Abstract
Multiple literature addresses cleft alveolar bone, with little consensus on the preferred surgical technique. Hence, we described a transoral approach for repair of cleft alveolar bone with Z-plasty and using bioactive glass. Study design: Case presentation and surgical technique description. In conclusion, transoral mucosal repair cleft alveolar bone Z-plasty using bioactive glass demonstrated an alternative easy and simple approach for augmentation of unilateral alveolar cleft patients.
Keywords: Bioactive materials, Bioglass®, cleft alveolar bone, mucosal Z-plasty
INTRODUCTION
Treatment of the residual alveolar defect in patients with cleft lip and palate often requires bone grafting.[1] An important goal for this treatment, apart from restoring the missing alveolar bone in the cleft area, is to obtain favorable periodontal conditions for the teeth adjacent to the defect. Attempts to move the teeth into the edentulous spaces often result in significant periodontal problems.[2]
The first report about the alveolar bone grafting aiming to obtain the continuity of the alveolar process was published by Lexer in 1908,[3] who used free bone grafting or pedicled flap of bone and soft tissues of the fifth digit. Various sources of autogenous bone are used, but an anterior iliac crest is considered the gold standard for grafting. Its resorption rate seems to be high within the 1st year after grafting.[4] From since, multiple techniques and materials have been described to repair the alveolar bone cleft deformity. We describe a transoral mucosal to repair cleft alveolar bone with Bioglass and Z-plasty.
CASE REPORT
A 10-year-old male, born with a unilateral left cleft lip and palate was presented to our clinic. The cleft lip was surgically repaired at an early age. The history indicated that there was no known familial incidence of cleft lip or palate. At the time of the initial dental evaluation, the patient show complete alveolar bone cleft on the left side of the premaxilla with nasolalvelar fistula [Figure 1a]. The patient complained from the nasal regurgitation of both food and fluids into the nose and the disfigurement during a smile.
Figure 1.
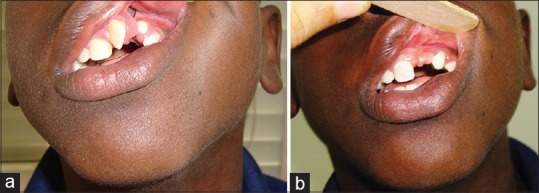
(a) Preoperative picture for patient with cleft alveolar. (b) Postoperative picture for patient with repaired cleft alveolar after 1-year
First, a Z-plasty was designed by donning a Z-incision in the mucosal side of the upper lip forming two mucosal triangles (1 and 2) flap with small mucosal triangle (3) in between [Figure 2a], this small mucosal triangle (3) used to cover the floor of the nose [Figure 2b]. In addition, the bioactive glass (Bioglass®) was mixed with blood [Figure 3] and then inserted into the pocket done after the closure of the nasal floor. Finally, the two triangles (1 and 2) are suture together using a 5-0 Vicryl by crossing each other. Wound healing of the recipient sites was observed. Wound complications such as bleeding, infection, dehiscence, and neurologic disturbance were recorded. Furthermore, the evaluation of bone graft quantities was performed according to the Bergland[5] scale (Oslo grading system). With this scale, the obtained bone level of the interdental septum is compared with the normal side, and it was type 1 in this case after 1-year [Figure 1b].
Figure 2.
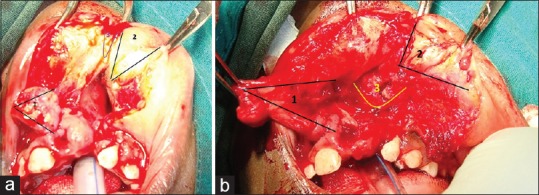
Intraoperative picture for patient with cleft alveolar. (a) Z-plasty mucosal triangle (1 and 2) flap with small mucosal triangle (3) in between (b) the small mucosal triangle (3) used to cover the floor of the nose
Figure 3.
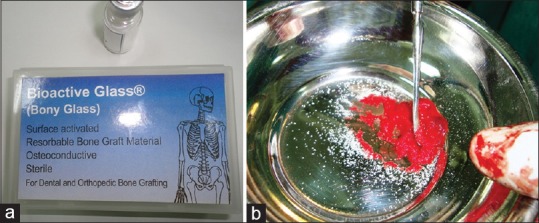
(a) Bioactive glass (Bioglass®) maples. (b) Bioglass® mixed with blood
DISCUSSION
Alloplastic grafts have been used successfully in the repair of artificial alveolar clefts in animals. According to the literature, autogenic grafts are mostly used; however, alloplastic graft material started to take place in repair alveolar clefts in human beings.[2]
Four major categories of surface-active biomaterials have been developed; dense hydroxylapatite ceramics, bioactive glasses, bioactive glass-ceramics, and bioactive composites. Bioactive glass is a commercially available family of bioactive glasses, composed of silicone dioxide (SiO2), sodium dioxide (Na2O), calcium oxide (CaO) and phosphorous pentoxide (P2O5) in specific proportions. Bioglass® or 45S5 are bioactive glass which is composed of 45% SiO, 24.5% CaO, 24.5% Na2O and 6% P2O5. Bioactive glass such as (e.g., 45S5 or Bioglass®) bind to soft tissues and bone, while Bioactive glass-ceramics (e.g., 5S4.3 or Ceravital®) bind only to bone, both designed to engender surface reactions that lead to osseointegration,[6] In this case I used the bioactive glass (Bioglass®).
Johnson et al.[7] reported that the bioactive glass material in animals was surrounded with osteoid and new bone. Alloplastic graft materials that provide simply a scaffolding effect to give support to vascular ingrowth and later calcification are known as osteoconductive. Osteoinductive materials, on the other hand, are those that contain morphogens, substances that initiate the development of tissues and organ systems by stimulating undifferentiated cells to convert phenotypically.[8]
Arctander et al.[9] suggest that one should graft as much bone as possible to obtain adequate facial appearance. Their study examined 18 patients with complete unilateral cleft lip and palate using computed tomography 20 years after secondary cancellous bone graft from the iliac crest. They concluded that, even though all dental gaps were closed, and patients were functionally intact, the amount of alveolar bone in the cleft side was less than that of the noncleft side. Feichtinger et al.[10] also showed that the absence of adjacent teeth to the cleft site leads to mean the bone volume loss of 95%. Hence, the augmentation of unilateral alveolar cleft could be archived perfect by using this technique and the bioactive glass material, which gave a result of Bergland's scale type 1 after 1-year of follow-up.
CONCLUSIONS AND RECOMMENDATION
Transoral mucosal repair of cleft alveolar bone by Z-plasty using bioactive glass demonstrated an alternative easy and simple approach for augmentation of unilateral alveolar cleft patients. Hence, we recommend more patients to undergo this new technique and a longer time for follow-up.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Witsenburg B. The reconstruction of anterior residual bone defects in patients with cleft lip, alveolus and palate. A review. J Maxillofac Surg. 1985;13:197–208. doi: 10.1016/s0301-0503(85)80048-5. [DOI] [PubMed] [Google Scholar]
- 2.Yilmaz S, Kiliç AR, Keles A, Efeoglu E. Reconstruction of an alveolar cleft for orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2000;117:156–63. doi: 10.1016/s0889-5406(00)70226-5. [DOI] [PubMed] [Google Scholar]
- 3.Yilmaz S, Kiliç AR, Keles A, Efeoglu E. Reconstruction of an alveolar cleft for orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2000;117:156–63. doi: 10.1016/s0889-5406(00)70226-5. [DOI] [PubMed] [Google Scholar]
- 4.Hallman M, Cederlund A, Lindskog S, Lundgren S, Sennerby L. A clinical histologic study of bovine hydroxyapatite in combination with autogenous bone and fibrin glue for maxillary sinus floor augmentation. Results after 6 to 8 months of healing. Clin Oral Implants Res. 2001;12:135–43. doi: 10.1034/j.1600-0501.2001.012002135.x. [DOI] [PubMed] [Google Scholar]
- 5.Bergland O, Semb G, Abyholm FE. Elimination of the residual alveolar cleft by secondary bone grafting and subsequent orthodontic treatment. Cleft Palate J. 1986;23:175–205. [PubMed] [Google Scholar]
- 6.Neo M, Kotani S, Nakamura T. A comparative study of ultrastructures of the interfaces between four kinds of surface-active ceramic and bone. J Biomed Mater Res. 1993;27:281–9. doi: 10.1002/jbm.820261103. [DOI] [PubMed] [Google Scholar]
- 7.Johnson MW, Sullivan SM, Rohrer M, Collier M. Regeneration of peri-implant infrabony defects using PerioGlas: A pilot study in rabbits. Int J Oral Maxillofac Implants. 1997;12:835–9. [PubMed] [Google Scholar]
- 8.Kenley RA, Yim K, Abrams J, Ron E, Turek T, Marden LJ, et al. Biotechnology and bone graft substitutes. Pharm Res. 1993;10:1393–401. doi: 10.1023/a:1018902720816. [DOI] [PubMed] [Google Scholar]
- 9.Arctander K, Kolbenstvedt A, Aaløkken TM, Abyholm F, Frøslie KF. Computed tomography of alveolar bone grafts 20 years after repair of unilateral cleft lip and palate. Scand J Plast Reconstr Surg Hand Surg. 2005;39:11–4. doi: 10.1080/02844310410021749. [DOI] [PubMed] [Google Scholar]
- 10.Feichtinger M, Zemann W, Mossböck R, Kärcher H. Three-dimensional evaluation of secondary alveolar bone grafting using a 3D- navigation system based on computed tomography: A two-year follow-up. Br J Oral Maxillofac Surg. 2008;46:278–82. doi: 10.1016/j.bjoms.2007.12.010. [DOI] [PubMed] [Google Scholar]


