1. Background
Over the last 20 years, the number of older adults requiring surgical interventions has substantially increased and will continue to escalate as the population ages. Perioperative management of older patients poses challenges not encountered in younger individuals. People over 70 years of age are more likely to have multiple comorbidities, physical and cognitive impairments, and reduced cardiac, pulmonary, and renal reserve. These factors predispose older patients to increased risk for perioperative complications and prolonged length of hospital stay, which in turn increase risk for iatrogenesis, nosocomial infections, and perioperative mortality.
Current recommendations for perioperative assessment and management for older patients are derived from data collected in predominantly younger cohorts. Given the paucity of evidence-based guidelines for this patient population, it is vital to understand the pathophysiologic changes that occur in the older patient in order to reduce their perioperative risk.
The objectives of this review are to briefly summarize age-related effects on organ system reserve, identify comorbidities and geriatric conditions that pose increased risk for perioperative complications, and increase awareness of the essentials of perioperative evaluation and therapy in the older surgical patient. The overall goals are to ensure appropriate perioperative assessment and medical management and to minimize the risk of complications in older patients undergoing surgical procedures.
2. Implications of aging on perioperative care in older adults
Advancing age is associated with a reduction in physiologic reserve of all organ systems, even in the absence of any underlying pathology, and these changes predispose to the development of perioperative adverse events. In addition, older patients often have multiple comorbidities requiring complex medical regimens that may further complicate perioperative management. In this context, age-related changes in gastrointestinal physiology, kidney function, body composition (such as reduction in muscle mass and intravascular volume) and metabolism lead to alterations in the pharmacodynamics and pharmacokinetics of most drugs. As a result, older patients are often more sensitive to anesthetic and analgesic agents administered during the perioperative period.
Other age-related physiologic alterations increase the likelihood of postoperative cardiac (e.g., atrial fibrillation, heart failure) and non-cardiac (e.g., delirium, pneumonia) complications. For these reasons, older patients undergoing major surgery require a comprehensive preoperative evaluation that should include assessment of functional status, cognition, and frailty. Combining these factors with conventional perioperative risk assessments facilitates the identification of older patients at risk for specific postoperative complications, and may enable implementation of management strategies designed to reduce perioperative risk and minimize delays in recovery.
3. Preoperative cardiac risk assessment in older adults
Preoperative cardiac risk assessment in the older surgical patient should focus on the following elements: the nature and urgency of the surgical procedure, the patient's functional capacity, and the individual's cardiac risk profile. The risk of perioperative cardiac adverse events increases with the urgency, extent, location, and duration of the procedure, as well as anticipated blood loss and potential fluid and electrolyte shifts. Based on these factors, the ACCF/AHA Guidelines on perioperative cardiovascular evaluation stratify perioperative cardiac risk as low [i.e., overall predicted risk of major adverse cardiac event (MACE) or myocardial infarction (MI) < 1% (e.g., cataract surgery)] or high [overall predicted risk of MACE or MI > 1% (e.g., major abdominal surgery)].[1] Previous risk-stratification schemes included low, intermediate, and high-risk classifications, but recently published guidelines simplified this into two categories due to similarities between intermediate and high-risk procedures.
Establishing the patient's baseline functional capacity is the second key step in assessing perioperative risk. Poor functional capacity [< 4 METS (functional capacity measured in metabolic equivalents)] is associated with higher risk of cardiac complications, as it implies substantially decreased cardiovascular reserve and less capacity to tolerate surgical stress. Conversely, optimal functional capacity (> 10 METS) carries lower risk for cardiac complications. In general, if the patient is able to perform > 4 METS (e.g., climbing a flight of stairs, walking on level ground at 4 mph, performing heavy work around the house), then he or she is considered to have moderate or greater functional capacity and no further testing is indicated. If the patient's baseline functional capacity is unknown and cannot be easily determined, it should be presumed to be low when evaluating perioperative risk.
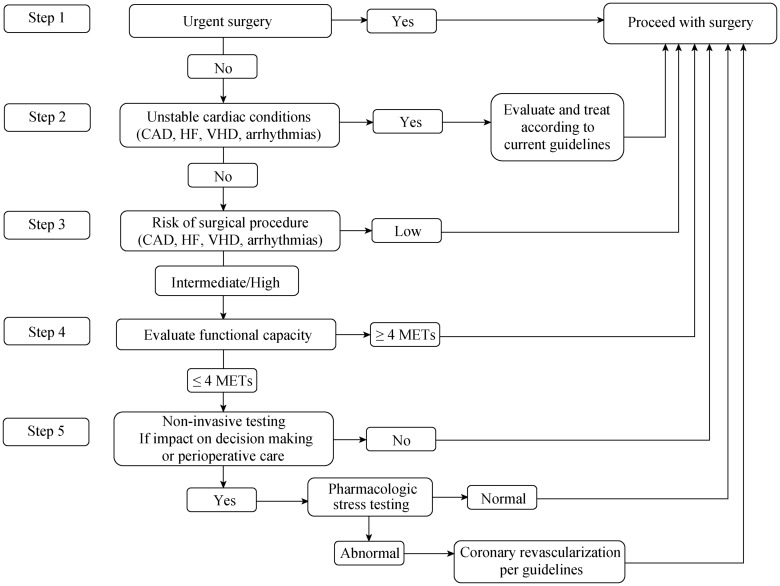
The third element of perioperative risk assessment involves evaluating the patient's cardiac risk profile. Acquisition of this information is based mainly on the clinical history and patient's status (e.g., presence of symptoms, physical findings, pertinent laboratory data). Patients with unstable or markedly symptomatic cardiovascular conditions (e.g., unstable coronary syndromes, decompensated heart failure, significant uncontrolled arrhythmias, or severe symptomatic valvular heart disease) are at high risk for perioperative complications and may benefit from additional evaluation and treatment prior to non-cardiac surgery. Importantly, preoperative cardiac testing should be performed only if it is anticipated that it will significantly change perioperative management, as well as in high-risk surgical patients with three or more clinical risk factors such as coronary artery disease, heart failure, cardiomyopathy, valvular heart disease, arrhythmias and conduction disorders, pulmonary vascular disease or adult congenital heart disease (Figure 1).[1]
Figure 1. Stepwise approach for perioperative cardiac risk assessment for noncardiac surgery.
CAD: coronary artery disease; HF: heart failure; VHD: valvular heart disease; MET: metabolic equivalent.
4. Perioperative cardiac and non-cardiac complications
As noted above, older patients are at increased risk for developing cardiac and non-cardiac complications following major surgery.[2] Common adverse cardiac events include myocardial ischemia, arrhythmias, and heart failure. In addition to advancing age, presence of multiple cardiac risk factors, unstable coronary artery disease, symptomatic heart failure, uncontrolled arrhythmias, severe valvular heart disease, and high-risk surgical procedures (e.g., intra-thoracic or vascular surgery) are associated with increased risk for perioperative cardiac complications. Common non-cardiac complications include delirium, cognitive impairment, hospital-acquired infections, respiratory insufficiency, venous thromboembolic disease, acute kidney injury, and pressure ulcers (especially in patients with prolonged hospitalization).
4.1. Management of postoperative cardiac complications
History of heart failure is among the predictors of perioperative cardiovascular risk, but it is an intermediate risk factor unless it is an acute, active problem, in which case it confers significant risk for mortality, especially in older patients. It is thus important to perform a careful clinical assessment to determine if there are symptoms or signs of decompensated heart failure. Laboratory parameters should be interpreted with caution, as there may be some physiologic variation with age. B-type natriuretic peptide tends to increase with age, especially in women, and in patients with renal disease.
Patients with decompensated heart failure should be treated in accordance with existing guidelines, and elective surgery should be delayed if feasible. Patients with stable compensated heart failure should be monitored closely to avoid volume overload, but in most cases there is no need to delay elective non-cardiac or cardiac surgery.[3]
Postoperative atrial fibrillation (AF) is associated with significant morbidity (increased hospital length of stay, risk for stroke) and mortality.[4] Increasing age is the strongest and most consistent risk factor for perioperative supraventricular arrhythmias.[5] Additional risk factors for the development of post-operative AF are listed in Table 1. For patients with hemodynamically unstable supraventricular arrhythmias, immediate direct current cardioversion (DCCV) is indicated. In stable patients, management includes correction of precipitating factors, control of heart rate, and anticoagulation (unless contraindicated) to reduce the risk of thrombus formation. AV-nodal blocking agents, such as beta-blockers or non-dihydropyridine calcium channel blockers (diltiazem, verapamil) are the drugs of first choice to lower the ventricular rate. Digoxin has limited efficacy in high adrenergic states but may be used in patients with heart failure or as a second line agent in patients who fail to respond (or do not tolerate) other AV-nodal blockers. Amiodarone has a slow onset of action, wide range of side effects and numerous drug interactions. However, it may be useful for controlling heart rate or restoring sinus rhythm when other measures are unsuccessful or contraindicated. Since most postoperative atrial arrhythmias revert to sinus rhythm once the heightened perioperative adrenergic state has resolved, achieving rhythm control (i.e., by DCCV or antiarrhythmic drugs) is not generally recommended in the absence of moderate or severe symptoms despite heart rate lowering medications. Cardioversion may also be considered, preferably under transesophageal echocardiographic guidance to exclude left atrial appendage thrombus, for those who remain in AF or atrial flutter for more than 24–48h.
Table 1. Risk factors for the development of postoperative atrial fibrillation.
| Aging |
| Male gender |
| Prior atrial fibrillation |
| Hypertension |
| Left ventricular hypertrophy |
| Obesity |
| Hyperthyroidism |
| Sympathomimetic drugs |
| Atrial pathology or injury |
| High preoperative heart rate (higher adrenergic/lower vagal tone)* |
| Reversible precipitating factors |
| Hypothermia |
| Hypoxemia |
| Hypercarbia |
| Acidosis |
| Hypotension |
| Electrolyte imbalances |
| Increased or decreased intravascular volume |
| Cardiac ischemia |
| Inadequate pain control |
| Increased sympathetic nervous system activity |
| Pulmonary disease (pneumonia, pulmonary embolism) |
*Independently associated with postoperative atrial fibrillation in older patients undergoing thoracic surgery.
Myocardial ischemia, often manifested as asymptomatic ECG changes and/or small elevations of cardiac biomarker proteins, e.g., troponin, should be managed following ACC/AHA guidelines as established in younger patients. In most cases, minimal elevations of cardiac biomarker proteins following surgery are attributable to demand ischemia (i.e., type II MI), rather than an acute coronary syndrome (type I MI). In some cases, this distinction may be difficult, but it is nonetheless important because type I MI generally warrants aggressive treatment while type II MI can usually be managed conservatively.
Although hypertension is the single most common cardiac condition in older adults, elevated blood pressure (BP) has not been shown to be a major perioperative cardiac risk predictor. While severe stage 2 hypertension (systolic BP > 180 mmHg, diastolic BP > 110 mmHg) may increase the risk for perioperative cardiovascular complications, stage 1 hypertension (systolic BP 140–159 mmHg, diastolic BP 90–99 mmHg) and even moderate stage 2 hypertension (systolic BP 160–179 mmHg, diastolic BP 100–109 mmHg) are not associated with increased perioperative risk. Achieving adequate BP control preceding an elective surgical procedure is desirable to ensure hemodynamic stability throughout the perioperative period, since labile heart rate, blood pressure, and volume status are associated with adverse cardiovascular events.[6] However, it should be noted that overly aggressive BP control may lead to intraoperative hypotension, which in turn may be associated with myocardial ischemia, acute kidney injury, and/or post-operative cognitive impairment. In severely hypertensive patients, some experts would consider delaying elective non-cardiac surgery, as there is potential for an exaggerated sympathetic hypertensive response during induction of anesthesia. These patients are also at risk for developing end-organ damage such as hypertensive encephalopathy, cerebrovascular accident (ischemic stroke or intracranial hemorrhage), acute pulmonary edema, heart failure, aortic dissection, acute MI or unstable angina, or worsening renal insufficiency. In general, unless there is clinical evidence for acute end-organ injury, no therapeutic changes are indicated in the perioperative setting.
4.2. Management of non-cardiac postoperative complications
Delirium is a common and often unrecognized postoperative complication, occurring in up to 50% of older patients undergoing major surgery. Among those requiring intensive care, the incidence has been reported to be as high as 87%.[7] Development of postoperative delirium may be associated with persistent cognitive deficits, functional decline, increased hospital stay and costs, and increased mortality. Age ≥ 70 years is an independent risk factor for postoperative delirium; other risk factors include pre-existing neuropsychological disorder, polypharmacy, renal failure, and excess alcohol intake. Precipitating factors include dehydration, sleep deprivation, infections, hypoxemia, malnutrition, use of physical restraints, and being in an unfamiliar environment. The key to delirium prevention is to identify patients at high risk.[8] Preventative strategies should focus on avoiding sensory deprivation, preserving normal social interactions and routine diurnal variations in activities, and maintaining physiological homeostasis. Specific interventions include using hearing aids/eyeglasses when appropriate, frequent orientation, presence of family, early mobilization, normalizing sleep/awake cycle, avoidance of restraints, adequate oxygenation, optimal pain management, medication review with avoidance of potentially harmful drugs (opioid analgesics, benzodiazepines, certain antidepressants, histamine-1 receptor blockers, non-steroidal anti-inflammatory drugs and corticosteroids) and adequate hydration. Once the diagnosis is confirmed, management of postoperative delirium is directed at identifying the underlying cause(s), providing supportive care, and controlling symptoms. Supportive measures include airway protection, prevention of aspiration, maintenance of euvolemia, adequate nutritional support, optimal skin care to prevent pressure ulcers, mechanical devices to prevent deep venous thrombosis, and early mobilization. Management of symptoms comprises continuation of delirium prevention strategies. In case of severe agitation, the off-label use of first-generation (haloperidol, chlorpromazine) or second-generation antipsychotics (risperidone, clozapine) has become common practice among clinicians.
With advancing age, stasis of blood and risk for thrombosis increase. In conjunction with a hypercoagulable state resulting from surgery and anesthesia, these factors predispose elderly patients to postoperative venous thromboembolic events (VTE). The risk for deep venous thrombosis in older patients undergoing elective low risk surgery ranges between 2%–4%, and for pulmonary embolism the risk ranges from 1% to 2%. However, in the absence of prophylaxis, the risk of VTE is up to 50% in high-risk settings (e.g., cancer surgery, joint replacement, previous VTE, trauma, spinal surgery, vascular surgery). Mechanical prophylaxis (use of compression stockings and/or graded pneumatic compression devices), anticoagulation, and early ambulation are cost-effective means for reducing the risk of VTE.
Aging is also associated with impaired thermoregulatory function. These changes may be exacerbated by anesthetic-induced inhibition of thermoregulatory reflexes, resulting in the mild hypothermia commonly noted in older adults following major surgery. Hypothermia may contribute to electrolyte abnormalities (hypokalemia, hypomagnesemia), platelet dysfunction, surgical wound infection, impaired drug metabolism, and postoperative myocardial ischemia in older patients. Active thermal management, including forced-air warming devices, maintaining room temperature above 21°C, and/or administering warming intravenous fluids, is usually indicated in older adults with significant postoperative hypothermia (core body temperature <34.5°C).
Due to age-associated loss of subcutaneous tissue and decreased elasticity of aged skin, the older surgical patient is at increased risk of developing pressure ulcers if the skin is compressed for prolonged periods of time. Presence of decubitus ulcers often leads to secondary infections and delayed recovery resulting in prolonged hospital stays. Preventive measures are associated with 60%–70% reduction in the incidence of pressure ulcers, and include routine postoperative skin surveys, frequent repositioning, pressure redistributing support surfaces, pressure-relieving overlays in the operating room, foam alternatives, and heel protectors.
Other common postoperative complications include urinary tract infections, respiratory insufficiency, hospital-acquired pneumonia, and acute kidney injury. Limiting the use of urinary catheters, maintaining excellent pulmonary toilet and precautions against transmission of pathogens (especially hand hygiene), minimizing the use of nephrotoxins, and ensuring adequate hydration are the most effective means to avoid these complications.
5. Clinical pearls
(1) Advancing age is associated with reductions in the physiologic reserve of all organ systems, which greatly increase the risk of perioperative complications. (2) Older patients who have multiple comorbidities, complex medication regimens, functional limitations, cognitive impairment, and/or frailty are at increased risk for perioperative morbidity and iatrogenic complications. (3) Functional status and the presence of coexisting diseases, rather than age alone, are the primary determinants of perioperative risk; thus, age per se should not be considered an exclusion criterion for surgery. (4) Optimal perioperative care often requires a multidisciplinary approach involving the anesthesiologist, surgeon, primary care physician, and, in selected cases, a geriatrician, subspecialty consultants, nurses, a pharmacist, and various therapists. (5) Current ACC/AHA recommendations for the perioperative assessment of patients undergoing non-cardiac surgery are similar in older and younger patients. Testing is not recommended in the absence of unstable cardiac conditions unless the results would alter perioperative management or the patient is at high surgical risk with three or more clinical risk factors.
References
- 1.Wijeysundera DN, Duncan D, Nkonde-Price C, et al. Perioperative beta blockade in noncardiac surgery: a systematic review for the 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64:2406–2425. doi: 10.1016/j.jacc.2014.07.939. [DOI] [PubMed] [Google Scholar]
- 2.Poldermans D, Bax JJ, Boersma E, et al. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery: the Task Force for Preoperative Cardiac Risk Assessment and Perioperative Cardiac Management in Non-cardiac Surgery of the European Society of Cardiology (ESC) and endorsed by the European Society of Anaesthesiology (ESA) Eur J Anaesthesiol. 2010;27:92–137. doi: 10.1097/EJA.0b013e328334c017. [DOI] [PubMed] [Google Scholar]
- 3.Mebazaa A, Pitsis A, Rudiger A, et al. Clinical review: Practical recommendations on the management of perioperative heart failure in cardiac surgery. Crit Care. 2010;14:201. doi: 10.1186/cc8153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fang MC, Chen J, Rich MW. Atrial fibrillation in the elderly. Am J Med. 2007;129:481–487. doi: 10.1016/j.amjmed.2007.01.026. [DOI] [PubMed] [Google Scholar]
- 5.Amar D, Zhang H, Leung DH, et al. Older age is the strongest predictor of postoperative atrial fibrillation. Anesthesiology. 2002;96:352–356. doi: 10.1097/00000542-200202000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Hanada S, Kawakami H, Goto T, et al. Hypertension and anesthesia. Curr Opin Anaesthesiol. 2006;19:315–319. doi: 10.1097/01.aco.0000192811.56161.23. [DOI] [PubMed] [Google Scholar]
- 7.Lagoo-Deenadayalan SA, Newell MA, Pofahl WE. Common perioperative complications in older patients. In: Rosenthal RA, Zenilman ME, Katlic MR, editors. Principles and Practice of Geriatric Surgery. New York, USA: Springer; 2011. [Google Scholar]
- 8.Rudolph JL, Jones RN, Levkoff SE, et al. Derivation and validation of a preoperative prediction rule for delirium after cardiac surgery. Circulation. 2009;119:229–236. doi: 10.1161/CIRCULATIONAHA.108.795260. [DOI] [PMC free article] [PubMed] [Google Scholar]