Abstract
Background
Sickle cell disease (SCD) patients hospitalized with vaso-occlusive pain crisis tend to have prolonged length of stay (LOS) and high 30-day readmission rates. We investigated the associations of demographic characteristics, comorbidities and blood transfusion during hospitalization with these outcomes.
Study Design
Repeated regression analysis was used to analyze 39,324 admissions of 4,348 adults with sickle cell crisis from 2007–2012 in the Truven Health MarketScan® Medicaid Databases.
Results
The mean (95% range) LOS was 5.9 (1.0–19.0) days and the 30-day readmission rate was 39.6% (95% confidence interval [CI]: 39.1%–40.0%). Older age, chronic cardiopulmonary, renal or liver disease and sepsis were associated with both longer LOS and greater 30-day readmission rate. Female gender, iron overload, acute chest syndrome, acute renal failure and stroke were additional predictors of longer LOS. Simple red blood cell transfusion was administered in 31.3% of the admissions, and these patients tended to have more severe disease (chronic cardiopulmonary or kidney disease, acute chest syndrome, acute kidney or liver failure, sepsis). Nevertheless, transfusion was associated with a reduced estimated odds ratio of inpatient mortality of 0.75 (95% CI: 0.57–0.99) and a decreased odds ratio of 30-day readmission of 0.78 (95% CI: 0.73–0.83).
Conclusion
Our findings point to blood transfusion as a potential means to reduce the 30-day readmission rate among Medicaid patients hospitalized with sickle cell crisis. There is a need for a prospective study to examine the potential benefit and safety of simple blood transfusion for this purpose.
Keywords: 30-day readmission, length of stay, blood transfusion, sickle cell disease, sickle cell crisis
Introduction
Sickle cell disease (SCD) is the most common genetic blood disorder in the United States, affecting over 90,000 people,1 the majority of whom are African Americans. SCD patients suffer severe pain episodes, acute chest syndrome and other complications which require multiple hospital admissions.2 SCD patients have more than 190,000 emergency department (ED) visits and 110,000 hospital admissions each year, and there are subgroups of patients that use health care resources with higher frequency.3,4 One in four SCD patients does not experience a major acute pain episode in an average year while one in five has more than three acute episodes annually.5
Hospital length of stay (LOS) and 30-day readmission rate are regarded as indicators of quality of care, and hospitals with high values for these measures will face reduced reimbursement from Medicare and Medicaid in the future6. Studies covering the years of 1997 to 2007 indicated that adults with SCD have a mean LOS of six to nine days7,8 and one of the highest 30-day readmission rates.9 LOS in SCD patients increases with age and is higher in females, patients insured by Medicare or Medicaid and patients with more comorbidities.10–12 These studies also indicated that hospital readmission rates are higher in males13 and those who receive corticosteroids.2,14
The purpose of the present study was to analyze a large US hospitalization database for contemporary factors associated with LOS and 30-day hospital readmission, and to determine the relative contribution of demographic and comorbid factors to these outcomes. We also aimed to assess the effect of inpatient blood transfusion on LOS and readmission rate in these patients.
Material and Methods
Database
We used the Truven Health MarketScan® Medicaid Databases to study discharge records of 44,151 hospital admissions involving 6,400 adults (≥18 years old) with SCD from 2007–2012. Hospital admissions with SCD diagnosis were identified based on International Classification of Disease (ICD)-9 codes, and the presence of certain clinical comorbidities was also identified using these codes (Table 1). Vital status and up to 15 clinical diagnoses and five procedure codes were provided in each record.
Table 1.
International Classification of Disease (ICD) 9 (M and P) codes for each clinical event
| Event | ICD 9 Codes |
|---|---|
| Sickle Cell Disease | 282.60–282.69, 282.41–282.42 |
| Sickle cell crisis | 282.62, 282.64, 282.69, 282.42 |
| Stroke | 430, 431, 433.x1, 434.x1, 436 |
| Chronic cardiopulmonary disease | 428.0–428.9, 402.0–402.91, 414.0–414.9, 416.0, 416.8, 518.83, 515, 490, 496, 491.0–495.9 |
| Iron overload | 275.0 |
| Asthma | 493.0–493.9 |
| Sepsis | 038.0–038.9, 995.91–995.92,999.3, 771.81 |
| Blood transfusion | 99.03–99.04 |
| Exchange blood transfusion | 99.01 |
| Chronic liver disease | 070.0–070.9, 571.0, 571.2–571.9 573.0–573.3, 573.8–573.9, 453.0 |
| Acute liver failure | 571.1, 573.4, 570 |
| Acute chest syndrome | 480.0–488.9, 518–81, 518.82, 518.84, 415.1 |
| Chronic renal disease | 586, 585.0–585.9, 403, V45.1, V56, V42.0, 54.98, 39.95 |
| Acute renal failure | 584.0–584.9, 639.3, 638.3, 669.3, 580.0–580.9 |
| Hemolytic reaction to blood transfusion | 999.83–999.85 |
| Transfusion related acute lung injury (TRALI) | 518.7 |
These records did not include detailed medical information, such as pain severity or the percentage of hemoglobin S prior to a blood transfusion. The dates of consecutive admissions were used to identify hospital admissions within 30 days of discharge. Acute multi-organ failure was defined as the presence at least two out of three diagnoses of acute liver failure, acute renal disease or acute lung disease including acute chest syndrome. Outpatient pharmaceutical claims were used to identify prescription of opioids, hydroxyurea, steroids or non-steroidal anti-inflammatory drugs (NSAIDS), and the prescription data was merged with the discharge file using the National Drug Code. If the period for which the drug was prescribed included the date of hospital admission, we assumed that the patient was on the prescription at the time of admission.
Statistical analysis
Univariate analysis of the association between candidate predictors and LOS was performed using mixed effect linear regression analysis. Univariate analysis of the association between potential predictors and 30-day readmission rate was performed by mixed effect logistic regression in non-fatal admissions. Multivariate analysis of the predictors of LOS and 30-day readmission was performed with variables having prevalence of ≥1% and P<0.20 from univariate analysis. In the multivariate model for LOS, beta was calculated as the measure of effect of each predictor on mean LOS. In the multivariate model for 30-day readmission, the odds ratio was calculated as the measure of effect on the odds (risk) of 30-day readmission Variables with adjusted P-values <0.05 were retained in the final models. The associations of simple red blood cell transfusion and exchange blood transfusion with LOS and with 30-day readmission rate were assessed in univariate models overall and by subgroup analysis in patients with certain comorbidities. The associations of simple red blood cell transfusion and of exchange blood transfusion with inpatient mortality were assessed using a multivariate Generalized Estimating Equation with adjustment for the significant predictors of mortality. Statistical analyses were performed using the STATA 13.0 (StataCorp., College station, TX).
Results
Hospital admissions with sickle cell crisis
Of the 44,151 adult hospital admissions with SCD diagnosis during 2007–2012, the present report focuses on 39,294 admissions (89.0%) involving 4,348 distinct patients with a discharge diagnosis of sickle cell crisis. The median number of hospital admissions per year was 1.5 per patient (interquartile range [IQR] of 0.5–3.3), the median age was 28 years (IQR: 22–35), and 60.6% percent of admissions were for females. The most frequent prescriptions at the time of admission were opioids, hydroxyurea and NSAIDs (Table 2). The most frequent chronic comorbidities were cardiopulmonary disease (25.5%), asthma (14.1%), and renal disease (4.5%) and the most frequent acute comorbidities were acute chest syndrome/pneumonia (17.2%), sepsis (5.2%) and acute renal failure (3.7%) (Table 2).
Table 2.
Patient demographics and baseline characteristics and association with hospital length of stay (LOS) and 30-day readmission in 39,324 hospital admissions for sickle cell crisis among 4,348 adult patients.
| Number of admissions | Mean (95% range) LOS in days | Number of non-fatal admissions | Rate (95% CI) of 30- day readmission | |
|---|---|---|---|---|
| Overall | 39,324 | 5.9 (1.0–19.0) | 39,136 | 39.6% |
| Baseline characteristics | ||||
| Age | ||||
| ≤ median of 28 years | 21,086 | 5.6 (1.0–18.0) | 21,009 | 41.5% (40.8%–42.1%) |
| > median of 28 years | 18,238 | 6.1 (1.0–21.0) | 18,127 | 37.4% (36.7%–38.1%) |
| Male | 15,486 | 5.6 (1.0–18.0) | 15,389 | 38.9% (38.1%–40.0%) |
| Female | 23,838 | 6.0 (1.0–20.0) | 23,747 | 39.9% (39.4%–40.6%) |
| Opioid treatment1 | 28,465 | 5.8 (1.0–19.0) | 28,360 | 45.7% (45.1%–46.3%) |
| Hydroxyurea1 | 11,299 | 5.7 (1.0–18.0) | 11,262 | 48.8% (47.8%–50.0%) |
| NSAID treatment1 | 11,050 | 5.4 (1.0–17.0) | 11,011 | 42.3% (41.4%–43.2%) |
| Steroid treatment1 | 2,284 | 5.8 (1.0–19.0) | 2,276 | 48.0% (45.9%–50.0%) |
| Cardiopulmonary disease | 10,030 | 6.2 (1.0–20.0) | 9,972 | 42.9% (41.9%–43.9%) |
| Chronic Asthma | 5,534 | 5.4 (1.0–16.0) | 5,524 | 47.0% (45.7%–48.3%) |
| Chronic renal disease | 1,733 | 7.2 (1.0–29.7) | 1,691 | 35.3% (33.0%–37.6%) |
| Chronic liver disease | 1,155 | 7.4 (1.0–23.1) | 1,143 | 43.7% (40.9%–46.6%) |
| Iron overload | 1,073 | 7.0 (2.0–22.0) | 1,073 | 45.2% (42.2%–48.2%) |
| Acute comorbidities | ||||
| Acute chest syndrome or pneumonia | 6,767 | 7.8 (1.0–26.0) | 6,644 | 32.5% (31.4%–33.6%) |
| Sepsis | 2,044 | 11.0 (1.0–38.0) | 1,969 | 44.4% (42.2%–46.6%) |
| Acute renal failure | 1,447 | 9.0 (1.0–33.8) | 1,374 | 34.6% (32.1%–37.1%) |
| Acute multi-organ failure | 527 | 12.0 (1.0–44.6) | 464 | 30.8% (26.6%–35.0%) |
| Acute stroke | 335 | 9.2 (1.0–36.6) | 319 | 35.4% (30.1%–40.7%) |
| Acute liver failure | 104 | 11.9 (1.0–54.3) | 85 | 30.6% (20.6%–40.6%) |
| Hospital course | ||||
| LOS, days | ||||
| 1–3 | 14,329 | NA | 14,238 | 37.1% (36.3%–37.9%) |
| 4+ | 24,995 | 24,898 | 41.0% (40.4%–41.6%) |
From outpatient claims
Predictors of hospital length of stay
The mean (95% range) LOS was 5.9 (1.0–19.0) days in adults with sickle cell crisis and did not change significantly during the study period. Table 2 summarizes the association of baseline characteristics and acute morbidities with LOS in univariate analysis. The baseline characteristics of female gender, iron overload and chronic renal, liver or cardiopulmonary disease were independently associated with longer average LOS of between 0.5 and 1.0 days by multivariate analysis (Table 3). The acute complications of acute chest syndrome, sepsis, acute renal failure and stroke during the hospitalization were independently associated with longer average LOS of between 1.9 and 4.3 days (Table 3).
Table 3.
Independent predictors of hospital length of stay (LOS) in sickle cell crisis hospital admissions*.
| Frequency of occurrence | Mean change in LOS (95%CI) | P value | |
|---|---|---|---|
| Baseline characteristics | |||
| Age (10 year) | -- | 0.1 (0.02–0.2) | 0.048 |
| Female | 60.6% | 0.5 (0.2–0.7) | <0.001 |
| Chronic cardiopulmonary disease | 25.5% | 0.9 (0.7–1.1) | <0.001 |
| Chronic asthma | 14.1% | −0.9 (−1.1– −0.6) | <0.001 |
| Chronic renal disease | 4.5% | 0.6 (0.3–0.9) | <0.001 |
| Chronic liver disease | 2.9% | 1.0 (0.7–1.3) | <0.001 |
| Iron overload | 2.7% | 0.5 (0.2–0.8) | 0.001 |
| Acute comorbidities and events | |||
| Acute chest syndrome or pneumonia | 17.2% | 1.9 (1.8–2.0) | <0.001 |
| Sepsis | 5.2% | 4.3 (4.1–4.6) | <0.001 |
| Acute renal failure | 3.7% | 2.3 (2.0–2.6) | <0.001 |
| Stroke | 0.9% | 2.7 (2.2–3.3) | <0.001 |
Variables with P ≤0.2 from univariate analysis and frequency of ≥1% were entered into the multivariate analysis.
Predictors of 30-day readmission to hospital
The number (%) of inpatient mortality in all admissions with sickle cell crisis was 188 (0.48%). The rate of hospital readmission within 30 days of discharge was 39.6% (95% CI: 39.1%–40.0%) for nonfatal admissions Table 2 summarizes associations with 30-day readmission rate in univariate analysis. Opioid, hydroxyurea or steroid therapy before admission, chronic cardiopulmonary, renal or liver disease, sepsis and longer LOS had independent associations with greater risk of 30-day readmission in multivariate analysis (Table 4). A subgroup of 4,832 admissions, characterized by age <30 years, outpatient opioid therapy before admission and chronic underlying renal, cardiopulmonary or liver disease, had a 49.6% risk of 30-day readmission. In comparison, a subgroup of 3,629 admissions without these factors had a 19.4% risk of 30-day readmission.
Table 4.
Independent predictors of 30-day hospital readmission in patients with sickle cell crisis.
| Frequency of occurrence | Odds Ratio (95%CI) | P value | |
|---|---|---|---|
| Baseline characteristics | |||
| Age (each 10 years) | --- | 0.8 (0.8–0.9) | <0.001 |
| Opioid treatment before admission | 72.4% | 2.7 (2.5–3.0) | <0.001 |
| Hydroxyurea treatment before admission | 28.7% | 1.3 (1.2–1.4) | <0.001 |
| Steroid therapy before admission | 5.8% | 1.3 (1.1–1.4) | <0.001 |
| Chronic cardiopulmonary disease | 25.5% | 1.1 (1.02–1.2) | 0.014 |
| Chronic renal disease | 4.5% | 1.4 (1.1–1.6) | 0.002 |
| Chronic liver disease | 2.9% | 1.2 (1.01–1.5) | 0.048 |
| Acute comorbidities | |||
| Sepsis | 5.2% | 1.4 (1.3–1.6) | <0.001 |
| Hospital course | |||
| LOS | <0.001 | ||
| 1–3 days | 36.4% | 1.0 | |
| 4+ days hospital duration | 63.6% | 1.2 (1.2–1.3) |
Relationship of blood transfusion during hospitalization to hospital outcomes
Blood transfusion is a form of therapy that fundamentally alters the pathology of SCD by decreasing the proportion of hemoglobin S circulating in the blood, increasing the oxygen carrying capacity of the blood and decreasing the degree of hemolysis. The patients received a simple red blood cell transfusion in 31.3% of the admissions and an exchange blood transfusion in 1.9% of the admissions.
Simple red blood cell transfusion
Simple red blood cell transfusion was administered significantly more often in patients who were older, of female gender, and characterized by more chronic or acute comorbidities (Table 5). The mean (95% range) hospital LOS was 6.7 (1.0–21.0) days among patients who received a simple red blood cell transfusion compared to 5.4 (1.0–18.0) days among those who did not (P <0.001), likely representing the tendency of those receiving transfusion to have more severe illness. Subgroup analyses revealed that simple red blood cell transfusion was associated with a shorter LOS in patients with chronic renal disease (P = 0.027) (Table 6). Red blood cell transfusion was not associated with a reduction in mortality in unadjusted analysis (Table 5), but in an analysis that adjusted for age, chronic kidney disease, acute chest syndrome, acute renal or multi-organ failure, sepsis and stroke, blood transfusion was associated with a decrease in the relative risk of death: odds ratio (95% CI) of 0.75 (0.57–0.99) (P = 0.040).
Table 5.
Characteristics of hospital admissions according to simple red blood cell transfusion and exchange blood transfusion status.
| Without simple red blood cell or exchange blood transfusion N = 26,334 | With blood simple red blood cell transfusion N = 12,746 | With exchange blood transfusion N = 244 | P value for simple transfusion vs. nontransfused1 | P value for exchange transfusion vs. nontransfused1 | |
|---|---|---|---|---|---|
| Baseline | |||||
| Age, median (IQR) | 27 (22–34) | 29 (23–36) | 26 (22–31) | <0.001 | 0.004 |
| Female gender (%) | 59.4% | 63.3% | 51.2% | 0.007 | 0.027 |
| Opioid treatment (%)2 | 74.4% | 68.2% | 68.4% | 0.001 | 0.5 |
| NSAID treatment (%)2 | 30.0% | 24.1% | 29.9% | 0.08 | 0.9 |
| Hydroxyurea treatment (%)2 | 29.8% | 26.5% | 25.8% | 0.2 | 0.4 |
| Steroid treatment (%)2 | 6.0% | 5.4% | 11.5% | 0.5 | 0.006 |
| Chronic conditions | |||||
| Cardiopulmonary disease (%) | 25.9% | 24.7% | 32.0% | <0.001 | 0.030 |
| Chronic Asthma | 15.7% | 10.7% | 14.8% | 0.037 | 0.3 |
| Chronic renal disease (%) | 3.3% | 6.7% | 4.9% | <0.001 | 0.3 |
| Chronic liver disease (%) | 2.8% | 3.2% | 4.1% | 0.3 | 0.1 |
| Acute comorbidities | |||||
| Acute chest syndrome or pneumonia | 14.6% | 21.7% | 58.2% | <0.001 | <0.001 |
| Acute renal failure | 2.7% | 5.4% | 12.7% | <0.001 | <0.001 |
| Sepsis | 4.4% | 6.7% | 11.5% | <0.001 | <0.001 |
| Acute multi-organ failure | 1.0% | 1.9% | 12.7% | <0.001 | <0.001 |
| Stroke | 0.8% | 0.9% | 9.0% | 0.6 | <0.001 |
| Acute liver failure | 0.2% | 0.4% | 2.5% | <0.001 | <0.001 |
| Hospital course | |||||
| LOS, mean (95%CI) day | 5.4 (5.3–5.5) | 6.7 (6.6–6.8) | 9.2 (8.1–10.3) | <0.001 | <0.001 |
| Mortality | 0.5% | 0.5% | 2.5% | 0.8 | <0.001 |
Unadjusted
From outpatient records
Table 6.
Hospital length of stay (LOS) and 30-day readmission rate by red blood cell transfusion status in subpopulations of sickle cell crisis admissions.
| Subpopulation | Hospital LOS | 30-Day Readmissions | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Without simple red or exchange blood transfusion* | With simple red blood transfusion* | P value | Without simple red or exchange blood transfusion* | With simple red blood transfusion* | P value | |||||
| N | Days (95%CI) | N | Days (95%CI) | N | Rate | N | Rate | |||
| Overall | 26334 | 5.4 (5.3–5.5) | 12746 | 6.7 (6.6–6.8) | <0.001 | 26215 | 42.6% | 12683 | 33.3% | <0.001 |
| Baseline characteristics | ||||||||||
| Cardiopulmonary | 6808 | 5.8 (6.5–5.9) | 3143 | 7.1 (6.9–7.3) | <0.001 | 6768 | 47.0% | 3126 | 33.9% | <0.001 |
| disease | ||||||||||
| Asthma | 4136 | 5.0 (4.9–5.2) | 1362 | 6.5 (6.2–6.7) | <0.001 | 4127 | 50.2% | 1361 | 37.3% | <0.001 |
| Chronic renal disease | 872 | 7.7 (7.0–8.4) | 849 | 6.7 (8.3–7.2) | 0.028 | 847 | 39.0% | 833 | 32.1% | 0.004 |
| Chronic liver disease | 742 | 6.8 (6.4–7.3) | 403 | 8.2 (7.4–9.0) | 0.001 | 733 | 46.0% | 401 | 40.2% | 0.4 |
| Iron overload disorders | 532 | 6.6 (6.2–7.0) | 532 | 7.4 (6.9–7.9) | 0.013 | 532 | 50.4% | 532 | 40.2% | 0.015 |
| Acute comorbidities | ||||||||||
| Acute chest syndrome or pneumonia | 3862 | 7.4 (7.2–7.7) | 2763 | 8.2 (7.9–8.4) | <0.001 | 3788 | 35.5% | 2719 | 28.1% | <0.001 |
| Sepsis | 1164 | 11.0 (10.3–11.6) | 852 | 11.0 (10.4–11.7) | 0.8 | 1116 | 47.8% | 828 | 40.2% | 0.005 |
| Acute renal failure | 722 | 8.9 (8.2–9.6) | 694 | 8.9 (8.2–9.6) | 0.9 | 684 | 37.6% | 660 | 31.8% | 0.003 |
| Acute multi-organ failure | 252 | 12.3 (10.7–13.9) | 244 | 11.6 (10.2–13.0) | 0.5 | 218 | 32.6% | 215 | 30.2% | 0.3 |
| Acute Stroke | 201 | 8.2 (7.0–9.5) | 112 | 10.4 (8.7–12.0) | 0.040 | 192 | 38.0% | 105 | 30.5% | 0.3 |
| Acute liver failure | 50 | 11.4 (8.2–14.6) | 48 | 11.6 (7.0–16.1) | 0.9 | 43 | 30.2% | 36 | 33.3% | 0.7 |
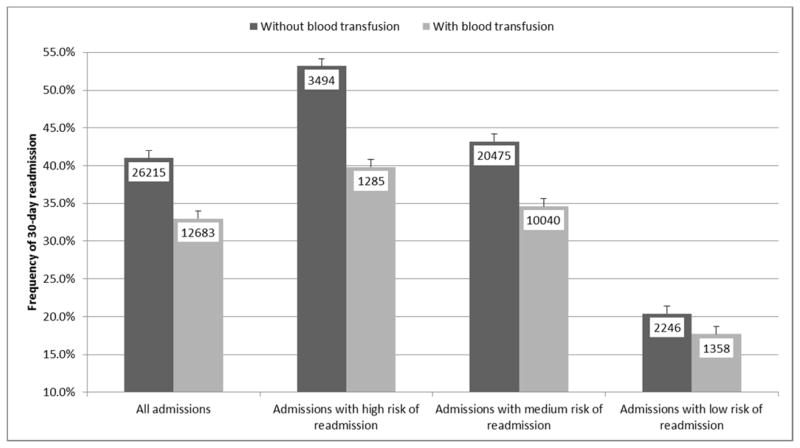
Among all 39,136 admissions in which the patient survived, simple red blood cell transfusion was associated with a decreased relative risk of 30-day readmission: odds ratio (95% CI) of 0.78 (0.73–0.83). This translates to a reduction in the 30-day readmission rate from 42.6% (95% CI of 42.0% to 43.2%) to 33.3% (95% CI of 32.5% to 34.1%) (Figure 1). Restricting the analysis to the subgroup of 4,832 admissions with age <30 years, opioid therapy at admission and chronic cardiopulmonary, renal or liver disease), simple red cell transfusion was associated with an odds ratio for 30-day readmission of 0.74 (95% CI: 0.62–0.89), or a rate reduction from 53.2% (95% CI of 51.5% to 54.8%) to 39.8% (95% CI of 37.1% to 42.4%) (Figure 1). Restricting the analysis to the subgroup of 3,629 admissions with age ≥30 years, not receiving opioid treatment at admission and absence of chronic cardiopulmonary, renal or liver disease, the reduction in risk of readmission was not statistically significant: odds ratio of 0.92 (95% CI: 0.72–1.21) or a rate reduction from 20.4 (95% CI:18.8%–22.1%) to 17.7 (95% CI:15.6%–19.7%). Blood transfusion complications of hemolytic transfusion reaction or transfusion related acute lung injury were reported in 0.1% of admissions in which transfusion was administered.
Figure 1.
Relationship of simple red blood cell transfusion with 30-day readmission rate in all sickle cell crisis admissions (P <0.001), and in subgroups with high risk of readmission (age <30 years, opioid therapy on admission and chronic cardiopulmonary, kidney or liver disease, P <0.001), with intermediate risk of readmission (P<0.001), and with low risk of readmission (age 30+ years, no opioid therapy on admission, no chronic cardiopulmonary, kidney or liver disease; P = 0.6). Bars show standard error. Number in box represents number of admissions in each category. Admissions with exchange blood transfusion were excluded from the analysis.
Exchange red blood cell transfusion
Patients with severe acute complications were markedly over represented in the patients who received exchange blood transfusion, in particular acute chest syndrome, acute renal failure, acute multi-organ failure and stroke (Table 5). From this perspective, it is not surprising that exchange transfusion was associated with a 4.1-day longer LOS on average. Exchange blood transfusion was also associated with an increased risk of death in unadjusted analysis (Table 5) but not after adjustment for significant predictors of mortality (estimated odds ratio 0.97, 95% CI of 0.36–2.44, P = 0.95). Exchange blood transfusion was not associated with a statistically significant change in the 30-day readmission rate (odds ratio 1.36, 95% CI of 0.96–1.91).
Discussion
This study has certain limitations. We studied Medicaid beneficiaries who have an increased LOS compared to private insurance and noninsured payers.10 Such patients also have a higher hospital admission rate and better self-reported health status compared to non-insured individuals.15 We analyzed administrative data recorded by ICD classification, which may be influenced by the accuracy of clinical diagnoses and coding procedures. The databases did not include detailed medical information, such as sickle genotype, pain severity score, percentage of hemoglobin S prior to a blood transfusion or use of inpatient medications, nor did they include community factors such as socioeconomic status, access to medical care or type and size of hospital. Despite these limitations, the large size of the data set and the uniform character of the data offered valuable insights into hospital LOS and 30-day readmission rate, important contemporary measures of quality of care.16
Blood transfusion is recommended for certain severe SCD complications including acute chest syndrome, splenic or hepatic sequestration, symptomatic anemia and multi-organ failure,17 and randomized clinical trials have indicated that blood transfusion is protective against stroke18 and perioperative complications.19 Simple red blood cell transfusion was associated with reduced inpatient mortality in the present study, a finding that is in keeping with these prior recommendations and observations. Furthermore, simple red blood cell transfusion was associated with only a modest one-day increase in the average LOS, considerably shorter than the increase in LOS when simple blood transfusion is administered for other admissions such as cardiac surgery and general pediatrics.20,21 That red blood cell transfusion in SCD is commonly given to treat the primary disease, i.e. to decrease the proportion of hemoglobin S and thereby anemia due to hemolysis, rather than to ameliorate complications of bleeding or acute severe anemia may help explain the different relationship of blood transfusion to LOS in SCD. It is of interest that transfusion was associated with a decreased LOS in the subset of SCD patients with chronic kidney disease.
There are important risks associated with blood transfusion, including alloimmunization,22 delayed hemolytic transfusion reaction,23 transfusion related acute lung injury (TRALI),24 transmission of viral and other infections,25 and stroke related to increased viscosity, especially if the hemoglobin concentration is raised above 10 g/dL.26 Therefore, blood transfusion must be administered cautiously, with attention to any alloantibodies that have been documented in the past, and one should consider extended blood typing.27 Encouragingly, rates of hemolytic transfusion reaction and TRALI were low in the sickle cell crisis patients who received blood transfusion in the present study.
One of the most interesting findings of our study is that simple red blood cell transfusion during hospitalization was associated with a more than 20% decrease in the rate of 30-day readmission for patients admitted with sickle cell crisis, which is striking given the greater severity of illness on average in patients receiving transfusion. Blood transfusion was associated with lower readmission rate in a previous report in children with SCD,2 adding strength to our present observation. Thus, our findings point to the possibility that blood transfusion during a hospitalization for sickle cell crisis leads to a decreased need for 30-day readmission and possibly to a decreased LOS after considering the severity of the illness. We believe our findings support the need for a prospective investigation in this regard.
Our study does not indicate a significant trend for a reduction in LOS from 2007 to 2012, in contrast to a reported reduction in LOS from 2003 to 2005 in the Nationwide Inpatient Sample database.10 Our observations that female gender and a number of chronic and acute morbidities are independently associated with LOS in patients admitted for sickle cell crisis tend to confirm and extend the findings of other investigators.8,10,28 The relationship between longer LOS and higher risk of 30-day readmission likely reflects that LOS serves as a retrospective marker of disease severity.
Our observation of higher rates of 30-day readmission in young and middle aged adults is consistent with another large study of SCD patients,5 and the relationship with cardiopulmonary disease mirrors a high rate of readmission with this complication in non-SCD patients.29 We do not believe our data point to long-term treatment with opioids or hydroxyurea as a cause of frequent readmission, but rather as a marker of more severe underlying disease. Opioids were prescribed in >95% of patients in whom hydroxyurea was prescribed before admission, underscoring that residual confounders may complicate the relationship of hydroxyurea therapy to readmission. In general, our findings point to multiple factors contributing to a high 30-day readmission rate, in keeping with a previous report.13 A prior study has shown that optimal post-discharge follow-up could reduce the readmission rate in SCD patients,30 and our findings suggest that it is possible to identify a subgroup of SCD patients who require especially close monitoring post-discharge for this purpose.
Conclusion
In the present study of adult Medicaid SCD patients having at least one hospital admission for sickle cell crisis from 2007 to 2012, the mean LOS of 5.9 days and 30-day readmission rate of 39.6% underscore the need for improved health care delivery in this population. Encouragingly, simple red blood cell transfusion was associated with a lower 30-day readmission rate of 42.6% vs 33.3% among all patients. We believe that our findings point to the need for a prospective, multi-center clinical study of simple blood transfusion to decrease 30-day readmission rate in patients hospitalized with sickle cell crisis.
Acknowledgments
Funding source: Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number P50HL118006.
Footnotes
Conflict of Interest: The authors have no conflict of interest to disclose.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Hassell KL. Population estimates of sickle cell disease in the U. S Am J Prev Med. 2010;38:S512–21. doi: 10.1016/j.amepre.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 2.Sobota A, Graham DA, Neufeld EJ, Heeney MM. Thirty-day readmission rates following hospitalization for pediatric sickle cell crisis at freestanding children’s hospitals: risk factors and hospital variation. Pediatr Blood Cancer. 2012;58:61–5. doi: 10.1002/pbc.23221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brousseau DC, Panepinto JA, Nimmer M, Hoffmann RG. The number of people with sickle-cell disease in the United States: national and state estimates. Am J Hematol. 2010;85:77–8. doi: 10.1002/ajh.21570. [DOI] [PubMed] [Google Scholar]
- 4.Yusuf HR, Atrash HK, Grosse SD, Parker CS, Grant AM. Emergency department visits made by patients with sickle cell disease: a descriptive study, 1999–2007. Am J Prev Med. 2010;38:S536–41. doi: 10.1016/j.amepre.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. Acute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010;303:1288–94. doi: 10.1001/jama.2010.378. [DOI] [PubMed] [Google Scholar]
- 6.Axon RN, Williams MV. Hospital readmission as an accountability measure. JAMA. 2011;305:504–5. doi: 10.1001/jama.2011.72. [DOI] [PubMed] [Google Scholar]
- 7.Strouse JJ, Jordan LC, Lanzkron S, Casella JF. The excess burden of stroke in hospitalized adults with sickle cell disease. Am J Hematol. 2009;84:548–52. doi: 10.1002/ajh.21476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vichinsky EP, Styles LA, Colangelo LH, Wright EC, Castro O, Nickerson B. Acute chest syndrome in sickle cell disease: clinical presentation and course. Cooperative Study of Sickle Cell Disease. Blood. 1997;89:1787–92. [PubMed] [Google Scholar]
- 9.Elixhauser A, Steiner C. Readmissions to US Hospitals by Diagnosis, 2010 HCUP Statistical Brief #153. Rockville, MD: Agency for Healthcare Research and Quality; 2013. [PubMed] [Google Scholar]
- 10.McCavit TL, Lin H, Zhang S, Ahn C, Quinn CT, Flores G. Hospital volume, hospital teaching status, patient socioeconomic status, and outcomes in patients hospitalized with sickle cell disease. Am J Hematol. 2011;86:377–80. doi: 10.1002/ajh.21977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panepinto JA, Brousseau DC, Hillery CA, Scott JP. Variation in hospitalizations and hospital length of stay in children with vaso-occlusive crises in sickle cell disease. Pediatr Blood Cancer. 2005;44:182–6. doi: 10.1002/pbc.20180. [DOI] [PubMed] [Google Scholar]
- 12.Mayer ML, Konrad TR, Dvorak CC. Hospital resource utilization among patients with sickle cell disease. J Health Care Poor Underserved. 2003;14:122–35. [PubMed] [Google Scholar]
- 13.Ballas SK, Lusardi M. Hospital readmission for adult acute sickle cell painful episodes: frequency, etiology, and prognostic significance. Am J Hematol. 2005;79:17–25. doi: 10.1002/ajh.20336. [DOI] [PubMed] [Google Scholar]
- 14.Sobota A, Graham DA, Heeney MM, Neufeld EJ. Corticosteroids for acute chest syndrome in children with sickle cell disease: variation in use and association with length of stay and readmission. Am J Hematol. 2010;85:24–8. doi: 10.1002/ajh.21565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baicker K, Finkelstein A. The effects of Medicaid coverage--learning from the Oregon experiment. N Engl J Med. 2011;365:683–5. doi: 10.1056/NEJMp1108222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schwalenstocker E, Gay J, Muldoon J, Sedman A. Appropriate use of quality measures: Response to “Risk factors for hospital readmission within 30 days: A new quality measure for children with sickle cell disease”. Pediatr Blood Cancer. 2009;53:1361. doi: 10.1002/pbc.22212. author reply 2–4. [DOI] [PubMed] [Google Scholar]
- 17.Yawn BP, Buchanan GR, Afenyi-Annan AN, Ballas SK, Hassell KL, James AH, Jordan L, Lanzkron SM, Lottenberg R, Savage WJ, Tanabe PJ, Ware RE, Murad MH, Goldsmith JC, Ortiz E, Fulwood R, Horton A, John-Sowah J. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA. 2014;312:1033–48. doi: 10.1001/jama.2014.10517. [DOI] [PubMed] [Google Scholar]
- 18.Wang WC, Dwan K. Blood transfusion for preventing primary and secondary stroke in people with sickle cell disease. Cochrane Database Syst Rev. 2013;11:CD003146. doi: 10.1002/14651858.CD003146.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howard J, Malfroy M, Llewelyn C, Choo L, Hodge R, Johnson T, Purohit S, Rees DC, Tillyer L, Walker I, Fijnvandraat K, Kirby-Allen M, Spackman E, Davies SC, Williamson LM. The Transfusion Alternatives Preoperatively in Sickle Cell Disease (TAPS) study: a randomised, controlled, multicentre clinical trial. Lancet. 2013;381:930–8. doi: 10.1016/S0140-6736(12)61726-7. [DOI] [PubMed] [Google Scholar]
- 20.Galas FR, Almeida JP, Fukushima JT, Osawa EA, Nakamura RE, Silva CM, de Almeida EP, Auler JO, Vincent JL, Hajjar LA. Blood transfusion in cardiac surgery is a risk factor for increased hospital length of stay in adult patients. J Cardiothorac Surg. 2013;8:54. doi: 10.1186/1749-8090-8-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slonim AD, Joseph JG, Turenne WM, Sharangpani A, Luban NL. Blood transfusions in children: a multi-institutional analysis of practices and complications. Transfusion. 2008;48:73–80. doi: 10.1111/j.1537-2995.2007.01484.x. [DOI] [PubMed] [Google Scholar]
- 22.Chou ST, Liem RI, Thompson AA. Challenges of alloimmunization in patients with haemoglobinopathies. Br J Haematol. 2012;159:394–404. doi: 10.1111/bjh.12061. [DOI] [PubMed] [Google Scholar]
- 23.Scheunemann LP, Ataga KI. Delayed hemolytic transfusion reaction in sickle cell disease. Am J Med Sci. 2010;339:266–9. doi: 10.1097/MAJ.0b013e3181c70e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kenz HE, Van der Linden P. Transfusion-related acute lung injury. Eur J Anaesthesiol. 2014;31:345–50. doi: 10.1097/EJA.0000000000000015. [DOI] [PubMed] [Google Scholar]
- 25.Bolton-Maggs PH, Cohen H. Serious Hazards of Transfusion (SHOT) haemovigilance and progress is improving transfusion safety. Br J Haematol. 2013;163:303–14. doi: 10.1111/bjh.12547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vichinsky EP. Current issues with blood transfusions in sickle cell disease. Semin Hematol. 2001;38:14–22. doi: 10.1016/s0037-1963(01)90056-3. [DOI] [PubMed] [Google Scholar]
- 27.Casas J, Friedman DF, Jackson T, Vege S, Westhoff CM, Chou ST. Changing practice: red blood cell typing by molecular methods for patients with sickle cell disease. Transfusion. 2015 doi: 10.1111/trf.12987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allareddy V, Roy A, Lee MK, Nalliah RP, Rampa S, Allareddy V, Rotta AT. Outcomes of acute chest syndrome in adult patients with sickle cell disease: predictors of mortality. PLoS One. 2014;9:e94387. doi: 10.1371/journal.pone.0094387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Joynt KE, Jha AK. Thirty-day readmissions--truth and consequences. N Engl J Med. 2012;366:1366–9. doi: 10.1056/NEJMp1201598. [DOI] [PubMed] [Google Scholar]
- 30.Frei-Jones MJ, Field JJ, DeBaun MR. Risk factors for hospital readmission within 30 days: a new quality measure for children with sickle cell disease. Pediatr Blood Cancer. 2009;52:481–5. doi: 10.1002/pbc.21854. [DOI] [PMC free article] [PubMed] [Google Scholar]