Shin [26] | Wan [27] | Yang [38] | Chen [28] | Ho [20] | Lau [35] | Finch [18] | Tsai [37] | Lin [36] | Cai [33] | ||
| Demographics | Age | 0 | − | Nonlinear | Nonlinear | − | − | + | ||||
| Education | 0 | 0 | + | Nonlinear | Nonlinear | − | − | |||||
| Income | + | + | + (pocket money) | + | Nonlinear | − (urban) + (rural) | ||||||
| Married | 0 | + | − | 0 | ||||||||
| Divorced | + | + | ||||||||||
| Living in rural areas | + | 0 | ||||||||||
| Renting | + | |||||||||||
| Individual | Knowledge of harms | 0 | − | − | ||||||||
| Support anti-smoking laws | − | − | ||||||||||
| Positive attitude of smokers | + | + | ||||||||||
| Negative attitude of smokers | − | − | ||||||||||
| Low refusal efficacy | + | |||||||||||
| Exposure to CMFW | + | + | + | |||||||||
| CMFW less harmful | + | 0 | ||||||||||
| Social | Partner smokes | + | + | + | + | 0 (urban) + (rural) | ||||||
| Partner discourages smoking | − | |||||||||||
| Friends smoke | 0 | + | ||||||||||
| Manager smoke | + | |||||||||||
| Family smokes | + | + | ||||||||||
| Family discourages smoking | − | |||||||||||
| Social trust | − | |||||||||||
| Job-related | Hours worked | + | ||||||||||
| Shift work | + | |||||||||||
| Sex worker | + | + | ||||||||||
| Job stability | − | |||||||||||
| Job satisfaction | − | − | − | |||||||||
| Life satisfaction | − | − | − | |||||||||
| Discrimination | + | |||||||||||
CMFW cigarettes made for women
Results
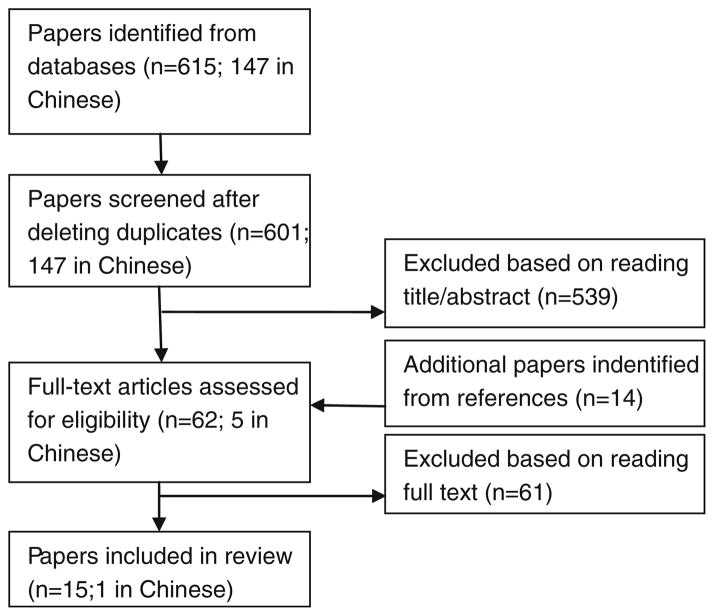
The initial search resulted in 601 unique papers that were potentially relevant (Fig. 1). We did not find any sources in gray literature. Of the 601 papers, 539 were excluded based on titles and abstracts. By checking the references of the remaining 62 papers, 14 additional papers were identified. Of these eligible papers, 61 were excluded based on reading the full text, and 15 articles were used in the final review [18,20,26–38].
Fig. 1.
Study flow
Characteristics of Primary Studies Reviewed
Among the 15 papers reviewed in detail (Table 1), eight were conducted in mainland China [18,20,26–29,31,33], one in Hong Kong [35], and six in Taiwan [30,32,34,36–38]. One paper was in Chinese language [33], while the rest were in English. Four studies addressed children and adolescents, and eleven addressed adults (one covered an age range of 14–24 years). All studies about youth targeted school-attending students. Most studies about adults targeted selected population subgroups. For example, four papers from three studies focused on rural-to-urban migrants [18,26–28], one focused on young women attending schools [20], one focused on employees of large microelectronics companies [36], and one study targeted aborigines in Taiwan [38].
All studies were cross-sectional and about half of them (n =8) applied random sampling [20,29,31,32,34,35,37,38]. Ten studies reported response rates and almost all of them were higher than 60 % (five studies had response rates from 94 % to nearly 99 %). All four studies on youth used self-administered surveys while most studies among adults used interviewer-administered surveys [18,26,27,32,33,37,38]. Sample sizes of the studies among youth ranged from 1,137 to 22,821 and those among adults from 90 to 74,236. The validity scores of the included studies ranged from 6 to 10.
Prevalence and Correlates of Smoking Among Chinese Girls
The prevalence of ever smoking or having ever tried smoking among Chinese girls ranged from 6 to 17 %, and the current smoking prevalence ranged from 1.4 to 5 % (Table 1). Several types of social influence were examined in relation to smoking among Chinese girls (Table 2). Peer smoking appeared to be the most consistent correlate and was significant in all three relevant studies [29,31,34]. All four youth studies examined parental smoking as a potential correlate of smoking among girls, and two of the studies found it to be statistically significant [30,31]. Teacher smoking was associated with girls’ smoking in one study [31]. Subjective norms of smoking in school and other public places were not associated with smoking [31,34]. Having anti-smoking curricula in schools was inversely associated with smoking among female elementary girls in one study [34]. There is insufficient evidence to draw conclusions about demographic or other individual-level correlates of smoking (e.g., knowledge) among Chinese girls.
Prevalence and Correlates of Smoking Among Chinese Women
Across samples, smoking prevalence among adult Chinese women varied greatly. The ever smoking rates ranged from 3.4 to 58 %, and the current smoking rates ranged from 2.7 to 41.9 % (the highest rates were among sex workers) (Table 1). Almost all studies on adults examined some demographic correlates of smoking, such as age and education (Table 3). Of the six studies that examined age, three found an inverse association between age and smoking [36–38], two found a nonlinear association [18,28], one found a positive association [33], and one found no significant association [26]. There was an overall positive association between income and smoking, with five studies demonstrating a positive association in the overall sample or a subsample [18,20,26,28,33], one study showing an inverse association among an urban subsample [33], and one study showing a nonlinear association [37]. Being divorced was a potential correlate of smoking [18,35], while being married was inconsistently associated with smoking. Smoking among Chinese women tended to correlate inversely with knowledge of harms and negative attitudes towards smoking [18,20,35]. In contrast, a positive attitude towards smoking, exposure to cigarettes made for women (CMFW), and misperceptions of the harms of CMFW were positively associated with smoking in a number of studies [18,20,27,35]. Among all social influence variables, partner smoking was the most frequently examined and most consistent correlate [20,27,33,35,38]. A small number of studies also found that other social influences, such as friend, manager, and family smoking, were positively associated with smoking [20,27,33,35]; however, the number of studies was too small to make conclusions for these social influences. Several aspects of job-related stress, such as shift work, long hours, instability, and low job satisfaction, have shown consistent and positive associations with smoking [18,26,28,36].
Discussion
To the authors’ knowledge, this study is the first to systematically review correlates of smoking among Chinese women and one of the first to review correlates of smoking among women worldwide. Findings from this review can help identify subgroups of girls and women who are particularly susceptible to smoking and guide the development of public health and behavioral medicine interventions that aim to prevent smoking uptake among Chinese women.
Thus far, most epidemiological and intervention studies on smoking in China have focused on smoking in men or have not been gender-specific. The lack of attention to Chinese girls and women is a result of the widespread acceptance of gender discrepancy in the smoking rates in China. However, the current review identified much higher smoking rates among some subgroups of women, such as rural-to-urban migrant women, sex workers, and young women in high school and college. These subgroups represent growing population segments in China as a result of urbanization and related societal changes. Given the growing number of women in such subgroups, if no proactive measures are taken, increasing smoking among these women is likely to lead to a much higher smoking rate nationwide. This, again, reinforces the importance of prevention at an early stage of the epidemic.
The associations between smoking and demographic characteristics among women were complex. Three studies among adults, all conducted in Taiwan, found an inverse association between age and smoking, suggesting that younger women were more likely to smoke. Two studies among rural-to-urban migrants, with relatively restrictive inclusion criteria for age, found nonlinear associations and that women aged 22–24 years had the highest smoking prevalence. These studies contradict previous nationally representative data from mainland China which indicated higher smoking rates among older women [39]. However, because samples of studies reviewed were not nationally representative, findings from these studies cannot be generalized to imply national smoking trends by age. The association between education and smoking was also inconclusive, which contrasts existing evidence among men or the general population in China [40,41] and elsewhere [42,43]; in these studies, smoking prevalence is almost always inversely associated with educational attainment. Most studies in the current review found a positive association between income and smoking, which is distinctive from the pattern observed in men and women in other countries [42,44]. This unique association between income and smoking in China may be a result of a rapidly growing new affluence, which has brought about increases in spending power among women in China [9,12,45].
A few studies found that having seen, heard about, or tried CMFW was strongly associated with current smoking. CMFW is an important marketing strategy the tobacco industry uses to attract new female smokers. These CMFW are usually thin, in beautiful colors, flavored, and elegantly packaged. In China, the names of CMFW tend to imply beauty and sexual appeal, such as “
 ” which refers to 12 famous beauties in Chinese traditional literature and “
” which refers to 12 famous beauties in Chinese traditional literature and “
 ” which means “the capital of dreams”. The tobacco industry also promotes products with fruity flavor, such as the “DJ Mix Light” with strawberry flavor. Some products feature “herbs” and “ginseng” as ingredients and are mislabeled as health promoting [46]. In summary, cigarette companies are trying to support a “new normal” for smoking among women—not only acceptable but also desirable, liberating, fashionable, and “glorious”. Based on the studies reviewed, it appears that this approach has had some success in recruiting female smokers in China. The success of the tobacco industry in China is a result of an overall loose tobacco control environment. Although the Chinese government has endorsed the WHO Framework Convention on Tobacco Control (FCTC); the actual implementation of advertisement and sponsorship regulations, warning labels, and cigarette tax is still quite poor in many instances [47,48].
” which means “the capital of dreams”. The tobacco industry also promotes products with fruity flavor, such as the “DJ Mix Light” with strawberry flavor. Some products feature “herbs” and “ginseng” as ingredients and are mislabeled as health promoting [46]. In summary, cigarette companies are trying to support a “new normal” for smoking among women—not only acceptable but also desirable, liberating, fashionable, and “glorious”. Based on the studies reviewed, it appears that this approach has had some success in recruiting female smokers in China. The success of the tobacco industry in China is a result of an overall loose tobacco control environment. Although the Chinese government has endorsed the WHO Framework Convention on Tobacco Control (FCTC); the actual implementation of advertisement and sponsorship regulations, warning labels, and cigarette tax is still quite poor in many instances [47,48].
Based on the literature review, work-related stress appeared to be another important risk factor for smoking. This is particularly salient among rural-to-urban migrant workers, a high-risk subpopulation for many health risk behaviors [49]. Rural-to-urban migrant workers are a growing yet marginalized group in the Chinese society. China has a “hukou” system that distinguishes between urban and rural residents. Migrants move from rural to urban areas in search of employment without establishing permanent urban residence. They tend to work in temporary jobs with poor wages and are subject to interpersonal and institutional discrimination [26,50], all of which induce stress [51]. There has been abundant evidence linking stress to smoking [52,53], and a recent study found a similar association between work-related stress and smoking among rural-to-urban migrant men in China [54]. Furthermore, female migrant workers tend to work in the service and entertainment industry, where the pressure or demands for smoking are high [55]. Tobacco control efforts among migrants cannot be successful without addressing their work conditions and the inequality in their daily life.
This review also identified social influences to be important for both women and young girls. Among young girls, friends/peer smoking was the most consistent correlate. Among adults, partner smoking is the most consistent correlate of smoking. For both women and girls, family/parent smoking plays a role in their own smoking. This suggests that smoking among girls and women is not an issue in and of itself; instead, it is embedded in their social environments that are overall friendly toward smoking. Such strong social influence on smoking is observed throughout mainland China, its special administrative regions, and Taiwan [32]. This suggests that interventions should target women’s immediate environments in addition to addressing individual behavior change. In the last few years, the Chinese government has launched several mass media campaigns aiming to deglamorize smoking, such as the “giving cigarettes is giving harm” campaign that criticizes cigarette gifting during holidays, a common practice in China [56]. Another example of anti-smoking campaigns that target social norms is the recent “smoke-free weddings” initiative [57], where the bride and groom take joint efforts to keep cigarettes out of their weddings. Long-term effects of such campaigns should be evaluated to determine whether they successfully changed social norms related to smoking.
Limitations in Current Studies
Behavioral medicine interventions should be based on evidence. However, currently, the evidence base in China on smoking epidemiology and prevention is quite limited, particularly regarding smoking in women. This is reflected by the small number of studies identified by the current review. Furthermore, all of the studies reviewed were cross-sectional and used only self-reported measures for smoking, which is likely to underestimate actual smoking prevalence among women. Social desirability bias for female smokers to lie about smoking status might be particularly strong in a society that discourages smoking in women [58]. Furthermore, smoking among Chinese women tends to be concentrated in special subgroups, such as migrant workers and sex workers, who are usually “hard to reach” by national smoking surveillance. Through the literature search, we did not identify any quality interventions on smoking prevention among Chinese girls and women. A recent review examined randomized control trials aimed at preventing smoking in China. Most studies lacked quality designs (e.g., not including post-intervention follow-up measures) and the findings were mixed [59].
Future Research and Intervention Needs
In order to effectively prevent smoking among Chinese women, more research with rigorous methodology is needed to fully understand the scope, trends, population distribution, and socio-ecological correlates of smoking among Chinese women. Future studies should apply a longitudinal study design to monitor smoking initiation among young women. Objective measures of smoking (e.g., cotinine) should be included to validate self-reported smoking among Chinese women. Future studies should include more comprehensive conceptualization and examination of social influences, such as social norms and contexts of smoking. Women-specific prevention interventions should be introduced to counter targeted promotion campaigns from the tobacco industry. Women should be encouraged and empowered to play a pivotal role in tobacco control interventions in their family and societies [60]. At the policy level, implementation of the MPOWER strategies (i.e., monitoring tobacco use and prevention policies; protecting people from tobacco smoke; offering help to quit tobacco; warning about the dangers of tobacco; enforcing bans on tobacco advertising, promotion, and sponsorship; and raising taxes [61]) and fulfilling the FCTC obligations can help reduce smoking in the overall population, including women.
Conclusions
Tobacco control research, policy, and practice should be gender specific [11]. We conducted a systematic review on correlates of smoking among Chinese women to inform women-specific research and interventions for tobacco control in China. Findings from the current study suggested that cigarette smoking is a much more significant problem for certain population subgroups, such as female rural-to-urban migrants and sex workers. Smoking was related to work-related stress and social modeling and was heavily influenced by the tobacco industry’s gender-specific marketing strategies. Findings from the current study provide a roadmap for future research and policy on preventing smoking among Chinese girls and women.
Acknowledgments
The authors wish to acknowledge the National Institute of Health (grant #1R03TW008361-01) for funding the research.
Contributor Information
Ding Ding, Email: melody.ding@sydney.edu.au, Sydney School of Public Health, The University of Sydney, Sydney, Australia.
Klaus Gebel, Sydney School of Public Health, The University of Sydney, Sydney, Australia.
Brian F. Oldenburg, School of Public Health & Preventive Medicine, Monash University, Melbourne, Australia
Xia Wan, School of Basic Medicine, Peking Union Medical College, Beijing, China.
Xuefeng Zhong, Institute of Health Education, Anhui Center for Disease Prevention and Control, Hefei, China.
Thomas E. Novotny, Graduate School of Public Health, San Diego State University, San Diego, USA
References
- 1.Li Q, Hsia J, Yang G. Prevalence of smoking in China in 2010. N Engl J Med. 2011;364(25):2469–70. doi: 10.1056/NEJMc1102459. [DOI] [PubMed] [Google Scholar]
- 2.China Centers for Disease Control and Prevention. Global adult tobacco survey (GATS) China 2010 country report. Beijing, China: 2011. [Google Scholar]
- 3.Gu D, Kelly TN, Wu X, Chen J, Samet JM, Huang JF, et al. Mortality attributable to smoking in China. N Engl J Med. 2009;360(2):150–9. doi: 10.1056/NEJMsa0802902. [DOI] [PubMed] [Google Scholar]
- 4.Liu BQ, Peto R, Chen ZM, Boreham J, Wu YP, Li JY, et al. Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. BMJ. 1998;317(7170):1411–22. doi: 10.1136/bmj.317.7170.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang J, Ou JX, Bai CX. Tobacco smoking in China: prevalence, disease burden, challenges and future strategies. Respirology. 2011;16(8):1165–72. doi: 10.1111/j.1440-1843.2011.02062.x. [DOI] [PubMed] [Google Scholar]
- 6.Novotny TE. The “ultimate prize” for big tobacco: opening the Chinese cigarette market by cigarette smuggling. PLoS Med. 2006;3(7):e279. doi: 10.1371/journal.pmed.0030279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rogers EM. Diffusion of innovations. 5. New York: Free Press; 2003. [Google Scholar]
- 8.Pampel FC. Diffusion, cohort change, and social patterns of smoking. Soc Sci Res. 2005;34(1):117–39. doi: 10.1016/j.ssresearch.2003.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mackay J, Amos A. Women and tobacco. Respirology. 2003;8(2):123–30. doi: 10.1046/j.1440-1843.2003.00464.x. [DOI] [PubMed] [Google Scholar]
- 10.Pampel FC. Global patterns and determinants of sex differences in smoking. Int J Comp Sociol. 2006;47(6):466–87. doi: 10.1177/0020715206070267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amos A, Greaves L, Nichter M, Bloch M. Women and tobacco: a call for including gender in tobacco control research, policy and practice. Tob Control. 2012;21(2):236–43. doi: 10.1136/tobaccocontrol-2011-050280. [DOI] [PubMed] [Google Scholar]
- 12.Hitchman SC, Fong GT. Gender empowerment and female-to-male smoking prevalence ratios. Bull World Health Organ. 2011;89(3):195–202. doi: 10.2471/BLT.10.079905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hermalin A, Lowry D. The decline of smoking among female birth cohorts in China in the 20th century: a case of arrested diffusion? Popul Res Policy Rev. 2012;31(4):545–70. doi: 10.1007/s11113-012-9239-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lam TH, Li ZB, Ho SY, Chan WM, Ho KS, Tham MK, et al. Smoking, quitting and mortality in an elderly cohort of 56,000 Hong Kong Chinese. Tob Control. 2007;16(3):182–9. doi: 10.1136/tc.2006.019505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin SJ. Estimating the determinants of smoking behavior in Taiwan. Subst Use Misuse. 2010;45(4):482–95. doi: 10.3109/10826080903498929. [DOI] [PubMed] [Google Scholar]
- 16.Morrow M, Barraclough S. Gender equity and tobacco control: bringing masculinity into focus. Glob Health Promot. 2010;17(1 Suppl):21–8. doi: 10.1177/1757975909358349. [DOI] [PubMed] [Google Scholar]
- 17.Khang Y-H, Cho H-J. Socioeconomic inequality in cigarette smoking: trends by gender, age, and socioeconomic position in South Korea, 1989–2003. Prev Med. 2006;42(6):415–22. doi: 10.1016/j.ypmed.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 18.Finch K, Novotny TE, Ma S, Qin D, Xia W, Xin G, et al. Smoking knowledge, attitudes, and behaviors among rural-to-urban migrant women in Beijing, China. Asia Pac J Public Health. 2010;22(3):342–53. doi: 10.1177/1010539509335034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Honjo K, Kawachi I. Effects of market liberalisation on smoking in Japan. Tob Control. 2000;9(2):193–200. doi: 10.1136/tc.9.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ho MG, Ma S, Chai W, Xia W, Yang G, Novotny TE. Smoking among rural and urban young women in China. Tob Control. 2010;19(1):13–8. doi: 10.1136/tc.2009.030981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright AA, Katz IT. Tobacco tightrope — balancing disease prevention and economic development in China. N Engl J Med. 2007;356(15):1493–6. doi: 10.1056/NEJMp078018. [DOI] [PubMed] [Google Scholar]
- 22.Xinhua. [Accessed 21 Feb 2013];Chinese women targeted by tobacco industry: report. 2010 http://www.china.org.cn/china/2010-05/29/content_20143458.htm.
- 23.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Uffelen JG, Wong J, Chau JY, van der Ploeg HP, Riphagen I, Gilson ND, et al. Occupational sitting and health risks: a systematic review. Am J Prev Med. 2010;39(4):379–88. doi: 10.1016/j.amepre.2010.05.024. [DOI] [PubMed] [Google Scholar]
- 25.Craggs C, Corder K, van Sluijs EM, Griffin SJ. Determinants of change in physical activity in children and adolescents: a systematic review. Am J Prev Med. 2011;40(6):645–58. doi: 10.1016/j.amepre.2011.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shin SS, Wan X, Wang Q, Raymond HF, Liu H, Ding D, et al. Perceived discrimination and smoking among rural-to-urban migrant women in China. J Immigr Minor Health. 2013;15(1):132–40. doi: 10.1007/s10903-012-9599-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wan X, Shin SS, Wang Q, Raymond HF, Liu H, Ding D, et al. Smoking among young rural to urban migrant women in China: a cross-sectional survey. PLoS ONE. 2011;6(8):e23028. doi: 10.1371/journal.pone.0023028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen X, Li X, Stanton B, Fang X, Lin D, Cole M, et al. Cigarette smoking among rural-to-urban migrants in Beijing, China. Prev Med. 2004;39(4):666–73. doi: 10.1016/j.ypmed.2004.02.033. [DOI] [PubMed] [Google Scholar]
- 29.Ma H, Unger JB, Chou CP, Sun P, Palmer PH, Zhou Y, et al. Risk factors for adolescent smoking in urban and rural China: findings from the China seven cities study. Addict Behav. 2008;33(8):1081–5. doi: 10.1016/j.addbeh.2008.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Wen CP, Tsai SP, Cheng TY, Hsu CC, Chen T, Lin HS. Role of parents and peers in influencing the smoking status of high school students in Taiwan. Tob Control. 2005;14 (Suppl 1):i10–5. doi: 10.1136/tc.2003.005637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang L, Wang W, Zhao Q, Vartiainen E. Psychosocial predictors of smoking among secondary school students in Henan, China. Health Educ Res. 2000;15(4):415–22. doi: 10.1093/her/15.4.415. [DOI] [PubMed] [Google Scholar]
- 32.Chuang Y-C, Chuang K-Y. Gender differences in relationships between social capital and individual smoking and drinking behavior in Taiwan. Soc Sci Med. 2008;67(8):1321–30. doi: 10.1016/j.socscimed.2008.06.033. [DOI] [PubMed] [Google Scholar]
- 33.Cai M, Qian J. Trends of smoking prevalence of Chinese women and associated factors. Chin J Hosp Stat. 2009;12(4):298–2. [Google Scholar]
- 34.Huang HL, Chen FL, Hsu CC, Yen YY, Chen T, Huang CM, et al. A multilevel-based study of school policy for tobacco control in relation to cigarette smoking among children in elementary schools: gender differences. Health Educ Res. 2010;25(3):451–63. doi: 10.1093/her/cyq014. [DOI] [PubMed] [Google Scholar]
- 35.Lau EM, Lee P, Lynn H, Sham A, Woo J. The epidemiology of cigarette smoking in Hong Kong Chinese women. Prev Med. 2003;37(5):383–8. doi: 10.1016/s0091-7435(03)00148-8. [DOI] [PubMed] [Google Scholar]
- 36.Lin YP, Yen LL, Pan LY, Chang PJ, Cheng TJ. Emerging epidemic in a growing industry: cigarette smoking among female microelectronics workers in Taiwan. Public Health. 2005;119(3):184–8. doi: 10.1016/j.puhe.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 37.Tsai YW, Tsai TI, Yang CL, Kuo KN, et al. Gender differences in smoking behaviors in an Asian population. J Womens Health. 2008;17(6):971–8. doi: 10.1089/jwh.2007.0621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang MS, Ko YC, Wen JK. Prevalences and related factors of substances use in female aborigines in southern Taiwan. Kaohsiung J Med Sci. 1996;12(11):634–40. [PubMed] [Google Scholar]
- 39.Yang G, Fan L, Tan J, Qi G, Zhang Y, Samet J, et al. Smoking in China: findings of the 1996 national Prevalence Survey. JAMA. 1999;282:1247–53. doi: 10.1001/jama.282.13.1247. [DOI] [PubMed] [Google Scholar]
- 40.Zheng P, Fu Y, Lu Y, Ji M, Hovell MF, Fu H. Community smoking behavior in Changqiao, Shanghai. Asia Pac J Public Health. 2008;20(2):94–101. doi: 10.1177/1010539507311182. [DOI] [PubMed] [Google Scholar]
- 41.Ding D, Hovell MF, Ji M, Hofstetter CR, Zheng P, Fu H, et al. Employment and social “determinants” of smoking in urbanizing China: a representative survey. Nicotine Tob Res. 2009;11(7):779–84. doi: 10.1093/ntr/ntp060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hosseinpoor AR, Parker LA, d’Espaignet ET, Chatterji S. Social determinants of smoking in low- and middle-income countries: results from the World Health Survey. PLoS One. 2011;6(5):e20331. doi: 10.1371/journal.pone.0020331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Centers for Disease Control and Prevention. Adult cigarette smoking in the United States: current estimate. 2011 http://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/
- 44.Huang Y, Ren J. Socioeconomic status and women’s smoking behavior: a literature review. Global J Health Sci. 2011;3(1):98–103. [Google Scholar]
- 45.Ma S. Affluence prompts more women in China to light up. CMAJ. 2010;182(12):557–8. doi: 10.1503/cmaj.109-3307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gan Q, Yang J, Yang G, Goniewicz M, Benowitz NL, Glantz SA. Chinese “herbal” cigarettes are as carcinogenic and addictive as regular cigarettes. Cancer Epidemiol Biomarkers Prev. 2009;18(12):3497–501. doi: 10.1158/1055-9965.EPI-09-0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wan X, Ma S, Hoek J, Yang J, Wu L, Zhou J, et al. Conflict of interest and FCTC implementation in China. Tob Control. 2012;21(4):412–5. doi: 10.1136/tc.2010.041327. [DOI] [PubMed] [Google Scholar]
- 48.Yang G. China wrestles with tobacco control. Bull World Health Organ. 2010;88:251–2. doi: 10.2471/BLT.10.040410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hu X, Cook S, Salazar MA. Internal migration and health in China. Lancet. 2008;372(9651):1717–9. doi: 10.1016/S0140-6736(08)61360-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wen M, Wang G. Demographic, psychological, and social environmental factors of loneliness and satisfaction among rural-to-urban migrants in Shanghai, China. Int J Comp Sociol. 2009;50(2):155–82. [Google Scholar]
- 51.Qiu P, Caine E, Yang Y, Chen Q, Li J, Ma X. Depression and associated factors in internal migrant workers in China. J Affect Disord. 2011;134(1–3):198–207. doi: 10.1016/j.jad.2011.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129(2):270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- 53.Niaura R, Shadel WG, Britt DM, Abrams DB. Response to social stress, urge to smoke, and smoking cessation. Addict Behav. 2002;27(2):241–50. doi: 10.1016/s0306-4603(00)00180-5. [DOI] [PubMed] [Google Scholar]
- 54.Cui X, Rockett IR, Yang T, Cao R. Work stress, life stress, and smoking among rural–urban migrant workers in China. BMC Public Health. 2012;12:979. doi: 10.1186/1471-2458-12-979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang X, Zhang J, Sun Y. Smoking status and its influence factors in female workers in public places in Hefei City. Chin J Public Health. 2012;1:100–2. [Google Scholar]
- 56.Alday J. [Accessed Feb 25 2013];Survey indicates fewer people in Beijing and Shanghai intended to give cigarettes as gifts after seeing mass media campaign. 2009 http://www.worldlungfoundation.org/ht/d/ReleaseDetails/i/6253FirefoxHTML%5CShell%5COpen%5CCommand.
- 57.Xinhua. [Accessed Jan 22 2013];Tobacco-free weddings: the new front in China’s anti-smoking campaign. 2011 http://news.xinhuanet.com/english2010/china/2011-10/05/c_131174900.htm.
- 58.Sarraf-Zadegan N, Boshtam M, Shahrokhi S, Naderi GA, Asgary S, Shahparian M, et al. Tobacco use among Iranian men, women and adolescents. Eur J Public Health. 2004;14(1):76–8. doi: 10.1093/eurpub/14.1.76. [DOI] [PubMed] [Google Scholar]
- 59.Schroer-Gunther MA, Zhou M, Gerber A, Passon AM. Primary tobacco prevention in China - a systematic review. Asian Pac J Cancer Prev. 2011;12(11):2973–80. [PubMed] [Google Scholar]
- 60.China Centers for Disease Control. 2010 China tobacco control report. Beijing: China Center for Disease Control, Office of Tobacco Control; 2010. [Google Scholar]
- 61.World Health Organization. WHO report on the global tobacco epidemic, 2008: The MPOWER package. Geneva: World Health Organization; 2008. [Google Scholar]