Abstract
Paraneoplastic leukemoid reaction is a rare syndrome defined by a leukocyte count exceeding 50 Giga/Liter (G/L), mostly described with progressive lung or renal carcinoma. We report a case of a 68-year-old man with recurrent pancreatic carcinoma presenting a leukemoid reaction with a white blood cell count of 63.87 G/L without identified infectious, iatrogenic or hematologic causes. His overall condition quickly degraded and he died three weeks after the discovery of the leukemoid reaction. This is the first case in French literature of leukemoid reaction in a patient with pancreatic carcinoma with poor prognostic value.
Keywords: Leukemoid reaction, Pancreatic neoplasms, Paraneoplastic syndrome, Prognosis
Core tip: Paraneoplastic leukemoid reaction is a rare syndrome which seems to be associated with aggressive tumors, rapid clinical deterioration, and short survival. We report a rare presentation of pancreatic cancer with leukemoid reaction in a 68-year-old man who died three weeks after its discovery. This paper may contribute to clinical practice when encountering such a patient because of its poor prognostic value.
INTRODUCTION
Carcinoma is the most common (90%) and gravest type of pancreatic tumor with 5-year global survival rates around 5%. In France, it is the fifth cause of cancer-related deaths and its incidence is increasing fast with approximately 8000 annual new cases. Paraneoplastic syndromes can occur in a minority of cancer cases (less than 10%) and are not directly related to the physical effects of the tumor. Those most frequently associated with pancreatic carcinoma are Trousseau’s syndrome, Cushing’s syndrome, and the unexplained prolonged fever. They can reveal the disease or arise during progression. They can decline under treatment, even disappear with the cure and reappear in case of relapse. Paraneoplastic leukemoid reaction is defined as leukocytosis exceeding 50 Giga/Liter (G/L). Its diagnosis rests essentially on the exclusion of infectious, hematologic or iatrogenic causes such as growth factor or corticosteroid therapy[1]. This syndrome is most frequently associated with carcinomas, in particular lung and renal[2,3], and is rarely described in cancers of the digestive tract, including pancreatic cancers.
CASE REPORT
We report the case of a 68-year-old man with pancreatic carcinoma, who was diagnosed with paraneoplastic leukemoid reaction in the absence of plausible differential diagnoses.
Our patient was diagnosed with pT2N0M0 carcinoma of the head of the pancreas, discovered by jaundice, and operated by cephalic duodenopancreatectomy. He then received adjuvant chemotherapy with 6 cycles of gemzar. One year later, tumor markers (carbohydrate antigen 19-9 and carcinoembryonic antigen) increased and a positron emission tomography scan detected a local recurrence. Radiological stabilization and a decrease of markers were obtained after 4 cycles of folfox. Therefore, 6 additional cycles were administered.
Follow-up imaging revealed local evolution and hepatic metastases. Tumor marker levels were increased. A new line of chemotherapy was begun with folfiri. After 4 cycles, hepatic (Figure 1) and pulmonary evolution were observed associated with a progressive generalized weakness. Nevertheless, due to the patient’s strong insistence on treatment and a relatively stable overall condition, a third line of 5-fluorouracil (5-FU)/cisplatin was considered. During the first cycle, a white blood cell count showed extreme leukocytosis of 63.87 G/L (Figure 2), with neutrophil predominance of 92.7%, associated with a myelaemia of 1%, without abnormal eosinophilia, basophilia or anomaly of the other cell lines (hemoglobin 10.5 g/dL and platelets 207 G/L).
Figure 1.
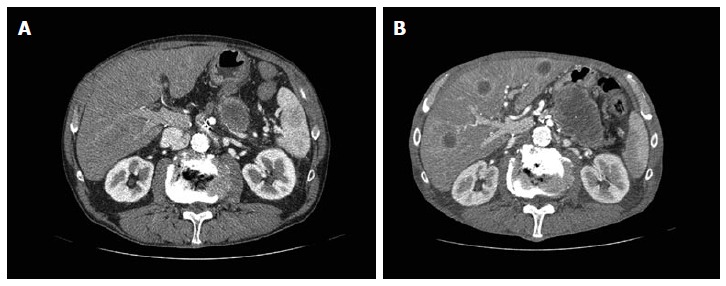
Computer tomography before (A) and after (B) leukemoid reaction. Pancreatic and hepatic evolution.
Figure 2.
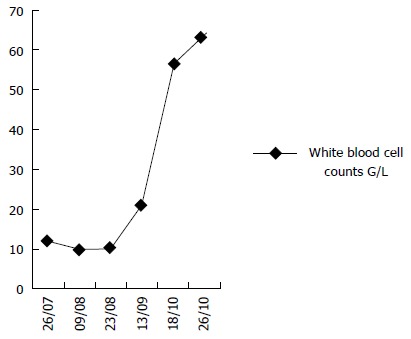
Evolution of white blood cell counts associated with leukemoid reaction. Leukocytosis rapid increase.
The patient had not received granulocyte colony-stimulating factors (G-CSF) or corticosteroids. Standard infectious investigations found no obvious sign of infection: C-reactive protein was slightly elevated at 138 mg/L, central and peripheral blood cultures as well as urine culture were negative, and a chest radiograph was normal. Moreover, a skeletal scintigraphy was performed and found no evidence of bone metastases. A cytological bone marrow examination showed a massively increased granulopoiesis with predominant neutrophils, complete maturation, without excess of blast cells or other anomalies that might suggest the existence of an acute leukaemia (Figure 3).
Figure 3.
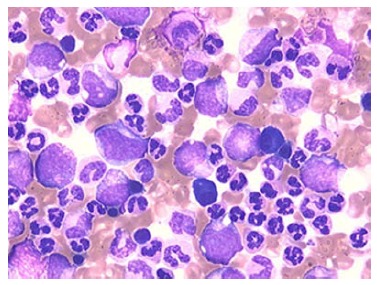
Bone marrow cytology (original magnification × 500). Increased granulopoiesis up to the neutrophils with a complete maturation and without blast cells.
Molecular genetic analysis did not find a BCR-ABL fusion gene or a V617F mutation in the JAK2 gene. The serum level of G-CSF was within normal range (< 40 pg/mL) and interleukin-6 (IL-6) was at 10 pg/mL (reference range: 0-10 pg/mL).
Only one cure of chemotherapy by 5-FU/cisplatin was administered, because of the patient’s rapid deterioration. He died three weeks after the development of the leukemoid reaction. During this period, leukocyte count remained above 50 G/L.
DISCUSSION
Paraneoplastic leukemoid reaction has rarely been described in cancers of the digestive tract, in particular pancreatic carcinoma, with only four cases found in the literature[4-7]. This seems to be the first case of leukemoid reaction in a patient with pancreatic cancer reported in the French literature.
Making this diagnosis requires eliminating an infection, a treatment with corticoids or G-CSF, and the existence of hematologic neoplasia. This paraneoplastic syndrome has a poor prognostic value without a fast effective anti-tumor treatment, as illustrated by other reviews of the literature. Indeed, it is associated with aggressive tumors, rapid clinical deterioration, and short survival. The mechanism of this reaction is still not formally identified. Some data, concerning essentially lung cancers, suggest a secretion by tumor cells of hematopoietic growth factors such as G-CSF or granulocyte-macrophage colony-stimulating factor (GM-CSF) inducing extreme leucocytosis[8,9]. Other mechanisms could also be involved in this reaction, in particular the production of pro-inflammatory cytokines in response to tumor progression or necrosis[10,11].
In our case, there was no elevation of G-CSF or IL-6, although serum levels were tested only once because of the fast change in the patient’s overall condition. No elevations of these levels were found in other reports, implying the existence of other factors.
Paraneoplastic leukemoid reaction is rarely associated with pancreatic cancer.
The mechanisms, prognosis, and management of this syndrome are poorly understood. More data are needed to conclude.
Leukemoid reaction appears at an advanced stage and may be a prognostic indicator in patients with pancreatic cancer. It is advisable to quickly diagnose the condition, after elimination of other plausible causes, because of its poor prognostic value.
COMMENTS
Case characteristics
A 68-year-old man with pancreatic carcinoma presented a paraneoplastic leukemoid reaction.
Clinical diagnosis
Rapid clinical deterioration with generalized weakness.
Differential diagnosis
Infection, treatment with corticoids or granulocyte colony-stimulating factors and hematologic neoplasia.
Laboratory diagnosis
White blood cell count showed extreme leukocytosis of 63.87 G/L.
Imaging diagnosis
Computer tomography scans revealed progression of local, liver and lung disease.
Pathological diagnosis
Carcinoma of the pancreas.
Treatment
The tumor was treated by cephalic duodenopancreatectomy associated with adjuvant chemotherapy, and three additional lines of chemotherapy for metastatic disease.
Related reports
Poor prognostic value is also illustrated by other reviews of the literature with short survival. The mechanism of this reaction is still not formally identified, but some data suggest a secretion by tumor cells of hematopoietic growth factors or pro-inflammatory cytokines.
Term explanation
Paraneoplastic leukemoid reaction is defined as leukocytosis exceeding 50 G/L.
Experiences and lessons
Paraneoplastic leukemoid reaction is a rare syndrome, infrequently described with pancreatic cancer, which seems to be associated with poor prognostic value.
Peer-review
A very rare complication of pancreatic cancer with very rare occurence in gastrointestinal cancers and pancreatic cancer in peculiar, worth publishing to inform physicians. It is a step forward on the way of clarifying the pathogeny of this syndrome.
Footnotes
Supported by The University Caen Basse Normandie, 14000 Caen, France.
Institutional review board statement: This case report was exempt from the Institutional Review Board: Comité de protection des personnes Nord Ouest III at CHU Caen.
Informed consent statement: The patient involved in this study died before the manuscript was written. However data are anonymized not to cause harm to the patient or their families, and risk of identification is low.
Conflict-of-interest statement: No conflict of interest to declare.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: April 3, 2015
First decision: July 10, 2015
Article in press: August 7, 2015
P- Reviewer: Matsumoto I, Surlin VM S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
References
- 1.Halkes CJ, Dijstelbloem HM, Eelkman Rooda SJ, Kramer MH. Extreme leucocytosis: not always leukaemia. Neth J Med. 2007;65:248–251. [PubMed] [Google Scholar]
- 2.Riesenberg H, Müller F, Görner M. Leukemoid reaction in a patient with adenocarcinoma of the lung: a case report. J Med Case Rep. 2012;6:211. doi: 10.1186/1752-1947-6-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang W, Wang F, Li Y, Duan F, Yu Z. Leukemoid reaction in sarcomatoid renal cell carcinoma: a two-case report. World J Surg Oncol. 2014;12:100. doi: 10.1186/1477-7819-12-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Qureshi KM, Raman AK, Tan D, Fakih MG. Leukemoid reaction in pancreatic cancer: a case report and review of the literature. JOP. 2006;7:631–634. [PubMed] [Google Scholar]
- 5.Godquin B. [Cancer of the pancreas and paraneoplastic leukemoid syndrome] Chirurgie. 1973;98:785–787. [PubMed] [Google Scholar]
- 6.Akoun G, Duhamel G, Duvaldestin P, Koubi G, Brocard H. Myeloid leukemoid reaction in cancer of the pancreas: paraneoplastic syndrome or myeloid leukosis? Sem Hop. 1972;48:861–863. [PubMed] [Google Scholar]
- 7.Akoun G, Duhamel G, Duvaldestin P, Koubi G, Brocard H. Paraneoplastic leukemoid reaction of a myeloid type or myeloid leukemia in cancer of the pancreas? Presse Med. 1971;79:2327. [PubMed] [Google Scholar]
- 8.Hocking W, Goodman J, Golde D. Granulocytosis associated with tumor cell production of colony-stimulating activity. Blood. 1983;61:600–603. [PubMed] [Google Scholar]
- 9.Jardin F, Vasse M, Debled M, Dominique S, Courville P, Callonnec F, Buchonnet G, Thiberville L, Tilly H. Intense paraneoplastic neutrophilic leukemoid reaction related to a G-CSF-secreting lung sarcoma. Am J Hematol. 2005;80:243–245. doi: 10.1002/ajh.20454. [DOI] [PubMed] [Google Scholar]
- 10.Inoue M, Minami M, Fujii Y, Matsuda H, Shirakura R, Kido T. Granulocyte colony-stimulating factor and interleukin-6-producing lung cancer cell line, LCAM. J Surg Oncol. 1997;64:347–350. doi: 10.1002/(sici)1096-9098(199704)64:4<347::aid-jso18>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 11.Chen YM, Whang-Peng J, Liu JM, Chao Y, Lai CR, Wang SY, Perng RP. Leukemoid reaction resulting from multiple cytokine production in metastatic mucoepidermoid carcinoma with central necrosis. Jpn J Clin Oncol. 1995;25:168–172. [PubMed] [Google Scholar]


