Abstract
Background:
Oral lichen planus (OLP) is a unique disorder affecting generally the older age group. Numerous studies have been done on various aspects of OLP such as pathogenesis, rate of malignant transformation, etc. However, very few studies are available with respect to clinical features especially association of hyperpigmentation and OLP. This study aims at studying the clinical aspects of OLP and study the association between hyperpigmentation and OLP in a south Indian population.
Materials and Methods:
A total of 58 patients with OLP who attended the outpatient department of our institution were included in the study and a complete history, followed by thorough intraoral examination was done. All the data were recorded and assessed for statistical analysis using SPSS software.
Results:
We found that the male to female ratio affected with OLP was 1:1 and the most common form of OLP that was seen was the reticular subtype. Also, buccal mucosa was the most common affected site and more than 60% patients had hyperpigmentation associated with the site affected by OLP. We found a statistically significant relation between the reticular type of OLP and the older age group (51–70 years) with hyperpigmentation.
Conclusion:
Although further studies are required to say anything conclusively, post-inflammatory changes occurring the mucosa due to OLP could be a cause for hyperpigmentation in the sites affected.
KEY WORDS: Clinical features, hyperpigmentation, inflammatory disorder, oral lichen planus, postinflammatory changes
Lichen planus (LP) is a unique mucocutaneous disorder that mainly affects the oral cavity, esophagus and genitals. Its first ever description was given by a famous British physician named Wilson in 1869.[1] The word “lichens” means primitive plants composed of symbiotic algae and fungi and the Latin term “planus” means flat. Apart from the aforementioned sites this disease may also affect other parts of the body such as hair follicles, nails, larynx and eyes.[2,3] LP of the skin are typically seen as small (2 mm) pruritic, white flat-topped papules, which increase in size to as much as 3 cm. The clinical presentations of LP may be in the form of striations, plaques, mucosal atrophy, erosions (shallow ulcers) and blisters. The LP of the skin is considered to have an acute progression and also a spontaneous remission. The disease has a predilection for the flexor surfaces of the forearms and legs and Koebner's phenomenon is commonly seen a feature of LP.[4,5,6,7]
The disease when it affects the oral cavity is termed oral LP (OLP). Unlike the skin lesions, mucosal lesions follow a more chronic course, and it has been observed that the oral lesions may persist up to 25 years. In general it is considered to affect about 1–2% of the general adult population, although young adults and children may also be affected.[6,8,9] OLP has been described as a disease of the middle-aged, predominantly in adults over the age of 40, and more common in women than men in ratio 1.4:1. In the oral cavity, the buccal mucosa, tongue and gingiva are the most favored sites whereas lesions of the palate are very rare. The lesions very occasionally seem to be unilateral or affect any one part of the oral cavity. It is usually bilateral or affects more than one part of the oral cavity and also may involve other mucous membranes.[6,10,11] One of the important clinical features of OLP is the presence of Wickham's striae. This was named after Louis Frédéric Wickham who described the clinical appearance of OLP as presence of greyish striae and dots.[12,13] Another clinical sign associated with OLP that has been observed is hyperpigmentation. Although it is a sign that is often seen in OLP, the reason for its appearance has not been determined. As far as OLP is considered there are a number of studies regarding the probable etiopathogenesis and malignant transformation but very few regarding the presence of hyperpigmentation.[14,15,16,17,18] So in this study, we aimed to analyze the clinical features of OLP including hyperpigmentation in 58 patients that reported to our institution.
Materials and Methods
The study consisted of 58 patients that attended to our institution who were clinically and histologically diagnosed with OLP with features recommended by WHO.[19] The study was undertaken after a clearance from the ethical committee of the university. After an informed consent, the demographic details were collected, and detailed case history was taken followed by a thorough extra and intra oral examination. All the clinical details were recorded in a case history format that was pretested. The following details were collected: Name, age, sex, habit of smoking, whether the patient's complaint is associated with OLP, whether the lesion is symptomatic, site of involvement, clinical type of OLP, and whether hyperpigmentation was present or not. All the data were analyzed in the SPSS software version 17.0 (IBM, USA) for Windows 7 (Microsoft, USA). Chi-square test for association was done to compare data and the level of association was set at 0.05 for significance.
Results
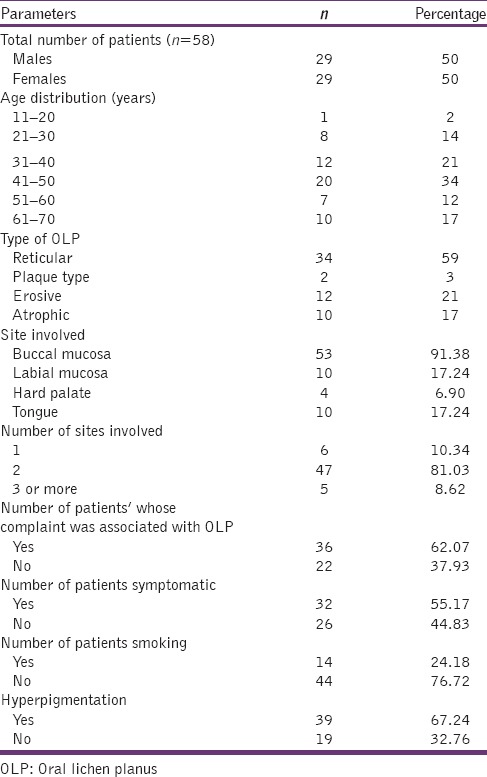
The total number of patients that participated in our study were 58, out of which 29 were male and 29 were female giving a ratio of 1:1. The mean age of the patients was 45.72 ± 13.10. The maximum numbers of patients were in the age group 41–50 years age group (34%), followed by 31–40 years (21%), 61–70 years (14%), 21–30 years (14%), 51–60 years (12%) and 11–20 years (2%) age groups. 62.07% of the patients had come with a complaint related to OLP, whereas 37.93% of patients were not aware of the lesions and were detected on routine examination. 55.17% of patients were symptomatic, that is, had pain or burning sensation, whereas 44.83% were asymptomatic. Reticular type of OLP was most common (59%), followed by erosive (21%), atrophic (17%) and plaque type OLP (3%). The site most commonly involved was the buccal mucosa (91.38%), followed by labial mucosa and tongue (17.24% each) and palate (6.29%). As far as the number of sites affected is considered only 10.34% of patients had a single site involvement, whereas 81.03% had two sites involved, and 8.62% had more than two sites in the oral involved. Hyperpigmentation was observed [Figures 1 and 2] in 67.24% of patients all data in Table 1.
Figure 1.

Intraoral photograph of 47 year-old female patient with reticular type of oral lichen planus and hyperpigmentation on the right buccal mucosa
Figure 2.

Intraoral photograph of 67-year-old male patient with reticular type of oral lichen planus hyperpigmentation on the left buccal mucosa
Table 1.
Descriptive statistics of patients included in the study
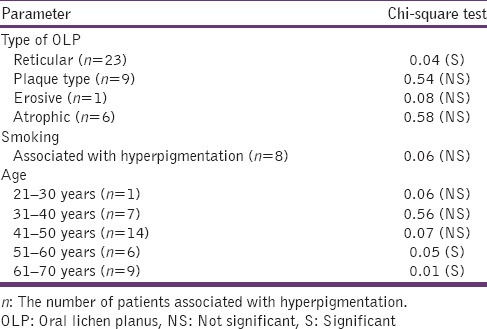
Chi-square test of association showed a statistically significant association between reticular type of OLP and hyperpigmentation when compared to other subtypes of OLP. Also we found that there was no significant association between smoking and younger age group with hyperpigmentation. However, we found a statistically significant association between the older age groups (51–60 and 61–70 years) and hyperpigmentation all data in Table 2.
Table 2.
Association of hyperpigmentation with type of OLP, smoking and age
Discussion
We performed this clinical study to assess the clinical features of OLP especially hyperpigmentation because there are very few studies in this aspect.[14] The ratio of male to female occurrence in our study was 1:1. These results were similar to the ones obtained by Lacy et al., and Anjum et al., who feel that there is no sex predliction as far as OLP is concerned, but many authors claim that OLP is more predominant in females and the reason might be stress and hormonal influences.[4,20,21,22] But in our study, we observed an equal distribution between males and females. This might be due to a small sample size as compared to other studies.
In our study, we found that maximum number of patients were seen in the 41–70 years age group. This was similar to studies observed by Persić et al., and Ahmed et al.[23,24,25] Although OLP is considered to be a disease of adulthood, there are some case reports where LP has been observed in a 6 months old infant.[26] The mean age of occurrence of OLP in our study was observed to be 45 years. This is similar to the one observed by few authors in Asia, whereas it is considerably lower than observed in European populations where the mean age observed was around 56 years.[27,28,29,30] This variation might be due to the difference in ethnicity and geographic locations.
The reticular type of OLP was the most common subtype observed in our study. This is similar to the studies by Bajaj et al., and Ingafou et al.[2,30] Similarly other results obtained in our study such as the patients complaint and the number of patients symptomatic were high and in accordance with the results obtained by Xue et al.[31] This is due to increased patient and dentist awareness regarding OLP and the clinical manifestations such as feeling of raised borders or slight roughness or dryness of the affected mucosal surfaces, especially in reticular and plaque type OLP and presence of pain and burning sensation in patients with atrophic and erosive type of OLP. The most common site where OLP was seen in our study was in the buccal mucosa, followed by the labial mucosa and tongue, and the hard palate. This is in accordance with the study done by Budimir et al., and Shen et al. Also most commonly the site of involvement was bilateral and two or more sites were involved in majority of the cases.[27,32]
The most important observation that we tried to associate with clinical factors in this study was the presence of hyperpigmentation. The various reasons that have been described for oral mucosal pigmentation are race, smoking, stress and anxiety, Addison's disease and postinflammatory changes.[33] In our study, we did not observe any racial associated pigmentation in any of the patients in the noninvolved sites. We could also rule out the possibility of Addison's disease to be a reason for the pigmentation in the patients included in our study. In this study we have studied the association of smoking and hyperpigmentation but we did not observe any statistical significance regarding the habit and presence of hyperpigmentation. This was probably due to a small proportion of patients (only 14) having a smoking habit. We also observed that there was a statistically significant association between old age (i.e. 51–70 years) and hyperpigmentation. The main reason could be that the hyperpigmentation was due to postinflammatory changes and repeated occurrence and healing of OLP. Also, the reticular form of OLP was found to be more associated with OLP as this form of OLP follows a more chronic course and results in inflammatory changes of the oral mucosa. The postinflammatory changes have been studied in detail by few authors. It is believed that this type of pigmentation is due to excessive melanin production after an inflammatory reaction.[34] Along with the increased melanin pigmentation, abnormal distribution of melanin and presence of melanophages is also considered to be the cause for hyperpigmentation of the mucosa after inflammation.[35,36] Although all these reports are from studies done in skin the same can be explained with OLP as it also an inflammatory disorder and the probable mechanism that has been suggested for the stimulation of melanocytes is due to the cytokines released by the subepithelial band of lymphocytes.[37] Thus, the reason for hyperpigmentation is still not clear, but it could be due the inflammation associated with OLP. Further studies are required to apprehend the relationship between hyperpigmentation and OLP in histopathological, immunohistochemical and biochemical aspects.
Summary
OLP is a chronic noninfectious disorder that affects majorly the adult age group. It is a T-cell mediated inflammatory disorder and one of the important features of OLP which is hyperpigmentation. Although further studies are required to understand why hyperpigmentation occurs in OLP, one of the reasons might be the postinflammatory changes that occur in the mucosa.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Wilson E. On lichen planus. J Cutan Med Dis Skin. 1869;3:117–32. [Google Scholar]
- 2.Bajaj DR, Khoso NA, Devrajani BR, Matlani BL, Lohana P. Oral lichen planus: A clinical study. J Coll Physicians Surg Pak. 2010;20:154–7. [PubMed] [Google Scholar]
- 3.Farhi D, Dupin N. Pathophysiology, etiologic factors, and clinical management of oral lichen planus, part I: Facts and controversies. Clin Dermatol. 2010;28:100–8. doi: 10.1016/j.clindermatol.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 4.Chainani-Wu N, Silverman S, Jr, Lozada-Nur F, Mayer P, Watson JJ. Oral lichen planus: Patient profile, disease progression and treatment responses. J Am Dent Assoc. 2001;132:901–9. doi: 10.14219/jada.archive.2001.0302. [DOI] [PubMed] [Google Scholar]
- 5.Lozada-Nur F, Miranda C. Oral lichen planus: Epidemiology, clinical characteristics, and associated diseases. Semin Cutan Med Surg. 1997;16:273–7. doi: 10.1016/s1085-5629(97)80016-8. [DOI] [PubMed] [Google Scholar]
- 6.Mollaoglu N. Oral lichen planus: A review. Br J Oral Maxillofac Surg. 2000;38:370–7. doi: 10.1054/bjom.2000.0335. [DOI] [PubMed] [Google Scholar]
- 7.Sangeetha S, Victor JD. The molecular aspects of oral mucocutaneous diseases: A review. Int J Genet Mol Biol. 2011;3:141–8. [Google Scholar]
- 8.de Sousa FA, Rosa LE. Oral lichen planus: Clinical and histopathological considerations. Rev Bras Otorrinolaringol. 2008;74:284–92. doi: 10.1016/S1808-8694(15)31102-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sugerman PB, Savage NW, Zhou X, Walsh LJ, Bigby M. Oral lichen planus. Clin Dermatol. 2000;18:533–9. doi: 10.1016/s0738-081x(00)00142-5. [DOI] [PubMed] [Google Scholar]
- 10.Lodi G, Scully C, Carrozzo M, Griffiths M, Sugerman PB, Thongprasom K. Current controversies in oral lichen planus: Report of an international consensus meeting. Part 1. Viral infections and etiopathogenesis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:40–51. doi: 10.1016/j.tripleo.2004.06.077. [DOI] [PubMed] [Google Scholar]
- 11.Sugerman PB, Savage NW. Oral lichen planus: Causes, diagnosis and management. Aust Dent J. 2002;47:290–7. doi: 10.1111/j.1834-7819.2002.tb00540.x. [DOI] [PubMed] [Google Scholar]
- 12.Anees MM, Szepietowski J. Oral lichen planus: A review of aetiopathogenesis, clinical manifestations, histology and treatment modalities. Clinical Dermatology. 2007;9:243–8. [Google Scholar]
- 13.Canto AM, Müller H, Freitas RR, Santos PS. Oral lichen planus (OLP): Clinical and complementary diagnosis. An Bras Dermatol. 2010;85:669–75. doi: 10.1590/s0365-05962010000500010. [DOI] [PubMed] [Google Scholar]
- 14.Murti PR, Bhonsle RB, Daftary DK, Mehta FS. Oral lichen planus associated with pigmentation. J Oral Med. 1979;34:23–4. [PubMed] [Google Scholar]
- 15.Roopashree MR, Gondhalekar RV, Shashikanth MC, George J, Thippeswamy SH, Shukla A. Pathogenesis of oral lichen planus - A review. J Oral Pathol Med. 2010;39:729–34. doi: 10.1111/j.1600-0714.2010.00946.x. [DOI] [PubMed] [Google Scholar]
- 16.van der Meij EH, Schepman KP, Smeele LE, van der Wal JE, Bezemer PD, van der Waal I. A review of the recent literature regarding malignant transformation of oral lichen planus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:307–10. doi: 10.1016/s1079-2104(99)70033-8. [DOI] [PubMed] [Google Scholar]
- 17.Mattsson U, Jontell M, Holmstrup P. Oral lichen planus and malignant transformation: Is a recall of patients justified? Crit Rev Oral Biol Med. 2002;13:390–6. doi: 10.1177/154411130201300503. [DOI] [PubMed] [Google Scholar]
- 18.Teja CS, Devy AS, Nirmal RM, Sunil PM, Deepasree M. Cytomorphometric analysis of exfoliated cells in oral lichen planus. Cytojournal. 2014;11:3. doi: 10.4103/1742-6413.127214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rad M, Hashemipoor MA, Mojtahedi A, Zarei MR, Chamani G, Kakoei S, et al. Correlation between clinical and histopathologic diagnoses of oral lichen planus based on modified WHO diagnostic criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:796–800. doi: 10.1016/j.tripleo.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 20.Lacy MF, Reade PC, Hay KD. Lichen planus: A theory of pathogenesis. Oral Surg Oral Med Oral Pathol. 1983;56:521–6. doi: 10.1016/0030-4220(83)90100-7. [DOI] [PubMed] [Google Scholar]
- 21.Anjum R, Singh J, Kuduva S. A clinicohistopathologic study and probable mechanism of pigmentation in oral lichen planus. World J Dent. 2012;3:330–4. [Google Scholar]
- 22.Silverman S, Jr, Bahl S. Oral lichen planus update: Clinical characteristics, treatment responses, and malignant transformation. Am J Dent. 1997;10:259–63. [PubMed] [Google Scholar]
- 23.Eisen D. The clinical features, malignant potential, and systemic associations of oral lichen planus: A study of 723 patients. J Am Acad Dermatol. 2002;46:207–14. doi: 10.1067/mjd.2002.120452. [DOI] [PubMed] [Google Scholar]
- 24.Persić S, Mihić LL, Budimir J, Situm M, Bulatz V, Krolo I. Oral lesions in patients with lichen planus. Acta Clin Croat. 2008;47:91–6. [PubMed] [Google Scholar]
- 25.Ahmed I, Nasreen S, Jehangir U, Wahid Z. Frequency of oral lichen planus in patients with noninsulin dependent diabetes mellitus. J Pak Assoc Dermatologists. 2012;22:30–4. [Google Scholar]
- 26.Pussey WA. Lichen planus in an infant less than 6 months old. Arch Dermatol Syph. 1929;19:671. [Google Scholar]
- 27.Shen ZY, Liu W, Zhu LK, Feng JQ, Tang GY, Zhou ZT. A retrospective clinicopathological study on oral lichen planus and malignant transformation: Analysis of 518 cases. Med Oral Patol Oral Cir Bucal. 2012;17:e943–7. doi: 10.4317/medoral.17778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gandolfo S, Richiardi L, Carrozzo M, Broccoletti R, Carbone M, Pagano M, et al. Risk of oral squamous cell carcinoma in 402 patients with oral lichen planus: A follow-up study in an Italian population. Oral Oncol. 2004;40:77–83. doi: 10.1016/s1368-8375(03)00139-8. [DOI] [PubMed] [Google Scholar]
- 29.Bermejo-Fenoll A, Sánchez-Siles M, López-Jornet P, Camacho-Alonso F, Salazar-Sánchez N. A retrospective clinicopathological study of 550 patients with oral lichen planus in south-eastern Spain. J Oral Pathol Med. 2010;39:491–6. doi: 10.1111/j.1600-0714.2010.00894.x. [DOI] [PubMed] [Google Scholar]
- 30.Ingafou M, Leao JC, Porter SR, Scully C. Oral lichen planus: A retrospective study of 690 British patients. Oral Dis. 2006;12:463–8. doi: 10.1111/j.1601-0825.2005.01221.x. [DOI] [PubMed] [Google Scholar]
- 31.Xue JL, Fan MW, Wang SZ, Chen XM, Li Y, Wang L. A clinical study of 674 patients with oral lichen planus in China. J Oral Pathol Med. 2005;34:467–72. doi: 10.1111/j.1600-0714.2005.00341.x. [DOI] [PubMed] [Google Scholar]
- 32.Budimir V, Richter I, Andabak-Rogulj A, Vucicevic-Boras V, Budimir J, Brailo V. Oral lichen planus – Retrospective study of 563 Croatian patients. Med Oral Patol Oral Cir Bucal. 2014;19:e255–60. doi: 10.4317/medoral.18940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kauzman A, Pavone M, Blanas N, Bradley G. Pigmented lesions of the oral cavity: Review, differential diagnosis, and case presentations. J Can Dent Assoc. 2004;70:682–3. [PubMed] [Google Scholar]
- 34.Patsakas A, Demetriou N, Angelopoulos A. Melanin pigmentation and inflammation in human gingiva. J Periodontol. 1981;52:701–4. doi: 10.1902/jop.1981.52.11.701. [DOI] [PubMed] [Google Scholar]
- 35.Morelli JG, Norris DA. Influence of inflammatory mediators and cytokines on human melanocyte function. J Invest Dermatol. 1993;100:191S–5. [PubMed] [Google Scholar]
- 36.Nordlund JJ. Postinflammatory hyperpigmentation. Dermatol Clin. 1988;6:185–92. [PubMed] [Google Scholar]
- 37.Mergoni G, Ergun S, Vescovi P, Mete Ö, Tanyeri H, Meleti M. Oral postinflammatory pigmentation: An analysis of 7 cases. Med Oral Patol Oral Cir Bucal. 2011;16:e11–4. doi: 10.4317/medoral.16.e11. [DOI] [PubMed] [Google Scholar]


