Abstract
The seven dimensions of quality of life are required for a healthy living. Any impairment or disability affects any one or more of these dimensions resulting in functional impairment or handicap, which indicates the presence of disease. The success of any oral treatment depends on how far the individual is relieved of his disease process. Relief of symptoms provides patient comfort and enable functional activities. This well-being is considered as a measure of oral health and reflects patient satisfaction. This article presents various instruments or tools available in the form of a questionnaire that estimates patient satisfaction and thereby oral health.
KEY WORDS: Oral health, patient satisfaction, quality of life
The tooth loss has an effect on the general health, general well-being, and psychosocial behavior of the patients.[1] The general health is affected due to the diminished intake of healthy diets owing to the reduced chewing ability.[2] The general well-being refers to the comfort and the confidence the patient exhibits after treatment. The psychosocial behavior depends on the patient's ability to interact and communicate without the feeling of disability. The restoration and replacement of teeth reduce these ill effects and improve the quality of life (QoL).[3] Any therapy is targeted at increasing their oral health and well-being. The patient's comfort is more vital to the acceptance of any intervention. Patient's acceptance, in other words, is patient satisfaction. The QoL is an estimate of patient satisfaction.
Several tools for evaluating of patient satisfaction are in practice. These tools measure oral health as an indicator of patient satisfaction. Each instrument gives unique results. Few tools have been tested, validated and are used during clinical trials. This article highlights various tools available for rating the patient satisfaction for various dental interventions. The following tools are in practice for measuring oral health and patient satisfaction.
The Social Impacts of Dental Disease
The social impacts of dental disease (SIDD) was the first attempt to measure dental impact on oral health and was developed in 1980.[4] This tool measures the dissatisfaction following the disease and health related issues on people. Wolinsky and Wolinsky constructed a health model based on physical, social and psychological aspects.[5] These aspects were used to construct the social impact of dental disease index. The SIDD index helps to evaluate the background and behavioral factors, namely vulnerability, motivational and preventive dimensions:
The vulnerability relates to socio-economic background, current home and work circumstances, dental history and experiences and access to dental service
Motivational dimension is beliefs, attitudes, concerns and expectation about dental health
Preventive dimension measures current dental practice such as self-care measures to improve dental health and prevent tooth loss.
The social and psychological aspect of dental diseases were divided into five categories namely eating restrictions, communication restrictions, pain, discomfort and esthetics. All these categories are measured from 0 to 5 except discomfort, which is measured from 0 to 4.
Limitations
Social impacts of dental disease evaluates the impact but not the severity. Hence further tools were developed to measure QoL.
Oral Health and Sickness Impact Profile
The sickness impact profile (SIP) was developed in 1970 and is used to measure sickness related issues perceived and reported by health care workers.[6] It is a behavior based health status.[7] The final version of SIP consists of 136-item and 12 subscales, which include sleep and rest, eating, home management, work, recreation, ambulatory status, emotional behavior, affective behavior, social interaction and communication. SIP has been used in cardiovascular, neurologic, internal, pain and musculoskeletal disorders and functional status of elderly individuals.
Uses
To assess the health of population, evaluate medical care program, evaluate treatment program, planning and program development, assessing individual health status and response to health care
Used in the mail, telephone surveys.[8]
Limitations
Elaborate and lengthy tool
Limited applications in dentistry due to lack of sensitivity.
Dental Health Questions from Rand Health Insurance Study
Health status measurement became advanced in 1980. Health Insurance Study (HIS) was developed by Ware, Brook, Brook et al.[9] The purpose of the study was to measure the effect of cost – sharing on the patient, health status, quality of care, utilization and cost of services. Physical, mental, social health and general health were also evaluated. A three impact question was also added to the questionnaire, which were directly related to the dental disease: Pain, worry and social interactions. This tool helps to evaluate adverse effects of dental diseases on individuals.
Questions can be avoided by responding like none of the time to most of the time. A 3-item index was constructed to analyze the pschyo social impact of oral conditions on the participants. The dental diseases assessed by HIS were pain and distress, worry or concern and reduced social interactions.
Uses
It is an insurance-based study
Measures effectiveness of interventions.
Limitations
It has limited measures of self-reported dental health
Less applications in dentistry.
Geriatric Oral Health Assessment Index
Geriatric Oral Health Assessment Index (GOHAI) measures patient reported oral functional problems. It was developed to measure the degree of psychosocial impact associated with oral diseases. It is used to evaluate the effectiveness of dental treatment. It includes items regarding freedom from pain and infection, patient ability to continue to their social roles. Initial items consist of a pilot instrument of 36-item[10] and final instrument containing 12-item were chosen.
The final scoring for 9-item has reverse scorings. Hence, the final scores for GOHAI represent more positive oral health. If the respondents do not respond to more than 3-item, their data becomes invalid and not considered for statistical analysis. Each final score of the 12-item is added to give the final scores. So GOHAI score usually ranges from 0 to 60.
Geriatric Oral Health Assessment Index has been alternatively used with three sets of response categories 3, 5 and 6 categories.[11,12] The 3 response category gives an acceptable information of the patients oral health. The 5 response category helps in clinical judgment and to determine which problem occurs with more frequency.
Uses
Indicates patients socio-economic status
It is useful for evaluating the effectiveness of dental treatment
Can be used in a younger generation also.
The term geriatric is now changed to General Oral Health Assessment Index.
Dental Impact Profile
Dental impact profile (DIP) was developed to evaluate how much do teeth and mouth have an impact in people's life.[12] The DIP indicates how QoL is affected, detracted or enhanced by oral health and oral structures. DIP is also a self-reported questionnaire. This set of questionnaire was developed by questioning and interviewing dentists, scientists and consumers. Initially 37-item were tested among elderly and college respondents and was later reduced to 25-item. The pilot study was done among the aged population and determined whether race, age and education influenced DIP. A good effect means most socially acceptable response of no effect means no dental effect. Subscales were developed to refine the psychometric scale. Test, retest is not done in DIP. It was found that impact on appearance, chewing and eating were more common. DIP was done on the different population to determine racial and ethnic effects. The population study revealed ethnic differences indicating that racial differences could affect the scores of DIP.
Uses
Dental impact profile was the first tool to introduce the concept that teeth and dentures have more positive and negative impact on life. It serves as an indicator to prove that, teeth are important for better life to an individual or population[13]
It helps the patients to appreciate and evaluate their dentition
DIP is brief and simple
Evaluates racial and ethnic influence on patient's life.[14]
Oral Health Impact Profile
Oral health impact profile (OHIP) is a tool for measuring the oral health[15] and measure the amount of burden relieved after a dental intervention.[16] OHIP is a self-reported measure of discomfort dysfunction and disability related to oral diseases. OHIP is associated with impairment. OHIP represents 4 out of seven QoL dimensions. It excludes perception of satisfaction, changes in oral health, prognosis or self-reported diagnosis. Lockers model of oral health was used to define 7 dimensions of oral health.
Oral health impact profile consists of 49 statements. Respondents were asked to respond on a five-point Likert's scale like never, hardly ever, occasionally, fairly often, very often. Respondents are given an option of don’t know. For few questions, a separate response option is provided for nondenture users. However the responses like “Don’t know” are entered as missing values which are recoded with average values of all responses. If nine responses are left blank or responded as don’t know the questionnaire is not included for statistical calculations.
Overall OHIP scores can be calculated in two ways. The first method is to count the number of impacts reported. The second method calculates the overall OHIP scores to standardize the subscale scores. The second method is usually done by computer programming. The reliability of OHIP varies among the different population. OHIP studies reveal edentulous patients have higher scores for functional and physical disability.
The number of missing items can be reduced with the interviewer version of OHIP. If the respondents questionnaire had one missing value or one blank entry, the blank entry was filled by the mean values of the sample. If more than 9 blank responses were noted then the response is discarded and not taken for statistical data. The OHIP scores are usually high, for patients with poor clinical oral status,[17] socially and economically disadvantage groups,[18] older adults,[19] HIV patients.[20] A shortened version with 14-item and a French and Spanish forms are available.[21]
Uses
Allows for a more elaborate evaluation of oral health
Used as a tool for outcome measure
Most commonly used questionnaire.
Subjective Oral Health Status Indicators
This was developed in Canada based on World Health Organization (WHO) model of oral disease and handicap[22] to estimate functional, social and psychological outcomes. It was initially used in oral health surveys of elderly people, but the abbreviated versions were used in the studies of adolescent and adult population. The aim of developing this tool was to identify the links between oral disease and the treatment outcomes.
It consists of 4 indexes and one scale. Among the 4 indexes one index denotes chewing capacity derived by Leake,[23] Index of oral and facial pain, index of oral symptoms, developed by Locker and Gruskha[24] and a psychosocial impact scale that is based on questions used in the Rand Health Insurance experiment that measures the effect of oral conditions on eating and social conditions.
Though these tools were applied to elderly patients, test-retest reliability indicated that these tools are generalizable and can be well used in younger adults also. This tool was efficient in obtaining the responses, and the nonresponse was noted in only 5% of the respondents. Hence, the efficiency rate is also high.
Uses
It is used for personal and telephone interview service
It is useful in descriptive surveys
It explores links between different dimensions of health
They are easy to complete and hence the response rate is high.
Limitations
It cannot be used as an outcome measure in clinical trials or evaluated studies.
Oral Health Quality of Life
Oral health quality of life (OHQoL) was developed in 1991 by a group of investigators who used questions that were related to oral health and QoL.[25] It consists of a pool of 3-item. Three items that were included in OHQoL were focused on daily work and social activities and communication problems.
The response for each item was collected on a six-point scale from all of a time to none of the time. It also contains 2-item for oral discomfort and scoring is on a five-point scale ranging from never to very often and 2-item from nutrition screening initiative (response yes or no format) assessing eating problems.
Oral health quality of life consists of eight factors, which include physical, emotional and social functioning, emotional, mental health, vitality, pain and general health. The 5th factor contributes to 5% of the variance. So this suggests that the impact of physical health on OHQoL is different from the impact of oral health on OHQoL. A Cronbach's alpha coefficient of 0.83, suggests a strong association between the general life satisfaction, oral discomfort and eating problem. Individuals with better oral health QoL had fewer eating problems and less discomfort combined with less dental pain and sought less dental treatment.
Uses
This brief tool is very ideal for population studies and surveys.
Limitations
It does asses the details of disease[26] and its impact on life.
Dental Impact on Daily Living
Developed by Leao and Sheiham,[27] DIDP is used to assess the importance that the respondents give to different dimensions of life. It is socio dental measure that assess oral impact on daily living. These questions were from interviews, literature review, and partly from SIDD. The scoring of the impacts was coded from negative to positive. If the final scoring is between 7 and 10 then the individual is satisfied, −6.9–0 indicates relatively satisfied and 0 indicates unsatisfied individuals. According to this tool, the dimension of appearance had a negative impact on QoL. But improvements on the dental impact on daily living are under research.
Oral Health Quality of Life Inventory
It is a 15-item dental specific measure that assesses a patient satisfaction with his or her oral health and functional status and the importance associated with it.[28] The specific aims of the study are to evaluate the impact of oral health and functional status on QoL and subjective and objective oral health and functional status to assess the overall QoL.
The 15-item scale includes a home –based interview, and a self-reported questionnaire of oral health and functional status, a nutritional QoL index and an interview version of the QoL inventory. The overall score ranges from −4 to +4. The final QoL inventory consists of 40 SROH items (sample oral pain items), 15OHQoL and 9 nutrition OHQoL items, which include a total 66-item in the final scale of OHQoL.
Alternate forms of OHQoL included San Antonio Longitudinal Study of Aging, a survey of Spanish speaking and English speaking Mexican American and English speaking European American.
Uses
To assess the subjective and objective functional status of an individual's oral health and also assesses the QoL
Separate scales and questionnaires for denture wearers makes it an easier tool for evaluating QoL after a prosthodontic intervention.
Oral Impact on Daily Performance
Oral impact on daily performance (OIDP) is an alternative socio dental tool[29] which evaluates the oral impact on person's ability to perform daily activities. Locker modified OIDP[30] by WHO's international classification of impairments, disabilities and handicaps. It includes three levels:
Level 1 - Oral status which includes oral impairment
Level 2 - “The intermediate impacts: The negative impacts on oral status like pain, discomfort etc
Level 3 - Evaluates physical, social and physiological performances.
The final scale consists of eight performances. The scoring is from 0 to 5 which represents periodic and spell pattern. Fractional response is not permitted. The alternate form was found to be a better predictor for detecting DMFT and also for detecting deep periodontal pockets.
Discussion
Patrick and Bergner proposed seven QoL dimensions[31] based on lockers model. The seven dimensions are physical diability, psychological disability, social disability, functional limitation, physical pain, psychological discomfort and handicap. This is based on WHO of handicap. Each tool helps is assessing different dimensions. The term items refer to set of questionnaires, indicators, etc., summary of different tools are listed in Table 1.
Table 1.
Summary of various tools for oral health assesment
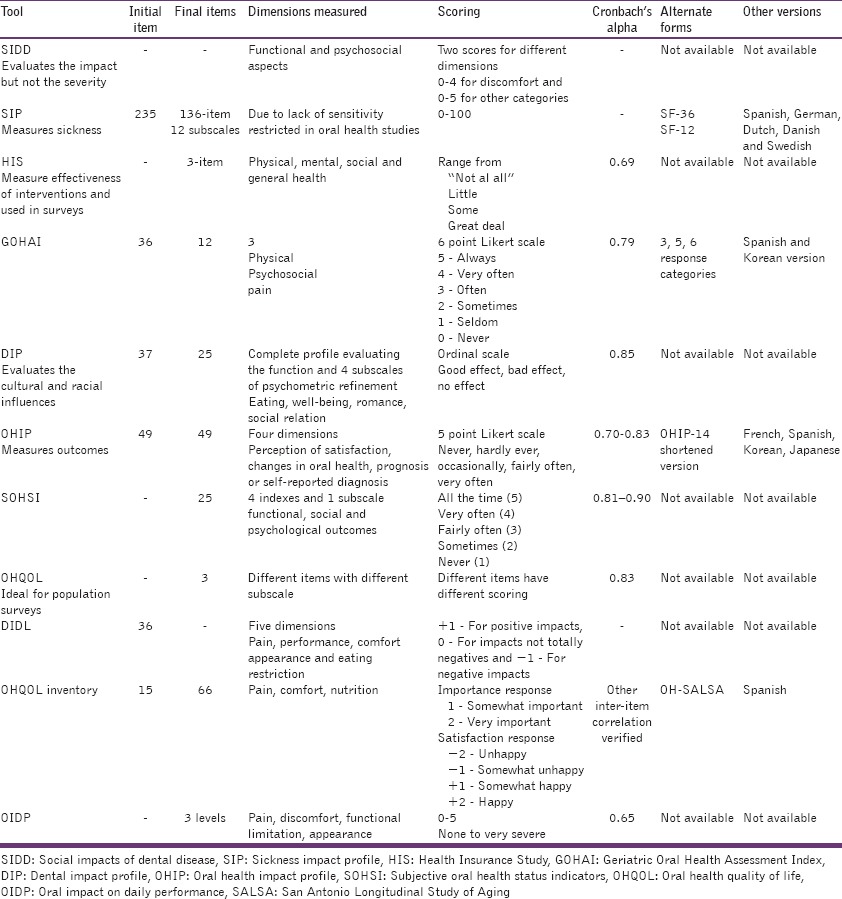
The tools for measuring oral health were validated and checked for reliability. Generalizability indicates that the tools are applicable for all age groups and ethnic populations. The efficiency of the study indicates the simplicity of the questionnaire and thereby obtaining maximum responses. Cronbach's α correlation indicates an estimate of reliability and hence higher Cronbach's value, higher the reliability of the questionnaire.
The term QoL includes a broader perspective. It includes all the dimensions of life namely comfort, impairment and social well-being. A good QoL reflects good health and better satisfaction of the patient. One of the biggest challenges is to calibrate the patient satisfaction after treatment. Different interventions result in different levels of patient satisfaction. The method of assessment should also vary according to the type of treatment.
The major limitations of this questionnaire are that they are self-reported. Certain items of the questionnaire may not be responded by the subject and values for those blank entries are computed by taking the average score. This may not reflect the actual patient satisfaction. In case of trials, where measuring outcomes is required, objective evaluation should be supported by an elaborate subjective evaluation to provide high quality of evidence. The questionnaires scores do not include subjective evaluation.
Conclusion
The WHO recommends seven QoL dimensions to measure oral health and QoL. The tools used do not include all seven dimensions. The inclusion of all seven dimensions appears to be an elaborate and lengthy tool. However, tools like OHIP are more commonly used for outcome evaluation and surveys with acceptable results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Zenthöfer A, Rammelsberg P, Cabrera T, Schröder J, Hassel AJ. Determinants of oral health-related quality of life of the institutionalized elderly. Psychogeriatrics. 2014;14:247–54. doi: 10.1111/psyg.12077. [DOI] [PubMed] [Google Scholar]
- 2.Ilhan B, Cal E, Dündar N, Güneri P, Daghan S. Oral health-related quality of life among institutionalized patients after dental rehabilitation. Geriatr Gerontol Int. 2014 Nov 19; doi: 10.1111/ggi.12413. DOI: 10.1111/ggi.12413. [DOI] [PubMed] [Google Scholar]
- 3.Sivakumar I, Sajjan S, Ramaraju AV, Rao B. Changes in oral health-related quality of life in elderly edentulous patients after complete denture therapy and possible role of their initial expectation: A follow-up study. J Prosthodont. 2014 Dec 18; doi: 10.1111/jopr.12238. DOI: 10.1111/jopr12238. [DOI] [PubMed] [Google Scholar]
- 4.Cushing AM, Sheiham A, Maizels J. Developing socio-dental indicators - The social impact of dental disease. Community Dent Health. 1986;3:3–17. [PubMed] [Google Scholar]
- 5.Wolinsky FD, Wolinsky SR. Background, attitudinal and behavioural patterns of individuals occupying eight discrete health states. Sociol Health Illn. 1981;3:31–48. doi: 10.1111/1467-9566.ep11343599. [DOI] [PubMed] [Google Scholar]
- 6.Bergner M, Bobbitt RA, Carter WB, Gilson BS. The Sickness Impact Profile: Development and final revision of a health status measure. Med Care. 1981;19:787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Pollard WE, Bobbitt RA, Bergner M, Martin DP, Gilson BS. The Sickness Impact Profile: Reliability of a health status measure. Med Care. 1976;14:146–55. doi: 10.1097/00005650-197602000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Bergner M. Development, testing and use of the Sickness Impact Profile. In: Walker SR, Rosser RM, editors. Quality of Life: Assessment and Applications (79-94) Lancaster: MTP Press Limited; 1987. [Google Scholar]
- 9.Brook RH, Ware JE, Jr, Davies-Avery A, Stewart AL, Donald CA, Rogers WH, et al. Overview of adult health measures fielded in Rand's Health Insurance Study. Med Care. 1979;17(7 Suppl):iii–x. 1-131. [PubMed] [Google Scholar]
- 10.Atchison KA, Dolan TA. Development of the Geriatric Oral Health Assessment Index. J Dent Educ. 1990;54:680–7. [PubMed] [Google Scholar]
- 11.Kressin NR. Associations among different assessments of oral health outcomes. J Dent Educ. 1996;60:501–7. [PubMed] [Google Scholar]
- 12.Calabrese JM, Friedman PK, Rose L, Jones JA. Oral health assessment of a frail elderly homebound population. J Dent Res. 1996;75 (IADR Abstracts):152, Abstract No. 1078. [Google Scholar]
- 13.Strauss RP, Hunt RJ. Understanding the value of teeth to older adults: Influences on the quality of life. J Am Dent Assoc. 1993;124:105–10. doi: 10.14219/jada.archive.1993.0019. [DOI] [PubMed] [Google Scholar]
- 14.Hunt RJ, Slade GD, Strauss RP. Racial variations in the impact of oral disorders in older adults. J Dent Res. 1993;72(special issue, 72) Abstract #1295:265. [Google Scholar]
- 15.Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health. 1994;11:3–11. [PubMed] [Google Scholar]
- 16.Tugwell P, Bennett KJ, Sackett D, Haynes B. Relative risks, benefits and costs of intervention. In: Warren KS, Mahmoud AA, editors. Tropical and Geographic Medicine. New York: McGraw Hill; 1985. pp. 1097–113. [Google Scholar]
- 17.Slade GD, Spencer AJ, Locker D, Hunt RJ, Strauss RP, Beck JD. Variations in the social impact of oral conditions among older adults in South Australia, Ontario, and North Carolina. J Dent Res. 1996;75:1439–50. doi: 10.1177/00220345960750070301. [DOI] [PubMed] [Google Scholar]
- 18.Locker D, Slade G. Association between clinical and subjective indicators of oral health status in an older adult population. Gerodontology. 1994;11:108–14. doi: 10.1111/j.1741-2358.1994.tb00116.x. [DOI] [PubMed] [Google Scholar]
- 19.Slade GD, Spencer AJ. Social impact of oral conditions among older adults. Aust Dent J. 1994;39:358–64. doi: 10.1111/j.1834-7819.1994.tb03106.x. [DOI] [PubMed] [Google Scholar]
- 20.Coates E, Slade GD, Goss AN, Gorkic E. Oral conditions and their social impact among HIV dental patients. Aust Dent J. 1996;41:33–6. doi: 10.1111/j.1834-7819.1996.tb05652.x. [DOI] [PubMed] [Google Scholar]
- 21.Slade GD. Derivation and validation of a short-form oral health impact profile. Community Dent Oral Epidemiol. 1997;25:284–90. doi: 10.1111/j.1600-0528.1997.tb00941.x. [DOI] [PubMed] [Google Scholar]
- 22.Locker D. Measuring oral health: A conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- 23.Leake JL. An index of chewing ability. J Public Health Dent. 1990;50:262–7. doi: 10.1111/j.1752-7325.1990.tb02133.x. [DOI] [PubMed] [Google Scholar]
- 24.Locker D, Grushka M. Prevalence of oral and facial pain and discomfort: Preliminary results of a mail survey. Community Dent Oral Epidemiol. 1987;15:169–72. doi: 10.1111/j.1600-0528.1987.tb00508.x. [DOI] [PubMed] [Google Scholar]
- 25.Stewart AL, Ware JE., Jr . Durham, NC: Duke University Press; 1992. Measuring Functioning and Well-being: The Medical Outcomes Study Approach. [Google Scholar]
- 26.Kressin NR. Associations among different assessments of oral health outcomes. J Dent Educ. 1996;60:502–6. [PubMed] [Google Scholar]
- 27.Leao A, Sheiham A. The development of a socio-dental measure of dental impacts on daily living. Community Dent Health. 1996;13:22–6. [PubMed] [Google Scholar]
- 28.Frisch MB. Minneapolis (MN): NCS; 1994. QOLI™: Quality of Life Inventory. [Google Scholar]
- 29.Adulyanon S. Ph.D. Thesis. London: University of London; 1996. An Integrated Socio-dental Approach to Dental Treatment Need Estimation. [Google Scholar]
- 30.Locker D. Measuring oral health: A conceptual framework. Community Dent Health. 1988;5:3–18. [PubMed] [Google Scholar]
- 31.Patrick DL, Bergner M. Measurement of health status in the 1990s. Annu Rev Public Health. 1990;11:165–83. doi: 10.1146/annurev.pu.11.050190.001121. [DOI] [PubMed] [Google Scholar]


