Abstract
Objectives
The purpose of this study was to compare demographic, clinical, and survival characteristics of drug-using safety-net primary care patients who used or did not use opioids, and to examine treatment implications of our findings.
Methods
The sample consisted of 868 adults who reported illicit drug use in the 90 days prior to study enrollment, 396 (45.6%) of whom were opioid users.
Results
Multiple measures indicated that, as a group, opioid users were less physically and psychiatrically healthy than drug users who did not endorse using opioids, and were heavy users of medical services (e.g., emergency departments, inpatient hospitals, outpatient medical) at considerable public expense. After adjusting for age, they were 2.61 (CI, 1.48-4.61) times more likely to die in the 1 to 5 years after study enrollment and more likely to die from accidental poisoning than non-opioid users. Subgroup analyses suggested patients using any non-prescribed opioids had more serious drug problems including more intravenous drug use and greater HIV risk than patients using opioids only as prescribed.
Conclusions
Use of opioids adds a dimension of severity over and above illicit drug use as it presents in the primary care setting. Opioid users may benefit from psychiatric and addiction care integrated into their primary care setting, naloxone overdose prevention kits, and prevention efforts such as clean needle exchanges. Addiction or primary care providers are in a key position to facilitate change among such patients, especially the third or more opioid users having a goal of abstinence from drugs.
Keywords: Opioid use, opiate use, safety-net, primary care, health care utilization and costs
Primary care clinics have become the “medical home” in healthcare reform, especially for inner city populations who present with both multiple medical problems and often co-occurring psychiatric and substance use problems (Chan et al., 2014). In response to this, integrated, collaborative care models for depression and anxiety disorders have been studied, shown effective (Bauer et al., 2014), and begun to be implemented widely. Integrated brief intervention (BI) models for alcohol problems in primary care settings have also been described and shown effective for mild to moderate problems, but not more severe dependence (Bertholet et al., 2005; Kaner et al., 2007; Saitz, 2010, 2014; Williams et al., 2014). Use of psychoactive drugs has been less studied in primary care settings, especially the issues related to opioids which are among the strongest and potentially most addictive and lethal of psychoactive drugs. Opioids have the unique position of being taken as prescribed medications for pain, taken as illegal (non-prescribed) prescription pain medications (e.g., snorting or injecting oxycodone to get high), or taken as illegal drugs (e.g., heroin). Importantly, the number of opioid prescriptions has quintupled in the last 20 years with a related national epidemic of prescription opioid abuse; recently more people have died from accidental prescription opioid overdose than in auto accidents (Warner et al., 2011). To further complicate matters, even when prescription opioids are taken as directed they may be used in conjunction with other drugs such as benzodiazepines which increases the risk of opioid overdose (Jones et al., 2014).
Because most opioids are prescribed in primary care settings (Manchikanti et al., 2012), the focus of this paper is on patients who use either prescribed or non-prescribed opioids and who present for care in a safety-net primary care setting. In this way we deliberately target the focus to a population likely to be encountered by an addiction specialist working in primary care or an opioid specialist working in specialty care. The goal of this paper is to describe drug-related problems in such patients along with their associated demographic, medical, psychiatric and substance use characteristics, as encountered in primary care clinics of an urban, county hospital system.
Methods
Participants
The present study was part of a large randomized clinical trial focused on brief interventions for problem drug use in 7 safety-net primary care clinics (Krupski et al., 2012; Roy-Byrne et al., 2014). Recruitment took place between April 2009 and September 2012 in Seattle, Washington, and included adults 18 years and older who reported using an illegal drug or non-prescribed medication at least once in the 90 days prior to being screened. All participants were English-speaking, able to read and comprehend consent forms, and were currently receiving and planned on continuing to receive care in the clinic from which they were recruited. All had phone or e-mail access to enable the scheduling of follow-up assessments. Since this was a randomized controlled trial of brief intervention for current drug use, patients who were currently in chemical dependency treatment, including opioid substitution treatment, or who attended formal substance abuse treatment in the past month (excluding self-help groups such as Narcotics Anonymous) were excluded from the study. Despite this exclusion criterion, 5 participants noted after randomization that they were, in fact, currently receiving methadone maintenance treatment at baseline. We decided not to exclude these 5 participants in that their exclusion would have no effect on the substantive results and because it allows this paper to be comparable with other published papers utilizing this sample. All enrolled participants received drug problem severity screening results and, at minimum, a list of substance abuse treatment resources. Those who were at imminent risk for suicide or had life-threatening medical illness, severe cognitive impairment, or active psychosis were also excluded. All participants provided written informed consent and received $25 gift cards as compensation. The trial protocol was approved by the University of Washington Institutional Review Boards.
Measures
Self-reported data for all 868 participants was extracted from the surveys administered at baseline. Measures included the DAST-10 (Skinner, 1982), the Addiction Severity Index-Lite (ASI) (Cacciola et al., 2007), the Treatment Services Review (Cacciola et al., 2008), the Thoughts About Abstinence Scale (Hall et al., 1990), the HIV Risk-Taking Behaviour Scale (Darke et al., 1991), the EQ-5D (Euroqol Group, 1990), and standard demographic information. Questions adding detail regarding prescribed versus non-prescribed use of prescription drugs and medical marijuana use was added to the ASI alcohol/drug section.
Data from state chemical dependency treatment records, medical costs and utilization from encounter and billing records maintained by the medical center where the study took place, arrest records from the Washington State Patrol, and death records from the state Department of Health were also available for 848 participants. Chronic conditions for each participant were identified using International Classification of Diseases version 9 (ICD-9) codes from medical records and the Chronic Illness and Disability Payment System (CDPS) (Kronick et al., 2000). Administrative records were available for two years prior to baseline for all measures, one year after study enrollment for chemical dependency records, and up to 5 years after study enrollment for death records.
Death data were obtained for the period 2009 through June 2014, with data from the first 6 months of 2014 being provisional. These records included the underlying cause of death and, in the case of patients who died of an opioid overdose, descriptions of all prescription drugs, illicit drugs, unknown drugs, and alcohol reported on the death certificate. Cause of death was categorized according to International Classification of Diseases version 10 (ICD-10) codes and was classified as 1) external, including accidental poisonings, accidents, and suicide; 2) cancer, cardiovascular; 3) infectious; and 4) chronic liver disease, other. Survival time was calculated as the number of days from date of enrollment to date of death or June 30, 2014 for survivors.
Types of Opioids and Construction of Subgroups
We report three types of opioids: heroin, methadone, and other opioid analgesics (which include all prescription opioids other than methadone). It was beyond the scope of this study to reliably identify quantities used of the three opioid types, or the quantities used of drugs other than opioids.
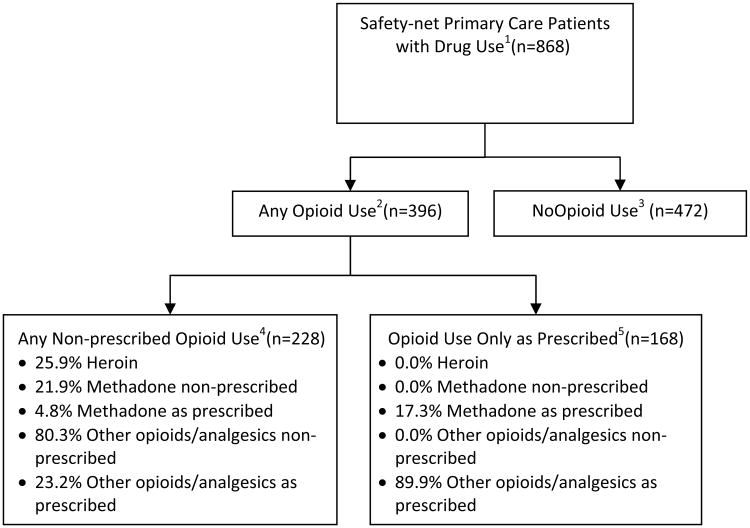
Subgroups are illustrated in Figure 1. All 868 primary care patients enrolled in the larger trial reported use of 1 or more illicit or non-prescribed drugs in the 90 days prior to study enrollment. These patients were sorted into subgroups based on whether they reported any (n=396) or no (n=472) opioid use in the 30 days prior to baseline. Opioid users were further classified into subgroups based on whether they reported any non-prescribed opioid use (n=228) or opioid use only as prescribed (n=168).
Figure 1.
Opioid Use Subgroups.
1Drug use was defined as self-reported use of an illegal drug or non-prescribed medication in the 90 days prior to study enrollment.
2Patients with any opioid use were those who self-reported using opioids one or more days in the past 30 days at baseline.
3Patients with no opioid use were those who did not report using an opioid in the 30 days prior to baseline.
4Patients in the non-prescribed opioid use subgroup included those who reported using heroin, methadone non-prescribed, or other opioid analgesics non-prescribed in the 30 days prior to baseline. Methadone as prescribed was always for pain treatment and not for opioid dependence.
5Patients with opioid use only as prescribed reported using opioids only according to the prescription in the 30 days prior to baseline. Methadone as prescribed was always for pain treatment and not for opioid dependence.
Statistical Analyses
Analyses consisted of two types of comparisons: (1) comparisons between patients who reported any opioid use (prescribed or non-prescribed) and those who reported no opioid use, and (2) among opioid users, comparisons between patients who reported any non-prescribed opioid use and those who reported using opioids only as prescribed. Baseline demographic, medical, psychiatric, substance use, chemical dependency treatment, and other psychosocial characteristics were compared using chi-square tests and t-tests for continuous measures; the same tests were used to compare admission to chemical dependency treatment in the 1 year following study enrollment. Cox proportional hazards regression was used to assess the association between opioid use and age-adjusted survival. Because of multiple comparisons in this analysis, we adopted a more conservative value of <0.01 for significance, in that we view results of analyses presented in this paper as hypothesis-generating rather than hypothesis testing.
Results
Patients with Any Opioid Use vs. Patients with No Opioid Use
Results of all comparisons between patients using any opioids and those not using opioids can be seen in Table 1. This table shows that opioid users as a whole were somewhat older, more likely to be or have been partnered, more likely to have gone beyond high school, and more likely to be unemployed due to disability than patients with problem drug use who reported no opioid use. A higher percentage of patients using opioids had an emergency department visit (67.4% vs 58%; P<0.001) or an inpatient hospital stay (34.7% vs 25.7%; P<0.001) in the two years prior to study enrollment along with almost double the inpatient costs compared to their non-opioid using counterparts ($10,192.70 vs $5,169.03; P=0.004). They also had a higher mean number of outpatient medical visits (21.5 vs 16.8; P<0.001) and higher associated costs ($8,124.86 vs $6,258.45; P=0.003) over the same time period. They had mean EQ-5D scores indicating lower self-reported health status (.64 vs .74; P<0.001), higher (i.e., less healthy) ASI medical composite scores (0.73 vs 0.59; P<0.001), and a higher mean number of CDPS chronic medical comorbidities than their non-opioid using counterparts (8.3 vs 6.7; P<0.001). They were also more likely to have been prescribed medication for psychological/emotional problems in their lifetime (78.0% vs 65.6%; P<0.001) and to have a mental illness diagnosis in their medical records (70.2% vs 58.6%; P<0.001). At baseline, patients using opioids were more likely to be taking 2 or more illicit or non-prescribed drugs in the past 30 days (64.1% vs 28.6%; P<0.001), to have also taken benzodiazepines non-prescribed one or more times in the past 30 days (8.1% vs 2.3%; P<0.001), and/or to have reported intravenous drug use one or more times in the past 30 days (14.0% vs 3.6%; P<0.001).
Table 1. Baseline Characteristics Overall and by Opioid Use (n=868).
| Characteristics | Overall (n=868) | Opioid Usea | ||
|---|---|---|---|---|
| Any Opioid Use (n=396) | No Opioid Use (n=472) | Pb | ||
| Demographics | ||||
| Age, mean in years (SD) | 47.8 (10.9) | 48.9 (10.1) | 46.8 (11.4) | 0.02 |
| Male | 69.6% | 68.2% | 70.8% | 0.41 |
| Racec | ||||
| White | 45.1% | 49.4% | 41.5% | 0.03 |
| Black | 37.4% | 32.9% | 41.1% | |
| Other | 17.5% | 17.7% | 17.3% | |
| Hispanic | 9.2% | 9.4% | 9.0% | 0.83 |
| Marital status | ||||
| Married/living with partner | 18.6% | 21.5% | 16.1% | < 0.001 |
| Divorced/separated/widowed | 40.2% | 43.8% | 37.2% | |
| Never married | 41.2% | 34.7% | 46.7% | |
| Education | ||||
| High school or less | 19.1% | 20.3% | 18.2% | 0.01 |
| High school graduate | 29.3% | 24.3% | 33.5% | |
| Beyond high school | 51.6% | 55.4% | 48.3% | |
| Employment status | ||||
| Working | 9.0% | 7.1% | 10.6% | < 0.001 |
| Unemployed/retired/in school/homemaker/other | 27.5% | 21.7% | 32.3% | |
| Disabled and unable to work | 63.6% | 71.2% | 57.1% | |
| Homeless in shelter or on street ≥1 night in past 3 monthsd | 30.4% | 27.9% | 32.4% | 0.15 |
| Medical | ||||
| Emergency departmente | ||||
| Any (%) | 62.3% | 67.4% | 58.0% | <0.001 |
| Mean visits (SD) | 2.5 (4.3) | 2.8 (4.5) | 2.3 (4.1) | 0.11 |
| Mean cost (SD) | $1,347.69 ($2,436.81) | $1,482.89 ($2,629.51) | $1,233.12 ($2,257.27) | 0.14 |
| Median visits | 1.0 | 1.0 | 1.0 | |
| Median cost | $363.81 | $565.03 | $189.70 | |
| Outpatient medicale | ||||
| Any (%) | 92.0% | 94.1% | 90.2% | 0.04 |
| Mean visits (SD) | 18.9 (18.0) | 21.5 (18.7) | 16.8 (17.1) | <0.001 |
| Mean cost (SD) | $7,114.62 ($8,918.87) | $8,124.86 ($9,599.48) | $6,258.45 ($8,212.24) | 0.003 |
| Median visits | 14.0 | 17.0 | 12.0 | |
| Median cost | $4,563.84 | $5,492.33 | $3,900.91 | |
| Inpatient medicale | ||||
| Any (%) | 29.8% | 34.7% | 25.7% | <0.001 |
| Mean admissions (SD) | 0.5 (1.1) | 0.6 (1.1) | 0.4 (1.0) | 0.02 |
| Mean cost (SD) | $7,473.52 ($24,451.98) | $10,192.70 ($30,250.08) | $5,169.03 ($17,858.05) | 0.004 |
| Median admissions | 0.0 | 0.0 | 0.0 | |
| Median cost | 0.0 | $0.00 | $0.00 | |
| ASI Medical Status composite score, mean (SD)f | 0.65 (0.33) | 0.73 (0.29) | 0.59 (0.35) | <0.001 |
| CDPS medical conditions, mean (SD)e | 7.4 (3.8) | 8.3 (3.5) | 6.7 (3.8) | <0.001 |
| EQ-5D score, mean (SD) | 0.70 (0.21) | 0.64 (0.22) | 0.74 (0.20) | <0.001 |
| EQ-5D Item 4: “I have moderate pain or discomfort” or “I have extreme pain or discomfort” | 78.0% | 86.4% | 71.0% | < 0.001 |
| Psychiatric | ||||
| ≥1 Mental illness ICD-9 diagnosise | 63.9% | 70.2% | 58.6% | < 0.001 |
| Prescribed medication for psychological or emotion problems, lifetime | 71.3% | 78.0% | 65.7% | < 0.001 |
| Substance Use/Treatment | ||||
| ASI days most frequently used drug, mean (SD)g | 13.8 (11.0) | 15.3 (10.95) | 12.6 (10.91) | <0.001 |
| ASI Drug Use composite score, mean (SD)f,g | 0.11 (10.0) | 0.14 (0.11) | 0.09 (0.09) | <0.001 |
| ASI drug use, any in past 30 days h | ||||
| Marijuana | 75.6% | 74.2% | 76.7% | 0.40 |
| Medical Marijuana | 15.1% | 15.4% | 14.9% | 0.83 |
| Stimulants | 41.7% | 45.2% | 38.8% | 0.06 |
| Cocaine | 37.4% | 40.7% | 34.7% | 0.07 |
| Amphetamines | 7.3% | 8.6% | 6.1% | 0.17 |
| Opioids | 45.6% | 100.0% | 0.0% | < 0.001 |
| Heroin | 6.8% | 14.9% | 0.0% | < 0.001 |
| Methadone non-prescribed | 5.8% | 12.6% | 0.0% | < 0.001 |
| Methadone as prescribed | 4.6% | 10.1% | 0.0% | < 0.001 |
| Other opioids/analgesics non-prescribed | 21.1% | 46.2% | 0.0% | < 0.001 |
| Other opioids/analgesics as prescribed | 23.5% | 51.5% | 0.0% | < 0.001 |
| Sedatives/hypnotics/tranquilizers | 8.3% | 12.4% | 4.9% | < 0.001 |
| Benzodiazepinesnon-prescribed | 4.9% | 8.1% | 2.3% | <0.001 |
| Other drugs g, i | 5.9% | 7.6% | 4.4% | 0.05 |
| 2 or more drugs used in past 30 days g, j | 44.8% | 64.1% | 28.6% | < 0.001 |
| Intravenous drug use past 30 days | 8.3% | 14.0% | 3.6% | < 0.001 |
| Goal of total abstinence from drugs g, k | 37.2% | 39.1% | 35.6% | 0.28 |
| DAST-10 drug use severity, mean score (SD)g | 4.26 (2.52) | 4.65 (2.68) | 3.93 (2.34) | <0.001 |
| Low (score 1-2) | 32.0% | 26.0% | 37.1% | <0.001 |
| Intermediate (score 3-5) | 37.8% | 39.6% | 36.2% | |
| Substantial/severe (score ≥ 6) | 30.2% | 34.3% | 26.7% | |
| ASI Alcohol Use composite score, mean (SD)f | 0.15 (0.20) | 0.14 (0.19) | 0.15 (0.21) | 0.43 |
| ASI alcohol use, any in past 30 days | 68.9% | 67.9% | 69.7% | 0.57 |
| Nicotine use, any in past 30 days | 71.6% | 73.7% | 69.8% | 0.20 |
| CD treatment services | ||||
| Admitted to CD treatmente | 17.3% | 18.0% | 16.8% | 0.64 |
| Detoxification (not followed by CD treatment)e | 7.7% | 8.0% | 7.4% | 0.76 |
| Other Psychosocial | ||||
| Arrests for felony or gross misdemeanore | 14.4% | 13.9% | 14.8% | 0.70 |
| HIV Risk-taking Behaviour score, mean (SD) | 3.3 (4.2) | 3.6 (4.5) | 3.1 (3.9) | 0.12 |
| ASI Family/Social composite score, mean (SD)f | 0.17 (0.22) | 0.19 (0.23) | 0.15 (0.20) | 0.02 |
Missing values are not included in this table.
Pvalue based on chi square or ANOVA.
Assessed by self-report using National Institutes of Health reporting categories for federally funded clinical research.
Homeless was defined as spending at least 1 night in the previous 90 either living on the streets, in an abandoned building, in a car, or in a shelter.
Administrative data available for 848 participants for the 2 years prior to enrollment.
ASI composite scores range from 0 to 1, with 1 indicating greatest problem severity.
Excludes use of alcohol or nicotine.
ASI drug use groups reported are not mutually exclusive. The groups reflect illicit or non-prescribed use only unless otherwise indicated.
“Other drugs” can include all other abused medications (e.g., antihistamines, antidepressants) or drugs of abuse (e.g., hallucinogens, inhalants) not included in the existing categories.
Problem drug or non-prescribed medication use only.
From the Thoughts About Abstinence measure which is used to assess one's goal for changing drug use (no goal, controlled use, occasional use, temporary abstinence, total abstinence slip is possible, total abstinence never use again). The reported “goal of total abstinence from drugs” includes “total abstinence, never use again” and “total abstinence, slip is possible.”
ASI, Addiction Severity Index; CD, chemical dependency; CDPS, Chronic Illness and Disability Payment System; DAST-10, Drug Abuse Screening Test 10-item; EQ-5D, Euroqol EQ-5D instrument.
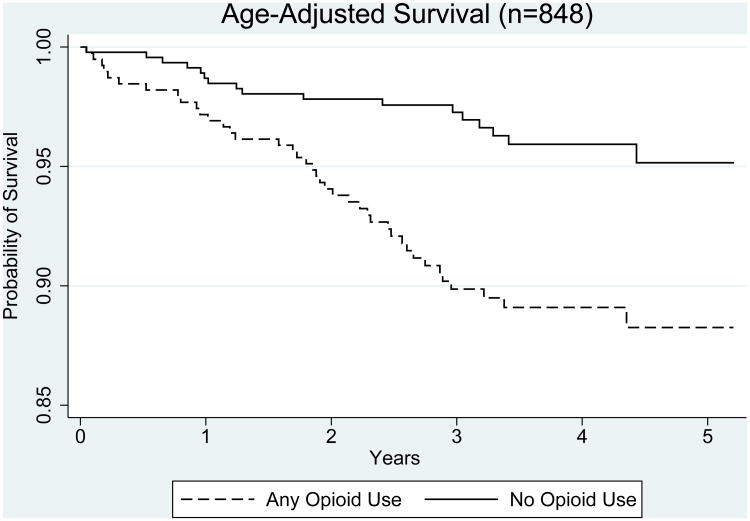
Figure 2 shows survival by opioid use; the overall age-adjusted difference in survival was statistically significant (P=0.003). Compared to patients with problem drug use who did not use opioids, the age-adjusted hazard of death was 2.61 (95% confidence interval, 1.48-4.61) times higher for opioid users. Opioid users (whether non-prescribed or only as prescribed) were more likely to die from external causes, especially accidental poisoning than non-opioid users (Table 2). There were a total of 11 cases of accidental poisoning among opioid users. According to the Department of Health opioid death files, nine were due to opioid overdose: 1 was identified as definitely related to prescription opioids, 1 as possibly related to prescription opioids, and the other 7 as related to other opioids, primarily heroin.
Figure 2.
Age-Adjusted Survival (n=848).
This graph depicts the age-adjusted differences in survival over the 1 to 5 years following study enrollment between primary care patients with any opioid use and patients with no opioid use. Data were available for 848 patients. The overall age-adjusted difference in survival between patients with any opioid use (non-prescribed or only as prescribed) and patients with no opioid use was statistically significant (P=0.003).
Table 2. Countsa of Causes of Death by General Cause and Opioid Use.
| Specific Cause | Opioid Use | ||
|---|---|---|---|
| Any Non-prescribed Opioid Use (n=227) | Opioid Use Only as Prescribed (n=162) | No Opioid Use (n=459) | |
| External | |||
| Accidental poisoning | 5 | 6 | 1 |
| Fall | 0 | 1 | 1 |
| Suicide | 0 | 0 | 1 |
| Legal intervention involving firearm discharge | 0 | 1 | 0 |
| Traffic accident | 0 | 1 | 0 |
| Cancer, Cardiovascular | 4 | 7 | 9 |
| Infectious | |||
| Hepatitis C | 1 | 1 | 0 |
| HIV/AIDS | 2 | 1 | 1 |
| Chronic Liver Disease, Otherb | 7 | 2 | 3 |
| Total | 19 | 20 | 16 |
Administrative data available for 848 participants for up to 5 years after study enrollment
Other includes alcoholic cirrhosis of the liver, unspecified cirrhosis of the liver, esophageal obstruction, chronic obstructive pulmonary disease, coagulation defect, schizophrenia, harmful use.
Patients with Any Non-prescribed Opioid Use vs. Patients with Opioid Use Only as Prescribed
Results of all comparisons between patients using any non-prescribed opioids and those using opioids only as prescribed can be seen in Table 3. This table shows that, compared to patients using opioids only as prescribed, those using any non-prescribed opioids were more likely to have been homeless one or more days in the past 90 (33.2% vs 20.8%; P=0.01). They also had more serious drug problems than those using opioids only as prescribed as indicated by higher DAST-10 scores (5.46 vs 3.54; P<0.001) and higher average ASI drug use composite scores (0.17 vs 0.10; P<0.001); were more likely to have used cocaine (47.8% vs 31.0%; P<0.001), amphetamines (12.3% vs 3.6%; P<0.001), and/or sedatives (18.9% vs 3.6%; P<0.001) in addition to opioids in the previous 30 days; more likely to have used 2 or more illicit or non-prescribed drugs in the previous 30 days (89.9% vs 29.2%; P<0.001); to engage in intravenous drug use in the previous 30 days (23.8% vs 0.6%; P<0.001); and to have a higher HIV risk-taking score (4.5 vs 2.4; P<0.001). Non-prescribed opioid users also had more problem alcohol use relative to their prescribed opioid user counterparts as indicated by higher mean ASI alcohol use composite scores (0.18 vs 0.10; P<0.001) and a higher proportion reporting one or more days of alcohol use in the previous 30 (74.6% vs 58.9%; P<0.001). On the other hand, patients using opioids only as prescribed were more likely to use marijuana (83.9% vs 67.1%; P<0.001) and almost three times more likely to use medical marijuana than patients using non-prescribed opioids (26.2% vs 7.5%; P<0.001). They also had a higher mean number of outpatient medical visits in the 2 years prior to study enrollment (24.3 vs 19.5; P=0.01). Although these subgroups did not differ on overall EQ-5D health status scores, a higher proportion of patients in the prescribed opioid use category reported having pain on the EQ-5D instrument (94.1% vs 80.7%; P<0.001), a finding similar to that reported by Brands and colleagues (2004).
Table 3. Baseline Characteristics by Opioid Use (n=396).
| Characteristics | Opioid Usea | Pb | |
|---|---|---|---|
| Any Non-prescribed Opioid Use (n=228) | Opioid Use Only as Prescribed (n=168) | ||
| Demographics | |||
| Age, mean in years (SD) | 48.4 (10.5) | 49.6 (9.6) | 0.25 |
| Male | 68.9% | 67.3% | 0.74 |
| Racec | |||
| White | 49.3% | 49.4% | 1.00 |
| Black | 32.9% | 32.9% | |
| Other | 17.8% | 17.7% | |
| Hispanic | 11.0% | 7.3% | 0.24 |
| Marital status | |||
| Married/living with partner | 20.2% | 23.4% | 0.63 |
| Divorced/separated/widowed | 43.4% | 44.3% | |
| Never married | 36.4% | 32.3% | |
| Education | |||
| High school or less | 22.0% | 17.9% | 0.52 |
| High school graduate | 24.7% | 23.8% | |
| Beyond high school | 53.3% | 58.3% | |
| Employment status | |||
| Working | 7.0% | 7.1% | 0.83 |
| Unemployed/retired/in school/homemaker/other | 22.8% | 20.2% | |
| Disabled and unable to work | 70.2% | 72.6% | |
| Homeless in shelter or on street ≥1 night in past 90 daysd | 33.2% | 20.8% | 0.01 |
| Medical | |||
| Emergency departmente | |||
| Any (%) | 68.7% | 65.4% | 0.50 |
| Mean visits (SD) | 3.0 (4.9) | 2.4 (3.9) | 0.19 |
| Mean cost (SD) | $1,550.34 ($2,526.56) | $1,388.38 ($2,772.55) | 0.55 |
| Median visits | 1.0 | 1.0 | |
| Median cost | $625.39 | $423.70 | |
| Outpatient medicale | |||
| Any (%) | 93.4% | 95.1% | 0.49 |
| Mean visits (SD) | 19.5 (18.1) | 24.3 (19.2) | 0.01 |
| Mean cost (SD) | $7,651.65 ($9,823.59) | $8,787.94 ($9,265.75) | 0.25 |
| Median visits | 15.0 | 20.0 | |
| Median cost | $4,742.62 | $6,572.43 | |
| Inpatient medicale | |||
| Any (%) | 34.8% | 34.6% | 0.96 |
| Mean admissions (SD) | 0.6 (1.2) | 0.6 (1.1) | 0.94 |
| Mean cost (SD) | $10,229.75 ($34,394.72) | $10,140.79 ($23,337.68) | 0.98 |
| Median admissions | 0.0 | 0.0 | |
| Median cost | $0.00 | $0.00 | |
| ASI Medical Status composite score, mean (SD)f | 0.70 (0.32) | 0.77 (0.25) | 0.02 |
| CDPS medical conditions, mean (SD)e | 8.0 (3.6) | 8.7 (3.4) | 0.06 |
| EQ-5D score, mean (SD) | 0.65 (0.22) | 0.63 (0.21) | 0.24 |
| EQ-5D Item 4: “I have moderate pain or discomfort” or “I have extreme pain or discomfort” | 80.7% | 94.1% | < 0.001 |
| Psychiatric | |||
| ≥1 Mental illness ICD-9 diagnosise | 70.0% | 70.4% | 0.94 |
| Prescribed medication for psychological or emotion problems, lifetime | 78.5% | 77.4% | 0.79 |
| Substance Use/Treatment | |||
| ASI days most frequently used drug, mean (SD)g | 16.35 (10.63) | 13.92 (11.24) | 0.03 |
| ASI Drug Use composite score, mean (SD)f,g | 0.17 (0.13) | 0.10 (0.08) | <0.001 |
| ASI drug use, any in past 30 days h | |||
| Marijuana | 67.1% | 83.9% | < 0.001 |
| Medical Marijuana | 7.5% | 26.2% | < 0.001 |
| Stimulants | 53.9% | 33.3% | < 0.001 |
| Cocaine | 47.8% | 31.0% | < 0.001 |
| Amphetamines | 12.3% | 3.6% | < 0.001 |
| Opioids | 100.0% | 100.0% | < 0.001 |
| Heroin | 25.9% | 0.0% | < 0.001 |
| Methadone non-prescribed | 21.9% | 0.0% | < 0.001 |
| Methadone prescribed | 4.8% | 17.3% | < 0.001 |
| Other opioids/analgesics non-prescribed | 80.3% | 0.0% | < 0.001 |
| Other opioids/analgesics prescribed | 23.2% | 89.9% | < 0.001 |
| Sedatives/hypnotics/tranquilizers | 18.9% | 3.6% | < 0.001 |
| Benzodiazepines non-prescribed | 12.7% | 1.8% | <0.001 |
| Other drugs g, i | 11.4% | 2.4% | < 0.001 |
| 2 or more drugs used in past 30 days g, j | 89.9% | 29.2% | < 0.001 |
| Intravenous drug use past 30 days | 23.8% | 0.6% | < 0.001 |
| Goal of total abstinence from drugsg, k | 43.0% | 33.9% | 0.07 |
| DAST-10 drug use severity, mean score (SD)g | 5.46 (2.69) | 3.54 (2.24) | <0.001 |
| Low (score 1-2) | 14.5% | 41.7% | <0.001 |
| Intermediate (score 3-5) | 40.8% | 38.1% | |
| Substantial/severe (score ≥ 6) | 44.7% | 20.2% | |
| ASI Alcohol Use composite score, mean (SD)f | 0.18 (0.21) | 0.10 (0.15) | <0.001 |
| ASI alcohol use, any in past 30 days | 74.6% | 58.9% | < 0.001 |
| Nicotine use, any in past 30 days | 76.8% | 69.6% | 0.11 |
| CD treatment services | |||
| Admitted to CD treatmente | 23.8% | 9.9% | < 0.001 |
| Detoxification (not followed by CD treatment)e | 9.7% | 5.6% | 0.14 |
| Other Psychosocial | |||
| Arrests for felony or gross misdemeanore | 14.5% | 13.0% | 0.66 |
| HIV Risk-taking Behaviour score, mean (SD) | 4.5 (5.1) | 2.4 (3.3) | <0.001 |
| ASI Family/Social composite score, mean (SD)f | 0.20 (0.24) | 0.18 (0.22) | 0.41 |
Missing values are not included in this table.
Pvalue based on chi square or ANOVA.
Assessed by self-report using National Institutes of Health reporting categories for federally funded clinical research.
Homeless was defined as spending at least 1 night in the previous 90 either living on the streets, in an abandoned building, in a car, or in a shelter.
Administrative data available for 389 participants for the 2 years prior to enrollment.
ASI composite scores range from 0 to 1, with 1 indicating greatest problem severity.
Excludes use of alcohol or nicotine.
ASI drug use groups reported are not mutually exclusive. The groups reflect illicit or non-prescribed use only unless otherwise indicated.
“Other drugs” can include all other abused medications (e.g., antihistamines, antidepressants) or drugs of abuse (e.g., hallucinogens, inhalants) not included in the existing categories.
Problem drugs or non-prescribed medications.
From the Thoughts About Abstinence measure which is used to assess one's goal for changing drug use (no goal, controlled use, occasional use, temporary abstinence, total abstinence slip is possible, total abstinence never use again). The reported “goal of total abstinence from drugs” includes “total abstinence, never use again” and “total abstinence, slip is possible.”
ASI, Addiction Severity Index; CD, chemical dependency; CDPS, Chronic Illness and Disability Payment System; DAST-10, Drug Abuse Screening Test 10-item; EQ-5D, Euroqol EQ-5D instrument.
A significantly higher percent of patients using non-prescribed opioids at baseline were admitted to chemical dependency treatment compared to patients using prescribed opioids in both the 2 years prior to enrollment in the study (23.8% vs 9.9%; P<0.001) and in the 1 year following study enrollment (22% vs 10%; P<0.001). Among those admitted to treatment in the 1 year following study enrollment, non-prescribed opioid users were more likely to attend inpatient (8% vs 1%; P<0.001) or methadone maintenance/opioid substitution treatment (11% vs 2%; P<0.001) than prescribed opioid users.
Discussion
The purpose of this study was to describe characteristics and service utilization patterns of safety-net primary care clinic patients who used opioids in order to help addiction specialists working in primary care and specialty settings plan for and manage problems related to such use. We did this in two ways—first, by comparing patients using any opioids (prescribed or non-prescribed) with patients not using opioids and, second, by comparing patients using any non-prescribed opioids with those using opioids only as prescribed. In both sets of comparisons we found significant and clinically meaningful differences between groups which may have implications for clinicians managing these patients.
Any Opioid Use vs No Opioid Use
Although all participants in this study had an unusually high average number of medical and psychiatric co-morbidities, patients using opioids, whether prescribed or not, had significantly more medical and psychiatric comorbidities than drug users who did not use opioids, a finding similar to that reported by Wu and colleagues (Wu et al., 2011). Multiple measures suggested opioid users were significantly less healthy including having an average of 8.3 CDPS comorbid medical conditions. To put this finding into perspective, the average number of CDPS conditions for disabled Medicaid beneficiaries is less than 2 (Kronick et al., 2000), so that an average of 8 is unusually high, even when compared to other drug users who did not use opioids where the average was 6.7. In addition, more than 70% had a mental illness diagnosis in their medical record compared to less than 59% of drug users who did not use opioids, and more than three-quarters (78%) admitted to having received prescribed medication for psychological or emotional problems in their lifetime compared to 66% of drug users who did not use opioids. The combination of significant medical and psychiatric co-morbidities could explain why a higher proportion of opioid users were heavy users of medical services, including emergency department and inpatient hospital services, in the two years prior to study enrollment with almost double the inpatient costs of their non-opioid using counterparts as well as having a higher mean number of outpatient medical services and associated costs—costs borne almost exclusively by the public system. It is important to keep in mind that all participants in this study were selected because they reported problem drug use—so comparisons reported here are between patients with self-reported drug use who used opioids and patients with self-reported drug use that did not. Nonetheless, the differences between these groups was striking, suggesting that use of opioids is associated with a dimension of severity over and above illicit drug use as it presents in the primary care setting. It is likely that opioid users with such chronic medical and psychiatric problems will need ongoing medical, psychiatric, and addictions care. Ideally, such care will include services that integrate behavioral and primary care, as well as onsite or easily accessed specialty addictions and psychiatric care.
Similar to reports of others (Calcaterra et al., 2013; King et al., 2014), patients using opioids were almost 3 times more likely to die in the 1 to 5 years following study enrollment irrespective of whether they used non-prescribed opioids or opioids only as prescribed. Further, opioid users were more likely to die of accidental poisonings than were patients who did not use opioids. More frequent accidental poisonings for patients using opioids may be a consequence of their greater likelihood of using additional drugs including benzodiazepines at baseline. It is known that such combinations are associated with overdose lethality (Jones et al., 2012; Weich et al., 2014) as well as more serious emergency department visit outcomes (Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality, 2014). There are at least two implications that follow from these findings: first, the frequency of deaths due to accidental poisonings among primary care patients who reported using opioids in the present study argues for providers making naloxone overdose prevention kits available to all opioid-using patients they treat (Wheeler et al., 2012). Second, the findings also argue for the availability of buprenorphine- or methadone-based addiction treatment integrated onsite, especially in safety-net clinics which often serve a relatively high proportion of patients with illicit drug use. Additionally, it is important that barriers to opioid replacement or blocker care be minimized. This would include administrative, financial, distance, and other barriers to access (Ward et al., 1999).
Any Non-prescribed Opioids vs Opioids Only as Prescribed
When patients using non-prescribed opioids were compared to those using prescribed opioids, the non-prescribed subgroup reported substantially more serious drug problems, significantly more intravenous drug use, and higher HIV risk-taking behavior. They also reported significantly more serious problems with alcohol. Importantly, with local and national efforts decreasing the amount and availability of both prescribed and non-prescribed opioid medications, the use of heroin is dramatically rising (Rudd et al., 2014). With increased heroin use come injection infections, hepatitis C, HIV, and other related problems. Implications for the apparent heroin epidemic include implementing the overdose and treatment access suggestions made earlier in this paper as well as preparing primary care and other hospital services for treatment of more intravenous heroin use consequences. In addition, other prevention efforts such as clean needle exchanges have been shown effective (Aspinall et al., 2014).
In contrast to patients using any non-prescribed opioids, patients using opioids only as prescribed were more likely to use marijuana and almost 3 times more likely to use medical marijuana than their non-prescribed opioid-using counterparts. Patients using opioids only as prescribed may have been using marijuana for perceived additional pain relief as evidenced by their more frequent outpatient medical visits, higher medical costs, and higher likelihood of reporting that they were experiencing pain. Washington is one of a growing number of states with laws allowing access to medical marijuana presumably for the treatment of chronic pain. A recent report indicates that such laws are associated with significantly lower state-level opioid overdose mortality (Bachhuber et al., 2014). Although the reported association may not be causal and is beyond the scope of this paper, it suggests an important direction for future research.
Readiness to Change
Despite the above challenges, it is important to recognize that 39% of opioid users in both the non-prescribed and only as prescribed subgroups who participated in the present study stated that they had a goal of abstinence from drugs and, further, that in the year following study enrollment, 22% of patients using non-prescribed opioids and almost 10% of those using prescribed opioids were admitted to specialized chemical dependency treatment. Thus, there is reason to believe that more than a third of persons with problem drug use who are also using opioids may be candidates for change and that the addictions or primary care provider could be in a key position to facilitate that change.
Strengths and Limitations
Strengths of this study are that it is based on a relatively large number of safety-net primary care patient participants (n=868), all with self-reported illicit drug use. We clearly missed patients with drug use who either denied using or did not want to be in a randomized study of brief intervention for drug use. Since the focus of the original study was brief intervention for drugs, primary care patients without recent drug use were not included, limiting the generalizability of our results. Similarly, patients who only used alcohol were not included. However, if addiction services are to be better developed in safety-net primary care clinics, alcohol problems will also need to be targeted. Further, death records may not have included Washington State residents who died out of state. The relatively few numbers of deaths also limited our ability to identify baseline predictors of mortality in the two groups. Since this study is based on secondary analyses of data generated in a randomized controlled trial on patients who self-reported recent use of illicit drugs, we did not have data on the general medical population available to us nor did we have data on other patients with addiction disorders treated in the primary care safety-net clinics. Finally, because of limitations inherent in secondary analyses, our study design does not allow us to determine whether particular patient characteristics such as IV drug use and/or polysubstance use were causally related to prescribed and non-prescribed opioid use. As such, we are not able to rule out the possibility that observed or unobserved differences between prescribed and non-prescribed opioid use subgroups may have confounded the associations we observed. Our study was an initial exploration of drug-related problems in drug-using patients who used or did not use opioids along with their associated demographic, medical, psychiatric and substance use characteristics as encountered in primary care clinics of an urban county hospital system. As such we emphasize that our results are meant to be descriptive and are best viewed as a rich source of hypotheses for the design of future studies rather than being definitive.
Conclusions
Results of this study suggest that use of opioids adds a dimension of severity over and above illicit drug use as it presents in the primary care setting. Multiple measures indicated that opioid users were less physically and psychiatrically healthy than drug users who did not endorse using opioids and that they were heavy users of medical services including emergency departments, inpatient hospitals, as well as outpatient medical services—at considerable public cost. It is likely that opioid users with such chronic medical and psychiatric problems will need ongoing medical, psychiatric, and addictions care. Ideally, such care will include services that integrate behavioral and primary care, as well as onsite or easily accessed specialty addictions and psychiatric care. Their higher likelihood of dying from accidental overdose argues for providers making naloxone overdose prevention kits available to all opioid-using patients they treat. Subgroup analyses suggested that persons using non-prescribed opioids differed from those using opioids only as prescribed in reporting substantially more serious drug use including more intravenous drug use and greater HIV risk-taking behavior—observations that argue for preparing primary care and other hospital services for treatment of more intravenous heroin use consequences coupled with prevention efforts such as clean needle exchanges. Despite the above challenges, more than a third of opioid users in both the non-prescribed and only as prescribed subgroups reported having a goal of abstinence from drugs, suggesting they may be candidates for change and that the addictions or primary care provider could be in a key position to facilitate that change.
Acknowledgments
This study was funded by grant R01 DA026014 from the National Institute on Drug Abuse awarded to Dr. Roy-Byrne. The views expressed reflect those of the authors and do not necessarily reflect the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Dr. Ries reported receiving financial support from Janssen Pharmaceuticals Inc and Alkermes, outside the submitted work. Dr. Roy-Byrne reported receiving financial support as the Editor-in-Chief of Depression and Anxiety, Journal Watch Psychiatry, and UpToDate Psychiatry, and receiving stock options for consultation to Valant Medical Solutions (behavioral health electronic medical record company), outside the submitted work. For the remaining authors none were declared.
We thank David C. Atkins, PhD, for his helpful contribution to the analysis and Joseph Merrill, MD, MPH, for his valuable comments on an earlier version of this manuscript.
References
- Aspinall E, Nambiar D, Goldberg D, et al. Are needle and syringe programmes associated with a reduction in HIV transmission among people who inject drugs: A systematic review and meta-analysis. Int J Epidemiol. 2014;43(1):235–248. doi: 10.1093/ije/dyt243. [DOI] [PubMed] [Google Scholar]
- Bachhuber M, Saloner B, Cunningham C, Barry C. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med. 2014;174(10):1668–1673. doi: 10.1001/jamainternmed.2014.4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer MA, Azzone V, Goldman H, et al. Implementation of collaborative depression management at community-based primary care clinics: An evaluation. Psychiatr Serv. 2014;62(9):1047–1053. doi: 10.1176/appi.ps.62.9.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: Systematic review and meta-analysis. Arch Intern Med. 2005;165(9):986–995. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- Brands B, Blake J, Sproule B, Gourlay D, Busto U. Prescription opioid abuse in patients presenting for methadone maintenance treatment. Drug Alcohol Depend. 2004;73(2):199–207. doi: 10.1016/j.drugalcdep.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, Lynch KG, Martin JM, Beauchamp ML, Mclellan AT. Initial reliability and validity studies of the revised Treatment Services Review (TSR-6) Drug Alcohol Depend. 2008;92(1-3):37–47. doi: 10.1016/j.drugalcdep.2007.06.004. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, Mclellan AT, Lin YT, Lynch KG. Initial evidence for the reliability and validity of a “Lite” version of the Addiction Severity Index. Drug Alcohol Depend. 2007;87(2-3):297–302. doi: 10.1016/j.drugalcdep.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Calcaterra S, Glanz J, Binswanger I. National trends in pharmaceutical opioid related overdose deaths compared to other substance related overdose deaths: 1999-2009. Drug Alcohol Depend. 2013;131(3):263–270. doi: 10.1016/j.drugalcdep.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan Y, Huang H, Bradley K, J U. Referral for substance abuse treatment and depression improvement among patients with co-occurring disorders seeking behavioral health services in primary care. J Subst Abuse Treat. 2014;46(2):106–116. doi: 10.1016/j.jsat.2013.08.016. [DOI] [PubMed] [Google Scholar]
- Darke S, Hall W, Heather N, Ward J, Wodak A. The reliability and validity of a scale to measure HIV risk-taking behaviour among intravenous drug users. AIDS. 1991;5(2):181–185. doi: 10.1097/00002030-199102000-00008. [DOI] [PubMed] [Google Scholar]
- Euroqol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- Hall SM, Havassy BE, Wasserman DA. Commitment to abstinence and acute stress in relapse to alcohol, opiates, and nicotine. J Consult Clin Psychol. 1990;58(2):175–181. doi: 10.1037//0022-006x.58.2.175. [DOI] [PubMed] [Google Scholar]
- Jones C, Paulozzi L, Mack K. Morbidity and Mortality Weekly Report. 40. Vol. 63. Atlanta, GA: Centers for Disease Control and Prevention; Oct 10, 2014. Alcohol involvement in opioid pain reliever and benzodiazepine drug abuse-related emergency department visits and drug-related deaths - United States, 2010; pp. 881–885. Available at: http://www.cdc.gov/mmwr/pdf/wk/mm6340.pdf. [PMC free article] [PubMed] [Google Scholar]
- Jones J, Mogali S, Comer S. Polydrug abuse: A review of opioid and benzodiazepine combination use. Drug Alcohol Depend. 2012;125(1-2):8–18. doi: 10.1016/j.drugalcdep.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Sys Rev. 2007;(2):CD004148. doi: 10.1002/14651858.CD004148.pub3. doi:004110.001002/14651858.CD14004148.pub14651853. [DOI] [PubMed] [Google Scholar]
- King N, Fraser V, Boikos C, Richardson R, Harper S. Determinants of increased opioid-related mortality in the United States and Canada, 1990-2013: A systematic review. Am J Public Health. 2014;104(8):e32–42. doi: 10.2105/AJPH.2014.301966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronick R, Gilmer T, Dreyfus T, Lee L. Improving health-based payment for Medicaid beneficiaries: CDPS. Health Care Financ Rev. 2000;21(3):29–64. [PMC free article] [PubMed] [Google Scholar]
- Krupski A, Joesch JM, Dunn C, et al. Testing the effects of brief intervention in primary care for problem drug use in a randomized controlled trial: Rationale, design, methods. Addict Sci Clin Pract. 2012;7(1):27. doi: 10.1186/1940-0640-7-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchikanti L, Abdi S, Atluri S, et al. American Society of Interventional Pain Physicians (ASIPP) guidelines for responsible opioid prescribing in chronic non-cancer pain: Part 2--guidance. Pain Physician. 2012;15(3 Suppl):S67–116. [PubMed] [Google Scholar]
- Roy-Byrne P, Bumgardner K, Krupski A, et al. Brief intervention for problem drug use in safety-net primary care settings: A randomized clinical trial. JAMA. 2014;312(5):492–501. doi: 10.1001/jama.2014.7860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd R, Paulozzi L, Bauer M, et al. Morbidity and Mortality Weekly Report. 39. Vol. 63. Atlanta, GA: Centers for Disease Control and Prevention; Oct 3, 2014. Increases in heroin overdose deaths - 28 states, 2010 to 2012; pp. 849–854. Available at: http://www.cdc.gov/mmwr/pdf/wk/mm6339.pdf. [PMC free article] [PubMed] [Google Scholar]
- Saitz R. Alcohol screening and brief intervention in primary care: Absence of evidence for efficacy in people with dependence or very heavy drinking. Drug Alcohol Rev. 2010;29(6):631–640. doi: 10.1111/j.1465-3362.2010.00217.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R. The best evidence for alcohol screening and brief intervention in primary care supports efficacy, at best, not effectiveness: You say tomāto, I say tomăto? That's not all it's about. Addict Sci Clin Pract. 2014;9:14. doi: 10.1186/1940-0640-9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA. The Drug Abuse Screening Test. Addict Behav. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality. The DAWN Report: Benzodiazepines in combination with opioid pain relievers or alcohol: Greater risk of more serious ED visit outcomes. Rockville, MD: Dec 18, 2014. 2014. Available at: http://www.samhsa.gov/data/sites/default/files/DAWN-SR192-BenzoCombos-2014/DAWN-SR192-BenzoCombos-2014.pdf. [PubMed] [Google Scholar]
- Ward J, Hall W, Mattick R. Role of maintenance treatment in opioid dependence. Lancet. 1999;353(9148):221–226. doi: 10.1016/S0140-6736(98)05356-2. [DOI] [PubMed] [Google Scholar]
- Warner M, Chen LH, Makuc DM, Anderson RN, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. Hyattsville, MD: National Center for Health Statistics; 2011. NCHS Data Brief, No. 81. Available at: http://www.cdc.gov/nchs/data/databriefs/db81.pdf. [Google Scholar]
- Weich S, Pearce H, Croft P, et al. Effect of anxiolytic and hypnotic drug prescriptions on mortality hazards: Retrospective cohort study. BMJ. 2014;348:g1996. doi: 10.1136/bmj.g1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler E, Davidson PJ, Jones TS, Irwin KS. Morbidity and Mortality Weekly Report. 6. Vol. 61. Atlanta, GA: Centers for Disease Control and Prevention; Feb 17, 2012. Community-based opioid overdose prevention programs providing naloxone - United States, 2010; pp. 101–105. Available at: http://www.cdc.gov/mmwr/pdf/wk/mm6106.pdf. [PMC free article] [PubMed] [Google Scholar]
- Williams EC, Rubinsky AD, Chavez LJ, et al. An early evaluation of implementation of brief intervention for unhealthy alcohol use in the US Veterans Health Administration. Addiction. 2014;109(9):1472–1481. doi: 10.1111/add.12600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L, Woody G, Yang C, Blazer D. How do prescription opioid users differ from users of heroin or other drugs in psychopathology: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Addict Med. 2011;5(1):28–35. doi: 10.1097/ADM.0b013e3181e0364e. [DOI] [PMC free article] [PubMed] [Google Scholar]