Abstract
Background:
Vascular endothelial growth factor (VEGF) has an essential role in tumor metastasis by inducing the construction of abnormal blood vessels. Epidermal growth factor receptor (EGFR) is involved in different parts of cancer growth such as tumor initiation, angiogenesis and metastasis.
Objectives:
The aim of this study was to evaluate the expression of VEGF and EGFR in ovarian cancer in southern Iran and to assess the correlation between expression of these two markers and patients’ age, tumor stage, and grade.
Patients and Methods:
In this cross-sectional study, 50 paraffin blocks of serous ovarian adenocarcinomas and 50 paraffin-embedded specimens from control individuals operated for reasons other than malignancy were immunohistochemically stained using anti-human VEGF and EGFR antibodies.
Results:
A significant difference in the frequency of positive expression of VEGF was observed in ovarian cancer patients (25.0%) compared with the control group (8.0%) (P = 0.023). A significant difference between EGFR expression in patients (56.8%) and controls (24.0%) was also obtained (P = 0.001). No significant correlation between VEGF and EGFR expression and patients’ age, tumor grade and stage were detected (P > 0.05).
Conclusions:
The significant increase in both VEGF and EGFR in the patients with ovarian cancer compared to healthy individuals could have prognostic value. Identifying these markers may be useful for chemopreventive and chemotherapeutic strategies for patients with serous ovarian cancer.
Keywords: Vascular Endothelial Growth Factor A, Ovarian Cancer, Endothelial Growth Factor Receptor, Angiogenic Factor
1. Background
Ovarian cancer is the sixth most common cause of diagnosed cancer among women in the world and the second most common gynecologic malignancy in females (1, 2). Despite recent developments in the management of ovarian cancer, it is still the most lethal female reproductive system tumor due to the lack of early warning signs and effective screening tools (3). Therefore, when cancer is diagnosed, it has often developed to an advanced stage. Although the ovarian cancer incidence in Iran is lower than US and Europe, it is still a great matter of concern for health organizations (4, 5). Recently, many studies have been directed toward improving the prognosis of ovarian cancer including screening tests for early stage tumors using both imaging methods and tumor markers. Abundant molecular agents from samples taken from clinically diagnosed ovarian cancer patients have demonstrated potential as diagnostic markers, but few have been used in preclinical evaluations and screening (6, 7).
The ability of tumors to form new blood-vessels has been a major focus of cancer research over the past few decades. The vascular endothelial growth factor (VEGF) family of growth factors and their receptors form an important pathway in signaling tumor angiogenesis. The prognostic significance of VEGF expression has been studied in many types of cancers such as cervical, gastric and lung cancers (8, 9). VEGF also plays an important role in tumor metastasis by inducing the construction of abnormal blood vessels (10). Advanced degrees of tumor angiogenesis and VEGF expression in ovarian cancer are associated with a poor prognosis. Regarding the vital role of VEGF in promoting different cancers, its signaling pathway has been considered to be an attractive target for cancer therapy (11). It has been shown that VEGF blockage normalizes tumor vessels and increases oxygen and chemotherapeutic agents' delivery into malignant tissues (10).
The epithelial growth factor receptor (EGFR) family of tyrosine kinase receptors is another target which has been considered for cancer immunotherapy. EGFR is one of four members of the human epidermal receptor (HER) which has been demonstrated to have physiologic and also oncogenic roles in a number of malignancies (12). Different pathways of EGFR take part as proto-oncogenes in several cancers such as gastrointestinal, oral and breast cancers (13). EGFR is over-expressed in up to 60% of ovarian epithelial malignancies (14) and its activation is associated with increased malignant tumor phenotype and poor patient prognosis (15). Since EGFR is involved in different parts of cancer growth such as tumor initiation, angiogenesis and metastasis, it represents an attractive target for therapeutic interventions (14, 15).
It has been shown that some factors including genetics are important in tumor gene expression and formation especially in breast and ovarian cancers (16). There was no information about the expression of these two markers in Iranian patients with ovarian cancer. The objective of this study was to evaluate the expression of VEGF and EGFR in patients with ovarian cancer referred to hospitals of the Shiraz University of Medical Sciences as reference hospitals in southern Iran in comparison with normal healthy patients using immunohistochemistry (IHC) techniques. The correlation between these markers and patients’ age, tumor stages, and grades were also investigated.
2. Objectives
The aim of this study was to evaluate the expression of VEGF and EGFR in ovarian cancer in southern Iran and to assess the correlation between expression of these two markers and patients’ age, tumor stage, and grade.
3. Patients and Methods
3.1. Study Population
In this cross-sectional study, 50 patients with serous ovarian adenocarcinomas who underwent surgical resection and 50 cases operated for reasons other than malignancies, as a control group, were selected. All cases were referred to the Shiraz University of Medical Science hospitals during the years 2010 - 2014. Written informed consent was obtained from all patients and controls after approval of the study by the ethical committee of Shiraz University of Medical Sciences. One archival paraffin-embedded tissue block from each case was included. Inclusion criteria for the patients were confirmed cases of serous ovarian adenocarcinomas staging based on international federation of obstetrics and gynecology (FIGO) (stages I - IV) and, for the control group, no history of malignancy or autoimmune disease in the individuals and their immediate relatives. The tumor grading was performed according to the three-tiered world health organization (WHO) criteria (17). The control group was age matched with the patients.
3.2. Immunohistochemistry
The paraffin embedded blocks were fixed in 10% natural buffered formalin solution for 24 hours and placed at 60°C, in an oven, for 20 minutes before dewaxing. Hot slides were deparaffinized in xylene and rehydrated through graded alcohol. After washing with distilled water and phosphate buffered saline PBS, the slides were immersed in methanol containing 10% hydrogen peroxide for 4 - 5 minutes in a dark place at room temperature to block endogenous peroxidase activity. Following washing with PBS, the slides were placed in hot Tris-EDTA buffer (95°C, pH = 9) to obtain a more vigorous antigen retrieval procedure. Tissue nonspecific binding sites were blocked by goat serum (diluted 1:10 in PBS) for 20 minutes to reduce the background. The sections were then incubated with primary antibody (mouse monoclonal anti-VEGF or anti-EGFR) (Dako, Denmark) for 1 hour at room temperature. After washing with PBS, secondary antibody (polyclonal goat anti-mouse horseradish peroxidase conjugated antibody) (Dako, Denmark) was added and the slides were placed in a humid chamber and incubated for 30 minutes. The samples were exposed to diaminobenzidine as a chromogen for 5 minutes, slightly counterstained with hematoxylin (for 5 - 7 minutes), dehydrated through graded alcohol and mounted with mounting media.
Formalin-fixed normal human bladder tissue was used as a positive control for VEGF and sections of small intestine were used as a positive control for EGFR. Negative control slides were prepared by omitting the primary antibody.
For the analysis of VEGF and EGFR immunostaining, all slides were observed by two pathologists who were blinded to the clinical outcome of the patients. Discordant cases were reevaluated by two pathologists simultaneously. IHC expression of VEGF and EGFR was considered positive whenever at least 10% of the cells were stained, as previously described (8, 18-20).
3.3. Statistical Analysis
The relationship of VEGF and EGFR to various clinicopathologic factors was evaluated using the Fisher’s Exact and Chi-square tests by SPSS software version 20. The P value for statistical significance was defined as P < 0.05.
4. Results
Patients’ ages in the ovarian cancer group ranged from 28 - 69 years (median 53 years) and the age range of the control group was 31 - 65 years (median 51 years). VEGF and EGFR expression analysis was performed on 48 and 44 tumor specimens, respectively, after excluding cases with insufficient documentation. Clinicopathologic characteristics of patients and control individuals are summarized in Table 1.
Table 1. VEGF and EGFR Expression and Clinicopathologic Variables in Patients With Serous Ovarian Carcinoma and Control a,b.
| Group | VEGF | EGFR | ||||
|---|---|---|---|---|---|---|
| Patients (n = 48) | Controls (n = 50) | P Value | Patients (n = 44) | Controls (n = 50) | P Value | |
| Age, y | 52.7 ± 8.5 | 50.4 ± 9.1 | 0.204 | 52.5 ± 8.5 | 50.4 ± 9.1 | 0.229 |
| Age group | 1.00 | 0.761 | ||||
| ≤ 53 | 25 (52.3) | 23 (52.1) | ||||
| > 53 | 23 (47.7) | 21 (47.9) | ||||
| FIGO stage | 0.402 | 0.406 | ||||
| I | 14 (29.2) | 11 (25) | ||||
| II | 4 (8.3) | 4 (9.1) | ||||
| III | 19 (39.6) | 19 (43.2) | ||||
| IV | 11 (22.9) | 10 (22.7) | ||||
| Histologic grade | 0.672 | 0.358 | ||||
| Well differentiated | 17 (35.4) | 16 (36.4) | ||||
| Moderately differentiated | 13 (27.1) | 12 (27.3) | ||||
| Poorly differentiated | 18 (37.5) | 16 (36.4) | ||||
a Abbreviations: EGFR, epidermal growth factor receptor; FIGO, international federation of obstetrics and gynecology; VEGF, vascular endothelial growth factor.
b Values are presented as No. (%) or mean ± SD.
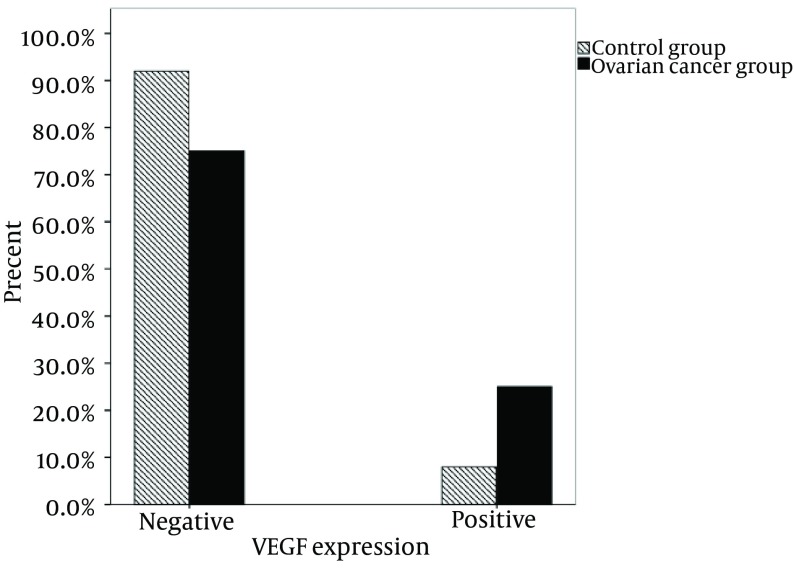
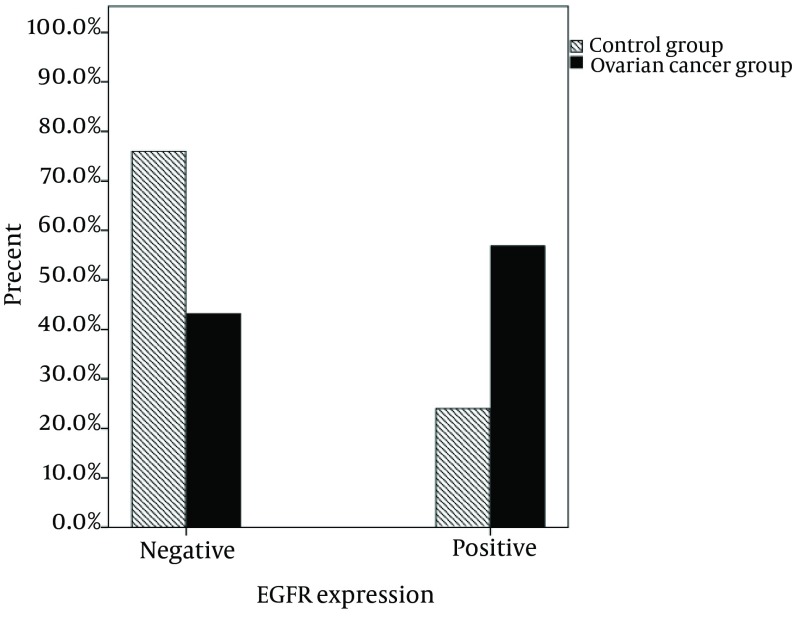
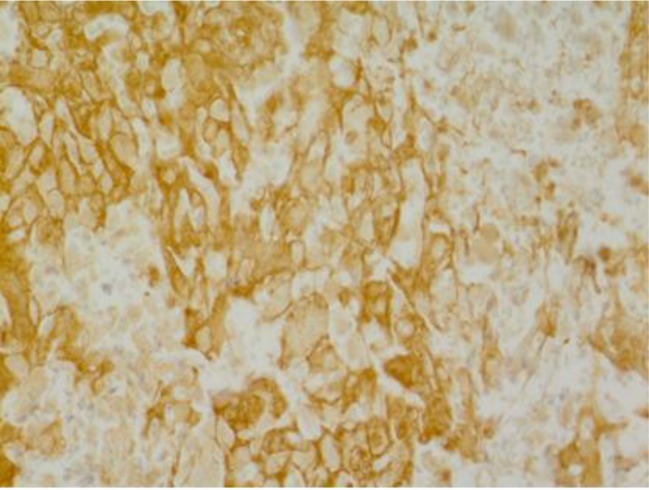
The statistical analysis showed a significant difference between VEGF expression in patients with ovarian cancer (25.0%) and control group (8.0%) (P = 0.023). There was also a significant difference between EGFR expression in patients (56.8%) and the controls (24.0%) (P = 0.001) (Table 2, Figures 1 and 2).The IHC positive staining for VEGF and EGFR are shown in Figures 3 and 4.
Table 2. VEGF and EGFR Expression in Patients With Serous Ovarian Carcinoma and Control Individuals a,b.
| Group | VEGF (n = 48) | EGFR (n = 44) | ||
|---|---|---|---|---|
| Positive | Negative | Positive | Negative | |
| FIGO Stage | ||||
| I | 4 (28.6) | 10 (71.4) | 6 (54.5) | 5 (45.5) |
| II | 2 (50) | 2 (50) | 1 (25) | 3 (75) |
| III | 5 (26.3) | 14 (73.7) | 13 (68.4) | 6 (31.6) |
| IV | 1 (9.1) | 10 (90.9) | 5 (50) | 5 (50) |
| Histologic Grade | ||||
| Well differentiated | 3 (17.6) | 14 (82.4) | 11 (68.8) | 5 (31.2) |
| Moderately differentiated | 4 (30.8) | 9 (69.2) | 5 (41.7) | 7 (58.3) |
| Poorly differentiated | 5 (27.8) | 13 (72.2) | 9 (56.2) | 7 (43.8) |
| Total patients | 12 (25) | 36 (75) | 25 (56.8) | 19 (43.2) |
| Controls | 4 (8) | 46 (92) | 12 (24) | 38 (76) |
| P value | 0.023 | 0.001 | ||
a Abbreviations: EGFR, epidermal growth factor receptor; FIGO, international federation of obstetrics and gynecology; VEGF, vascular endothelial growth factor.
b Values are presented as No. (%) or mean ± SD.
Figure 1. Vascular Endothelial Growth Factor Expression Was Observed More Frequently in the Patients With Serous Ovarian Carcinoma (P < 0.05).
Figure 2. Epidermal Growth Factor Receptor Expression Was Observed More Frequently in the Patients With Serous Ovarian Carcinoma (P < 0.05).
Figure 3. Immunohistochemical Staining for Vascular Endothelial Growth Factor (VEGF) in Serous Ovarian Carcinoma Tissue Showing Positive Expression of VEGF.
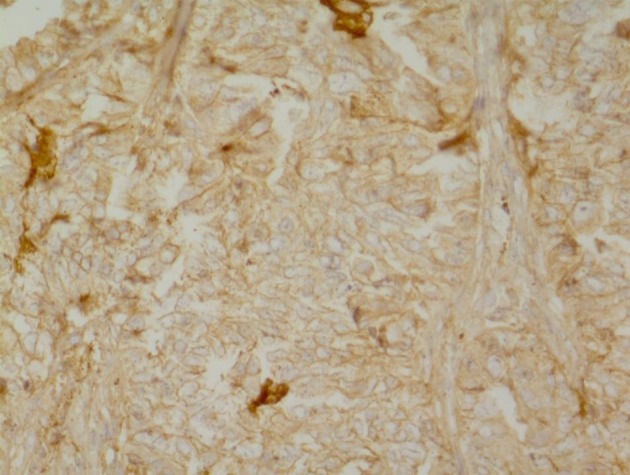
Figure 4. Immunohistochemical Staining for Epidermal Growth Factor Receptor (EGFR) in Serous Ovarian Carcinoma Tissue Showing Positive Expression of EGFR.
No significant differences in VEGF (P = 0.402) or EGFR (P = 0.406) expression at different stages was obtained (Table 1). The stages I and II were considered early stage and stages III and IV as late stage. Positive immunostaining for VEGF was found in 33.3% of early stage and 20.0% of late stage tumors. The expression of EGFR was more frequent in late stage tumors (62.1%) than in early stage tumors (46.7%). Differences between VEGF and EGFR expressions in the early and late stages were not statistically significant (P > 0.05) (Table 3).
Table 3. VEGF and EGFR Expression in Early Stage (Stages I and II) and Late Stage (Stages III and IV) of Ovarian Cancer.
| Group | VEGF (n=48) | EGFR (n=44) | ||
|---|---|---|---|---|
| Positive (n = 12) | Negative (n = 36) | Positive (n = 25) | Negative (n = 19) | |
| Early stage | 6 (33.3) | 12 (66.7) | 7 (46.7) | 8 (53.3) |
| Late stage | 6 (20.0) | 24 (80.0) | 18 (62.1) | 11 (37.9) |
| P value | 0.325 | 0.357 | ||
Compared to well differentiated tumors (17.6%), a higher percentage of moderately (30.8%) and poorly (27.8%) differentiated tumors showed positive expression of VEGF. EGFR expression was positive in 68.8% of well differentiated, 41.7% of moderately, and 56.2% of poorly differentiated tumors. VEGF and EGFR expression did not correlate with tumor grade and patients’ age (P > 0.05) (Table 1).
5. Discussion
Our results revealed significantly more frequent expression of VEGF and EGFR in the ovarian carcinoma than in the control group. No association between these markers and patients’ age, tumor stages, and grades were found.
VEGF as an angiogenic factor plays a critical role in tumor angiogenesis and neovascularization (21). The clinicopathologic and prognostic value of VEGF in ovarian cancer has been investigated in different studies. Many of these studies confirmed that intratumoral VEGF is overexpressed in ovarian cancer and it could be considered to be a prognostic factor. However, the association between VEGF expression and other prognostic factors including tumor stage and grade has been shown some controversies. Findings of a study performed by Shen et al. (22) showed more frequent expression of VEGF in ovarian adenocarcinoma than in borderline and benign tumors. They found a significant, strongly-positive VEGF expression in late stage and high grade tumors. Some other studies also showed that VEGF overexpression is related to advanced tumor stages in patients with ovarian cancer (23, 24). However, there are some reports that failed to identify a significant association between VEGF and clinicopathologic factors (25-27). Duncan et al. (26) showed that high VEGF expression was related to a shorter survival. But they did not find any association between VEGF expression and patients’ age, tumor stage and grade. Similar results are reported by Siddiqui et al. (27). Consistent with these results, our study revealed positive expression of VEGF at a significantly higher frequency in ovarian tumor specimens relative to the control group. No association between VEGF expression and age, tumor stage and grade was found. Although it was not statistically significant, we observed positive expression of VEGF in a higher percentage of early stage tumors (33.3%) than late stage tumors (20%). High expression of VEGF in early stage disease has been reported in some tumors (28-30). In the other study (29) researchers showed that protein and gene expression levels of VEGF is higher in early stage patients of prostate cancer. They concluded that VEGF, as an angiogenic isoform, is overexpressed in early stages while in advanced stages of disease the lymphangiogenic isoform VEGF-D is up-regulated. In a study by Paley et al. (30) it was illustrated that elevated VEGF expression in early stages of ovarian cancer is related to a worse prognosis. Findings of a meta-analysis showed that intratumoral overexpression of VEGF is a significant prognostic factor in early stages, but not in late stages of ovarian cancer (31).
The correlation of EGFR expression level with aggressive phenotypes, metastasis and poor prognosis of solid tumors including breast, gastric and colorectal carcinoma has been reported in several studies (32-34). Several anti-EGFR therapeutics are currently approved by the US Food and Drug Administration for treatment of various tumor types, including tyrosine kinase inhibitors (TKIs) such as lapatinib and erlotinib and monoclonal antibodies such as cetuximab and panitumumab (35). Overexpression of EGFR in ovarian tumors has also been reported. In a study by Brustmann (36), EGFR was expressed in 64% of the ovarian serous carcinomas while serous cystadenomas and serous borderline ovarian tumors did not show any EGFR immunoreactivity. Significant strong EGFR expression was observed in higher grades tumors. Psyrri et al. (37) found a significant association between EGFR overexpression and decreased survival in ovarian cancer patients. However EGFR expression did not correlate with any clinicopathologic variables, including age, tumor grade and stage. The results of a study performed on patients with advanced ovarian tumors could not confirm the prognostic significance of EGFR and its association with clinical parameters (38). Several studies have investigated protein expression, gene amplification, and mutations of EGFR in ovarian cancer. Lassus et al. (39), showed that EGFR amplification and overexpression is related to patients’ age, high tumor grade, and poor prognosis. No mutations in the EGFR gene were observed. They suggested that EGFR amplification has a greater prognostic value than EGFR protein overexpression. It also has been shown that EGFR protein expression is related to its gene amplification in primary ovarian tumors (40). Despite the rare frequency of EGFR gene mutations in ovarian cancer (39, 40) Tanaka et al. (41) reported high frequency of EGFR mutations in Japanese ovarian cancer patients which might suggest the effect of ethnicity. They also found a correlation between EGFR gene mutations and histological types, but not FIGO stage or 5 years survival. In our study, EGFR protein was detectable in 56.8% of ovarian cancer patients and 24.0% of control individuals. A significant difference between these two groups was obtained. Consistent with the results of the previous studies (37, 38) we could not find any association between EGFR expression and age, histologic grade, and FIGO stage. However, we observed EGFR expression in the majority (62.1%) of late stage patients.
Our study revealed positive expression of VEGF and EGFR at a significant frequency in patients with serous ovarian adenocarcinomas. This is the first study that has evaluated the expression of these markers in Iranian patients. Identifying VEGF and EGFR could have clinical significance and may be useful for targeted therapy in ovarian cancer patients sensitive to VEGF and EGFR inhibitors. However larger scale investigation with more samples at different stages and grades can support the results of present study.
Acknowledgments
The authors acknowledge Shiraz University of Medical Sciences for financial support grant no: 4899.The cooperation of Baqiyatallah University is acknowledged. We thank Pamela Waltl (AuthorAID in the Eastern Mediterranean) for improving the use of English in the text.
Footnotes
Authors’ Contributions: Reza Ranjbar participated in the study conception and helped draft and revise the manuscript. Foroogh Nejatollahi conceived of the study and its design, coordinated and helped to draft the manuscript, and revised the manuscript for intellectual content. Ahmad Sina Nedaei Ahmadi performed data collection, analyzed the data and drafted the manuscript. Hossein Hafezi participated in data collection and interpretation and helped draft the manuscript. Akbar Safaie performed immunostaining analysis and helped draft the manuscript. All authors read and approved the final manuscript.
Conflict of Interests: The authors declare that there are no conflicts of interest.
Financial Disclosure: There is no financial disclosure.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 3.Ramakrishnan S, Subramanian IV, Yokoyama Y, Geller M. Angiogenesis in normal and neoplastic ovaries. Angiogenesis. 2005;8(2):169–82. doi: 10.1007/s10456-005-9001-1. [DOI] [PubMed] [Google Scholar]
- 4.Arab M, Khayamzadeh M, Tehranian A, Tabatabaeefar M, Hosseini M, Anbiaee R, et al. Incidence rate of ovarian cancer in Iran in comparison with developed countries. Indian J Cancer. 2010;47(3):322–7. doi: 10.4103/0019-509X.64721. [DOI] [PubMed] [Google Scholar]
- 5.Masoompour SM, Yarmohammadi H, Rezaianzadeh A, Lankarani KB. Cancer incidence in southern Iran, 1998-2002: results of population-based cancer registry. Cancer Epidemiol. 2011;35(5):e42–7. doi: 10.1016/j.canep.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 6.Jacobs IJ, Menon U. Progress and challenges in screening for early detection of ovarian cancer. Mol Cell Proteomics. 2004;3(4):355–66. doi: 10.1074/mcp.R400006-MCP200. [DOI] [PubMed] [Google Scholar]
- 7.Robati M, Ghaderi A, Mehraban M, Shafizad A, Nasrolahi H, Mohammadianpanah M. Vascular endothelial growth factor (VEGF) improves the sensitivity of CA125 for differentiation of epithelial ovarian cancers from ovarian cysts. Arch Gynecol Obstet. 2013;288(4):859–65. doi: 10.1007/s00404-013-2819-7. [DOI] [PubMed] [Google Scholar]
- 8.Choi CH, Song SY, Choi JJ, Park YA, Kang H, Kim TJ, et al. Prognostic significance of VEGF expression in patients with bulky cervical carcinoma undergoing neoadjuvant chemotherapy. BMC Cancer. 2008;8:295. doi: 10.1186/1471-2407-8-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaya A, Ciledag A, Gulbay BE, Poyraz BM, Celik G, Sen E, et al. The prognostic significance of vascular endothelial growth factor levels in sera of non-small cell lung cancer patients. Respir Med. 2004;98(7):632–6. doi: 10.1016/j.rmed.2003.12.017. [DOI] [PubMed] [Google Scholar]
- 10.Kumaran GC, Jayson GC, Clamp AR. Antiangiogenic drugs in ovarian cancer. Br J Cancer. 2009;100(1):1–7. doi: 10.1038/sj.bjc.6604767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chambers SK, Clouser MC, Baker AF, Roe DJ, Cui H, Brewer MA, et al. Overexpression of tumor vascular endothelial growth factor A may portend an increased likelihood of progression in a phase II trial of bevacizumab and erlotinib in resistant ovarian cancer. Clin Cancer Res. 2010;16(21):5320–8. doi: 10.1158/1078-0432.CCR-10-0974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bull Phelps SL, Schorge JO, Peyton MJ, Shigematsu H, Xiang LL, Miller DS, et al. Implications of EGFR inhibition in ovarian cancer cell proliferation. Gynecol Oncol. 2008;109(3):411–7. doi: 10.1016/j.ygyno.2008.02.030. [DOI] [PubMed] [Google Scholar]
- 13.Tanaka K, Babic I, Nathanson D, Akhavan D, Guo D, Gini B, et al. Oncogenic EGFR signaling activates an mTORC2-NF-kappaB pathway that promotes chemotherapy resistance. Cancer Discov. 2011;1(6):524–38. doi: 10.1158/2159-8290.CD-11-0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Noske A, Schwabe M, Weichert W, Darb-Esfahani S, Buckendahl AC, Sehouli J, et al. An intracellular targeted antibody detects EGFR as an independent prognostic factor in ovarian carcinomas. BMC Cancer. 2011;11:294. doi: 10.1186/1471-2407-11-294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Landen CJ, Birrer MJ, Sood AK. Early events in the pathogenesis of epithelial ovarian cancer. J Clin Oncol. 2008;26(6):995–1005. doi: 10.1200/JCO.2006.07.9970. [DOI] [PubMed] [Google Scholar]
- 16.Grazio D, Pichler I, Fuchsberger C, Zolezzi F, Guarnieri P, Heidegger H, et al. Differential gene expression analysis of ovarian cancer in a population isolate. Eur J Gynaecol Oncol. 2008;29(4):357–63. [PubMed] [Google Scholar]
- 17.Serov SF, Scully RE, Sobin LH. Histological typing of ovarian tumours. Geneva : World Health Organization; 1973. [Google Scholar]
- 18.Yao G, He P, Chen L, Hu X, Gu F, Ye C. MT1-MMP in breast cancer: induction of VEGF-C correlates with metastasis and poor prognosis. Cancer Cell Int. 2013;13(1):98. doi: 10.1186/1475-2867-13-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen J, Zhou SJ, Zhang Y, Zhang GQ, Zha TZ, Feng YZ, et al. Clinicopathological and prognostic significance of galectin-1 and vascular endothelial growth factor expression in gastric cancer. World J Gastroenterol. 2013;19(13):2073–9. doi: 10.3748/wjg.v19.i13.2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Skirnisdottir I, Seidal T, Sorbe B. A new prognostic model comprising p53, EGFR, and tumor grade in early stage epithelial ovarian carcinoma and avoiding the problem of inaccurate surgical staging. Int J Gynecol Cancer. 2004;14(2):259–70. doi: 10.1111/j.1048-891X.2004.014209.x. [DOI] [PubMed] [Google Scholar]
- 21.Roskoski RJ. Vascular endothelial growth factor (VEGF) signaling in tumor progression. Crit Rev Oncol Hematol. 2007;62(3):179–213. doi: 10.1016/j.critrevonc.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 22.Shen GH, Ghazizadeh M, Kawanami O, Shimizu H, Jin E, Araki T, et al. Prognostic significance of vascular endothelial growth factor expression in human ovarian carcinoma. Br J Cancer. 2000;83(2):196–203. doi: 10.1054/bjoc.2000.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raspollini MR, Amunni G, Villanucci A, Baroni G, Boddi V, Taddei GL. Prognostic significance of microvessel density and vascular endothelial growth factor expression in advanced ovarian serous carcinoma. Int J Gynecol Cancer. 2004;14(5):815–23. doi: 10.1111/j.1048-891X.2004.014514.x. [DOI] [PubMed] [Google Scholar]
- 24.Brustmann H, Naude S. Vascular endothelial growth factor expression in serous ovarian carcinoma: relationship with high mitotic activity and high FIGO stage. Gynecol Oncol. 2002;84(1):47–52. doi: 10.1006/gyno.2001.6467. [DOI] [PubMed] [Google Scholar]
- 25.Sonmezer M, Gungor M, Ensari A, Ortac F. Prognostic significance of tumor angiogenesis in epithelial ovarian cancer: in association with transforming growth factor beta and vascular endothelial growth factor. Int J Gynecol Cancer. 2004;14(1):82–8. doi: 10.1111/j.1048-891x.2004.14202.x. [DOI] [PubMed] [Google Scholar]
- 26.Duncan TJ, Al-Attar A, Rolland P, Scott IV, Deen S, Liu DT, et al. Vascular endothelial growth factor expression in ovarian cancer: a model for targeted use of novel therapies? Clin Cancer Res. 2008;14(10):3030–5. doi: 10.1158/1078-0432.CCR-07-1888. [DOI] [PubMed] [Google Scholar]
- 27.Siddiqui GK, Elmasry K, Wong Te Fong AC, Perrett C, Morris R, Crow JC, et al. Prognostic significance of intratumoral vascular endothelial growth factor as a marker of tumour angiogenesis in epithelial ovarian cancer. Eur J Gynaecol Oncol. 2010;31(2):156–9. [PubMed] [Google Scholar]
- 28.Comsa S, Cоmpean M, Ceauşu R, Suciu C, Raica M. Correlations between vascular endothelial growth factor expression, microvascular density in tumor tissues and TNM staging in breast cancer. Archives of Biological Sciences. 2012;64(2):409–17. doi: 10.2298/abs1202409c. [DOI] [Google Scholar]
- 29.Clatworthy MR, Sivaprakasam R, Butler AJ, Watson CJ. Subcutaneous administration of alemtuzumab in simultaneous pancreas-kidney transplantation. Transplantation. 2007;84(12):1563–7. doi: 10.1097/01.tp.0000295718.55669.3a. [DOI] [PubMed] [Google Scholar]
- 30.Paley PJ, Staskus KA, Gebhard K, Mohanraj D, Twiggs LB, Carson LF, et al. Vascular endothelial growth factor expression in early stage ovarian carcinoma. Cancer. 1997;80(1):98–106. doi: 10.1002/(sici)1097-0142(19970701)80:1<98::aid-cncr13>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 31.Yu L, Deng L, Li J, Zhang Y, Hu L. The prognostic value of vascular endothelial growth factor in ovarian cancer: a systematic review and meta-analysis. Gynecol Oncol. 2013;128(2):391–6. doi: 10.1016/j.ygyno.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 32.Huang CW, Tsai HL, Chen YT, Huang CM, Ma CJ, Lu CY, et al. The prognostic values of EGFR expression and KRAS mutation in patients with synchronous or metachronous metastatic colorectal cancer. BMC Cancer. 2013;13:599. doi: 10.1186/1471-2407-13-599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsutsui S, Kataoka A, Ohno S, Murakami S, Kinoshita J, Hachitanda Y. Prognostic and predictive value of epidermal growth factor receptor in recurrent breast cancer. Clin Cancer Res. 2002;8(11):3454–60. [PubMed] [Google Scholar]
- 34.Galizia G, Lieto E, Orditura M, Castellano P, Mura AL, Imperatore V, et al. Epidermal growth factor receptor (EGFR) expression is associated with a worse prognosis in gastric cancer patients undergoing curative surgery. World J Surg. 2007;31(7):1458–68. doi: 10.1007/s00268-007-9016-4. [DOI] [PubMed] [Google Scholar]
- 35.Dziadziuszko R, Jassem J. Epidermal growth factor receptor (EGFR) inhibitors and derived treatments. Ann Oncol. 2012;23(suppl 10):193–6. doi: 10.1093/annonc/mds351. [DOI] [PubMed] [Google Scholar]
- 36.Brustmann H. Epidermal growth factor receptor expression in serous ovarian carcinoma: an immunohistochemical study with galectin-3 and cyclin D1 and outcome. Int J Gynecol Pathol. 2008;27(3):380–9. doi: 10.1097/PGP.0b013e31815d060d. [DOI] [PubMed] [Google Scholar]
- 37.Psyrri A, Kassar M, Yu Z, Bamias A, Weinberger PM, Markakis S, et al. Effect of epidermal growth factor receptor expression level on survival in patients with epithelial ovarian cancer. Clin Cancer Res. 2005;11(24 Pt 1):8637–43. doi: 10.1158/1078-0432.CCR-05-1436. [DOI] [PubMed] [Google Scholar]
- 38.Elie C, Geay JF, Morcos M, Le Tourneau A, Girre V, Broet P, et al. Lack of relationship between EGFR-1 immunohistochemical expression and prognosis in a multicentre clinical trial of 93 patients with advanced primary ovarian epithelial cancer (GINECO group). Br J Cancer. 2004;91(3):470–5. doi: 10.1038/sj.bjc.6601961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lassus H, Sihto H, Leminen A, Joensuu H, Isola J, Nupponen NN, et al. Gene amplification, mutation, and protein expression of EGFR and mutations of ERBB2 in serous ovarian carcinoma. J Mol Med (Berl). 2006;84(8):671–81. doi: 10.1007/s00109-006-0054-4. [DOI] [PubMed] [Google Scholar]
- 40.Stadlmann S, Gueth U, Reiser U, Diener PA, Zeimet AG, Wight E, et al. Epithelial growth factor receptor status in primary and recurrent ovarian cancer. Modern Pathol. 2006;19(4):607–10. doi: 10.1038/modpathol.3800575. [DOI] [PubMed] [Google Scholar]
- 41.Tanaka Y, Terai Y, Tanabe A, Sasaki H, Sekijima T, Fujiwara S, et al. Prognostic effect of epidermal growth factor receptor gene mutations and the aberrant phosphorylation of Akt and ERK in ovarian cancer. Cancer Biol Ther. 2011;11(1):50–7. doi: 10.4161/cbt.11.1.13877. [DOI] [PMC free article] [PubMed] [Google Scholar]