Abstract
OBJECTIVE
To estimate nationwide trends in the prevalence of maternal congenital heart disease (CHD) and determine whether women with CHD are more likely than women without maternal CHD to have medical and obstetric complications.
METHODS
The 2000–2010 Nationwide Inpatient Sample was queried for International Classification of Diseases, 9th Revision, Clinical Modification codes to identify delivery hospitalizations of women with and without CHD. Trends in the prevalence of CHD were determined and then rates of complications were reported for CHD per 10,000 delivery hospitalizations. For Nationwide Inpatient Sample 2008–2010, logistic regression was used to examine associations between CHD and complications.
RESULTS
From 2000 to 2010, there was a significant linear increase in the prevalence of CHD from 6.4 to 9.0 per 10,000 delivery hospitalizations (P<.001). Multivariable logistic regression demonstrated that all selected medical complications, including mortality (17.8 compared with 0.7/10,000 deliveries, adjusted odds ratio [OR] 22.10, 95% confidence interval [CI] 13.96–34.97), mechanical ventilation (91.9 compared with 6.9/10,000, adjusted OR 9.94, 95% CI 7.99–12.37), and a composite cardiovascular outcome (614 compared with 34.3/10,000, adjusted OR 10.54, 95% CI 9.55–11.64) were more likely to occur among delivery hospitalizations with maternal CHD than without. Obstetric complications were also common among women with CHD. Delivery hospitalizations with maternal CHD that also included codes for pulmonary circulatory disorders had higher rates of medical complications compared with hospitalizations with maternal CHD without pulmonary circulatory disorders.
CONCLUSION
The number of delivery hospitalizations with maternal CHD in the United States is increasing, and although we were not able to determine whether correction of the cardiac lesion affected outcomes, these hospitalizations have a high burden of medical and obstetric complications.
Congenital heart disease (CHD) is common and is estimated to affect approximately 1% of neonates born in the United States annually,1 but there are wide variations in the incidence reported, primarily as a result of variations between studies and in the types of congenital lesions included in the definition of CHD.2 Advances in medical and surgical treatment of CHD have significantly improved the long-term outcomes of children with CHD with increasing numbers of those affected now surviving into adulthood.3 It was estimated in 2005 that there were 1 million adults living with CHD, with an anticipated growth in prevalence at a rate of 5% per year.3–7 As more women with CHD survive into childbearing age, a larger number of them has the potential to become pregnant.
Physiologic changes in pregnancy increase demands on the heart. Increases in cardiac output, blood volume, contractility, and heart rate can cause significant circulatory burden, which can lead to cardiac decompensation, especially in a pregnant women with CHD.8 Previous studies in pregnant women with CHD have found rates of cardiac complications ranging from 11% to 19% as well as increased obstetric and neonatal complications in comparison with women without CHD.4,5,9–11 At least two studies investigated the risk of cardiac morbidity and mortality during pregnancy for women with cardiac disease10,11 taking into account prior cardiac events as well as echocardiographic results. These studies, however, have largely been limited to single academic centers and had small sample sizes. Some have included patients with multiple forms of heart disease, congenital and acquired, making it difficult to determine risks of death or severe complications associated with CHD. Therefore, using a nationwide database, we sought to estimate the nationwide prevalence of CHD among delivery hospitalizations and test the hypothesis that, when compared with delivery hospitalizations without maternal CHD, these hospitalizations are more likely to result in medical and obstetric complications.
MATERIALS AND METHODS
The Nationwide Inpatient Sample from the Healthcare Cost and Utilization Project of the Agency for Health-care Research and Quality was queried for delivery-related discharges during 2000–2010.12 The Nationwide Inpatient Sample is a 20% stratified sample of discharges from U.S. community hospitals, excluding rehabilitation and long-term acute care hospitals. Hospitals are stratified based on ownership, bed size, teaching status, urban–rural location, and region. The Nationwide Inpatient Sample contains information from approximately 8 million hospital discharges from more than 1,000 hospitals and represents the largest all-payer inpatient care database in the United States.
The information included in the Nationwide Inpatient Sample contains safeguards to protect the privacy of individual patients, physicians, and hospitals. Although the data are limited to discharge diagnoses and demographic information, the Nationwide Inpatient Sample allows for the study of relatively rare conditions because of the large sample size. Information in the Nationwide Inpatient Sample includes discharge diagnoses and procedure codes based on the International Classification of Diseases, 9th Revision, Clinical Modifications (ICD-9-CM).12
Using the Nationwide Inpatient Sample for each of the years from 2000 through 2010, all delivery-related discharge records were identified. A delivery hospitalization was defined by discharge records that included a delivery code (ICD-9-CM codes 74.x [except 74.91] for cesarean delivery; and codes V27, 72.x, 73.x, and 650–659 [with appropriate delivery code subheadings] for general delivery). Delivery hospitalizations were also identified by diagnosis-related group codes. For the years 2000–2007, diagnosis-related group codes 370, 371, 372, 373, 374, and 375 were used to identify cesarean and vaginal deliveries, respectively. For 2008–2010, diagnosis-related group codes 765 or 766 and codes 767, 768, 774, and 775 were used to identify cesarean and vaginal delivery hospitalizations, respectively.13–20
Delivery hospitalizations with CHD were identified by ICD-9-CM codes 745.x–747.x and 648.5× in line with our previous work.16 The delivery hospitalization is the unit of analysis in our study and there are no links in the Nationwide Inpatient Sample that allow individuals to be followed for multiple admissions.
Medical complications that served as outcomes included: in-hospital mortality, mechanical ventilation, transfusion, myocardial infarction–ischemia, cardiac arrest–ventricular fibrillation, acute heart failure, pneumonia, pulmonary edema, acute respiratory distress syndrome, pulmonary embolism, deep vein thrombosis, stroke–cerebrovascular accident, sepsis, pyelonephritis, and acute renal failure. We also investigated a composite cardiovascular outcome because it was used in previous studies that included any one of the following: in-hospital mortality, myocardial infarction, cardiac arrest, arrhythmia, heart failure, or stroke.10,11
Obstetric complications that also were analyzed as outcomes included: cesarean delivery, operative vaginal delivery, gestational diabetes, hypertensive disorders in pregnancy (eclampsia, preeclampsia, and gestational hypertension), fetal growth restriction, stillbirth, preterm labor, placental abruption, postpartum hemorrhage, and chorioamnionitis.
Pulmonary hypertension and other pulmonary circulatory disorders are a source of significant morbidity and mortality among pregnant women and can be associated with CHD.21 Thus, in our study we also tested the hypothesis that pulmonary disorders (defined by ICD-9-CM codes for secondary pulmonary hypertension, disorders of pulmonary circulation, and pulmonary heart disease) would modify the effect of CHD on medical and obstetric outcomes. We therefore stratified the analyses for women with and without these pulmonary conditions. Race–ethnicity is categorized by the Nationwide Inpatient Sample as: white, black, Hispanic, Asian or Pacific Islander, Native American, other, unknown, or missing. In-hospital mortality was determined by the Nationwide Inpatient Sample variable “DIED” being coded as 1.
A priori, we elected to control for comorbid conditions. Our list of preselected comorbid conditions included asthma, pregestational diabetes, thyroid disorders, systemic lupus erythematosus, rheumatoid arthritis–collagen vascular disease, human immunocompromised virus, thrombophilia–antiphospholipid antibody syndrome, anemia, thrombocytopenia, drug use, alcohol use, tobacco use, chronic hypertension, and chronic renal failure. The list of ICD-9-CM codes used to identify selected co-morbid conditions as well as medical and obstetric complications can be found in Appendix 1, available online at http://links.lww.com/AOG/A662.
To determine the change in prevalence of CHD among delivery hospitalizations from 2000 through 2010, for each year, the number of delivery hospitalizations with CHD and without CHD was determined. The rate of delivery hospitalization with CHD per 10,000 total delivery hospitalizations was then calculated. Linear regression was then used to determine whether there was a linear change in CHD prevalence at delivery over the 11-year time period.
Because previous studies have shown that the prevalence of several comorbid conditions has been changing rapidly among delivery hospitalizations in the United States,20 we examined maternal characteristics and risk of severe medical and obstetric complications among hospitalizations with and without CHD using the last 3 years of data (2008–2010) to provide a contemporary picture. We assessed differences in demographic variables between delivery discharges with CHD and delivery discharges without CHD using Student’s t test or Wilcoxon signed-rank tests for continuous variables and χ2 tests for categorical variables. We obtained the crude and adjusted odds ratios and their 95% confidence intervals (CIs) of medical and obstetric complications present during delivery hospitalizations with CHD compared with those without CHD using logistic regression. Each adjusted logistic regression model included age, race–ethnicity, insurance status, multiple gestation, mode of delivery, and all preselected comorbid conditions. Absolute rates with 95% CIs for medical and obstetric complications were also determined from the Nationwide Inpatient Sample and expressed per 10,000 deliveries. To determine the absolute risk of each outcome among women with CHD compared with the entire pregnant population, the population-attributable risk percent for each outcome was calculated.22 Discharge weighting variables are available in the Nationwide Inpatient Sample from which national estimates were made. Statistical significance was assigned based on a P value <.05 for all analyses. Analyses were performed using SAS 9.3 and GraphPad Prism 6.0 for Macintosh. The study was reviewed and deemed exempt by the Duke University Health System and the Centers for Disease Control and Prevention institutional review boards.
RESULTS
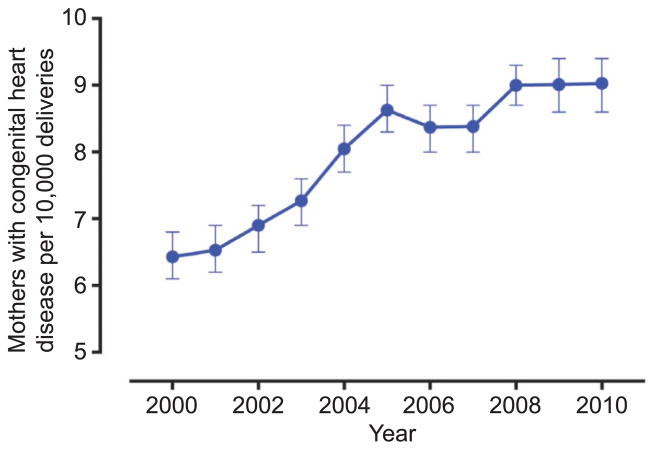
During 2000–2010, there was a significant linear increase in the number of delivery hospitalizations of women with CHD; the rate of CHD among delivery hospitalizations increased from 6.4 (95% CI 6.2–6.7) per 10,000 delivery hospitalizations in 2000 to 9.0 (95% CI 8.7–9.3) per 10,000 delivery hospitalizations in 2010 (P<.001; Fig. 1). Among the 12,524,118 delivery hospitalizations between 2008 and 2010, 10,660 (8.51 [95% CI 8.4–8.7]/10,000 deliveries) occurred in women with CHD. White race was more prevalent among women with delivery hospitalizations with CHD compared with women with delivery hospitalizations without CHD (52.6% compared with 44.2%, P<.001), whereas black, Hispanic, or Asian-Pacific race was less prevalent (8.9% compared with 11.9%, 15.2% compared with 19.2%, and 2.5 compared with 4.4%, respectively). Race–ethnicity data were missing for 16.6% and 15.5% of the delivery hospitalizations with CHD and without CHD, respectively (Table 1). Hospitalizations with CHD had a slightly longer median length of stay and were accompanied by greater hospital charges compared with hospitalizations without CHD. There was no statistical difference in the mean age of women with and without CHD at a delivery hospitalization (Table 1).
Fig. 1.
Trend in delivery hospitalizations among women with congenital heart disease per 10,000. There was a significant linear increase in the delivery hospitalizations of women with congenital heart disease from 6.4 (95% confidence interval [CI] 6.2–6.7) per 10,000 delivery hospitalizations in 2000 to 9.0 (95% CI 8.7–9.3) per 10,000 delivery hospitalizations in 2010 (R2=0.91, P<.001). Error bars at each point estimate are 95% CIs.
Thompson. Maternal Congenital Heart Disease and Outcomes. Obstet Gynecol 2015.
Table 1.
Characteristics of Women With and Without Congenital Heart Disease at Delivery Hospitalizations, Nationwide Inpatient Sample, 2008–2010
| Characteristic | CHD (n=10,660) | No CHD (n=12,513,458) | P |
|---|---|---|---|
| Race–ethnicity | <.001 | ||
| White | 5,607 (52.6) | 5,528,356 (44.2) | |
| Black | 948 (8.9) | 1,489,885 (11.9) | |
| Hispanic | 1,625 (15.2) | 2,403,708 (19.2) | |
| Asian-Pacific islander | 267 (2.5) | 556,216 (4.4) | |
| Native American | 104 (1.0) | 95,130 (0.8) | |
| Other | 341 (3.2) | 502,099 (4.0) | |
| Missing | 1,768 (16.6) | 1,938,065 (15.5) | |
| Age (y) | 27.4±13.9 | 27.6±13.7 | .053 |
| Private insurance | 5,427 (50.9) | 6,216,056 (49.7) | <.001 |
| Resides in zip code with median income in lowest quartile | 2,786 (26.1) | 3,303,121 (26.4) | <.001 |
| Length of stay (d) | 3 (2–4) | 2 (2–3) | <.001 |
| Total charges ($) | 12,315 (8,089–19,844) | 10,022 (6,807–15,108) | <.001 |
CHD, congenital heart disease.
Data are n (%), mean±standard deviation, or median (interquartile range) unless otherwise specified.
Among delivery hospitalizations with CHD, the most commonly coded congenital heart lesions were atrial septal defects (22.6%), ventricular septal defects (14.5%), left-sided congenital valvular lesions (13.8%), and right-sided congenital valvular lesions (7.5%). Other lesions included coarctation of the aorta (2.9%), tetralogy of Fallot (2.6%), transposition of the great vessels (1.5%), Ebstein’s anomaly (1.4%), total anomalous pulmonary return (0.1%), and truncus arteriosus (0.1%). Approximately 15% (1,604) of delivery hospitalizations with CHD had a nonspecific code for CHD. There were no delivery hospitalizations with codes for hypoplastic left heart syndrome. Of hospitalizations with CHD, 3.6% (n=388) also had a code for secondary pulmonary hypertension, pulmonary heart disease, or disorders of pulmonary circulation.
The absolute rates and odds for comorbid conditions, except for alcohol and substance abuse, were higher among women with delivery hospitalizations with CHD than without CHD codes (Appendix 2, available online at http://links.lww.com/AOG/A663). The absolute rate of in-hospital mortality and the composite cardiovascular outcome was higher among delivery hospitalizations with CHD compared with delivery hospitalizations without CHD (in-hospital mortality: 17.8 [95% CI 10.7–27.8] compared with 0.71 [95% CI 0.61–0.82]/10,000 deliveries; composite cardiovascular outcome: 614 [95% CI 570–662] compared with 34.3 [95% CI 33.9–34.6]/10,000 deliveries). Other absolute rates of medical complications are found in Table 2. The odds of in-hospital mortality (adjusted OR [OR] 22.10, 95% CI 13.96–34.97), mechanical ventilation (adjusted OR 9.94, 95% CI 7.99–12.37), and transfusion (adjusted OR 2.56, 95% CI 2.29–2.89) were greater among delivery hospitalizations with CHD in comparison with delivery hospitalizations without CHD (Table 2). The odds of severe cardiac and thromboembolic events were greater among delivery hospitalizations with than without CHD with adjusted ORs ranging from 3.15 (95% CI 2.01–4.92) for deep vein thrombosis to 35.49 (95% CI 20.54–61.33) for myocardial infarction (Table 2). The odds of most obstetric complications also were significantly greater among hospitalizations with CHD with adjusted ORs ranging from 1.17 (95% CI 1.07–1.27) for gestational diabetes to 2.08 (95% CI 1.88–2.30) for fetal growth restriction (Table 2).
Table 2.
Estimated Total and Rate (per 10,000 Delivery Hospitalizations) of Medical and Obstetric Complications Among Women With and Without Congenital Heart Disease at Delivery Hospitalization
| Condition or Event | CHD (n=10,660), n (per 10,000 [95% CI]) | No CHD (n=12,513,458), n (per 10,000 [95% CI]) | Adjusted OR* (95% CI) | Population-Attributable Risk Percent† |
|---|---|---|---|---|
| In-hospital mortality | 19 (17.8 [10.7–27.8]) | 892 (0.71 [0.67–0.76]) | 22.10 (13.96–34.97) | 2.0 |
| Composite cardiovascular outcome‡ | 655 (614 [570–662) | 42,887 (34.3 [33.9–34.6]) | 10.54 (9.55–11.64) | 1.4 |
| Mechanical ventilation | 98 (91.9 [74.7–112]) | 8,660 (6.9 [6.8–7.1]) | 9.94 (7.99–12.37) | 1.0 |
| Transfusion | 320 (300 [269–334]) | 129,347 (103 [103–104]) | 2.56 (2.29–2.89) | 0.2 |
| Cardiac events | ||||
| Myocardial infarction–ischemia | 14 (13.1 [7.2–22.0]) | 366 (0.29 [0.26–0.32]) | 35.49 (20.54–61.33) | 3.6 |
| Cardiac arrest–ventricular fibrillation | 15 (14.1 [7.9–23.2]) | 839 (0.67 [0.63–0.72]) | 13.4 (7.22–24.86) | 1.7 |
| Arrhythmia | 453 (425 [387–465]) | 36,641 (29.3 [29.0–29.6]) | 11.70 (10.50–13.03) | 4.1 |
| Acute heart failure | 184 (173 [149–199]) | 4,254 (3.4 [3.3–3.5]) | 35.42 (29.89–41.98) | 1.1 |
| Pulmonary events | ||||
| Pneumonia | 69 (64.7 [50.4–81.8]) | 11,821 (9.4 [9.3–9.6]) | 5.06 (3.87–6.61) | 0.5 |
| Pulmonary edema | 11 (10.3 [5.2–18.5]) | 1,997 (1.6 [1.5–1.7]) | 2.85 (1.22–6.64) | 0.5 |
| Acute respiratory distress syndrome | 34 (31.9 [22.1–44.5]) | 2,791 (2.2 [2.1–2.3]) | 12.44 (8.83–17.52) | 1.1 |
| Thromboembolic events | ||||
| Pulmonary embolism | 35 (32.8 [22.9–45.6]) | 3,405 (2.7 [2.6–2.8]) | 9.74 (6.95–13.64) | 0.9 |
| Deep vein thrombosis | 20 (18.8 [11.5–29.0]) | 6,165 (4.9 [4.8–5.1]) | 3.15 (2.01–4.92) | 0.2 |
| Stroke–cerebrovascular accident | 39 (36.6 [26.0–50.0]) | 1,720 (1.4 [1.3–1.4]) | 22.23 (16.09–30.73) | 2.1 |
| Infections | ||||
| Sepsis | 24 (22.5 [14.4–33.5]) | 6,280 (5.0 [4.9–5.1]) | 3.50 (2.22–5.51) | 0.3 |
| Renal event | ||||
| Acute renal failure | 31 (29.1 [19.8–41.3]) | 6,873 (5.5 [5.4–5.6]) | 2.68 (1.73–4.15) | 0.4 |
| Obstetric events | ||||
| Cesarean delivery§ | 4,335 (4,067 [3,973–4,161]) | 4,037,021 (3,226 [3,223–3,229]) 1.36 (1.30–1.42) | 0.02 | |
| Operative vaginal delivery§ | 984 (923 [869–980]) | 791,259 (632 [631–634]) | 1.54 (1.44–1.66) | 0.04 |
| Gestational diabetes | 669 (628 [582–675]) | 708,403 (566 [565–567]) | 1.17 (1.07–1.27) | 0.01 |
| Hypertensive disorders in pregnancy | 948 (889 [836–945]) | 922,514 (737 [736–739]) | 1.05 (0.97–1.13) | 0.02 |
| Fetal growth restriction | 525 (492 [452–535]) | 270,954 (216 [216–217]) | 2.08 (1.88–2.30) | 0.11 |
| Stillbirth | 58 (54.4 [41.3–70.3]) | 51,016 (40.8 [40.4–41.1]) | 1.50 (1.16–1.94) | 0.03 |
| Preterm labor | 1,423 (1,335 [1,271–1,401]) | 1,016,901 (813 [811–814]) | 1.66 (1.56–1.77) | 0.05 |
| Placental abruption | 178 (167 [143–193]) | 134,591 (108 [107–108]) | 1.54 (1.32–1.80) | 0.05 |
| Postpartum hemorrhage | 384 (360 [326–397]) | 319,079 (255 [254–256]) | 1.38 (1.24–1.54) | 0.04 |
| Chorioamnionitis | 260 (244 [215–275]) | 323,216 (258 [257–259]) | 0.91 (0.79–1.04) | 0.00 |
CHD, congenital heart disease; CI, confidence interval; OR, odds ratio.
Data are n (/10,000 [95% CI]) unless otherwise specified.
Adjusted ORs for each outcome associated with CHD and population-attributable risk percent for each outcome attributed to delivery hospitalizations with CHD, Nationwide Inpatient Sample, 2008–2010.
OR adjusted for age, race–ethnicity, insurance status, multiple gestation, mode of delivery, asthma, diabetes, thyroid disorders, systemic lupus erythematosus, rheumatoid arthritis–collagen vascular disease, human immunodeficiency virus, thrombophilia–antiphospholipid antibody syndrome, anemia, thrombocytopenia, drug use, alcohol use, tobacco, chronic hypertension, and chronic renal failure. Referent group is hospitalizations in women without CHD.
Population-attributable risk percent was calculated using the equation: PAR, Pe (RRe−1)/[1+Pe (RRe−1)], where PAR, population-attributable risk; Pe, prevalence of the exposure; and RRe, relative risk of disease resulting from the exposure.22
Cardiovascular composite outcome includes in-hospital mortality, myocardial infarction, cardiac arrest, arrhythmia, heart failure, or stroke.
Mode of delivery not controlled for in calculating adjusted OR for cesarean and operative vaginal delivery.
Delivery hospitalizations with CHD represented 0.085% of all deliveries between 2008 and 2010, but 2.0% of all in-hospital deaths occurred among women with a CHD code at delivery discharge (Table 2). Similarly, delivery hospitalizations for women with CHD contributed 3.6% cases of myocardial infarction, 1.7% cases of cardiac arrest–ventricular fibrillation, 1.1% cases of acute heart failure, 4.1% cases of arrhythmia, and 2.1% cases of stroke among women during admissions for delivery between 2008 and 2010. Table 2 provides additional population-attributable risk percent values for other medical and obstetric outcomes calculated for delivery hospitalizations with CHD. Population-attributable risk percent for obstetric complications except for fetal growth restriction (0.11%) was less than 0.05%.
There were 19 deaths among delivery hospitalizations with CHD providing an in-hospital mortality rate of 17.8 (95% CI 10.7–27.8) deaths per 10,000 deliveries among women with CHD compared with 0.71 (95% CI 0.67–0.76) deaths per 100,000 deliveries among delivery hospitalizations without CHD. The odds of in-hospital mortality, cardiovascular composite outcome variable, and other medical complications varied among delivery hospitalizations with CHD compared with hospitalizations without CHD depending on whether women with CHD also had pulmonary circulatory disorders (Table 3). The odds of in-hospital mortality, acute heart failure, arrhythmia, acute respiratory distress syndrome, mechanical ventilation, blood transfusion, and the composite cardiovascular outcome were greater for delivery hospitalizations with CHD and a pulmonary circulatory disorder compared with hospitalizations without CHD (Table 3). The adjusted ORs for these adverse cardiac outcomes, except for arrhythmia, were also greater among hospital discharges having both CHD and a pulmonary circulatory disorder compared with hospital discharges with CHD but without pulmonary circulatory disorders. Within hospitalizations that included both CHD and pulmonary vascular conditions, the number of these patients with myocardial infarction, cardiac arrest, deep venous thrombosis, pulmonary embolism, stroke, sepsis, or acute renal failure was fewer than 11 and was therefore not reported.12 The adjusted ORs for obstetric complications among delivery hospitalizations with CHD complicated by pulmonary circulatory disorder were also greater compared with adjusted ORs for obstetric complications among delivery hospitalizations without CHD uncomplicated by pulmonary circulatory disorder. However, the difference in obstetric complications between women with CHD who had pulmonary circulatory disorders and women with CHD who did not have pulmonary circulatory disorders was small and did not reach statistical significance based on overlapping of 95% CIs (Table 3).
Table 3.
Estimated Total, Rate (per 10,000 Delivery Hospitalizations), and Adjusted Odds Ratios for Medical and Obstetric Complications Among Women With Congenital Heart Disease at Delivery Hospitalization Stratified by Presence of Pulmonary Circulatory Disorders, Nationwide Inpatient Sample, 2008–2010
| Medical or Obstetric Outcome | Deliveries With Pulmonary Circulatory Disorder
|
Deliveries Without Pulmonary Circulatory Disorder
|
||
|---|---|---|---|---|
| CHD With Pulmonary Circulatory Disorder (n=388)* | Adjusted OR† (95% CI) | CHD Without Pulmonary Circulatory Disorder (n=10,272) | Adjusted OR† (95% CI) | |
| Medical complications | ||||
| In-hospital mortality | — | 146 (75.09–283.05) | — | 11.45 (5.95–22.02) |
| Composite cardiovascular outcome‡ | 70 (1,804 [1,434–2,224]) | 43.07 (32.51–57.07) | 585 (569 [525–616]) | 14.00 (12.74–15.40) |
| Mechanical ventilation | 15 (387 [218–630]) | 19.88 (11.52–34.31) | 83 (80.8 [64.4–100]) | 8.86 (6.97–11.25) |
| Transfusion | 40 (1,031 [747–1,377]) | 5.63 (3.79–8.18) | 280 (273 [242–306]) | 2.35 (2.07–2.68) |
| Acute heart failure | 54 (1,392 [1,063–1,777]) | 188 (132–269) | 130 (127 [106–150]) | 24.72 (20.12–30.38) |
| Arrhythmia | 11 (283 [142–502]) | 6.78 (3.63–12.69) | 442 (430 [392–471]) | 11.91 (10.68–13.29) |
| Acute respiratory distress syndrome | 11 (283 [142–502]) | 47.21 (24.35–91.54) | 23 (22.4 [14.2–33.6]) | 9.47 (6.32–14.19) |
| Obstetric events | ||||
| Cesarean delivery§ | 191 (4,923 [4,415–5,432]) | 1.78 (1.44–2.21) | 4,144 (4,034 [3,939–4,130]) | 1.34 (1.28–1.40) |
| Operative vaginal delivery§ | 39 (1,005 [725–1,348]) | 1.81 (1.27–2.58) | 945 (920 [865–977]) | 1.53 (1.43–1.65) |
| Gestational diabetes | 42 (1,082 [791–1,435]) | 1.47 (1.04–2.08) | 627 (610 [565–658]) | 1.15 (1.05–1.26) |
| Hypertensive disorders in pregnancy | 70 (1,804 [1,434–2,227]) | 1.83 (1.37–2.45) | 878 (855 [801–910] | 1.01 (0.94–1.10) |
| Fetal growth restriction | 20 (515 [318–785]) | 2.28 (1.45–3.59) | 505 (492 [451–535]) | 2.07 (1.87–2.29) |
| Stillbirth | 0 (0 [0–94.6]) | — | 58 (56.5 [42.9–72.9]) | 1.58 (1.22–2.05) |
| Preterm labor | 67 (1,727 [1,364–2,140]) | 1.82 (1.37–2.44) | 1,356 (1,320 [1,255–1,387]) | 1.65 (1.55–1.76) |
| Postpartum hemorrhage | 14 (361 [199–598]) | 0.79 (0.41–1.51) | 370 (360 [325–398]) | 1.41 (1.26–1.58) |
| Chorioamnionitis | 16 (412 [237–661]) | 1.71 (1.03–2.85) | 244 (237 [209–269]) | 0.87 (0.76–1.01) |
CHD, congenital heart disease; CI, confidence interval; OR, odds ratio.
Data are n (/10,000 [95% CI]) unless otherwise specified.
The number of patients with CHD and who also a had pulmonary circulatory disorder who experienced a myocardial Infarction, cardiac arrest, deep venous thrombosis, pulmonary embolism, stroke, sepsis, or acute renal failure was fewer than 11 and were therefore not reported. When the 19 deaths that occurred in the entire CHD population were divided into presence or absence of pulmonary circulatory disorder, one of the groups had fewer than 11 patients; therefore, neither were reported.
OR adjusted for age, race–ethnicity, insurance status, multiple gestation, mode of delivery, asthma, diabetes, thyroid disorders, systemic lupus erythematosus, rheumatoid arthritis–collagen vascular disease, human immunodeficiency virus, thrombophilia–antiphospholipid antibody syndrome, anemia, thrombocytopenia, drug use, alcohol use, tobacco, chronic hypertension, and chronic renal failure. Referent group is delivery hospitalizations among women without CHD.
Cardiovascular composite outcome includes in-hospital mortality, myocardial infarction, cardiac arrest, arrhythmia, heart failure, or stroke.
Mode of delivery not controlled for in calculating adjusted OR for cesarean and operative vaginal delivery.
The risk for the composite cardiovascular outcome differed by specific cardiac lesion. The composite cardiovascular outcome was commonly seen among women with CHD who also had a code for pulmonary circulatory disorder. Of the 655 women with CHD who had the composite cardiovascular outcome, 585 (89.3%) also had a code for pulmonary circulatory disorder. Among all 655 women with CHD, the risk for the composite cardiovascular outcome by cardiac lesion was as follows: atrial septal defect (138/2,408 [5.7%] of discharges), ventricular septal defect (64/ 1,549 [4.1%]), congenital left-sided valvular lesions (88/ 1,562 [5.6%]), congenital right-sided valvular lesions (51/801 [6.4%]), coarctation of the aorta (31/315 [9.8%]), tetralogy of Fallot (21/277 [7.6%]), transposition of the great vessels (19/156 [12.2%]), Ebstein’s anomaly (39/153 [25.5%]), and unspecified lesion (77/1,578 [4.9%]). There were only 19 deaths to women with CHD. When these deaths were subclassified by specific cardiac lesion, each group had 10 or fewer women and, therefore, could not be reported per Nationwide Inpatient Sample data use agreement.
DISCUSSION
In this nationwide U.S. study, we demonstrated that the number of delivery hospitalizations with CHD has significantly increased from 6.4 to 9.0 per 10,000 deliveries from 2000 to 2010. After controlling for age, race, insurance status, multiple gestation, mode of delivery, and comorbid conditions, the odds of medical cardiovascular and obstetric complications occurring were 10.5–35.5 and 1.2–2.1 times higher, respectively, among delivery hospitalizations with CHD compared with those without CHD. Additionally, although delivery hospitalizations with CHD made up only 0.085% of all deliveries, they accounted for 2% of in-hospital deaths and between 1.1% and 4.1% of medical cardiovascular complications such as myocardial infarction, cardiac arrest, arrhythmia, heart failure, and stroke. Finally, in our study, all adverse medical outcomes except for arrhythmia were significantly more likely among hospitalizations that had both CHD and pulmonary vascular conditions compared with hospitalization with CHD only.
Our findings add to those from prior publications, which have reported worse outcomes in pregnant women with CHD compared with those without such conditions.4,5,9–11 In a study of 562 pregnant women with heart disease receiving care in 13 Canadian cardiac and obstetric teaching hospitals, Siu et al10 found that composite cardiovascular outcome (pulmonary edema, arrhythmia, stroke, or cardiac death) complicated 13% of 617 pregnancies. Two other groups of researchers have utilized the Nationwide Inpatient Sample to determine associated outcomes among pregnant women with CHD; both studies primarily focused on cardiovascular events.4,23 The Registry of Pregnancy and Cardiac disease investigators recently published on outcomes of 872 women with congenital heart disease.24 Among these women, they found a maternal mortality rate of 0.5% and 8.0% of women with CHD developed heart failure during the pregnancy.24 Using 1998–2007 data on delivery hospitalizations in the Nationwide Inpatient Sample, Karamlou et al4 found a rate of composite cardiac complications (cardiac arrhythmia, cardiac arrest, or cardiac events related to anesthesia) of 2.3% in women with CHD compared with 0.2% in those without CHD; they also reported a maternal in-hospital mortality rate of 93 per 100,000 deliveries among women with CHD. Opotowsky et al23 also studied delivery discharges over the same timeframe and found that 4.0% of CHD delivery hospitalizations were associated with a cardiovascular event defined as death, heart failure, arrhythmia, cerebrovascular accident–transient ischemic attack, thromboembolic events, and unspecified cardiovascular complications of pregnancy compared with a 0.28% among delivery hospitalizations without CHD; the in-hospital mortality rate in their study was 150 per 100,000 deliveries among women with CHD. Although our study also used the Nationwide Inpatient Sample, we analyzed a much wider range of medical and obstetric complications, utilized more recent data, controlled for comorbidities that likely were pre-existing medical conditions, and then provided outcome data stratified by the presence or absence of pulmonary circulatory disorders, which is an important predictor of adverse outcomes. Lastly, the inclusion of population-attributable risk percent calculations in our study provides an estimate of the total burden of CHD to adverse outcomes among all delivery hospitalizations.
Given that certain maternal cardiac conditions are associated with high maternal morbidity and mortality rates, timely and competent counseling about contraception is an essential component of care of women with CHD. A limited number of studies have investigated physician’s knowledge, attitudes, and practices regarding contraception among women with CHD. According to the results of a study from Germany, of those women with CHD who were using contraception, approximately 20% were using a form felt to be contraindicated for their specific cardiac condition and almost 30% of sexually active women in the group with high pregnancy-associated risks were not using contraception.25 In the same study, 43% of the women had not been counseled about contraception, and 48% had not been informed of the pregnancy-related risks by their treating physician.
There are limitations to our study. First, the Nationwide Inpatient Sample relies on accurate coding of medical conditions at the time of discharge. It is possible that unless a condition was clinically present at the time of discharge, it may not have been coded during that admission. Furthermore, women with CHD may have been more likely to have comorbid conditions coded than women without CHD. By controlling for coexisting medical conditions, we attempted to estimate the role of CHD alone on medical and obstetric outcomes at the time of delivery. However, if a comorbid condition was present but not coded, we may have overestimated the adverse effect of CHD on the outcomes of interest. Next, the Nationwide Inpatient Sample is unable to distinguish between women with repaired compared with unrepaired CHD lesions. Other studies suggest that pregnant women with repaired lesions tend to do better overall than those without repair; however, as a result of limitations with the Nationwide Inpatient Sample, we could not determine whether outcomes varied by whether the CHD lesion was corrected or not.5,6 Next, our study only evaluated outcomes in women at the time of delivery. Because women could have multiple antepartum or postpartum admissions, but only one admission for delivery, we estimated the number of medical and obstetric complications occurring at the subject level for a given pregnancy. However, by limiting the study to only delivery hospitalizations, we were unable to draw conclusions concerning outcomes occurring at other times during pregnancy or in the postpartum period. Similarly, by focusing only on delivery hospitalization, we did not identify all maternal deaths, defined as deaths from pregnancy complications occurring during pregnancy or within 42 days of delivery.26 Hence, it is possible that we underestimated the overall risk of maternal mortality and severe complications among women with CHD. Lastly, our study demonstrated an increase in the number of deliveries to women with CHD over the study time period. Although unlikely, it is possible that rather than an increase in the number of women with CHD who are becoming pregnant, the increase could be the result of better coding and identification of women with CHD at the time of delivery.
In summary, the number of births to women with CHD is increasing. In-hospital mortality, medical cardiovascular complications including myocardial infarction, cardiac arrest, arrhythmia, heart failure, and stroke as well as obstetric complications are more likely to take place among delivery hospitalizations with CHD in comparison with delivery hospitalizations without CHD. Furthermore, the risks of medical complications are even greater among women with CHD who also have pulmonary circulatory disorders. Although these complications are infrequent, they are not trivial. With pediatric medical and surgical technologies continuing to advance, increasing numbers of women with CHD will survive to childbearing age and, therefore, the percentage of pregnancies to these women will likely continue to increase. Women with CHD as well as their physicians should be aware of the increased risks of medical and obstetric complications, including maternal death during delivery hospitalizations, and these women should be counseled accordingly, ideally before becoming pregnant. Appropriate prenatal and antenatal care by a multidisciplinary team is essential to help ensure a successful pregnancy for both the woman and the fetus, although there is no recommended optimal management plan for pregnant women with CHD. Thus, further studies are required to determine which other factors (eg, types and severity of CHD lesions, previous surgical treatment of CHD, prenatal care, mode of delivery, clinical management, cardiac function) may influence the risk for adverse outcomes among women with CHD during pregnancy and delivery.
Supplementary Material
Footnotes
Presented in part as an abstract at the 34th Annual Meeting of the Society for Maternal-Fetal Medicine, New Orleans, Louisiana, February 3–8, 2014.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
LEVEL OF EVIDENCE: II
Financial Disclosure
The authors did not report any potential conflicts of interest.
References
- 1.Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002;39:1890–900. doi: 10.1016/s0735-1097(02)01886-7. [DOI] [PubMed] [Google Scholar]
- 2.Cantinotti M, Assanta N, Murzi B, Lopez L. Controversies in the definition and management of insignificant left-to-right shunts. Heart. 2014;100:200–5. doi: 10.1136/heartjnl-2013-304372. [DOI] [PubMed] [Google Scholar]
- 3.Williams RG, Pearson GD, Barst RJ, Child JS, del Nido P, Gersony WM, et al. Report of the National Heart, Lung, and Blood Institute Working Group on research in adult congenital heart disease. J Am Coll Cardiol. 2006;47:701–7. doi: 10.1016/j.jacc.2005.08.074. [DOI] [PubMed] [Google Scholar]
- 4.Karamlou T, Diggs BS, McCrindle BW, Welke KF. A growing problem: maternal death and peripartum complications are higher in women with grown-up congenital heart disease. Ann Thorac Surg. 2011;92:2193–8. doi: 10.1016/j.athoracsur.2011.05.088. [DOI] [PubMed] [Google Scholar]
- 5.Drenthen W, Pieper PG, Roos-Hesselink JW, van Lottum WA, Voors AA, Mulder BJ, et al. Outcome of pregnancy in women with congenital heart disease: a literature review. J Am Coll Cardiol. 2007;49:2303–11. doi: 10.1016/j.jacc.2007.03.027. [DOI] [PubMed] [Google Scholar]
- 6.Uebing A, Steer PJ, Yentis SM, Gatzoulis MA. Pregnancy and congenital heart disease. BMJ. 2006;332:401–6. doi: 10.1136/bmj.332.7538.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brickner ME, Hillis LD, Lange RA. Congenital heart disease in adults. First of two parts. N Engl J Med. 2000;342:256–63. doi: 10.1056/NEJM200001273420407. [DOI] [PubMed] [Google Scholar]
- 8.Moghbeli N, Pare E, Webb G. Practical assessment of maternal cardiovascular risk in pregnancy. Congenit Heart Dis. 2008;3:308–16. doi: 10.1111/j.1747-0803.2008.00207.x. [DOI] [PubMed] [Google Scholar]
- 9.Khairy P, Ouyang DW, Fernandes SM, Lee-Parritz A, Economy KE, Landzberg MJ. Pregnancy outcomes in women with congenital heart disease. Circulation. 2006;113:517–24. doi: 10.1161/CIRCULATIONAHA.105.589655. [DOI] [PubMed] [Google Scholar]
- 10.Siu SC, Sermer M, Colman JM, Alvarez AN, Mercier LA, Morton BC, et al. Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001;104:515–21. doi: 10.1161/hc3001.093437. [DOI] [PubMed] [Google Scholar]
- 11.Jain VD, Moghbeli N, Webb G, Srinivas SK, Elovitz MA, Paré E. Pregnancy in women with congenital heart disease: the impact of a systemic right ventricle. Congenit Heart Dis. 2011;6:147–56. doi: 10.1111/j.1747-0803.2011.00497.x. [DOI] [PubMed] [Google Scholar]
- 12.Healthcare Cost Utilization Project HCUP. Overview of the Nationwide Inpatient Sample (NIS) Available at: http://www.hcup-us.ahrq.gov/nisoverview.jsp. Retrieved October 1, 2012.
- 13.Kuklina EV, Whiteman MK, Hillis SD, Jamieson DJ, Meikle SF, Posner SF, et al. An enhanced method for identifying obstetric deliveries: implications for estimating maternal morbidity. Matern Child Health J. 2008;12:469–77. doi: 10.1007/s10995-007-0256-6. [DOI] [PubMed] [Google Scholar]
- 14.Grotegut C, Kuklina E, Anstrom K, Heine R, Callaghan W, Myers E, et al. Factors associated with the change in prevalence of cardiomyopathy at delivery in the period 2000–2009: a population-based prevalence study. BJOG. 2014;121:1386–94. doi: 10.1111/1471-0528.12726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Podulka J, Stranges E, Steiner C. HCUP Statistical Brief #110. Rockville (MD): Agency for Healthcare Research and Quality; 2011. Hospitalizations related to childbirth, 2008. [PubMed] [Google Scholar]
- 16.Kuklina E, Callaghan W. Chronic heart disease and severe obstetric morbidity among hospitalisations for pregnancy in the USA: 1995–2006. BJOG. 2011;118:345–52. doi: 10.1111/j.1471-0528.2010.02743.x. [DOI] [PubMed] [Google Scholar]
- 17.James AH, Jamison MG, Biswas MS, Brancazio LR, Swamy GK, Myers ER. Acute myocardial infarction in pregnancy: a United States population-based study. Circulation. 2006;113:1564–71. doi: 10.1161/CIRCULATIONAHA.105.576751. [DOI] [PubMed] [Google Scholar]
- 18.James AH, Bushnell CD, Jamison MG, Myers ER. Incidence and risk factors for stroke in pregnancy and the puerperium. Obstet Gynecol. 2005;106:509–16. doi: 10.1097/01.AOG.0000172428.78411.b0. [DOI] [PubMed] [Google Scholar]
- 19.Grotegut CA, Chisholm CA, Johnson LN, Brown HL, Heine RP, James AH. Medical and obstetric complications among pregnant women aged 45 and older. PLoS One. 2014;9:e96237. doi: 10.1371/journal.pone.0096237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120:1029–36. doi: 10.1097/aog.0b013e31826d60c5. [DOI] [PubMed] [Google Scholar]
- 21.Weiss BM, Zemp L, Seifert B, Hess OM. Outcome of pulmonary vascular disease in pregnancy: a systematic overview from 1978 through 1996. J Am Coll Cardiol. 1998;31:1650–7. doi: 10.1016/s0735-1097(98)00162-4. [DOI] [PubMed] [Google Scholar]
- 22.University of Ottawa. Society, the individual, and medicine. Attributable risk and population attributable risk (PAP) measures. Available at: http://www.med.uottawa.ca/sim/data/PAR_e.htm. Retrieved March 7, 2014.
- 23.Opotowsky AR, Siddiqi OK, D’Souza B, Webb GD, Fernandes SM, Landzberg MJ. Maternal cardiovascular events during childbirth among women with congenital heart disease. Heart. 2012;98:145–51. doi: 10.1136/heartjnl-2011-300828. [DOI] [PubMed] [Google Scholar]
- 24.Roos-Hesselink JW, Ruys TP, Stein JI, Thilén U, Webb GD, Niwa K, et al. Outcome of pregnancy in patients with structural or ischaemic heart disease: results of a registry of the European Society of Cardiology. Eur Heart J. 2013;34:657–65. doi: 10.1093/eurheartj/ehs270. [DOI] [PubMed] [Google Scholar]
- 25.Vigl M, Kaemmerer M, Seifert-Klauss V, Niggemeyer E, Nagdyman N, Trigas V, et al. Contraception in women with congenital heart disease. Am J Cardiol. 2010;106:1317–21. doi: 10.1016/j.amjcard.2010.06.060. [DOI] [PubMed] [Google Scholar]
- 26.Hoyert DL. Maternal mortality and related concepts. National Center for Health Statistics Vital Health Stat. 2007;3:1–13. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.