Abstract
Cephalometrics has given us a different perspective of interpreting various skeletal problems in the dentofacial complex. Natural head position (NHP) is a reproducible, physiologically determined aspect of function. To determine NHP, a horizontal or vertical reference line outside the crania was used, but preference was given generally to the horizontal. Various intra and extracranial cephalometric horizontal reference planes have been used to formulate diagnosis and plan individualized treatment for an integrated correction of the malocclusion cephalometrics is constantly undergoing refinements in its techniques and analyses to improve the clinical applications. Even though various methods for establishing NHP have been proposed, still it remains a challenge to the clinicians to implement the concept of NHP thoroughly in all the stages of treatment because of practical difficulties in the clinical scenario.
KEY WORDS: Cephalometrics, malocclusion, natural head position
Natural head position (NHP) is a standardized and reproducible position, of the head in an upright posture, the eyes focused on a point in the distance at eye level, which implies that the visual axis is horizontal.[1] Artists, anatomists, and anthropologists have used NHP to study man's face throughout the ages. Moreover, NHP has been used routinely for clinical examination in medicine and dentistry by plastic and maxillofacial surgeons, as well as by orthodontists.
As early as the 1860's, craniologists realized that skulls had to be oriented in a manner approximating the NHP of the living for craniometric studies. To determine NHP, a horizontal or vertical reference line outside the crania was used, but the preference was generally given to the horizontal. Efforts were made to determine the landmarks through which a horizontal plane traverses the living head in its “natural position.” The next task was to apply this concept to craniology and determine which anatomic plane within the skull corresponded closest to the “horizontal.”
After considerable deliberation at four anthropologic congresses, an agreement was reached finally at the craniometric conference in Frankfurt in 1884 to accept the plane through left and right porion and left orbitale, proposed at the meeting in 1882, as the best compromise for the orientation of crania. This Frankfurt horizontal supposedly yield maximal differences in the configuration of the cranium between racial groups and the smallest variability within each group.
Orthodontists dealing with living objects, rather than inert crania have used this “Frankfurt horizontal” faithfully in cephalometrics. Cephalometric findings can be misleading, when using the nasion-sella line in the anterior skull base as a reference line, because landmarks for all intracranial reference lines are not stable points in the cranium and are subject to biologic variation in the vertical relationship of their landmarks, namely sella to nasion and for the Frankfurt horizontal porion to orbitale.
The inherent variability of intracranial cephalometric reference structures makes an analysis based on them potentially misleading, with serious implications for orthodontic and orthognathic surgical treatment planning.[2,3] Variations in the location of cranial landmarks can confound cephalometric interpretation when they are combined with nonstandardized cephalometric techniques. Obtaining a standardized orientation of the head, referred to as NHP, is possible by focusing on a distant point.[4]
Following the introduction of cephalometric radiography, there was a call for the use of a standardized, reproducible head position, to facilitate accurate radiographic cephalometric orthodontic evaluation.[5,6] For many years, there has been an intuitive belief that the visual axis of the skull, the alignment of the cervical column, natural body posture and NHP are closely associated and that NHP is highly reproducible.[7,8,9] The concept of a NHP, originally defined by Broca as being the position of the head when an individual stands with the visual axis in the horizontal plane, was introduced to orthodontics in the 1950's.[4,10,11]
The visual axis can be aligned with the horizontal plane by asking a relaxed subject to look at a distant reference point or by asking an individual to take a step forward.[4,7] While taking a step forward, an individual usually will attain NHP also known in this instance as the “orthoposition.” To classify all of the aforementioned cranial orientations as being NHP is probably correct, whereas natural head posture denotes a range of normal cranial orientations that may vary to a greater or lesser degree from the NHPs. For cephalometric analysis, the standardized NHP is preferable to natural head posture that is subject to individual variation.
Orientation in Natural Head Position
The simplest procedure to obtain photographs and head radiographs in NHP is to instruct patients to sit upright and look straight ahead to a point at eye level on the wall in front of them. In cephalometrics, it is registered by instructing the subject standing or sitting in the cephalostat to look at a point on the wall in front, exactly at eye level [Figure 1]. A small mirror the midpoint of which also at eye level, can be used also for head orientation. Mirror orientation has the additional advantage that the patient is able to self-align the midline of the head with the vertical ruler attached in the middle of the cephalostat.[1]
Figure 1.

Orientation of natural head position
Factors Influencing the Natural Head Position
Cranial posture is controlled by neuromuscular systems that appear to be influenced by normal functions such as mastication and respiration. A recent trend for research has been to focus on the possible role of extrinsic factors that are able to affect cranial posture in a manner that could be associated with aspects of specific malocclusions.[12] In this regard, extension and flexion of the head away from the NHP have been observed to be associated with morphologic patterns.[13] Two major physiologic cranial functions – Cranial posture and respiration, have been implicated as possible modifying factors in the control of growth and the establishment of dentofacial morphology.
Cleall[14] demonstrated that cranial extension results when the tongue is deflected by the insertion of an intraoral appliance. Cranial extension beyond the normal cranial position also occurs when full dentures are inserted in patients who are edentulous and when a transpalatal bar is inserted as part of orthodontic treatment.[15] The appliances displace the tongue by intruding into the space of the oral cavity. In addition, the placement of full dentures tends to rotate the mandible in a clockwise direction. This finding follows the observations made by Vig et al.,[16] who noted a jaw opening movement beyond the normal average freeway space during nasal obstruction. The long-term changes in the hyoid bone position and craniovertical posture in complete denture wearers were studied over a period of 15 years. In that study, the vertical changes in the hyoid bone position followed the patterns of change in the mandibular inclination, whereas the horizontal changes were more with the changes in cervical inclination and craniovertical angulation.[17]
Thurow[18] demonstrated that the hyoid bone is pulled forward by a passive stretch of the suprahyoid muscles when the head is extended. Such cranial extension is seen commonly in mouth breathers, and this postural change could represent an important compensation for nasal airway inadequacy.
Two major group of muscles, the suprahyoid and infrahyoid, attach to the hyoid bone. The digastric muscles increase the anteroposterior dimension of the oropharynx during deglutition, whereas the posterior belly of the digastric and the stylohyoid muscle act together to prevent regurgitation of food after swallowing.[19] The suprahyoid muscles depress the mandible by contacting against a fixed hyoid bone platform while they also play an active and important part in maintaining cranial balance. In turn, the suprahyoid muscles suspend the hyoid bone, the larynx, the pharynx and the tongue. Because these muscles attach at or near the symphysis of the mandible, it follows that should the hyoid bone passively follow the movements of the chin, all of the soft tissue structures could move to impinge on the oropharyngeal airway. The fibrous mylohyoid raphe and the stylohyoid ligament act as “rigging lines” that dictate the range of possible movements of the hyoid bone. Precise measurement of the hyoid bone by cephalometric means is difficult, but within certain limitations one can make definite conclusions concerning the normal hyoid position.[20,21] The hyoid bone moves back during cranial extension and forward during cranial flexion but largely maintains its level, moving slightly backward, during mandibular opening.[22]
Hyoid Triangle
The relationship that exists between the hyoid bone, the mandible and the cervical vertebrae is maintained from the age of 3 years, at which age the hyoid bone is located at the level of the inferior portion of the third cervical vertebra.[23,24] As age advances, the hyoid bone may descend to lie at the level of the fourth cervical vertebra. Radiographic cephalometric studies of the hyoid bone usually use intracranial reference planes to measure the position of the hyoid bone. The hyoid triangle [Figure 2] was developed to avoid the false relational effects that changes in the orientation of the cranial planes would have on measurements of the position of the hyoid bone.[25] The hyoid triangle and analysis use planes that are located between the cervical vertebra and the mandibular symphysis, which greatly reduces the effects that changes in cranial posture have on assessment of the position of the hyoid bone. The hyoid analysis fixes the position of the hyoid bone in three planes without the use of intracranial reference planes.
Figure 2.
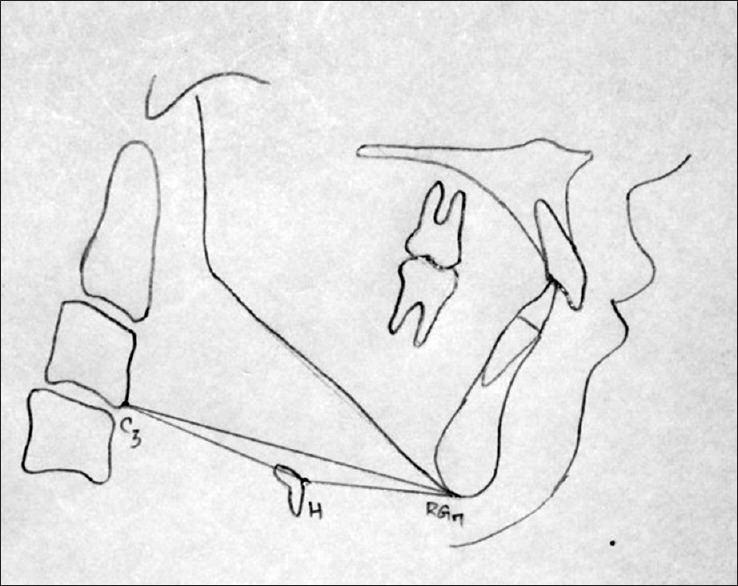
The hyoid triangle is formed by joining the cephalometric points retrognathion (RGN, the most inferior, posterior point in the mandibular symphysis), hyoidale (H, the most superior, anterior point on the body of the hyoid bone), and C3 (the most inferior, anterior point on the third cervical vertebra)
From studies of the hyoid bone, it appears that angular and vertical relationships of this bone are more variable than its horizontal location. The anteroposterior dimension of the nasopharynx – from the most anterior midline point on the arch of the Atlas vertebra to the posterior nasal spine, seems to be determined at an early age, after which this distance is relatively similar for most normal adult human beings.[24,25] The linear depth of the nasopharynx compares with the distance between the body of the hyoid bone and the cervical vertebra (C3), which is relatively constant in adults.
Cervical Posture, Respiration and Dental Occlusion
Gresham and Smithells reported that there is a relation between cervical posture and dental occlusion such that children with an Angle Class II malocclusion tend to have an exaggerated kyphosis of their cervical spines compared with children who have normal occlusions.[26] This increased cervical curvature shortens the length of the neck and results in a greater cervical inclination and cranial extension than are seen in children with normal occlusions. Moderate cranial extension is thought to decrease the resistance to airflow in the upper airway passages.[27,28]
Woodside and Linder-Aronson[29] postulated that mouth breathers tip their heads backward in an attempt to increase their airway, while nothing that the creation of a normal airway by adenoidectomy results in a less extended posture of the head. Butler[30] measured nasal resistance in normal subjects using a body plethysmograph and posterior rhinometry. He found the resistance to airflow via the nasal cavity to be more variable than the resistance of the lower airway. Hyperextension of the cranium in anesthetized subjects increases the patency of the oropharynx by separating the base of the tongue and the posterior pharyngeal wall.[31] Weber et al.[32] reported that upper airway resistance during complete respiratory half cycles, a cranial extension of 10° from the customary head position did not significantly affect the upper airway resistance.
Weber et al.[32] produced pure cranial extension in their subjects, whereas upper airway obstruction usually is associated with cranial extension in combination with a cervical lordosis. Experimentally, complete obstruction of the nasal airway has been associated with a 5° increase in craniocervical extension.[33]
This extended head posture is accompanied by a change in the resting position of the mandible and subsequently in an increase in the occlusal freeway space. Linder-Aronson[33] reported an average of a 6° increase in craniocervical extension in a group of children who required adenoidectomy because of nasopharyngeal obstruction. Adenoidectomy alone may change only the breathing pattern without having a significant effect on malocclusion or facial type.[34]
There is an associated increase in craniocervical angulation in subjects with obstructed nasopharyngeal airways. In these subjects, the elimination of the airway obstruction is associated with a reduction in the craniocervical angulation. Reduced functional adequacy of the upper airway, altered head posture and posture induced soft tissue stretching has been suggested as being linked in a cycle that affects cranial growth and thus facial form.[35]
Natural head position is the most acceptable reproducible position clinically and true horizontal planes derived from NHP registration represent a more valid craniofacial reference system.
For diagnosis and correction of facial dysmorphology and malocclusion, harmonious proportional relationships of facial landmarks remain key to their correction.
Conclusion
“The search for an ideal.” Cephalometrics is constantly undergoing refinements in its techniques and analyses to improve the clinical applications. Even though various methods for establishing NHP have been proposed, still it remains a challenge to the clinicians to implement the concept of NHP thoroughly in all the stages of treatment because of practical difficulties in the clinical scenario.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Jacobson A. Publisher location: Carol Stream Quintessence; 1995. Radiographic Cephalometry. From Basics to Video Imaging. [Google Scholar]
- 2.Houston WJ. Bases for the analysis of cephalometric radiographs: Intracranial reference structures or natural head position. Proc Finn Dent Soc. 1991;87:43–9. [PubMed] [Google Scholar]
- 3.Lundström A, Lundström F. The Frankfort horizontal as a basis for cephalometric analysis. Am J Orthod Dentofacial Orthop. 1995;107:537–40. doi: 10.1016/s0889-5406(95)70121-4. [DOI] [PubMed] [Google Scholar]
- 4.Moorrees CF, Kean MR. Natural head position: A basic consideration in the interpretation of cephalometric radiographs. Am J Phys Anthropol. 1958;16:213. [Google Scholar]
- 5.Grabber TM. Implementation of the roentgenographic cephalometric technique. Am J Orthod. 1958:906–32. [Google Scholar]
- 6.Moorrees CF. Natural head position: Introduction to radiographic cephlometry. In: Jacobson A, editor. Radiographic Cephalometry: From Basics to Video imaging. Carol Stream, III: Quintessence; 1995. [Google Scholar]
- 7.Cooke MS, Wei SH. The reproducibility of natural head posture: A methodological study. Am J Orthod Dentofacial Orthop. 1988;93:280–8. doi: 10.1016/0889-5406(88)90157-6. [DOI] [PubMed] [Google Scholar]
- 8.Bass NM. Measurement of the profile angle and the aesthetic analysis of the facial profile. J Orthod. 2003;30:3–9. doi: 10.1093/ortho/30.1.3. [DOI] [PubMed] [Google Scholar]
- 9.Peng L, Cooke MS. Fifteen-year reproducibility of natural head posture: A longitudinal study. Am J Orthod Dentofacial Orthop. 1999;116:82–5. doi: 10.1016/s0889-5406(99)70306-9. [DOI] [PubMed] [Google Scholar]
- 10.Downs WB. Analysis of the dentofacial profile. Am J Orthod Oral Surg. 1956;26:192–212. [Google Scholar]
- 11.Bjerin R. A comparison between the Frankfort horizontal and the sella-nasion as reference planes in cephalometric analysis. Acta Odontol Scand. 1957;15:1–12. [Google Scholar]
- 12.Solow B, Sonnesen L. Head posture and malocclusions. Eur J Orthod. 1998;20:685–93. doi: 10.1093/ejo/20.6.685. [DOI] [PubMed] [Google Scholar]
- 13.Solow B, Tallgren A. Head posture and craniofacial morphology. Am J Phys Anthropol. 1976;44:417–35. doi: 10.1002/ajpa.1330440306. [DOI] [PubMed] [Google Scholar]
- 14.Cleall JF. Circumstances limiting the development and verification of a comprehensive theory of craniofacial morphogenesis. Acta Morphol Neerl Scand. 1972;10:115–26. [PubMed] [Google Scholar]
- 15.Salonen MA, Raustia AM, Huggare JA. Changes in head and cervical-spine postures and EMG activities of masticatory muscles following treatment with complete upper and partial lower denture. Cranio. 1994;12:222–6. doi: 10.1080/08869634.1994.11678025. [DOI] [PubMed] [Google Scholar]
- 16.Vig PS, Showfety KJ, Phillips C. Experimental manipulation of head posture. Am J Orthod. 1980;77:258–68. doi: 10.1016/0002-9416(80)90081-0. [DOI] [PubMed] [Google Scholar]
- 17.Tallgren A, Solow B. Long-term changes in hyoid bone position and craniocervical posture in complete denture wearers. Acta Odontol Scand. 1984;42:257–67. doi: 10.3109/00016358408993879. [DOI] [PubMed] [Google Scholar]
- 18.Thurow RC. Atlas of Orthodontic Principles. St. Louis: CV Mosby; 1978. [Google Scholar]
- 19.Goss CM, editor. Anatomy of the Human Body. 28th ed. Philadelphia: Lea and Febiger; 1967. [Google Scholar]
- 20.Graber LW. Hyoid changes following orthopedic treatment of mandibular prognathism. Angle Orthod. 1978;48:33–8. doi: 10.1043/0003-3219(1978)048<0033:HCFOTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Stepovich ML. A cephalometric positional study of the hyoid bone. Am J Orthod. 1965;51:882–900. doi: 10.1016/0002-9416(65)90202-2. [DOI] [PubMed] [Google Scholar]
- 22.Ingervall B, Carlsson GE, Helkimo M. Change in location of hyoid bone with mandibular positions. Acta Odontol Scand. 1970;28:337–61. doi: 10.3109/00016357009032039. [DOI] [PubMed] [Google Scholar]
- 23.King EW. A roentgenographic study of pharyngeal growth. Angle Orthod. 1952;22:23–37. [Google Scholar]
- 24.Bench RW. Growth of the cervical vertebrae as related to tongue, face, and denture behavior. Am J Orthod. 1963;49:183–214. [Google Scholar]
- 25.Bibby RE, Preston CB. The hyoid triangle. Am J Orthod. 1981;80:92–7. doi: 10.1016/0002-9416(81)90199-8. [DOI] [PubMed] [Google Scholar]
- 26.Gresham H, Smithells PA. Cervical and mandibular posture. Dent Rec. 1954;74:261–4. [Google Scholar]
- 27.Linder-Aronson S, Backstrom A. A comparison between mouth and nose breathers with respect to occlusion and facial dimensions. Odontol Rev. 1980;11:343–76. [Google Scholar]
- 28.Ricketts RM. Respiratory obstruction syndrome. Am J Orthod. 1968;54:495–507. doi: 10.1016/0002-9416(68)90218-2. [DOI] [PubMed] [Google Scholar]
- 29.Woodside DG, Linder-Aronson S. The channelization of upper and lower anterior face heights compared to population standard in males between ages 6 to 20 years. Eur J Orthod. 1979;1:25–40. doi: 10.1093/ejo/1.1.25. [DOI] [PubMed] [Google Scholar]
- 30.Butler J. The work of breathing through the nose. Clin Sci. 1960;19:55–62. [PubMed] [Google Scholar]
- 31.Greene DG, Elam JO, Dobkin AB, Studley CL. Cinefluorographic study of hyperextension of the neck and upper airway patency. JAMA. 1961;176:570–3. doi: 10.1001/jama.1961.03040200006002. [DOI] [PubMed] [Google Scholar]
- 32.Weber ZJ, Preston CB, Wright PG. Resistance to nasal airflow related to changes in head posture. Am J Orthod. 1981;80:536–45. doi: 10.1016/0002-9416(81)90248-7. [DOI] [PubMed] [Google Scholar]
- 33.Linder-Aronson S. Respiratory function in relation to facial morphology and the dentition. Br J Orthod. 1979;6:59–71. doi: 10.1179/bjo.6.2.59. [DOI] [PubMed] [Google Scholar]
- 34.Guray E, Karaman I. Effects of adenoidectomy on dentofacial structures: A 6-year longitudinal study. World J Orthod. 2002;3:73–81. [Google Scholar]
- 35.Solow B, Kreiborg S. Soft-tissue stretching: A possible control factor in craniofacial morphogenesis. Scand J Dent Res. 1977;85:505–7. doi: 10.1111/j.1600-0722.1977.tb00587.x. [DOI] [PubMed] [Google Scholar]


