Abstract
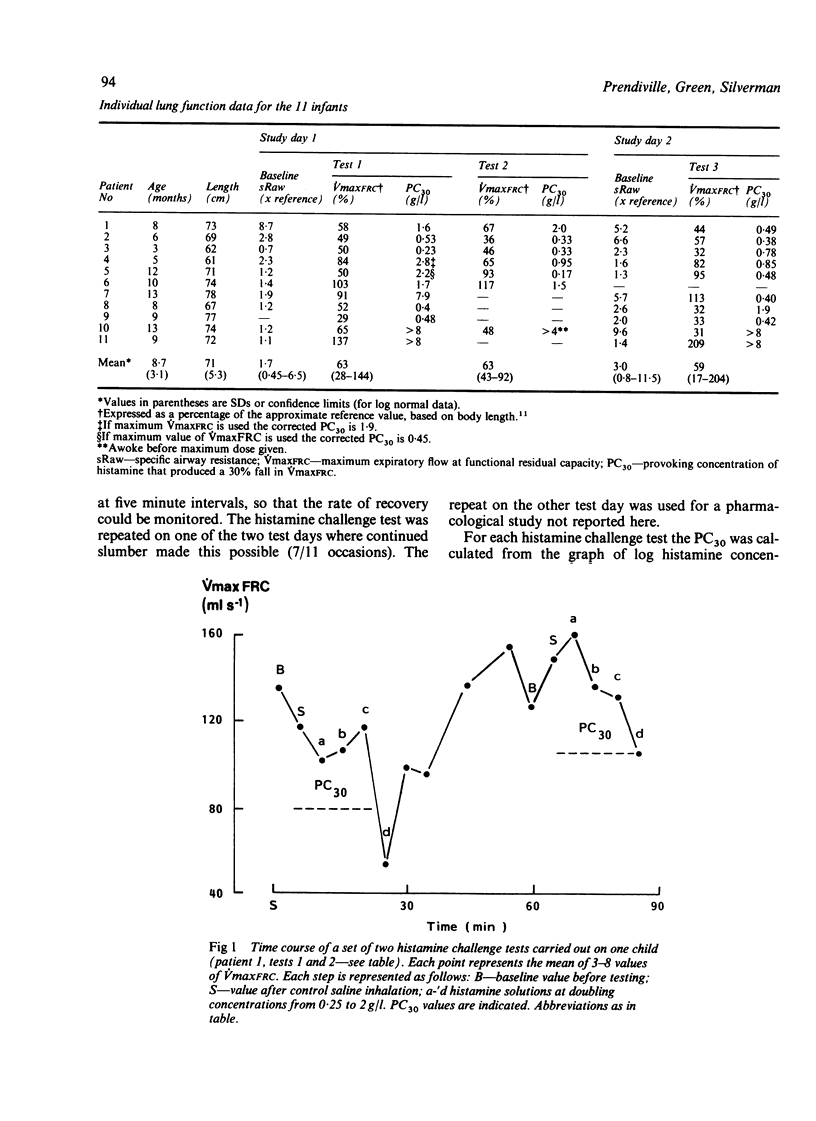
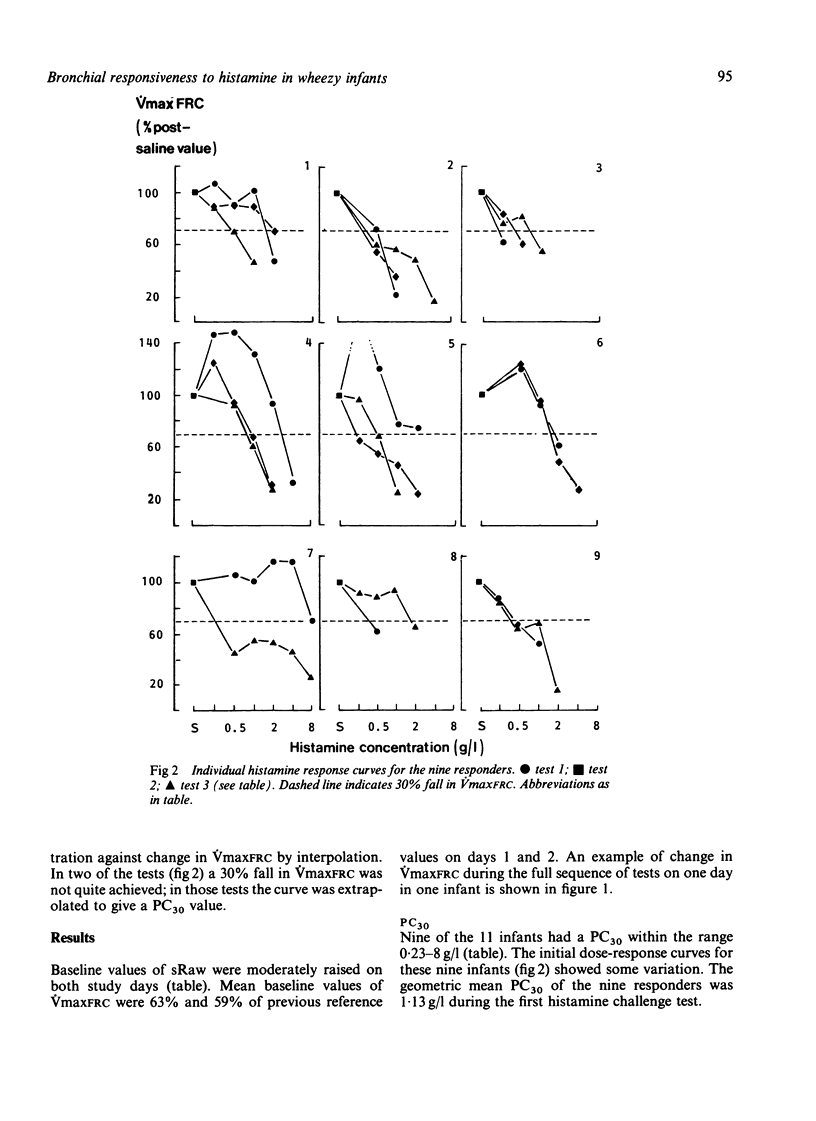
Little is known about airway responsiveness in infancy. The bronchial response to incremental doses of nebulised histamine (to a maximum dose of 8 g/l) was measured in 11 wheezy infants with a mean age of 8.7 months. The study was repeated after a 30-40 minute recovery period in seven infants and again on a separate day in 10. The index of response was the provoking concentration of histamine that produced a 30% fall in the maximum expiratory flow at functional residual capacity (PC30), taken from partial forced expiratory flow-volume curves produced in a pressure jacket. Nine of 11 infants had a PC30 of less than 8 g/l. The response was consistent between tests in both the nine responders and the two who failed to respond at 8 g/l. The PC30 was lower in infants with more severe baseline airway obstruction. Spontaneous recovery after challenge was complete in 30 minutes in seven of eight infants studied. The highest doses of histamine caused changes in the configuration of the flow-volume curves and symptomatic cough and wheeze in addition to a change in forced flow rates. This study provides clear evidence of intrathoracic airway responsiveness to histamine in infancy.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Boushey H. A., Holtzman M. J. Experimental airway inflammation and hyperreactivity. Searching for cells and mediators. Am Rev Respir Dis. 1985 Mar;131(3):312–313. doi: 10.1164/arrd.1985.131.3.312. [DOI] [PubMed] [Google Scholar]
- Boushey H. A., Holtzman M. J., Sheller J. R., Nadel J. A. Bronchial hyperreactivity. Am Rev Respir Dis. 1980 Feb;121(2):389–413. doi: 10.1164/arrd.1980.121.2.389. [DOI] [PubMed] [Google Scholar]
- Cartier A., Malo J. L., Bégin P., Sestier M., Martin R. R. Time course of the bronchoconstriction induced by inhaled histamine and methacholine. J Appl Physiol Respir Environ Exerc Physiol. 1983 Mar;54(3):821–826. doi: 10.1152/jappl.1983.54.3.821. [DOI] [PubMed] [Google Scholar]
- Cockcroft D. W., Killian D. N., Mellon J. J., Hargreave F. E. Bronchial reactivity to inhaled histamine: a method and clinical survey. Clin Allergy. 1977 May;7(3):235–243. doi: 10.1111/j.1365-2222.1977.tb01448.x. [DOI] [PubMed] [Google Scholar]
- Dab I., Alexander F. On the advantages of specific airway resistance. Pediatr Res. 1978 Aug;12(8):878–881. doi: 10.1203/00006450-197808000-00016. [DOI] [PubMed] [Google Scholar]
- England S. J., Ho V., Zamel N. Laryngeal constriction in normal humans during experimentally induced bronchoconstriction. J Appl Physiol (1985) 1985 Feb;58(2):352–356. doi: 10.1152/jappl.1985.58.2.352. [DOI] [PubMed] [Google Scholar]
- Godfrey S., Bar-Yishay E., Arad I., Landau L. I., Taussig L. M. Flow-volume curves in infants with lung disease. Pediatrics. 1983 Oct;72(4):517–522. [PubMed] [Google Scholar]
- Godfrey S., Beardsmore C. S., Maayan C., Bar-Yishay E. Can thoracic gas volume be measured in infants with airways obstruction? Am Rev Respir Dis. 1986 Feb;133(2):245–251. doi: 10.1164/arrd.1986.133.2.245. [DOI] [PubMed] [Google Scholar]
- Hariparsad D., Wilson N., Dixon C., Silverman M. Reproducibility of histamine challenge tests in asthmatic children. Thorax. 1983 Apr;38(4):258–260. doi: 10.1136/thx.38.4.258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higenbottam T. Narrowing of glottis opening in humans associated with experimentally induced bronchoconstriction. J Appl Physiol Respir Environ Exerc Physiol. 1980 Sep;49(3):403–407. doi: 10.1152/jappl.1980.49.3.403. [DOI] [PubMed] [Google Scholar]
- Juniper E. F., Syty-Golda M., Hargreave F. E. Histamine inhalation tests: inhalation of aerosol via a facemask versus a valve box with mouthpiece. Thorax. 1984 Jul;39(7):556–557. doi: 10.1136/thx.39.7.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mygind N. Mediators of nasal allergy. J Allergy Clin Immunol. 1982 Sep;70(3):149–159. doi: 10.1016/0091-6749(82)90036-7. [DOI] [PubMed] [Google Scholar]
- Neijens H. J., Duiverman E. J., Kerrebijn K. F. Bronchial responsiveness in children. Pediatr Clin North Am. 1983 Oct;30(5):829–846. doi: 10.1016/s0031-3955(16)34468-6. [DOI] [PubMed] [Google Scholar]
- Prendiville A., Green S., Silverman M. Paradoxical response to nebulised salbutamol in wheezy infants, assessed by partial expiratory flow-volume curves. Thorax. 1987 Feb;42(2):86–91. doi: 10.1136/thx.42.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman M. Bronchodilators for wheezy infants? Arch Dis Child. 1984 Jan;59(1):84–87. doi: 10.1136/adc.59.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman M., Prendiville A., Green S. Partial expiratory flow-volume curves in infancy: technical aspects. Bull Eur Physiopathol Respir. 1986 May-Jun;22(3):257–262. [PubMed] [Google Scholar]
- Stocks J., Levy N. M., Godfrey S. A new apparatus for the accurate measurement of airway resistance in infancy. J Appl Physiol Respir Environ Exerc Physiol. 1977 Jul;43(1):155–159. doi: 10.1152/jappl.1977.43.1.155. [DOI] [PubMed] [Google Scholar]
- Stocks J. The functional growth and development of the lung during the first year of life. Early Hum Dev. 1977 Dec;1(3):285–309. doi: 10.1016/0378-3782(77)90041-x. [DOI] [PubMed] [Google Scholar]
- Stocks J., Thomson A., Silverman M. The numerical analysis of pressure-flow curves in infancy. Pediatr Pulmonol. 1985 Jan-Feb;1(1):19–26. doi: 10.1002/ppul.1950010107. [DOI] [PubMed] [Google Scholar]
- Taussig L. M., Landau L. I., Godfrey S., Arad I. Determinants of forced expiratory flows in newborn infants. J Appl Physiol Respir Environ Exerc Physiol. 1982 Nov;53(5):1220–1227. doi: 10.1152/jappl.1982.53.5.1220. [DOI] [PubMed] [Google Scholar]
- Tien Y. K., Elliott E. A., Mead J. Variability of the configuration of maximum expiratory flow-volume curves. J Appl Physiol Respir Environ Exerc Physiol. 1979 Mar;46(3):565–570. doi: 10.1152/jappl.1979.46.3.565. [DOI] [PubMed] [Google Scholar]



