Abstract
Introduction:
The presence of gingival recession associated with an insufficient amount of keratinized tissue may indicate gingival augmentation procedure. It is a multifaceted problem for which several treatment options are available. The most predictable technique used for gingival augmentation is the subepithelial connective tissue graft (SCTG). Platelet-rich plasma (PRP) is an enhanced source of growth factors and helps in accelerated periodontal repair and regeneration.
Aims:
The aim of this study was to evaluate the efficacy of SCTG along with PRP in the treatment of Miller's class I and II gingival recessions.
Materials and Methods:
Eleven subjects with Miller's class I and II gingival recessions were treated using SCTG with PRP. Clinical variables, including plaque index, gingival index, recession depth (RD), Recession width (RW), width of the keratinized gingiva, probing pocket depth (PD) and clinical attachment level (CAL) were recorded. Patients were recalled at baseline, 3 months, 6 months and 1-year after surgery and clinical recordings were taken. Root coverage percentage (%) was measured at the end of 1-year.
Results:
The clinical parameters were analyzed during the follow-up period by repeated measures ANOVA test. Twelve months follow-up results showed significant improvements in all the clinical parameters. Reduction of recession resulted in a significant decrease in CAL, PD, RW and RD at the end of 12 months. A statistically significant gain in width of keratinized gingiva and a mean root coverage of 84.72 ± 19.10 was obtained at the end of 12 months.
Conclusion:
From the results of this study, it may be concluded that SCTG with PRP is an effective and predictable method to treat miller's class I and II gingival recession.
KEY WORDS: Gingival recession, growth factors, platelet-rich plasma, subepithelial connective tissue graft
Marginal gingival recession can cause major functional and esthetic problems.[1] It has been clinically related to higher incidence of root caries, attachment loss, hypersensitivity and esthetic concerns. Treatment of denuded roots surfaces may improve esthetics, controls plaque retention, reduce the risk of caries and establish an adequate zone of attached gingiva.
Since the middle of 20th century, different techniques have been developed to cover the denuded roots.[2,3] The introduction of the subepithelial connective tissue graft (SCTG) into the mucogingival armamentarium significantly improved the predictability of mucogingival surgical procedures.[4] The SCTG technique quickly became a popular modality of esthetic root coverage procedure because of its high degree of success and greater predictability.
A recent innovation in dentistry is platelet-rich plasma (PRP), a concentrated suspension of the growth factors found in platelets.[5] These growth factors are important at all stages of cell cycle and may stimulate chemotaxis and production of extracellular matrix proteins.[6] Its application has been reported as an effective way to induce tissue repair and regeneration.[7]
In an attempt to increase the success rate of the connective tissue grafting procedure as well as to increase the successful use of tissue regeneration barriers to provide root coverage, the use of PRP has been incorporated into the surgical protocol.[8]
The purpose of the present clinical study was to evaluate the efficacy of subepithelial connective graft along with autologous PRP in the treatment of localized gingival recession.
Materials and Methods
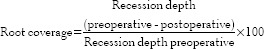
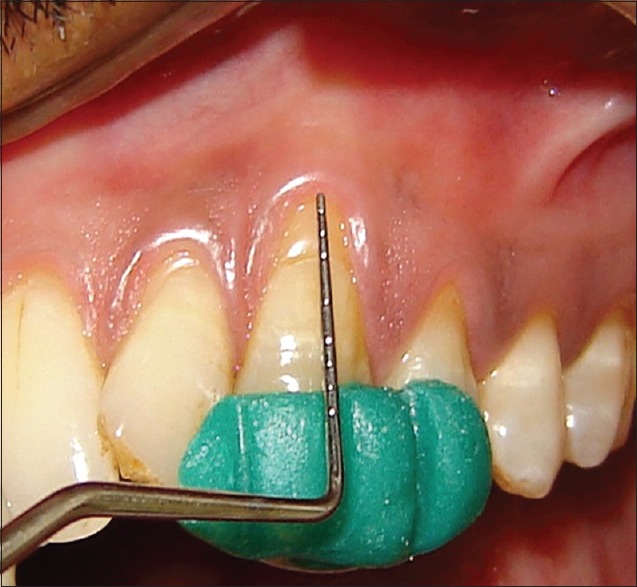
The present clinical study includes 11 patients, 7 males and 4 females, who have been referred to the department of periodontology, Sree Sai Dental College and Research Institute, Srikakulam (Andhra Pradesh state) from the Department of Dentistry, Rajiv Gandhi Institute of Medical Sciences, Srikakulam after performing scaling and root planning. On periodontal examination and radiographic evaluation, the patients presenting with Miller's class I and II gingival recession were selected for the study [Figure 1].
Figure 1.

Preoperative view
Selection criteria
Inclusion criteria
Patients in the age group of 20–40 years
Recessions located on maxillary incisors or cuspids
Patients in good general health
Patients showing a tendency to maintain a good oral hygiene after Phase I therapy
Miller's class I and II gingival recessions defects measuring ≥3 mm only
Vital teeth without any previous history of periodontal surgery.
Exclusion criteria
Medically compromised patients
The presence of severe cervical abrasion, erosion or root caries that would require restoration
Patients with smoking habits.
All the patients were subjected to Phase I therapy. Trauma from occlusion if detected was eliminated. At the end, only those patients demonstrating the acceptable oral hygiene standards and gingival health were considered for the present study. Each patient was explained about treatment design. An informed consent was taken from each of the participating subject.
Clinical parameters
All the clinical parameters were recorded with a William's periodontal probe and the values were rounded off to the nearest 0.5 mm.
The following clinical parameters were recorded:
Clinical parameters were recorded as follows
Recession depth: It was recorded from the occlusal level of the stent to the crest of the gingival margin at the mid-labial region
Recession width: It was recorded with a periodontal probe, from the mesial to distal gingival margin at the level of cementoenamel junction (CEJ)
Width of Keratinized gingiva: It was recorded with a periodontal probe, from the crest of gingival margin to the mucogingival junction
Probing pocket depth: It was measured from crest of the gingival margin to the base of the pocket at the mid-labial region
Clinical attachment level: It was recorded from the occlusal level of the stent to the base of the pocket by inserting the periodontal probe at the mid-labial region
Root coverage: Percentage of root coverage was calculated according to the formula.[13]
Recession depth and CAL were recorded using an occlusal stent [Figure 2]. The use of an occlusal stent (with guiding grooves) and the William's periodontal probe provided a fixed reference point and fixed angulation for measurements at each site at different time intervals.[12] All the above clinical parameters except the probing depth and the CAL were recorded at the baseline, 3 months, 6 months and 1-year postoperatively. The probing depth and CAL were measured only at baseline, 6 months and 1-year postoperatively. Percentage of root coverage was calculated at 1-year postoperatively.
Figure 2.
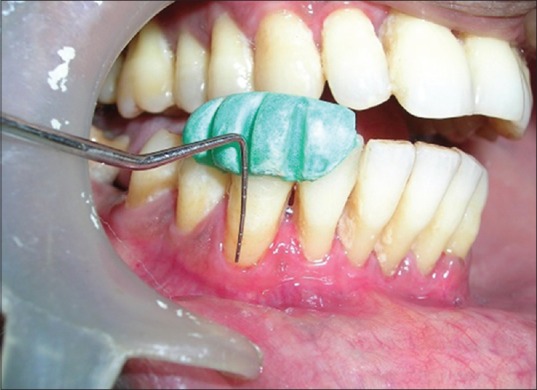
Clinical recordings using occlusal stent
Preparation of platelet-rich plasma
An hour prior to surgery, blood was taken from the anticubital region with a 21-gauge needle and injected into the 10-mL blood collection tube containing 3.2% anticoagulant sodium citrate. To separate and concentrate platelets, two separate centrifugations (referred to as spin) were done. In the first spin, the blood was centrifuged at 2000 rpm for 2 min. This separates the red blood cells from the rest of the whole blood (white blood cells, platelets and plasma) with a thin white line in between (called as buffy coat), which has maximum concentration of platelets. The plasma and the buffy coat were pipetted out in a separate test tube and centrifuged (second spin) at 4000 rpm for 8 min. The second spin results in two separate fragments. The bottom layer is the PRP which is overlaid by supernatant fluid platelet poor plasma (PPP). PPP is pipetted out in a separate test tube, and the PRP is then used for the procedure.[14] In this study, PRP was obtained by the modified method of Curasan.[15]
Surgical technique
Preparation of recipient bed
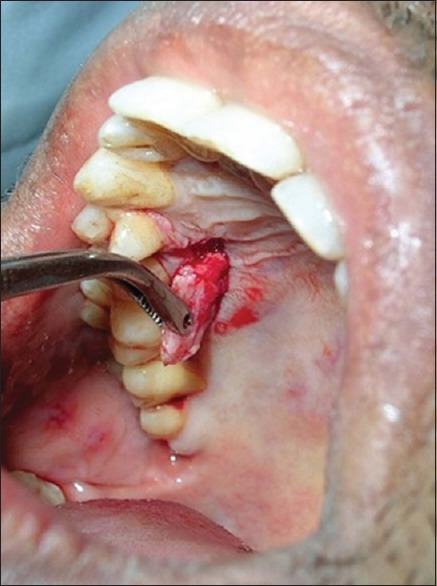
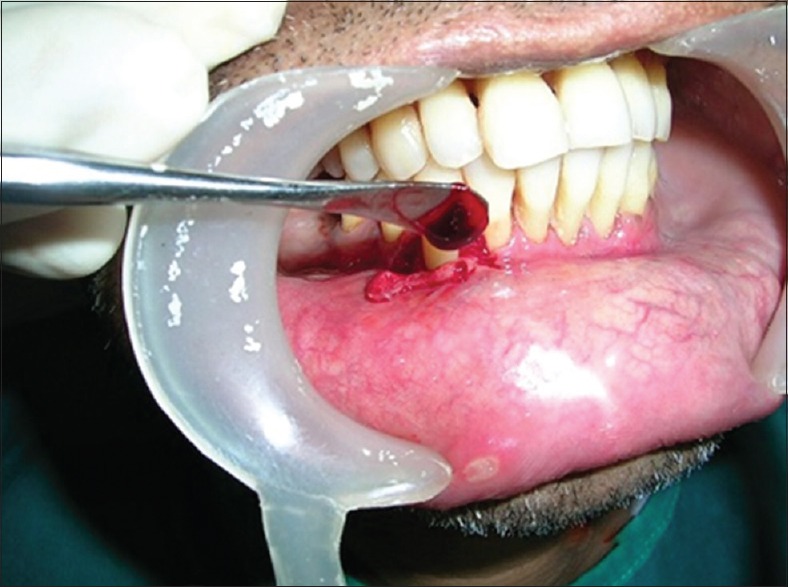
The surgical area was prepared and adequately anesthetized using 2% lignocaine HCL containing 1:80,000 epinephrine by giving block and infiltration anesthesia. After obtaining adequate anesthesia, two vertically divergent incisions (i.e. one mesial and one distal, immediately adjacent to the defect) extending beyond the MGJ were made on the buccal aspect of the involved tooth. The sulcular incision was then placed up to the end of vertical incisions [Figure 3]. Care was taken to see that the papilla was intact. A trapezoidal flap was elevated by sharp dissection with no. 15 scalpel blade to raise a combined full-partial thickness flap to the level of the MGJ [Figure 4].
Figure 3.

Sulcular incision given
Figure 4.

Partial – full thickness flap raised
The flap was extended well beyond the mucogingival junction so that it exhibited no tension when pulled coronally beyond the CEJ and should be extended at least 5 mm coronal to the most apical margin of the bony dehiscence. The intact papillae mesial and distal to the recession were deepithelized to provide bleeding connective tissue bed for future SCTG.
Root conditioning with tetracycline solution: (100 mg/ml)
A fresh tetracycline solution (100 mg/ml) was prepared and applied to the root surface for each surgery. Cotton pellets soaked in tetracycline solution (100 mg/ml) were burnished to the root surface with a light pressure for 4 min [Figure 5]. The root surface was then extensively rinsed with saline solution.
Figure 5.

Tetracycline solution root conditioning
Graft harvesting from donor site
A measurement of the approximate length and width of the graft required was taken and obtained from the palate by bruno's technique[16] [Figure 6]. After its removal from the palate, the CTG was placed on the saline soaked gauze while the palatal wound was closed. Horizontal crossed/parallel suspension silk sutures were used to simultaneously approximate both the flap margins and the entirely undermined donor area.
Figure 6.
Connective tissue graft harvesting from palate
Smearing of platelet-rich plasma to the connective tissue graft
After the required amount of connective tissue graft (CTG) was harvested, the tissue was coated with PRP to allow the growth factors impregnate the CTG. However, before securing the PRP impregnated CTG, PRP is also applied to the exposed and prepared root surfaces [Figure 7].
Figure 7.
Platelet-rich plasma applied to prepared root surface
Placement of connective tissue graft with platelet-rich plasma on the recipient bed
CTG with PRP was secured in position to cover the defect 3 mm apically over the adjacent alveolar crest and 1mm coronal to the CEJ and then sutured with 5–0 vicryl sutures [Figure 8]. Then the overlying full-partial thickness flap was positioned over the CTG with very little tension using sling, suspensory sutures into the mesial and distal papillae, covering as much of the CTG as possible [Figure 9].
Figure 8.

Connective tissue graft sutured
Figure 9.

Flap sutured
Periodontal dressings Coe-Pak™ (Coe Laboratories, Alsip, IL, USA) were placed on recipient and donor sites. Postoperative antibiotics, analgesics and mouthwash were prescribed, postoperative instructions were given and were recalled after 9 days for suture removal.
Postsurgical procedure
On 10th day following surgery, the periodontal dressing and sutures were removed, and the area was thoroughly irrigated with saline. Any signs of swelling, infection, flap displacement, hematoma and necrosis were noted. Symptoms regarding discomfort, pain and sensitivity were asked to the patient. Recall appointments were made after 1-month, 3 months, 6 months and 1-year postsurgery [Figures 10 and 11] and at each visit, oral hygiene instructions were reinforced and scaling was done whenever necessary. Patients were advised for chlorhexidine mouth rinse twice daily for another 3 weeks.
Figure 10.

Six month's postoperative photograph
Figure 11.

one year postoperative photograph with occlusal stent
Case 2
Pre-operative and Post-operative photographs of case 2 showing complete root coverage [Figures 12–15].
Figure 12.

Case - 2, preoperative photographs
Figure 15.

Case - 2, 1 year postoperative photograph with occlusal stent
Figure 13.
Case - 2, Preoperative photograph with occlusal stent
Figure 14.

Case - 2, 1 year postoperative photograph
Results
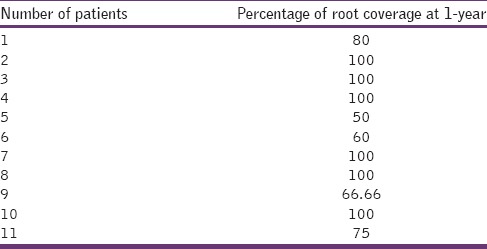
All 11 patients between 20 and 40 years of age (mean age 29) completed the study. Surgical sites healed uneventfully. No cases of graft necrosis or infection were detected. Clinical evaluation of postsurgical healing revealed an excellent root coverage with no adverse complications. The results of all clinical parameters obtained in the patients were summarized in Table 1. Percentage of root coverage of all patients at the end of 1-year is summarized in Table 2.
Table 1.
Clinical parameters
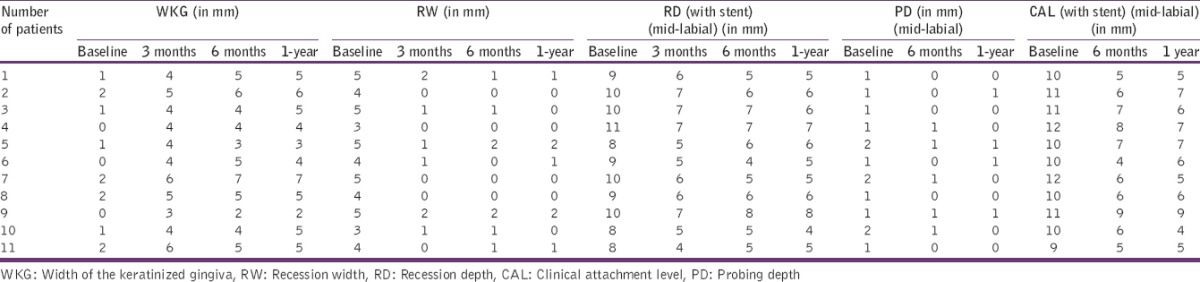
Table 2.
Percentage of root coverage at 1-year
Statistical analysis
The significance of changes in clinical parameters during the follow-up period was tested by repeated measures ANOVA test. P < 0.05 was considered as statistically significant.
Clinical parameters
Overall findings at baseline, 3, 6 and 12 months postsurgery showed that favorable results were obtained using SCTG along with PRP in the treatment of Miller's class I and class II gingival recessions. Mean and standard deviation of baseline, 3, 6, and 12 months postoperative of all the clinical parameters (n = 11 sites) were summarized in Table 3.
Table 3.
Statistical analysis of all the clinical parameters
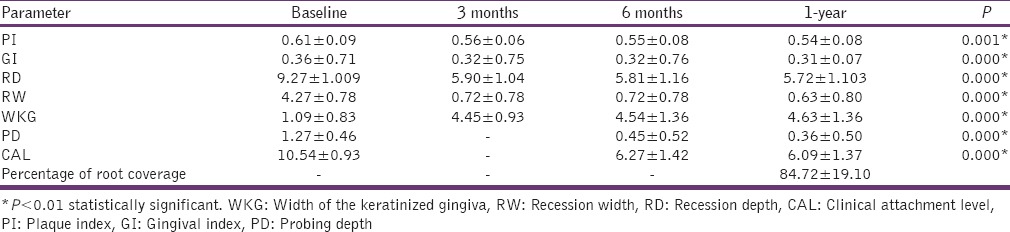
Plaque index and gingival index
The decrease in the mean PI and mean gingival index from baseline to 12 months was statistically highly significant (P < 0.05).
Recession depth (with stent) - mid facial
The mean RD (reduced from baseline value of 9.27 ± 1.009–5.90 ± 1.04, 5.81 ± 1.16 and 5.72 ± 1.103 at the end of 3, 6 and 12 months postoperatively, which was statistically highly significant (P < 0.05).
Recession width
The mean RW reduced from baseline value of 4.27 ± 0.78–0.72 ± 0.78, 0.72 ± 0.78 and 0.63 ± 0.80 at the end of 3, 6 and 12 months postoperatively and was found to be statistically highly significant (P < 0.05).
Width of keratinized gingiva
The mean gain in width of keratinized gingiva was 45 ± 0.93, 4.54 ± 1.36 and 4.63 ± 1.36 at the end of 3, 6 and 12 months postoperatively and was found to be statistically highly significant (P < 0.05).
Probing pocket depth and clinical attachment level (with stent) - midfacial
Mean probing depth was decreased to 0.45 ± 0.52 and 0.36 ± 0.50 at the end of 3 and 6 months and mean CAL was reduced to 6.27 ± 1.42 and 6.09 ± 1.37 at the end of 3 and 6 months postoperatively. Both the clinical parameters showed a statistically highly significant reduction (P < 0.05).
Percentage of root coverage
The mean percentage of root coverage at the end of 1-year was found to be 84.72 ± 19.10.
Discussion
Successful coverage of exposed roots for esthetic and functional reasons has been the objective of various mucogingival procedures. This generates a need for the clinician to develop newer techniques to fulfill these requirements without compromising esthetics and comfort.[4]
Root preparation before root coverage procedure can be mechanical, chemical, or a combination of both. Chemical biomodification of the root has centered on acid therapy, supposedly to demineralize a hypermineralized root. In the present study, root preparation included scaling and root planing, and tetracycline root conditioning (100 mg/ml) to enhance new attachment to the root surface and provide antimicrobial activity. In one of the clinical study, root coverage procedure using the SCTG was attempted after treating the root surfaces with Tetracycline HCI (125 mg/ml) and obtained higher (96.2%) mean root coverage.[17]
There are several techniques available to obtain a suitable SCTG. As advocated in different techniques, patient's palatal mucosa served as a source of CTG in the present study. Bruno's technique with two incisions was used because this technique provides better visibility and less postoperative pain and discomfort.[16]
The predictability of the SCTG procedure is excellent. The main advantages of this procedure are: (1) It provides a good blood supply to the graft and, therefore, has a very good predictability of success, (2) It provides gingival color match and esthetics, (3) The donor site wound is less extensive and hemorrhagic and perhaps less uncomfortable to the patient, (4) It is applicable to both single and multiple recessions. However the disadvantages of this technique include: (a) It is technically demanding and (b) It is more time-consuming.
The platelet-rich plasma is an enhanced concentration of platelets processed from the autologous blood. In vitro studies have demonstrated that PRP affects cell biologic activities on both genetic and cellular levels.[18] Recent evidence suggests that the fibrin clot derived from PRP was able to stimulate type I collagen synthesis.[19] Since PRP has a-higher number of platelets per milliliter, it is expected that it contains a higher concentration of growth factors to accelerate or enhance the periodontal regeneration.
In the present study, PRP was prepared 1 h prior to surgery, and when the platelet count was randomly checked, the number of platelets were 4 times greater than the baseline value of 1.5 lakh/μl. This was similar to the value obtained by Marx who has shown that this concentration was enough to produce clinical benefits.[5]
The mean plaque and gingival score showed a decline when baseline plaque and gingival scores were compared with that of 3 months, 6 months and 1-year postoperative values. A mean reduction of plaque and a gingival score of 0.06 ± 0.03 and 0.04 ± 0.03 was noted at the end of 1-year compared to baseline values. The mean reduction in RW, RD and CAL at the end of 1-year was found to be 3.63 ± 0.80, 3.54 ± 0.93 and 4.45 ± 1.36 respectively compared to baseline values. The mean gain in the width of keratinized gingiva was 3.54 ± 0.93 at the end of 1-year compared to baseline values. All the clinical parameters have shown highly statistically significant improvement when compared to baseline values. The root coverage obtained with this procedure improved the esthetics and met the expectations and demands of the patient. The grafted sites were followed up for a period of 1-year in order: (i) To verify the true effectiveness of the two grafting procedures in terms of root coverage. (ii) To observe and compare the stabilization of results obtained with both the experimental procedures.
There are isolated case reports[8,20] and clinical studies[21] wherein PRP was used along with CTG for the treatment of gingival recession defects. In other studies, a collagen sponge was soaked with platelet concentrate in the treatment of recession defects.[22,23] The results in all the studies were encouraging. However, no long-term clinical trials have been reported in the literature using PRP smeared over CTG in the treatment of gingival recession.
Conclusion
The favorable results obtained with SCTG + PRP combination in improving the clinical parameters and getting significant root coverage can be attributed to: (1) PRP delivers growth factors to enhance the soft tissue healing and maturation rate, (2) It promotes more rapid revascularization rate of the grafted connective tissue, (3) The cohesive properties of PRP which can be compared to a growth-factor impregnated fibrin glue, act to stabilize the graft and (4) Along with proper suturing methods, it minimizes the potential of micromovement of the graft during wound healing.
No postoperative complications other than those considered normal, following any surgical procedure either at the recipient or donor site were noticed. In the present study, during 1-week postoperative examination, the gingival appearance was evaluated by examining for erythema and edema. In all cases, the gingival appearance was nearly normal with appearance varying between “no gingival erythema or edema to a slight erythema and edema.” Patient discomfort was present only on the 1st day and with very minimal postoperative pain. This shows an accelerated soft-tissue healing. Furthermore, no antigenic reactions were observed in any of the patients thereby, indicating the safety autogenous PRP and the human thrombin used for activation of PRP. Hence, the advent and use of PRP in combination with SCTG represents a novel approach in the mucogingival therapy.
Financial support and sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
References
- 1.Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc. 2003;134:220–5. doi: 10.14219/jada.archive.2003.0137. [DOI] [PubMed] [Google Scholar]
- 2.Novaes AB, Ruben MP, Kon S, Goldman HM, Novaes AB., Jr The development of the periodontal cleft. A clinical and histopathologic study. J Periodontol. 1975;46:701–9. doi: 10.1902/jop.1975.46.12.701. [DOI] [PubMed] [Google Scholar]
- 3.Maynard JG. The rationale for mucogingival therapy in the child and adolescent. Int J Periodontics Restorative Dent. 1987;7:36–51. [PubMed] [Google Scholar]
- 4.Edel A. Clinical evaluation of free connective tissue grafts used to increase the width of keratinised gingiva. J Clin Periodontol. 1974;1:185–96. doi: 10.1111/j.1600-051x.1974.tb01257.x. [DOI] [PubMed] [Google Scholar]
- 5.Marx RE. Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant Dent. 2001;10:225–8. doi: 10.1097/00008505-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Lynch SE. The role of growth factors in periodontal repair and regeneration. In: Polson AM, editor. Periodontal Regeneration: Current Status and Directions. St Louis: Quintessence Publishing Co, Inc; 1994. pp. 179–98. [Google Scholar]
- 7.Pierce GF, Mustoe TA, Altrock BW, Deuel TF, Thomason A. Role of platelet-derived growth factor in wound healing. J Cell Biochem. 1991;45:319–26. doi: 10.1002/jcb.240450403. [DOI] [PubMed] [Google Scholar]
- 8.Petrungaro PS. Using platelet-rich plasma to accelerate soft tissue maturation in esthetic periodontal surgery. Compend Contin Educ Dent. 2001;22:729–32. [PubMed] [Google Scholar]
- 9.Silness J, Loe H. Periodontal disease in pregnancy. II. correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 10.Loe H, silness J. periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 11.Lynch SE. Methods for evaluation of regenerative procedures. J Periodontol. 1992;63:1085–92. doi: 10.1902/jop.1992.63.12s.1085. [DOI] [PubMed] [Google Scholar]
- 12.Clark DC, Chin Quee T, Bergeron MJ, Chan EC, Lautar-Lemay C, de Gruchy K. Reliability of attachment level measurements using the cementoenamel junction and a plastic stent. J Periodontol. 1987;58:115–8. doi: 10.1902/jop.1987.58.2.115. [DOI] [PubMed] [Google Scholar]
- 13.Shieh AT, Wang HL, O’Neal R, Glickman GN, MacNeil RL. Development and clinical evaluation of a root coverage procedure using a collagen barrier membrane. J Periodontol. 1997;68:770–8. doi: 10.1902/jop.1997.68.8.770. [DOI] [PubMed] [Google Scholar]
- 14.Tözüm TF, Demiralp B. Platelet-rich plasma: A promising innovation in dentistry. J Can Dent Assoc. 2003;69:664. [PubMed] [Google Scholar]
- 15.Weibrich G, Kleis WK. Curasan PRP kit vs. PCCS PRP system. Collection efficiency and platelet counts of two different methods for the preparation of platelet-rich plasma. Clin Oral Implants Res. 2002;13:437–43. doi: 10.1034/j.1600-0501.2002.130413.x. [DOI] [PubMed] [Google Scholar]
- 16.Bruno JF. Connective tissue graft technique assuring wide root coverage. Int J Periodontics Restorative Dent. 1994;14:126–37. [PubMed] [Google Scholar]
- 17.Harris RJ. A comparative study of root coverage obtained with an acellular dermal matrix versus a connective tissue graft: Results of 107 recession defects in 50 consecutively treated patients. Int J Periodontics Restorative Dent. 2000;20:51–9. [PubMed] [Google Scholar]
- 18.Oates TW, Kose KN, Xie JF, Graves DT, Collins JM, Cochran DL. Receptor binding of PDGF-AA and PDGF-BB, and the modulation of PDGF receptors by TGF-beta, in human periodontal ligament cells. J Cell Physiol. 1995;162:359–66. doi: 10.1002/jcp.1041620308. [DOI] [PubMed] [Google Scholar]
- 19.Okuda K, Kawase T, Momose M, Murata M, Saito Y, Suzuki H, et al. Platelet-rich plasma contains high levels of platelet-derived growth factor and transforming growth factor-beta and modulates the proliferation of periodontally related cells in vitro. J Periodontol. 2003;74:849–57. doi: 10.1902/jop.2003.74.6.849. [DOI] [PubMed] [Google Scholar]
- 20.Kumar A, Triveni MG, Mehta DS. Subepithelial connective tissue graft used with platelet-rich plasma in treatment of gingival recession. Dent Update. 2012;39:218–20. doi: 10.12968/denu.2012.39.3.218. [DOI] [PubMed] [Google Scholar]
- 21.Cheung WS, Griffin TJ. A comparative study of root coverage with connective tissue and platelet concentrate grafts: 8-month results. J Periodontol. 2004;75:1678–87. doi: 10.1902/jop.2004.75.12.1678. [DOI] [PubMed] [Google Scholar]
- 22.Griffin TJ, Cheung WS. Treatment of gingival recession with a platelet concentrate graft: A report of two cases. Int J Periodontics Restorative Dent. 2004;24:589–95. [PubMed] [Google Scholar]
- 23.Chinnappa AB, Dwarkanath CD, Naik AR, Naik MS, Ramesh AV. Use of autologous platelet rich plasma to treat gingival recession in esthetic periodontal surgery. J Indian Soc Periodontol. 2013;17:345–53. doi: 10.4103/0972-124X.115665. [DOI] [PMC free article] [PubMed] [Google Scholar]


