Abstract
Background
Fetal death certificates (FDC) are the main source of stillbirth surveillance data in the United States yet previous studies suggest FDC have incomplete ascertainment. In 2005, Centers for Disease Control and Prevention (CDC) funded two pilot programs to determine the feasibility of expanding existing birth defects surveillance systems employing active case finding methods to conduct surveillance of stillbirths. The objectives of this analysis were to: 1) estimate the completeness of ascertainment of stillbirths identified through one of the pilot programs, the Metropolitan Atlanta Congenital Defects Program (MACDP), and 2) compare the prevalence of stillbirths obtained through active case finding (MACDP) with data available from FDC.
Methods
Stillbirths in metropolitan Atlanta were independently ascertained by both FDC and MACDP in 2006 and 2008. Capture-recapture methods were used to estimate the total number of stillbirths in the surveillance area. The sensitivities for capturing stillbirths were estimated for FDC, MACDP, and both sources combined. Prevalence estimates for each data source and for the combined data sources were calculated using a denominator of live births plus FDC-identified stillbirths.
Results
An estimated 1,118 stillbirths occurred in metropolitan Atlanta. MACDP captured 863 and FDC captured 862. There were 198 stillbirths captured by MACDP and not reported by FDC, and 197 stillbirths identified in FDC were not initially captured by MACDP. The estimated sensitivities were 77.1%, 77.2%, and 94.8% for FDC, MACDP, and both sources combined, respectively. The stillbirth prevalences for 2006 and 2008 using FDC data alone were 8.2 and 7.4 per 1,000 live births plus stillbirths, respectively, and 9.9 and 9.3 per 1,000 live births plus stillbirths, respectively using both data sources combined.
Conclusions
Leveraging the resources of existing birth defects surveillance programs in combination with FDC could improve population-based ascertainment of stillbirths.
Keywords: birth defects, sensitivity, stillbirth, surveillance, prevalence
Introduction
Stillbirth is an important public health concern. Despite improvements in prenatal and perinatal care in recent decades, stillbirth occurs in approximately 1 out of every 200 pregnancies and has a tremendous emotional and psychological impact upon families. 1, 2
Although reporting requirements vary, stillbirth is a reportable event in all 50 states and U.S. territories. Data on stillbirths are regularly collected, analyzed and reported by the National Center for Health Statistics (NCHS) through collaborative agreements with states as part of the National Vital Statistics System.3 Based on these data provided to NCHS, in 2005 the prevalence of stillbirths in the United States was 6.22 per 1,000 live births plus stillbirths.4 The use of vital records for surveillance purposes, however, has been problematic.5–8 The American College of Obstetricians and Gynecologists (ACOG) has published recommended guidelines for conducting postmortem stillbirth evaluations.9 However, several studies have shown that data on fetal death certificates (FDC) not only yield inaccurate and incomplete information with respect to certain variables such as maternal health conditions, presence of a birth defect, and causes of death, but they also potentially underestimate the true prevalence of this event. 10–15 Without reliable population-based data, the conduct of epidemiologic studies of risk factors and causes of stillbirth are challenging.
In 2005, the Centers for Disease Control and Prevention (CDC) funded two pilot projects – one in Iowa and one in metropolitan Atlanta, to assess the feasibility of expanding existing population-based birth defects surveillance programs to include surveillance of stillbirths with or without birth defects. The hypothesis was that using the infrastructure of established birth defects surveillance programs employing active case finding methods to collect, analyze and report data on stillbirths could enhance existing surveillance information on stillbirths. These enhancements would need to demonstrate improvements not only in the quantity and quality of information collected, but also completeness of case ascertainment. In 2008, Duke and colleagues evaluated a revised data collection tool for use in the surveillance of stillbirths as part of the Metropolitan Atlanta Congenital Defects Program (MACDP).10 After linking MACDP-identified stillbirths with FDC, the analysis demonstrated that overall there was less missing information for critical variables, such as birth weight and fetal sex, compared with corresponding information on FDC. Also, the amount and quality of clinical and pathological information abstracted from the medical record through MACDP surveillance was improved and could potentially allow for a better understanding of the contributing factors associated with the fetal death. The current paper reports the results of a follow-up study; the objectives were to evaluate the completeness of case ascertainment and compare prevalence of stillbirths identified through MACDP, FDC, and both data sources combined for the years 2006 and 2008.
Methods
Pregnancy Outcome Determination
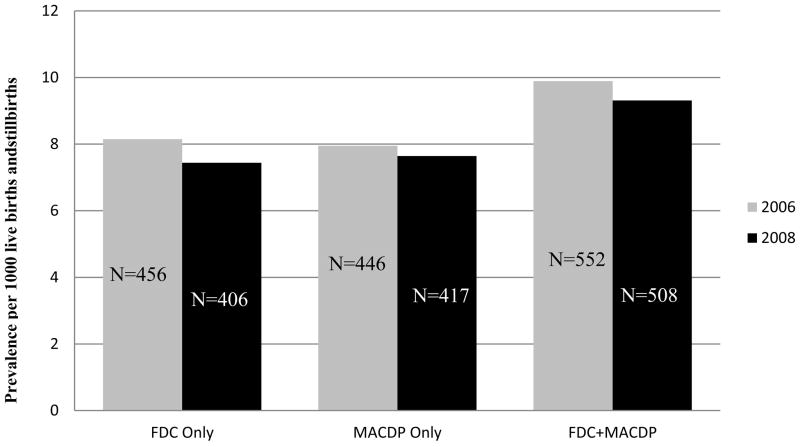
Pregnancy outcome classification was based on the definitions for live birth, fetal death and induced termination of pregnancy provided by the 1992 Revision of the Model State Vital Statistics Act and Regulation (Model Law, page 2).3 There is no universally accepted definition of stillbirth that includes the criteria for gestational age or birth weight. For surveillance purposes, stillbirth was defined by MACDP as a fetal death occurring at 20 or more weeks of gestation or 350 or more grams if the gestational age is not known. The gestational age used was the age of the fetus as indicated by the physician in the medical record. Lastly, the Model Law defines an induced termination of pregnancy as “…the purposeful interruption of an intrauterine pregnancy with the intention other than to produce a live born infant and which does not result in a live birth and…excludes management of prolonged retention of products of conception following fetal death.” While fetal heart tones may be present and documented in the medical record prior to the induction of labor, the ‘intention’ is not always clear; therefore, assessing misreporting of these outcomes as fetal deaths is problematic. For MACDP stillbirth surveillance purposes these cases are ascertained and reported as stillbirths resulting from medical intervention along with the indication for induction of labor (Figure 1).
Figure 1.
Schematic used by MACDP for case classification of outcome
MACDP: Metropolitan Atlanta Congenital Defects Program U/S: Ultrasound IUFD: Intrauterine fetal death FHTs: Fetal heart tones HR: Heart rate
Case Ascertainment
Stillbirths were independently ascertained though FDC provided by the state of Georgia and MACDP. Georgia requires all fetal deaths to be reported if brought to the attention of a healthcare provider; more information on fetal death registration requirements in Georgia can be found in Chapter 31 of the Official Code of Georgia (O.C.G.A § 31-10-18). Prior to 2006, MACDP received FDC on an ongoing basis as one data source for ascertainment of birth defects; however, due to an administrative lapse, FDC for 2006 and later were not obtained until late 2009, allowing for the independence of sources in case finding for the current assessment. A complete file of FDC for 2007 was never obtained, necessitating the exclusion of that year from this analysis.
MACDP is a population-based active surveillance system ascertaining structural and chromosomal anomalies among pregnancies resulting in a live birth, stillbirth or termination. Trained medical records abstractors visit area birthing hospitals, pediatric hospitals and other clinical providers including prenatal diagnostic centers and genetics clinics located in the five central counties of metropolitan Atlanta to identify and abstract information on potential cases. In 1994, MACDP abstractors began to visit the outpatient offices of area perinatologists and maternal–fetal medicine specialists to abstract information about pregnancies diagnosed prenatally with congenital abnormalities.16 Clinical reviewers review each potential case and determine eligibility for inclusion in the surveillance system and code the birth defects. MACDP methods for birth defects surveillance have been previously described.17, 18 In 2006, after minor revisions to the data collection tool and surveillance methods, MACDP began active surveillance for all stillbirths, with or without birth defects. The sources for active ascertainment of stillbirths by MACDP largely overlapped with the sources for birth defects ascertainment but included a few additional sources such as emergency department records, and autopsy and placental histopathology reports. In addition, mothers diagnosed with an intrauterine fetal death at 20 or more weeks of gestation in the specialty clinics previously mentioned were also ascertained with follow-up attempted at the delivering hospital. Stillbirths which occur without any resulting contact with a health care provider (e.g. no emergency department visit, hospitalization or visit to selected Atlanta-area prenatal care providers) are not able to be ascertained by MACDP. Furthermore, MACDP does not have access to abortion clinic records and any stillbirths or terminations occurring at such facilities would be missed.
Live birth certificates and FDC for 2006 and 2008 were obtained from two departments within the Georgia Department of Public Health. In 2006, data came from the Office of Health Indicators for Planning and in 2008 from the Office of Vital Statistics. The records of stillbirths identified through MACDP were linked to FDC for the same birth cohorts (2006 and 2008) by means of a deterministic matching process with multiple iterations using the following variables: mother’s name and race, father’s name, gender of fetus, date of event, hospital, county of residence, and mother’s address at the time of delivery. Manual matches were also attempted for stillbirths that did not link. For those stillbirths in the FDC that did not link to a stillbirth in MACDP, abstractors were asked to locate the medical records for those stillbirths and abstract the relevant information if the mother was a resident of the five-county surveillance area.
Data Analysis
To evaluate the total number of stillbirths occurring among the surveillance population and the relative contribution of each data source for case finding (active surveillance through MACDP; passive surveillance through FDC), capture-recapture methods were used.6, 19, 20 Briefly, this method can be used to estimate total prevalence and to evaluate the relative contribution of independent case sources. The number of stillbirths missed by both sources was estimated by the product of the number missed by each source, divided by the number identified by both sources. These stillbirths missed by both sources were then added to the total number identified by either source to estimate the total prevalence. The prevalence of stillbirths was then calculated by each data source alone as well as for both data sources combined. Estimates were also calculated including and excluding stillbirths resulting from induction of labor as a medical intervention. The denominator for all prevalence estimates included live births plus stillbirths from vital records restricted to the five-county area as recorded in vital records. Using a normal approximation, 95% confidence intervals were calculated for all estimates of prevalence, as well as for the sensitivities and specificities of each data source alone and the data sources in combination.
Results
In 2006 and 2008 there were 2,252 stillbirths reported in the state with just under half of these occurring among mothers residing in the 5-county metropolitan Atlanta area (Table 1). Because Georgia law requires that all fetal deaths be reported regardless of gestational age if brought to the attention of a healthcare provider, the majority of fetal deaths in Georgia are losses before 20 weeks of gestation (Table 1). The year 2008 had substantially more fetal deaths with a missing gestational age than the year 2006 because of differences in data sources from the state. The data from 2006 from the Office of Health Indicators for Planning had missing clinical estimates of gestational age recoded as the gestational age based on the last menstrual period, if available. The data from 2008 were the raw vital statistics data that did not undergo this assignment process.
Table 1.
Fetal deaths reported by gestational age, Georgia and metropolitan Atlanta, 2006 and 2008
| Georgia | Metropolitan Atlanta | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| 2006 | 2008 | 2006 | 2008 | |||||
|
| ||||||||
| Gestational age | N | % | N | % | N | % | N | % |
| < 20 weeks* | 6894 | 71.9 | 5061 | 62.1 | 3159 | 78.2 | 2208 | 65.1 |
| ≥ 20 weeks | 1141 | 12.6 | 1111 | 13.4 | 474 | 11.7 | 459 | 13.5 |
| 20–27 weeks | 722 | 4.6 | 652 | 7.9 | 305 | 7.6 | 279 | 8.2 |
| 28 + weeks | 419 | 6.8 | 459 | 5.5 | 169 | 4.2 | 180 | 5.3 |
| Missing | 985 | 2.5 | 2092 | 25.3 | 405 | 10.0 | 724 | 21.4 |
|
| ||||||||
| Total | 9020 | 100 | 8264 | 100 | 4038 | 100 | 3391 | 100 |
Fetal deaths before 20 weeks of gestation, also known as miscarriages or early fetal losses, were not considered in this analysis
2006 data were from Georgia Department of Public Health, Office of Health Indicators for Planning
2008 data were from Georgia Department of Public Health, State Office of Vital Records
MACDP captured 863 stillbirths and FDC captured 862. Of these, 665 stillbirths were independently captured by both sources (Table 2). MACDP captured an additional 198 stillbirths for which no FDC could be found. Similarly, a total of 197 stillbirths were identified based soley on the FDC for case finding (Table 2). These cases would have been missed if FDC had not been available for retrospective case finding and abstraction. Using capture-recapture methods, 58 stillbirths were estimated as missed by both sources [(198 x 197)/665 = 58], resulting in 1118 total stillbirths (95% confidence interval [CI]: 1052, 1183) in metropolitan Atlanta during 2006 and 2008. The estimated sensitivities for capturing a stillbirth were 77.1% (95% CI: 74.7%, 79.7%) for FDC alone, 77.1% (95% CI: 74.7%, 79.7%) for MACDP alone and 94.8% (95% CI: 93.5%, 96.1%) for both sources combined. Of the 197 stillbirths identified solely through FDC, medical records were sought but not found for 30 of them, and 26 additional stillbirths occurred among mothers who resided within the catchment area, but delivered in a facility outside of it. The medical records for these 26 stillbirths were not sought by MACDP.
Table 2.
Distribution of stillbirths by source of identification and estimated total stillbirths in metropolitan Atlanta, 2006 and 2008
| Identified by MACDP | Total | |||
|---|---|---|---|---|
| Yes | No | |||
| Identified by | Yes | 665 | 197 * | 862 |
| FDC | No | 198 | (58) ** | 256 |
|
| ||||
| Total | 863 | 255 | (1118) | |
MACDP, Metropolitan Atlanta Congenital Defects Program; FDC, fetal death certificates
Includes 30 stillbirths for which no medical record could be found and 26 that were delivered in a county outside MACDP catchment area
Stillbirths missed by both sources
Furthermore, MACDP captured 61 stillbirths for which induction of labor was performed due to the fetus being affected by a birth defect. Of these, 31 linked to FDC and 30 could not be linked. MACDP ascertained another 49 stillbirths for which induction of labor was performed secondary to a pregnancy complication such as pre-eclampsia, premature rupture of membranes, or chorioamnionitis. Thirty-seven of these were issued a FDC and 12 did not link (Table 3). The 30 cases for which the medical record could not be found and the 26 cases that were delivered outside the catchment area are not included in the assessment of ascertainment by pregnancy outcome reported in Table 3.
Table 3.
Distribution of stillbirths by pregnancy outcome, initial source of identification, and linkage status, metropolitan Atlanta, 2006 and 2008
| Pregnancy Outcome | Linked | Did Not Link | Total | ||
|---|---|---|---|---|---|
| Identified by MACDP | Identified by FDC | Identified by MACDP | Identified by FDC | ||
| Stillbirth with birth defect | 82 | 4 | 17 | 0 | 103 |
| Stillbirth without birth defect | 520 | 130 | 139 | 2 | 791 |
| Stillbirth due to induction of labor for birth defect | 31 | 0 | 30 | 0 | 61 |
| Stillbirth due to induction of labor for other pregnancy complication* | 32 | 5 | 12 | 0 | 49 |
|
| |||||
| Total | 665 | 139 | 198 | 2 | 1004** |
MACDP, Metropolitan Atlanta Congenital Defects Program; FDC, fetal death certificates
Complications such as chorioamnionitis, premature rupture of membranes, and pre-eclampsia
Does not include 30 stillbirths for which no medical record could be found and 26 that delivered in a county outside MACDP catchment area
Lastly, there were an additional 114 stillbirths identified through FDC with a gestational age of 20 or more weeks that were subsequently excluded after reviewing the medical record. The reasons for excluding these cases are listed in Table 4. Forty-five cases were excluded after review of the medical record clearly indicated that the death occurred before 20 weeks of gestation. Thirty-four cases were singleton stillbirths for which 2 identical FDC were generated. Twenty cases had medical record documentation that the fetus was born alive and expired shortly after birth. Another 13 cases were excluded because the mother did not reside in the surveillance catchment area and 2 cases had the wrong year of birth on the FDC.
Table 4.
Reasons for excluding stillbirths identified through fetal death certificiates as occurring at 20 or more weeks of gestation, metropolitan Atlanta, 2006 and 2008
| Reason for Exclusion | N | (%) |
|---|---|---|
| Medical record indicated less than 20 weeks* | 45 | (39.5) |
| Duplicate FDC | 34 | (29.8) |
| Live birth | 20 | (17.5) |
| Non-resident** | 13 | (11.4) |
| Wrong year of FDC | 2 | (1.8) |
| Total | 114 | (100.0) |
FDC, fetal death certificates
Medical record review clearly indicated the death occurred prior to 20 weeks of gestation indicating that the death was misclassified as a death occurring at less than 20 weeks on the FDC.
Medical records documented these mothers as not residing in the metropolitan-Atlanta surveillance catchment area
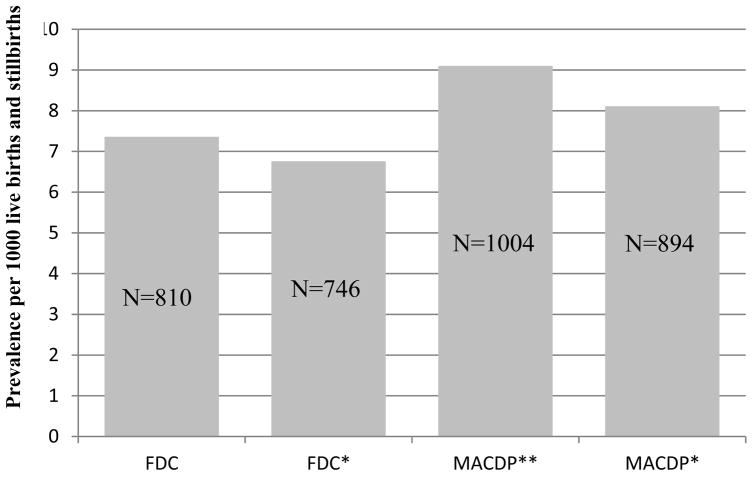
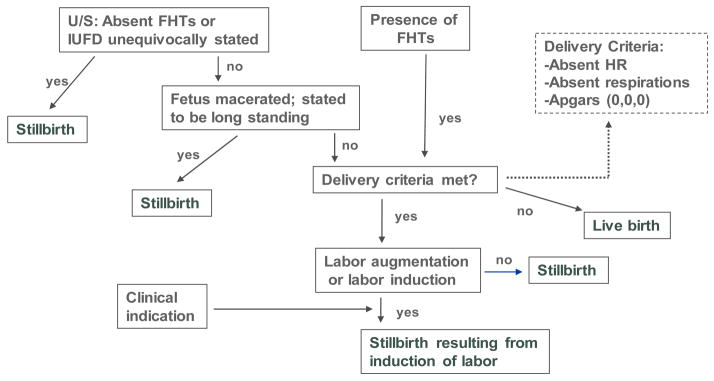
There were 55,707 and 54,581 live births and stillbirths (the stillbirths in the denominator were based on the number ascertained by FDC) delivered in the metropolitan Atlanta surveillance area in 2006 and 2008 respectively. Using only those stillbirths identified from FDC, the prevalence of stillbirth was 8.2 per 1,000 live births plus stillbirths in 2006 (95% CI: 7.4, 8.9) and 7.4 per 1,000 live births plus stillbirths in 2008 (95% CI: 6.7, 8.2). Using only ascertainment by MACDP, the estimates were 8.0 and 7.6 per 1,000 live births plus stillbirths (95% CIs: 7.3, 8.7 and 6.9, 8.4), respectively. Using both sources for ascertainment yielded estimates of 9.9 and 9.3 per 1,000 live births plus stillbirths (95% CIs: 8.1, 10.7 and 8.5, 10.1), respectively (Figure 2). Prevalence estimates were compared including and excluding stillbirths occurring after induction of labor as a medical intervention (Figure 3). Excluding stillbirths occurring after induction of labor naturally reduced the prevalence; we observed a greater reduction for MACDP identified stillbirths than FDC identified stillbirths.
Figure 2.
Prevalence of stillbirths by data source, metropolitan Atlanta, 2006 and 2008
FDC: Fetal death certificates
MACDP: Metropolitan Atlanta Congenital Defects Program
Figure 3.
Prevalence of stillbirths with and without those resulting from induction of labor, metropolitan Atlanta, 2006 and 2008
*Excludes stillbirths occurring after induction of labor
** MACDP numerator includes stillbirths identified through FDC and linked (n=139)
FDC: Fetal death certificates
MACDP: Metropolitan Atlanta Congenital Defects Program
Discussion
The use of FDC alone for population-based surveillance of stillbirths is limited and uncertainty about the utility of FDC data for risk factor analysis has been previously noted. 7, 10–12 Complete and reliable surveillance data is needed if hypothesis-driven epidemiologic studies are to be conducted. The current study demonstrated that expanding the capabilities of an existing birth defect surveillance system to include active ascertainment of stillbirths and combining that information with what is gathered from FDC, is feasible and results in the ascertainment of cases that would have otherwise been missed by either system alone. Expanding MACDP to include surveillance of stillbirths required a few modifications to the birth defects surveillance protocol, such as accessing emergency department records (to capture cases arriving as an emergency and potentially getting discharged without hospital admission), and autopsy and placental histopathology information. There was no additional staff required to implement stillbirth surveillance as sources for case finding overlapped with sources already used for birth defects surveillance and were already being reviewed by clinical abstractors.
Each data source – FDC and MACDP – has limitations. The current analysis, as well as previous studies, indicate that FDC underreport stillbirths, as well as often misreport the pregnancy outcome and contain large amounts of missing information for critical variables such as gestational age, birth weight, and the cause of death. 10, 18 With respect to cause of death, this may in part be explained by the fact that the majority of FDC are completed before all post-mortem evaluation information is available. 21 For MACDP, our analyses suggest that a large number of stillbirths would have been missed if not for the availability of FDC as a source for case finding. Routine precedures for MACDP normally involve obtaining FDC on a monthly basis, from which stillbirths can be identified on an ongoing basis. This was not the case for our study years, allowing for the application of capture-recapture methods to estimate the number of stillbirths occurring in the surveillance population. Active ascertainment by MACDP was only able to collect what was available from the medical record. However, when both MACDP and FDC were used together, they ascertained more stillbirths than either system captured independently. The factors influencing case ascertainment within each data source are not clear. The underascertainment of stillbirths is not likely a random event; it may be associated with factors such as maternal race/ethnicity, gestational age, delivery facility or the cause of death, or perhaps factors that are not even recorded. More analyses need to be undertaken to better understand the role that these factors may play in the ascertainment of stillbirths. This could provide potentially valuable information to inform training needs and strategies to improve the reporting process.
Active case finding of stillbirths has several strengths. Trained abstractors visit area hospitals, locate medical records for potential cases, and record the relevant information. The abstracted information for each potential stillbirth is systematically reviewed by one or more MACDP clinicians to ensure that inclusion criteria are met and to designate the appropriate outcome classification. Previous studies by Duke and colleagues, using data from MACDP, have demonstrated that active ascertainment and medical chart review improves upon the quantity and quality of the data collected. 10, 22 In addition, the in-depth medical record review resulted in more accurate classification of pregnancy outcomes, which provided insight into the potential misclassification of pregnancy outcomes by FDC. This information is important to better understand stillbirth prevalence estimates that are based on FDC alone. Active ascertainment can allow for the inclusion or exclusion of stillbirths resulting from the medical induction of labor or stillbirths that were actually live births. As shown in Table 3, about 50% of the inductions performed for a fetus affected by a birth defect linked to a FDC, whereas about 75% of those inductions performed for other pregnancy complications were issued a FDC. It is not possible to know if the cases that did not link were issued an Induced Termination of Pregnancy (ITOP) certificate, data for which are deidentified and unlinkable with information from other sources. Anectdotally the majority of inductions performed in the setting of a fetus affected by a birth defect are done subsequent to the administration of intrauterine potassium chloride, and identifying these events through the review of medical records is relatively straightforward. Therefore, from a surveillance perspective, the intent of the procedure is apparent, and ITOP certificate should have been issued. However many of these birth defects can be considered lethal anomalies and should be considered when understanding fetal mortality rates. On the other hand, inductions performed in the context of other clinical scenarios, such as severe chorioamnionitis, are most often conducted in the best medical interest of the mother and the intent may very well have been to produce a live birth. It is likely that these clinical situations explain the differences in whether a FDC was issued or not. Active case finding allows for these events to be captured and documented based on the thorough review of medical records, potentially improving our understanding of the impact of these events on estimates of the prevalence of stillbirths. These distinctions cannot be made when using FDC data alone.
We capitalized on a lapse of availability of FDC to MACDP for case ascertainment. Having two independent data sources for stillbirth ascertainment allowed us to conduct a capture-recapture analysis to estimate the total number of stillbirths occurring within metropolitan Atlanta – and the number potentially missed by the two data sources working independently. This normally cannot be done when FDC are obtained and used on an ongoing basis as a source for case finding.
This analysis is subject to several limitations, however. First, we were limited to only two years of data; a similar analysis is planned for stillbirths occurring in 2009 and later. Second, we did not assess or compare data quality between sources - an important next step to further demonstrate the utility of this approach to stillbirth surveillance. Third, it was not possible or practical to capture every fetal death. Stillbirths that occurred to mothers residing in metropolitan Atlanta but delivering outside the catchment area were missed by MACDP and were therefore not subjected to medical chart review. However, they could be identified if issued a FDC and were included in the analysis as shown in Table 2. Similarly, medical records for terminations and stillbirths delivered at abortion clinics are not accessible by MACDP. Lastly, it is not clear why such a large number of medical records could not be located (n=30). This may reflect inadequate staffing and resources to conduct an exhaustive search for the medical record as many healthcare facilities store medical records off-site after a certain length of time.
Fetal death reporting by states to the National Vital Statistics System is and will remain the core infrastructure for stillbirth surveillance in the United States; however, expanding existing birth defects surveillance programs to include active ascertainment of stillbirth is potentially a valuable approach to help address our current knowledge gaps about the frequency and risk factors for stillbirths. More importantly, improvements to surveillance data on stillbirths will require multidisciplinary efforts to increase and standardize the use of ACOG recommended clinical guidelines for postmortem stillbirth evaluation.
Footnotes
CDC Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Contributor Information
Wes Duke, Email: CJI7@cdc.gov, Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities, Division of Birth Defects and Developmental Disabilities, Mail Stop E-86, Atlanta, GA 30333.
Suzanne M. Gilboa, Email: SUZ0@cdc.gov, Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities, Division of Birth Defects and Developmental Disabilities.
References
- 1.American College of Obstetricians and Gynecologists. ACOG practice bulletin. Antepartum fetal surveillance. Number 9, October 1999 (replaces Technical Bulletin Number 188, January 1994). Clinical management guidelines for obstetrician-gynecologists. Int J Gynaecol Obstet. 2000;68:175–185. [PubMed] [Google Scholar]
- 2.Cacciatore J, Bushfield S. Stillbirth: the mother's experience and implications for improving care. J Soc Work End Life Palliat Care. 2007;3(3):59–79. doi: 10.1300/J457v03n03_06. [DOI] [PubMed] [Google Scholar]
- 3.Model State Vital Statistics Act and Regulations, 1992 Revision. DHHS Publication No (PHS) 94-11151995.
- 4.MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2009;57(8):1–19. [PubMed] [Google Scholar]
- 5.Duke CW, Correa A, Romitti PA, Martin J, Kirby RS. Challenges and priorities for surveillance of stillbirths: a report on two workshops. Public Health Rep. 2009;124(5):652–659. doi: 10.1177/003335490912400507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Honein MA, Paulozzi LJ. Birth Defects Surveillance: Assessing the “Gold Standard”. American Journal of Public Health. 1999;89(8):1238–1239. doi: 10.2105/ajph.89.8.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martin JA, Hoyert DL. The National Fetal Death File. Semin Perinatol. 2002;26(1):3–11. doi: 10.1053/sper:2002.29834. [DOI] [PubMed] [Google Scholar]
- 8.Northam S, Knapp TR. The reliability and validity of birth certificates. JOGNN. 2006;35(1):3–12. doi: 10.1111/j.1552-6909.2006.00016.x. [DOI] [PubMed] [Google Scholar]
- 9.American College of Obstetricians and Gynecologists. Practice Bulletin No. 102: management of stillbirth. Obstet Gynecol. 2009;113(3):748–761. doi: 10.1097/AOG.0b013e31819e9ee2. [DOI] [PubMed] [Google Scholar]
- 10.Duke W, Williams L, Correa A. Using active birth defects surveillance programs to supplement data on fetal death reports: improving surveillance data on stillbirths. Birth Defects Res A Clin Mol Teratol. 2008;82(11):799–804. doi: 10.1002/bdra.20526. [DOI] [PubMed] [Google Scholar]
- 11.Goldhaber MK. Fetal death ratios in a prospective study compared to state fetal death certificate reporting. AJPH. 1989;79(9):1268–1270. doi: 10.2105/ajph.79.9.1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greb AE, Pauli RM, Kirby R. Accuracy of fetal death reports: Comparison with data from an independent stillbirth assessment program. AJPH. 1987;77(9):1202–1206. doi: 10.2105/ajph.77.9.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lydon-Rochelle MT, Cardenas V, Nelson JL, Tomashek KM, Mueller BA, Easterling TR. Validity of maternal and perinatal risk factors reported on fetal death certificates. Am J Public Health. 2005;95(11):1948–1951. doi: 10.2105/AJPH.2004.044305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heuser CC, Hunn J, Varner M, Hossain S, Vered S, Silver RM. Correlation between stillbirth vital statistics and medical records. Obstetrics and gynecology. 2010;116(6):1296–1301. doi: 10.1097/AOG.0b013e3181fb8838. [DOI] [PubMed] [Google Scholar]
- 15.Gaudino JA, Jr, Blackmore-Prince C, Yip R, Rochat RW. Quality assessment of fetal death records in Georgia: a method for improvement. Am J Public Health. 1997;87(8):1323–1327. doi: 10.2105/ajph.87.8.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cragan JD, Gilboa SM. Including prenatal diagnoses in birth defects monitoring: Experience of the Metropolitan Atlanta Congenital Defects Program. Birth Defects Res A Clin Mol Teratol. 2009;85(1):20–29. doi: 10.1002/bdra.20508. [DOI] [PubMed] [Google Scholar]
- 17.Correa-Villasenor A, Cragan J, Kucik J, O'Leary L, Siffel C, Williams L. The Metropolitan Atlanta Congenital Defects Program: 35 years of birth defects surveillance at the Centers for Disease Control and Prevention. Birth Defects Res A Clin Mol Teratol. 2003;67(9):617–624. doi: 10.1002/bdra.10111. [DOI] [PubMed] [Google Scholar]
- 18.Correa A, Cragan JD, Kucik JE, Alverson CJ, Gilboa SM, Balakrishnan R, et al. Reporting birth defects surveillance data 1968–2003. Birth Defects Res A Clin Mol Teratol. 2007;79(2):65–186. doi: 10.1002/bdra.20350. [DOI] [PubMed] [Google Scholar]
- 19.Capture-recapture and multiple-record systems estimation II: Applications in human diseases. International Working Group for Disease Monitoring and Forecasting. American journal of epidemiology. 1995;142(10):1059–1068. [PubMed] [Google Scholar]
- 20.Capture-recapture and multiple-record systems estimation I: History and theoretical development. International Working Group for Disease Monitoring and Forecasting. American journal of epidemiology. 1995;142(10):1047–1058. [PubMed] [Google Scholar]
- 21.Duke W, Shin M, Correa A, Alverson CJ. Survey of knowledge, attitudes, and practice management patterns of Atlanta-area obstetricians regarding stillbirth. Women's health issues : official publication of the Jacobs Institute of Women's Health. 2010;20(5):366–370. doi: 10.1016/j.whi.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 22.Duke CW, Alverson CJ, Correa A. Fetal death certificates as a source of surveillance data for stillbirths with birth defects. Public Health Rep. 2007;122(5):664–669. doi: 10.1177/003335490712200514. [DOI] [PMC free article] [PubMed] [Google Scholar]