Abstract
Background:
Cerebral palsy (CP) is described as a group of conditions usually occurring in childhood, where children have motor dysfunction and are unable to adequately master the necessary techniques of plaque control, which ultimately leads to dental caries and periodontal problems.
Aims:
The objective of this study was to educate the parents/caretakers/institution staff and children with CP about the different preventive home care measures and to evaluate the oral hygiene and gingival health status of these children before and after the institution of different preventive home care measures.
Materials and Methods:
A total of 64 individuals with CP, aged between 6 and 18 years, were examined for their oral hygiene and gingival health status, after which the parents/caretakers received a health education program. The children were then randomly divided into four groups. Each group was administered a specific preventive home care measure (mechanical and chemotherapeutic) to be followed for a period of 6 weeks, and the oral hygiene and the gingival health status were recorded at the end of 1 week, 2 weeks, and 6 weeks. The data were then subjected to statistical analysis.
Results:
In the sample of 64 children diagnosed with CP, the mean OHI(S) score among the groups of children who were given different preventive home care measures was compared at baseline, 1 week, 2 weeks, and 6 weeks. Group 4 showed a marked reduction in the OHI(S) score measured from baseline to 6 weeks, when compared to the other three groups which wa statistically very highly significant (P < 0.001) The mean MGI score was compared at baseline, 1 week, 2 weeks, and 6 weeks home, Group 4 showed a marked reduction in the MGI score measured from baseline to 6 weeks, when compared to the other three groups. When the mean MGI score was compared from baseline to 6 weeks, there was a gradual decrease in the MGI score, which was statistically highly significant between baseline and 1 week (P < 0.05) and statistically very highly significant between 1 and 2 weeks (P < 0.001). However, this improvement was not statistically significant between 2 and 6 weeks (P > 0.05).
Conclusion:
A combined mechanical and chemotherapeutic measure is highly recommended to maintain the oral hygiene and gingival health of these special children because of their difficulties and their limited abilities to control dental plaque.
Keywords: Cerebral palsy, gingival health status, oral hygiene status, plaque control methods
INTRODUCTION
Cerebral palsy (CP) is a neuromuscular disorder which is defined as a group of disorders of development of posture and movement, causing limitations in activity that are attributable to non-progressive disturbances which have occurred in the developing fetal or infant brain.[1] The neuromuscular problems inherent in CP can affect the oral health significantly, such as changes in structure of the oro-facial region, development of para-functional habits, feeding problems, difficulty with maintaining oral hygiene, and encountering barriers to oral care access.[2] The process of developing gingival and periodontal diseases in disabled individuals does not differ from that in non-disabled individuals. The main factor related to gingival/periodontal problems in disabled individuals is the inadequacy of plaque removal from the teeth. Motor incoordination problems and muscular limitation in neuromuscularly disabled individuals, along with difficulty in understanding the importance of oral hygiene in these individuals result in the progression of inflammatory disease. Hence, it is perceived that by establishing an early contact with CP children, certain preventive home care measures can be introduced so as to prevent major oral health concerns.[3] The maintenance of good oral hygiene in these children by tooth brushing is not completely possible owing to the limited manual dexterity and skill of these children. As a result, chemical plaque control has been recommended as an alternative and adjunctive to mechanical plaque control in these special patient groups and chlorhexidine gluconate (CHX) may be one of the best answers in this regard.[4] In CP patients, the advantages of CHX spray application are ease of use, effective plaque control, reduced adverse effects, and also reduced swallowing problems.[3]
Previous studies on these children have reflected their poor oral hygiene and suggested that not much attention is given to improve the oral hygiene in these children.[5,6,7] These facts reinforce the need to study the effects of various oral hygiene measures on the symptoms of gingival inflammation and to evaluate the effectiveness of combined oral hygiene strategies (CHX as an adjunct to manual and powered toothbrushes) in elimination of dental plaque and its sequel in CP children. Hence, this study was formulated.
MATERIALS AND METHODS
This was a randomized, open-blinded study. Two special schools in the city of Bangalore, India, dealing with CP children were included in the study, after informed consent was obtained from the school authorities. There were a total of 73 children diagnosed with CP in these schools. All the children along with their caretakers and parents were invited to participate in the study. The children were between the ages of 6 and 18 years. Children with severe neuromuscular incoordination as per the classification given by Palisano et al.,[8] children who were unable to cooperate, and those whose parents were not willing to participate were excluded from the study. After considering all the exclusion criteria, 64 children were included in the study population. Ethical approval was obtained from the ethical committee of the respective university.
During the first visit, the children were accompanied by their parents/caretakers. The children were examined in their respective schools, seated on an ordinary chair, unless confined to a wheel chair, under natural light using sterile instruments, during which the baseline data of oral hygiene index simplified [OHI (S)][9] and modified gingival index (MGI)[10] were recorded.
The parents/caretakers/institution staff were then administered a health education program including the importance of oral hygiene maintenance and knowledge regarding the four preventive home care measures that were included as a part of the present study, and these four measures were divided among four groups of the study population.
The children who were part of the study were randomly divided into four groups of 16 children each as follows:
Group 1: Manual toothbrush with fluoridated toothpaste
Group 2: Manual toothbrush with fluoridated toothpaste and CHX spray
Group 3: Powered toothbrush with fluoridated toothpaste
Group 4: Powered toothbrush with fluoridated toothpaste and CHX spray.
A toothbrush (manual or powered as per the group), fluoridated toothpaste, and a custom-made CHX spray were provided to the parents/caretakers. Horizontal tooth brushing with manual toothbrush and the correct usage of powered toothbrush with pea-sized amount of fluoridated toothpaste was advised to be performed twice daily (once in the morning and the other time in the night following dinner) by the parents/caretakers. The caretakers were requested to complete the activity of brushing in 2 min.[11]
The parents/caretakers applied the custom-made 0.2% CHX spray formulations (a total of 12 sprays were applied), one each on the buccal and the lingual surfaces of each arch on a twice-daily basis after half an hour of tooth brushing. The CHX spray was applied half an hour after tooth brushing to prevent any possible interaction with the anionic ingredients present in the toothpaste and competition for oral retention sites.[4] The children in the group who were asked to use CHX spray were instructed to stop the usage of the spray at the end of 1 week and continue tooth brushing alone, because of the reported short-term side effects of chlorhexidine.[12]
Preventive home care measures were advised to be followed for a period of 6 weeks. The oral hygiene and the gingival health status were recorded at baseline and the end of 1 week, 2 weeks, and 6 weeks using OHI(S) and MGI indices, respectively. All the data were subjected to statistical analysis using SPSS 19. One-way analysis of variance (ANOVA) was used for intergroup comparison of oral hygiene and gingival status. Paired t-test was used for comparison of oral hygiene and gingival status from baseline to 6 weeks within each group.
RESULTS
A total of 64 CP children between the ages of 6 years and 18 years were studied, of whom 42 (65.2%) were males and 22 (34.8%) were females. The OHI(S) and MGI indices were scored to evaluate the oral hygiene status and gingival inflammation status in these children at the onset and after educating and administering the preventive oral hygiene measures over a period of 6 weeks.
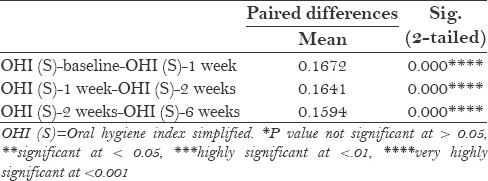
In the sample of 64 children diagnosed with CP, the mean OHI (S) score among the groups of children who were given different preventive home care measures was compared at baseline, 1 week, 2 weeks, and 6 weeks. Group 4 [Table 1 and 2] showed a marked reduction in the OHI (S) score measured from baseline to 6 weeks, when compared to the other three groups. The results were statistically very highly significant (P < 0.001) [Table 3].
Table 1.
OHI (S) score at baseline (B), 1 week, 2 weeks, and 6 weeks
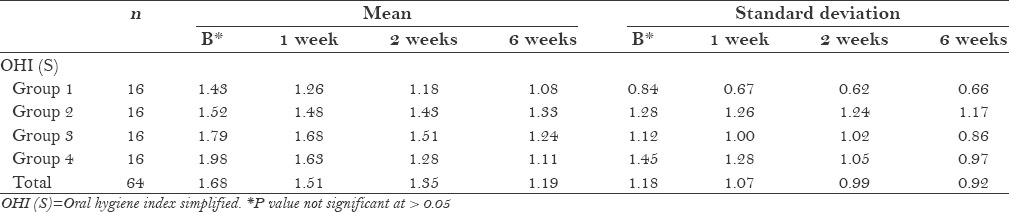
Table 2.
Intergroup comparison of OHI (S) scores at baseline, 1 week, 2 weeks, and 6 weeks
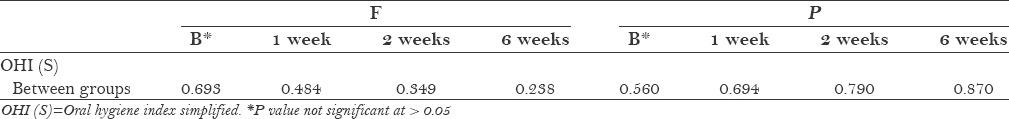
Table 3.
Comparison of OHI (S) scores from baseline to 6 weeks
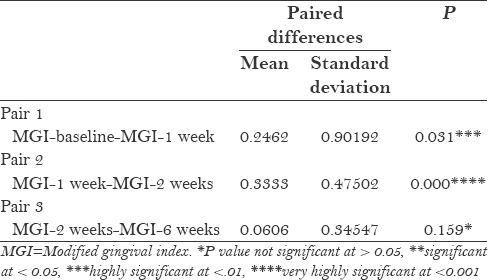
In the sample of 64 CP children, the mean MGI score was compared at baseline, 1 week, 2 weeks, and 6 weeks among the groups of children who were administered different preventive home care measures. Group 4 [Table 4 and 5] showed a marked reduction in the MGI score measured from baseline to 6 weeks, when compared to the other three groups. When the mean MGI score was compared from baseline to 6 weeks, there was a gradual decrease in the MGI score, which was statistically highly significant between baseline and 1 week (P < 0.05) and statistically very highly significant between 1 and 2 weeks (P < 0.001). However, this improvement was not statistically significant between 2 and 6 weeks (P > 0.05) [Table 6].
Table 4.
MGI scores at baseline, 1 week, 2 weeks, and 6 weeks
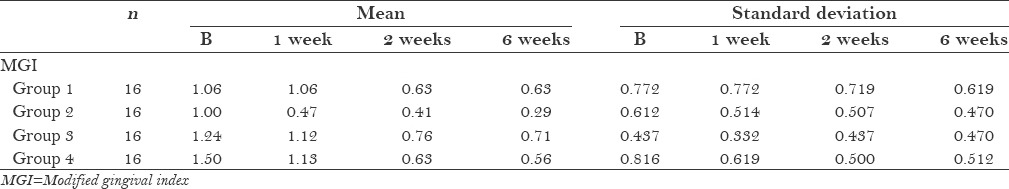
Table 5.
Intergroup comparison of MGI scores at baseline, 1 week, 2 weeks, and 6 weeks
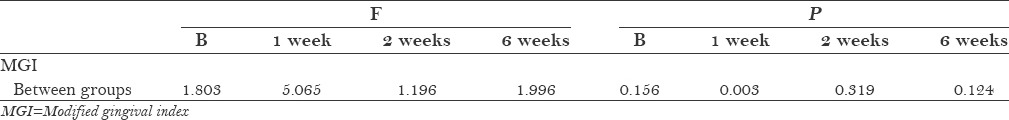
Table 6.
Comparison of MGI scores from baseline to 6 weeks
DISCUSSION
CP is a term used to describe a group of disorders of movement, muscle tone, or other features that reflect abnormal control over motor function by the central nervous system.[13] Developmentally disabled children have poor oral health and the main factor related to the gingival and periodontal problems in disabled children is the inadequacy of the plaque removal from the teeth. Tooth brushing (using manual/powered toothbrush) in developmentally disabled individuals may be difficult because of motor coordination problems and muscular limitation. Some studies have evaluated CHX as a plaque control agent when used as a mouth rinse, spray, or gel. Each of these delivery methods was found to lower the plaque levels below those achieved with routine tooth brushing. CHX spray application may be an ideal adjunct to provide a degree of control commensurate with good oral health in developmentally disabled patients because of its simple use and effectiveness on plaque control. Hence, it is clear that developmentally disabled individuals require a technique that is easy to use and reliable, in order to achieve some degree of acceptable plaque control.[3]
A total of 64 CP children aged between 6 years and 18 years were studied, including 42 males and 22 females.
In the present study, we compared the children who used powered toothbrushes to those using manual toothbrushes along with fluoridated toothpaste with or without CHX spray. The results showed a marked reduction in the OHI (S) scores in the group using powered toothbrush, fluoridated toothpaste, and CHX spray. The superior action of powered toothbrush could be because of the ease of using powered toothbrush and the smaller size of the brush head. These toothbrushes require lesser effort on the part of the patient by virtue of their automated action. Their machined rotatory bristles offer the necessary movement for removal of plaque, an action similar to that performed by the patient's hand in case of a manual toothbrush, without the patient's personal physical effort.[11] The gradual and lesser significant decrease in the OHI (S) scores noticed with manual toothbrush which was clinically evident was in accordance with the study by Haffajjee et al.,[13] where the powered toothbrush significantly reduced the plaque index score in a 6-week time interval, suggesting that powered toothbrush delivers superior plaque control compared to manual toothbrush.
Intergroup comparison of the post application scores of OHI (S) following different preventive home care measures showed no statistical significant difference, suggesting that no group had a greater improvement than the other.
In the present study, we compared the children who used powered toothbrushes to those using manual toothbrushes along with fluoridated toothpaste with or without CHX spray. The results showed a marked reduction in the MGI scores in the group using powered toothbrush, fluoridated toothpaste and CHX spray.
Intergroup comparison of MGI scores from baseline to 6 weeks showed statistically highly significant difference between baseline and 1 week and statistically very highly significant difference between 1 week and 2 weeks. However, the difference at the end of 2 weeks and 6 weeks was not statistically significant, the reason being that the groups using CHX spray were instructed to stop the usage of spray at the end of 1 week and continue with the tooth brushing alone as instructed for the rest of the study period. The above finding is in accordance with the study done by Bozkurt et al.[3] where the oral hygiene status and gingival health status were reported to improve in the nueromuscularly disabled children over a period of 3 weeks when the children used powered tooth brush and CHX spray, suggesting that CHX was an effective chemical plaque control agent in improving the gingival health and could be used as an adjuvant to the mechanical methods of maintaining oral hygiene.
The present study reveals the generalized reduction of gingivitis and plaque formation independent of the type of brush used and the recommended the use of combined oral hygiene strategies. Probable explanation for the same could be related to the supervised brushing, which was performed in these developmentally disabled individuals as they lacked manual dexterity, suffered co-operation difficulties, and had confounding medical conditions along with poor oral health. The CHX spray application when used as an adjunct along with its antibacterial activity also inhibits plaque and is highly recommended in these developmentally disabled children. Irrespective of the brush used, supervised brushing along with CHX spray can be recommended for better oral health in these children. However, long-term studies are required to assess the oral hygiene and the gingival health status of these children and also the alternate delivery systems of CHX could be used.
CONCLUSION
There was a general improvement in oral hygiene and gingival health status of all the children following the combined oral hygiene strategies
A combined mechanical and chemotherapeutic measure is highly recommended to maintain the oral hygiene of these special children.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Scully C, Cawson RA. Neurological disorders I: Epilepsy, stroke and craniofacial neuropathies. In: Scully C, Cawson RA, editors. Medical Problems in Dentistry. 5th ed. Philadelphia: Elsevier, Churchill Livingstone; 2005. pp. 297–8. [Google Scholar]
- 2.Dougherty NJ. A review of cerebral palsy for the oral health professional. Dent Clin North Am. 2009;53:329–38. doi: 10.1016/j.cden.2008.12.001. x. [DOI] [PubMed] [Google Scholar]
- 3.Bozkurt FY, Fentoglu O, Yetkin Z. The comparison of various oral hygiene strategies in nueromuscularly disabled individuals. J Contemp Dent Pract. 2004;5:23–31. [PubMed] [Google Scholar]
- 4.Balagopal S, Arjunkumar R. Chlorhexidine: The gold standard antiplaque agent. J Pharm Sci Res. 2013;5:270–4. [Google Scholar]
- 5.Nallegowda M, Mathur V, Singh U, Prakash H, Khanna M, Sachdev G, et al. Oral health status in Indian children with cerebral palsy-a pilot study. IJPMR. 2005;16:1–4. [Google Scholar]
- 6.Rodrigues dos Santos MT, Masiero D, Novo NF, Simionato MR. Oral conditions in children with cerebral palsy. J Dent Child (Chic) 2003;70:40–6. [PubMed] [Google Scholar]
- 7.Dos Santos MT, Nogueira ML. Infantile reflexes and their effects on dental caries and oral hygiene in cerebral palsy individuals. J Oral Rehabil. 2005;32:880–5. doi: 10.1111/j.1365-2842.2005.01518.x. [DOI] [PubMed] [Google Scholar]
- 8.Wood E, Rosenbaum P. The gross motor function classification system for cerebral palsy: A study of reliability and stability over time. Dev Med Child Neurol. 2000;42:292–6. doi: 10.1017/s0012162200000529. [DOI] [PubMed] [Google Scholar]
- 9.Greene JC, Vermillon JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:7–13. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 10.Newman MG, Takei HH, Carranza FA. 9th ed. Philadelphia: Saunders An imprint of Elsevier; 2004. Clinical Periodontology; pp. 79–80. [Google Scholar]
- 11.Goyal S, Thomas BS, Bhat KM, Bhat GS. Manual toothbrushing reinforced with audiovisual instruction versus powered toothbrushing among institutionalized mentally challenged subjects-a randomized cross-over clinical trial. Med Oral Patol Oral Cir Bucal. 2011;16:e359–64. doi: 10.4317/medoral.16.e359. [DOI] [PubMed] [Google Scholar]
- 12.Gürgan CA, Zaim E, Bakirsoy I, Soykan E. Short-term side effects of 0.2% alcohol-free chlorhexidine mouthrinse used as an adjunct to non-surgical periodontal treatment: A double-blind clinical study. J Periodontol. 2006;77:370–84. doi: 10.1902/jop.2006.050141. [DOI] [PubMed] [Google Scholar]
- 13.Haffajee AD, Thompson M, Torresyap G, Guerrero D, Socransky SS. Efficacy of manual and powered toothbrushes (I). Effect on clinical parameters. J Clin Periodontol. 2001;28:937–46. doi: 10.1034/j.1600-051x.2001.028010937.x. [DOI] [PubMed] [Google Scholar]


