Abstract
Background:
Maxillary nerve block through the greater palatine canal is rarely adopted by dental practitioners due to lack of experience in the technique at hand which may lead into several complications. Nevertheless, it is an excellent method to achieve profound anesthesia in the maxilla. This review focuses on the anatomy as well as the indications, contraindications, and complications associated with this technique.
Materials and Methods:
A literature search was performed using the scientific databases (PubMed and Google Scholar) for articles published up to December 2014 in English, using the key words “maxillary nerve block via the greater palatine canal.” A total of 34 references met the inclusion criteria for this review and were selected.
Conclusion:
Block of the maxillary nerve through the greater palatine canal is a useful technique providing profound anesthesia in the hemi-maxilla, if practiced properly.
Keywords: Anesthesia, cone beam computed tomography, greater palatine canal, greater palatine foramen, maxillary nerve block, pterygopalatine fossa
INTRODUCTION
The greater palatine canal (GPC) transmits the greater palatine nerve [branch of the pterygopalatine ganglion that carries both general sensory fibers from the maxillary nerve (V2) and parasympathetic fibers from the nerve of the pterygoid canal] and the descending palatine artery (branch of the maxillary artery) from the pterygopalatine fossa (PPF) to the oral cavity through its lower orifice, the greater palatine foramen (GPF). Blocking of the V2 through the GPC is an old technique, which was described for the first time in 1917 by Nevin.[1] It is one of two intraoral approaches, the other being the high tuberosity technique, to administer local anesthesia to the PPF in order to anesthetize the maxillary division of the trigeminal nerve. With time, it lost its interest due to the numerous complications (diplopia, ptosis, infraorbital nerve injury, etc.) resulting from improper operation, mostly due to the poor knowledge of the region's anatomy such as GPF location and GPC length.[2,3,4] However, this technique consists of a single injection resulting in an anesthetic effect to the entire hemi-maxilla, including teeth, palatal and gingival mucosa, skin of the midface, maxillary sinus, and nasal cavity.[2] Silverman,[3] Wong and Sved,[4] and many other authors have tried to revise this technique and even modify it in order to minimize the complications that can occur during and/or post procedure. Among these modifications are the use of new palatal landmarks to enable consistent canal location, an increase in the needle/maxillary occlusal angle from 45° to 60°, and utilization of standard dental syringe.
The aim of this article is to review the technique of the V2 block through the GPC from an anatomic point of view, its indications, contraindications, and complications, and to highlight the advantages presented by the cone beam computed tomography (CBCT) technique in observing the exact pathway of the GPC in order to increase the success of the technique and decrease any potential complications. Literature was retrieved through databases including PubMed and Google Scholar.
Anatomy
V2 is the second of the three branches of the trigeminal nerve, the fifth (V) cranial nerve. Purely sensory, it leaves the skull via the foramen rotundum opening directly into the posterior wall of the PPF.[5]
The PPF, located between the maxilla, sphenoid, and palatine bones, is a bilateral, inversed, pyramidal-shaped structure extending from the infratemporal fossa to the nasal cavity via the sphenopalatine foramen.[6]
Its small size combined with the numerous structures that traffic through makes the PPF a complex region.
Beside its communication with the middle cranial fossa through the foramen rotundum (and the pterygoid canal also known as vidian canal), the PPF communicates with the following:[6,7]
The infratemporal fossa (via the pterygomaxillary fissure)
The nasopharynx (via the pharyngeal canal)
The nasal cavity (via the sphenopalatine foramen)
The orbit (via the infraorbital fissure)
The oral cavity (via the GPC).
These communications transmit blood vessels and nerves between these regions.
The openings between the PPF and other regions, and the nerve and vessels passing through are summarized in Table 1.
Table 1.
The openings between the PPF and other regions and the nerve and vessels passing through

After leaving the skull through the foramen rotundum, the V2 crosses the PPF giving off a number of branches (infraorbital nerve, zygomatic nerve, nasopalatine nerve, superior alveolar nerves, pharyngeal nerve, and palatine nerves), inclines laterally on the back of the maxilla, traverses the infraorbital groove and canal, and opens through the infraorbital foramen. There, it becomes the infraorbital nerve, a terminal branch, and gives lower eyelid, nasal and labial branches.[8]
In the PPF, the greater palatine nerve leaves V2, crosses the GPC located in the thickness of the lateral wall of the nasal cavities, emerges through the GPF, and runs forward in a groove almost up to the incisor teeth where it communicates with the nasopalatine nerve. The latter, which is also a branch of the V2, enters the palate through the incisive foramen and innervates the anterior part of the hard palate behind the incisor teeth.[9]
MATERIALS AND METHODS
Knowing that the success of the technique of the V2 block through the GPC is based on knowledge of the anatomy of the palatal region, our goal in this review was to describe, based on previous studies found in the literature, the location of the GPF according to intraoral landmarks that enable the clinician to locate it in a consistently reliable manner and the average length of the GPC.
Matsuda was the first to describe the location of the GPF.[10] Most textbooks locate the foramen in a general way:
Close to the lateral palatal border[11]
In the posterolateral border[12]
Medial to the 3rd maxillary molar[13]
Opposite to the 3rd maxillary molar.[14]
For other more specialized studies, the location of the GPF was observed using many palatal landmarks such as:
Its relation to the maxillary molar teeth
Its distance from the midline maxillary suture (MMS)
Its distance from the posterior border of the hard palate (PBHP)….
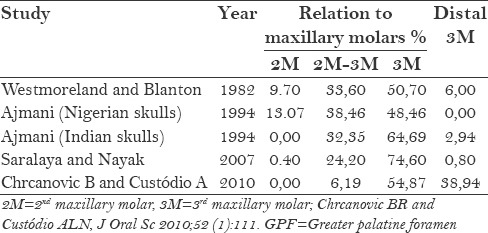
The study of Slavkin et al.[15] found the GPF 1–3 mm distal to the 3rd maxillary molar in adult skulls. In 1982, Westmoreland and Blanton[16] observed only 6% of the foramen distal to the 3rd molar and 9.7% medial to the maxillary 2nd molar. According to Ajmani,[17] 48% of the GPF in Nigerian and 64% in Indian skulls were located medial or opposite to the maxillary 3rd molar. Saralaya and Nayak[18] and Chrcanovic and Custódio[19] concluded in their studies that 74.6% and 54.87% of the GPF, respectively, were opposite to the 3rd molar.
Some data retrieved from the literature regarding the positional variance of the GPF with respect to the maxillary molars are compared and summarized in Table 2.
Table 2.
Comparison of some data from the literature on the positional variance of the GPF with respect to the maxillary molars
As for the distance between the GPF and the MMS, it was found to be around 15 mm according to the study of Westmoreland and Blanton.[16] Ajmani reported a distance of 15.4 mm in Nigerian skulls and a mean of 14.7 mm in Indian skulls.[17] The same distance (14.7 mm) was reported by the study of Saralaya and Nayakand[18] and an average of 14.56 mm was reported by Chrcanovic and Custódio.[19]
Concerning the mean distance of the GPF from the PBHP, it varies between 1.9 mm and 4.2 mm.[16,17,18,19]
Some data retrieved from the literature regarding the mean distance of the GPF from the MMS and the PBHP are compared and summarized in Table 3.
Table 3.
Comparison of some data from the literature on the mean distance of the GPF from the MMS and the PBHP

Regarding the length of the GPC, Swirzinski et al.[20] and Sheikhi et al.,[21] in their studies based on CBCT observations, concluded that the average length of the GPC in adult population was 29 ± 3 mm (ranging from 22 to 40 mm) and 31.82 ± 1.37 mm, respectively. Tomaszewska et al.[22] observed 1500 adult Caucasian head CT scans and found that the average length of the GPC was 31.1 ± 2.9 mm (range 15–44) mm. According to Das et al.,[23] the range of the GPC length is located between 27 and 44 mm with a mean of 32 mm.
Some data retrieved from the literature regarding the length of the GPC are compared and summarized in Table 4.
Table 4.
Comparison of some data from the literaturte on the length of GPC

Clinical applications
Clinically, the GPF is located by applying pressure on a cotton swab at the junction of the hard palate and the maxillary alveolar process until it falls into the depression of the GPF.
As mentioned above, the GPF is most often located distal to the 2nd maxillary molar and its average length is 32 mm.[2,23] Knowing that long canals could lead to lack of anesthesia and, conversely, short ones could have a higher occurrence of complications if the standard needle is used,[20] a CBCT is indicated prior to the procedure to analyze the GPC anatomy, mainly its localization and length [Figures 1 and 2].
Figure 1.

Sagittal view showing the GPC; the arrows show the superior and inferior openings of the canal
Figure 2.

Axial view showing the GPF
Once the GPF is identified, at the most a 27 G needle on a dental syringe is inserted perpendicularly until bone contact and 0.5 ml of local anesthetic is deposited to provide local anesthesia in the area to be injected. After waiting for 3–5 min, the needle is introduced slowly at an angle of 45° to the long axis of the hard palate in the canal to nearly a depth of 32 mm for adults.[2]
Exactly 1.8 ml of local anesthetic is injected without any compression, in order to avoid the risk of tissue necrosis.[24,25] Maximum anesthesia effect is obtained in 5–15 min.[26]
Aspiration is necessary before injection; if blood (needle is in a vessel) or bubbles (needle is in the nasopharynx) are aspirated, the needle is removed, redirected, and reinserted at a different angle.
Indications and contraindications
Maxillary nerve block via the GPC achieves anesthesia of the following:
The hemi-maxilla including teeth, bone, and soft tissue (this effect could be useful for surgical procedures in this region)[2,20,27]
The skin of the midface (for patients with maxillary trauma)[28]
The nasal cavity and sinus (during endoscopic sinus surgery and septorhinoplasty).[22,29,30]
Furthermore, this technique is used for the diagnosis and treatment of chronic oral and maxillofacial pain syndromes.[28]
Jonas et al.[31] successfully treated posterior epistaxis (nosebleeds) with endoscopic sphenopalatine artery ligation technique by infiltration of local anesthesia with vasoconstrictors via the GPC in the PPF. This process can cause vasospasm of the terminal (third) part of the maxillary artery, decreasing the blood flow in its terminal branch and thus facilitating the ligation procedure.
As for the contraindications, the following can be mentioned:
Complications
Complications can be as follows:
-
Related to the local anesthetic:
- Toxicity caused by a large quantity of the anesthetic or an intravascular injection. The toxicity may develop minimal to moderate symptoms such as anxiety, numbness, dizziness, weakness, and tremors. Sometimes, more severe symptoms like central nervous system or cardiovascular collapse may occur
- Allergic reaction caused generally by an ester group local anesthetic and/or the preservatives added to it (methylparaben, sodium metabisulfite, etc.)[33]
-
Related to the technique itself:
- Persistent paresthesia and numbness due to V2 trauma or local hematoma formation
- Transient ophthalmoplegia by anesthetizing the extraocular muscles of the eye[25]
- Ptosis (upper eyelid paralysis) due to anesthesia of the superior division of the oculomotor nerve (the 3rd cranial nerve) responsible of the innervation of the upper eyelid levator muscle.[27]
More serious complications can occur such as:[33]
Infraorbital nerve injury and/or injection (accidental penetration of the orbit)
Neural tissue damage
Temporary blindness from vasoconstriction of the ophthalmic artery or block of the optic nerve
Unconsciousness from intracranial injection (diffusion of the anesthetic via the foramen rotundum).
CONCLUSION
The maxillary nerve block via the GPC was revisited regarding its implementation by a dental practitioner. The technique is deemed advantageous in terms of achieving profound anesthesia of the hemi-maxilla, especially for oral surgeons; however, due to the possibility of rare but potentially serious complications, the said technique should only be performed by proficient and qualified personnel with all necessary equipments at hand. This being said, it is to be noted that a CBCT is imperative to analyze the GPC anatomy, mainly its localization and length.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nevin M, Puterbaugh PG. 4th ed. New York: Dent Items Interest Publishing co; 1938. Conduction, Infiltration and General Anesthesia in Dentistry; p. 140. [Google Scholar]
- 2.Lepere A. Maxillary nerve block via the greater palatine canal: New look at an old technique. Anesth Pain Control Dent. 1993;2:195–7. [PubMed] [Google Scholar]
- 3.Silverman SL. A new and more accurate technique for injecting the superior maxillary division. J Am Med Assoc. 1923;81:112. [Google Scholar]
- 4.Wong JD, Sved AM. Maxillary nerve block anaesthesia via the greater palatine canal: A modified technique and case reports. Aust Dent J. 1991;36:15–21. doi: 10.1111/j.1834-7819.1991.tb00802.x. [DOI] [PubMed] [Google Scholar]
- 5.Hawkins JM, Isen D. Maxillary nerve block: The pterygopalatine canal approach. J Calif Dent Assoc. 1998;26:658–64. [PubMed] [Google Scholar]
- 6.Erdogan N, Unur E, Baykara M. CT anatomy of pterygopalatine fossa and its communications: A pictorial review. Comput Med Imaging Graph. 2003;27:481–7. doi: 10.1016/s0895-6111(03)00038-7. [DOI] [PubMed] [Google Scholar]
- 7.Gray H, Standring S, Ellis H, Berkovitz BKB. New York: Edinburgh, Elsevier Churchill Livingstone; 2005. Gray's Anatomy: The anatomical Basis of Clinical Practice; p. 1627. [Google Scholar]
- 8.Carpentier P. Trigeminal sensory pathways: A guide for anesthesia. Actual Odonto-Stomatol. 1992;179:453–67. [Google Scholar]
- 9.Standring S, Ellis H, Healy JC, et al. Oral cavity. In: Standring S, editor. Gray's Anatomy: The Anatomical Basis of Clinical Practice. 39th ed. London: Elsevier, Churchill Livingstone; 2005. p. 584. [Google Scholar]
- 10.Matsuda Y. Location of the dental foramina in human skulls from statistical observations. Int J Orthod Oral Surg Radiogra. 1927;13:299–305. [Google Scholar]
- 11.Williams PL, Warwick R, Dyson M, Bannster H. Gray's Anatomy. 38th ed. London: Longmans; 1995. pp. 187–91. [Google Scholar]
- 12.Gardner E, Gray DJ, O’Rahilly R. 4th ed. Philadelphia: WB Saunders; 1975. Anatomy; p. 997. [Google Scholar]
- 13.Moore KL. Baltimore: Williams and Wilkins; 1980. Clinically Oriented Anatomy; p. 1004. [Google Scholar]
- 14.Romanes GJ. 12th ed. New York: Oxford University Press; 1981. Cunningham's Textbook of Anatomy; p. 166. [Google Scholar]
- 15.Slavkin HC, Canter MR, Canter SR. An anatomic study of the pterygomaxillary region in the craniums of infants and children. Oral Surg Oral Med Oral Pathol. 1996;21:225–35. doi: 10.1016/0030-4220(66)90248-9. [DOI] [PubMed] [Google Scholar]
- 16.Westmoreland EE, Blanton PL. An analysis of the variations in position of the greater palatine foramen in the adult human skull. Anat Rec. 1982;204:383–8. doi: 10.1002/ar.1092040412. [DOI] [PubMed] [Google Scholar]
- 17.Ajmani ML. Anatomical variation in position of the greater palatine foramen in the adult human skull. J Anat. 1994;184:635–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Saralaya V, Nayak SR. The relative position of the greater palatine foramen in dry Indian skulls. Singapore Med J. 2007;48:1143–6. [PubMed] [Google Scholar]
- 19.Chrcanovic BR, Custódio AL. Anatomical variation in the position of the greater palatine foramen. J Oral Sci. 2010;52:109–13. doi: 10.2334/josnusd.52.109. [DOI] [PubMed] [Google Scholar]
- 20.Swirzinski KH, Edwards PC, Saini TS, Norton NS. Length and geometric patterns of the greater palatine canal observed in cone beam computed tomography. Int J Dent 2010. 2010 doi: 10.1155/2010/292753. pii: 292753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sheikhi M, Zamaninaser A, Jalalian F. Length and anatomic routes of the greater palatine canal as observed by cone beam computed tomography. Dent Res J (Isfahan) 2013;10:155–61. doi: 10.4103/1735-3327.113324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tomaszewska IM, Kmiotek EK, Pena IZ, Sredniawa M, Czyzowska K, Chrzan R, et al. Computed tomography morphometric analysis of the greater palatine canal: A study of 1,500 head CT scans and a systematic review of literature. Anat Sci Int. 2014 Dec 3; doi: 10.1007/s12565-014-0263-9. doi: 10.1007/s12565-014-0263-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Das S, Kim D, Cannon TY, Ebert JR, Senior BA. High-resolution computed tomography analysis of the greater palatine canal. Am J Rhinol. 2006;20:603–8. doi: 10.2500/ajr.2006.20.2949. [DOI] [PubMed] [Google Scholar]
- 24.Nish LA, Pynn BR, Holmes HI, Young ER. Maxillary nerve block: A case report and review of intraoral technique. J Can Dent Assoc. 1995;61:305–10. [PubMed] [Google Scholar]
- 25.Malamed SF, Trieger N. Intraoral maxillary nerve block: An anatomical and clinical study. Anesth Prog. 1983;30:44–8. [PMC free article] [PubMed] [Google Scholar]
- 26.Mahoney PM. Maxillary nerve block. Anesth Prog. 1977;24:47–9. [PMC free article] [PubMed] [Google Scholar]
- 27.Sved AM, Wong JD, Donkor P, Horan J, Rix L, Curtin J, et al. Complications associated with maxillary nerve block anesthesia via the greater palatine canal. Aust Dent J. 1992;37:340–5. doi: 10.1111/j.1834-7819.1992.tb00758.x. [DOI] [PubMed] [Google Scholar]
- 28.Methathrathip D, Apinhasmit W, Chompoopong S, Lertsirithong A, Ariyawatkul T, Sangvichien S, et al. Anatomy of greater palatine foramen and canal and pterygopalatine fossa in Thais: Considerations for maxillary nerve block. Surg Radiol Anat. 2005;27:511–6. doi: 10.1007/s00276-005-0016-5. [DOI] [PubMed] [Google Scholar]
- 29.Wormald PJ, Athanasiadis T, Rees G, Robinson S. An evaluation of effect of pterygopalatine fossa injection with local anaesthetic and adrenalin in the control of nasal bleeding during endoscopic sinus surgery. Am J Rhinol. 2005;19:288–92. [PubMed] [Google Scholar]
- 30.Wormald PJ, Wee DT, van Hasselt CA. Endoscopic ligation of the sphenopalatine artery for refractory posterior epistaxis. Am J Rhinol. 2000;14:261–4. doi: 10.2500/105065800779954455. [DOI] [PubMed] [Google Scholar]
- 31.Jonas N, Viani L, Walsh M. Sphenopalatine artery ligation under local anesthesia: A report of two cases and review of the literature. Local Reg Anesth. 2010;3:1–4. doi: 10.2147/lra.s6770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sharma NA, Garud RS. Greater palatine foramen-key to successful hemimaxillary anaesthesia: A morphometric study and report of a rare aberration. Singapore Med J. 2013;54:152–9. doi: 10.11622/smedj.2013052. [DOI] [PubMed] [Google Scholar]
- 33.Poore TE, Carney MT. Maxillary nerve block: A useful technique. J Oral Surg. 1973;31:749–54. [PubMed] [Google Scholar]
- 34.Douglas R, Wormald PJ. Pterygopalatine fossa infiltration through the greater palatine foramen: Where to bend the needle. Laryngoscope. 2006;116:1255–7. doi: 10.1097/01.mlg.0000226005.43817.a2. [DOI] [PubMed] [Google Scholar]


