Abstract
It is universally accepted that correction of cleft lip nose deformity remains a formidable challenge for any cleft surgeon. The nose is a prominent part of the face, and hence a masterly executed cleft lip repair directs the beholders’ eyes from the deformed lip to the deformed nose. A deformed nose that results from unilateral cleft of the lip and palate is likened to a tent whose one side is depressed. Many investigators believe that the deformity of the nose is produced by the malpositioning of essentially normal structures, on the other hand some cleft surgeons contend that it is the intrinsic defects in nasal structures that result in cleft nasal deformity. Depressed and hypoplastic bony scaffolding is the most important aspect of cleft nose deformity and addressing this aspect of cleft nose deformity is the secret of success of a perfect secondary rhinoplasty. Controversy still exists on timing of cleft nasal deformity. Proponents of delayed nasal repair suggest that altering the cartilages in early nasal repair at the time of lip repair would complicate future corrective nasal surgeries if the primary repair would prove unsatisfactory. The correction of nasal deformity could be performed with closed or open technique. This paper highlights one such challenging unilateral cleft lip nasal deformity in a adult patient treated by secondary rhinoplasty by open technique.
KEY WORDS: Cartilages, cleft lip, cleft nose, open rhinoplasty, secondary rhinoplasty
Nasal deformity correction in cleft lip patients remains a challenging problem. Cleft lip nasal deformity is a complex three-dimensional deformity involving skin, cartilage, vestibular lining and skeletal platform. The primary deformity is an imbalance between abnormal muscle insertion and maxillary skeletal hypoplasia.[1]
Controversies exist on the timing of rhinoplasty in cleft lip patients and is categorized as primary rhinoplasty performed at the time of cleft lip repair, intermediate rhinoplasty at the age of 5–11 years and definitive rhinoplasty.[2] The general characteristics of the nasal deformity in cleft lip patients are a very short columella, downward tip rotation and diminished nasal projection.
The objectives of a rhinoplasty are positioning of lower lateral cartilage to a more normal anatomic position, achieving a symmetric projection of both alar domes, elongation of columella when deemed necessary, moving the cleft alar base more medially to achieve nasal floor symmetry and to provide a structural support by means of bone or cartilage grafts.[3]
The surgical approaches for a cleft lip rhinoplasty can be a closed endonasal or an open approach.[4] The open or external approach is indicated in cases where there is a severe deformity of the nasal tip.
A case of unilateral cleft nasal deformity where a definitive rhinoplasty was done through an open approach has been discussed.
Case Report
A 26-year-old female was referred to our department of oral and maxillofacial surgery with a chief complaint of deviated nose and smaller nostril on the right side. Past surgical history revealed that she had undergone cleft lip repair at the age of 3 years.
Extra oral examination findings were nasal pyramid was tilted to the cleft side, the columella was short on the cleft side and deviated towards the noncleft side, the lateral crux of the lower lateral cartilage was displaced lower and to the cleft side resulting in excessive skin on the dome of lower lateral cartilage on the cleft side, nasal tip was asymmetrical, nostril on the cleft side was small and the entire nostril was retropositioned [Figure 1a–c].
Figure 1.

(a) Patients preoperative profile view. (b) Cleft nasal deformity of the patient. (c) Schematic representation of cleft nasal deformity. Columella short on the cleft side and deviated towards the noncleft side; the lateral crux of the lower lateral cartilage was displaced lower and to the cleft side
Intraoral examination revealed a class I molar relation on the right and left the side with generalized spacing of upper and lower anteriors and a missing left upper lateral incisor with an alveolar cleft [Figure 2].
Figure 2.

Class I occlusion on both sides with alveolar cleft. (Lateral incisor absent)
A definitive open rhinoplasty was planned for the cleft nasal deformity. The surgery was carried out under general anesthesia through orotracheal intubation. An inverted-V transcolumellar incision with bilateral marginal incisions was made, the lower lateral cartilage and septal cartilage were exposed [Figure 3a], the cartilaginous septum was separated from the maxillary crest and secured to the midline using 5–0 PDS suture, deviated portions of the septum were then removed and the excess cartilage is preserved for graft in future use [Figure 3b], while preserving an adequate dorsal and caudal strut. The tip projection and symmetry was increased with a strut graft in the columella in a pocket between medial crura, medial advancement of lower lateral cartilage was done [Figure 4]. Alar hooding was improved and alar collapse was prevented by placing a spreader graft [Figure 5].
Figure 3.
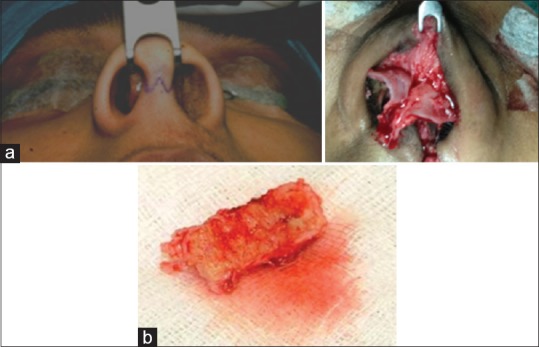
(a) Inverted-V transcolumellar inscision with marginal extention. Exposure of nasal septum and lower lateral cartilatge. Septum mobilized from nasal crest. (b) Harvested excess septal cartilage
Figure 4.

Columellar strut graft to support the columella
Figure 5.

Spreader graft is placed to prevent alar collapse
Postoperatively the healing was satisfactory with no evidence of infection or wound dehiscence. The symmetry of the nasal tip was achieved, nostril on the cleft side was of the same size as the noncleft side, there was good projection of the nasal dorsum and nasal tip postoperatively [Figure 6]. The results were stable with no evidence of relapse with a period of follow-up of 1-year.
Figure 6.

Three months postoperative photograph frontal view
Discussion
Unilateral cleft lip nasal deformity is the result of undue forces to which the nasal tip is subjected as a consequence of uncoupling of the palatal shelves.[5] The alar cartilage is splayed apart and rotated caudally as a bucket handle. The drawbacks of primary rhinoplasty are relapse and growth impairment, however the studies by Mccomb and Salyer[6,7] stated that nasal cartilage growth is unaffected by nasal surgery but in our case a definitive rhinoplasty was done. The goals of definitive rhinoplasty include creation of symmetry, definition of nasal base and tip, relief of nasal obstruction and management of nasal scarring and webbing.[8]
One of the cleft lip nasal deformities is the alar columellar web deformity in which excess skin overhangs the superomedial side of the nostril. Tajima and Maruyama described a reverse U incision with a suture suspension of repositioned cleft lower lateral cartilage.[9] Nakajima et al. modified the technique by adding a Z-plasty in the lateral nasal vestibule.[10] Cronin and Denkler reported on V-Yplasty of nasal mucosa left by the advancement of the lateral crus.[11] They proposed that the vestibular lining of the lateral crus remain attached to add circulation and support especially when scoring of the cartilage is needed. Maeda et al. reported using a bilateral reverse U incision in combination with Cronins method.[12] Nakajima and Yoshimura used a bilateral reverse U incision combined with a short banked forked flap in bilateral cleft lip nasal deformity.[13] A traditional inverted-V transcolumellar incision advocated by Potter and Merville and popularized by Goodman[14] was used in this case and there was good visibility and access to the displaced structures with this incision.
Some stress the need for lateral to medial advancement and lateral release of the lateral crus,[15] others prefer a medial to lateral rotation,[16] however, only a few use total detachment of the lateral crus from the vestibular skin.[17] Some surgeons mobilize the lateral crus together with vestibular skin to create a medially based chondrocutaneous flap.[14,15] A lateral to medial advancement was preferred in our case.
Different techniques are described to repair the lateral vestibular wall following medial advancement of the crus. Tajima and Maruyama state that there is no redundant skin[9] whereas Gubisch uses a surplus of vestibular skin to close a gap between two flaps at the lateral nostril.[18] Millard excises not only part of the lateral crus but also the skin excess from the vestibular fold.[19] Most authors report a defect in the lateral wall and suggest direct approximation or standard flaps such as Z-plasty or V-Y advancement.[20]
Ayhan et al. published a series of cases where composite conchal cartilage was used in various forms to repair columellar deficit, to form nasal tubercle and nostril sill in cleft lip nasal deformity patients and concluded that conchal cartilage achieved symmetric and functional results.[21] Turkaslan et al. described a technique to place a cartilage graft at the posterior dome area after the release of cleft side ala from vestibular mucosa and skin to elevate the ala depression and tip projection.[22] Septal cartilage was used in presented case and was satisfactory and a second donor site morbidity was avoided.
Flores published a retrospective review where a combination of Dibbell and Tajima was used and concluded that there was a statistically significant decrease in alar base width, increase in columellar height and nostril height on the affected side.[23] Similar results were achieved in our case.
There are very few studies to assess the outcomes of cleft lip rhinoplasty in terms of patients’ satisfaction. Huempfner-Hierl et al. evaluated esthetic and respiratory outcome with active change in nasal airflow and hydraulic diameter could be found and hence stated that while esthetic improvement of the cleft nose is a goal, which can be achieved in regularity nasal respiration still seems to be a challenge in cleft patients.[24] Analysis of respiratory outcome was not done in the case presented though the patient was satisfactory about the aesthetic result.
Sandor and Ylikontiola in their study on 35 patients with cleft nasal deformity treated by external rhinoplasty evaluated for satisfaction and perception of outcomes.[25] The highest improvement was seen for the tip, followed by alar position, dorsum and symmetry of nostrils. Leipzig in a similar study described high satisfaction rates by patients undergoing surgery for cleft nasal deformities.[26]
Conclusion
The cleft lip nasal deformity will continue to remain a challenge to the surgeons. Correction of the deformity requires a thorough and in detail understanding of the anatomy of cleft pathology and accurate assessment of both esthetic and functional impairments. An individualized treatment plan is needed taking into consideration the above mentioned factors. Open external approach rhinoplasty allows maximum exposure for structural graft placement to improve tip projection, definition, support, and function.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Sykes JM, Senders CW. Pathologic anatomy of cleft lip, palate and nasal deformities. In: Meyers AD, editor. Biological Basis of Facial Plastic Surgery. New York: Thieme Medical Publishers; 1993. pp. 57–71. [Google Scholar]
- 2.Sykes JM, Senders CW. Surgical treatment of the unilateral cleft nasal deformity at the time of lip repair. Facial Plast Surg Clin North Am. 1995;3:69–77. [Google Scholar]
- 3.Ortiz-Monasterio F, Rua EJ. Cleft lip rhinoplasty: The role of bone and cartilage grafts. Clin Plast Surg. 1989;16:177–86. [PubMed] [Google Scholar]
- 4.McComb H. Treatment of the unilateral cleft lip nose. Plast Reconstr Surg. 1975;55:596–601. doi: 10.1097/00006534-197505000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Blair V. Nasal deformities associated with congenital cleft of the lip. J Am Med Assoc. 1925;84:185. [Google Scholar]
- 6.McComb H. Primary correction of unilateral cleft lip nasal deformity: A 10-year review. Plast Reconstr Surg. 1985;75:791–9. doi: 10.1097/00006534-198506000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Salyer KE. Primary correction of the unilateral cleft lip nose: A 15-year experience. Plast Reconstr Surg. 1986;77:558–68. doi: 10.1097/00006534-198604000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Gillies H, Millard DR. The Principles and Art of Plastic Surgery. Boston, Mass: Little Brown and Co; 1966. pp. 320–37. [Google Scholar]
- 9.Tajima S, Maruyama M. Reverse-U incision for secondary repair of cleft lip nose. Plast Reconstr Surg. 1977;60:256–61. doi: 10.1097/00006534-197708000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Nakajima T, Yoshimura Y, Kami T. Refinement of the “reverse-U” incision for the repair of cleft lip nose deformity. Br J Plast Surg. 1986;39:345–51. doi: 10.1016/0007-1226(86)90045-7. [DOI] [PubMed] [Google Scholar]
- 11.Cronin TD, Denkler KA. Correction of the unilateral cleft lip nose. Plast Reconstr Surg. 1988;82:419–32. doi: 10.1097/00006534-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Maeda K, Ojimi H, Yoshida T. A new method of secondary correction of the bilateral cleft lip nose. Br J Plast Surg. 1987;40:52–60. doi: 10.1016/0007-1226(87)90011-7. [DOI] [PubMed] [Google Scholar]
- 13.Nakajima T, Yoshimura Y. Secondary repair of unilateral cleft lip nose deformity with bilateral reverse-U access incision. Br J Plast Surg. 1998;51:176–80. doi: 10.1054/bjps.1997.0071. [DOI] [PubMed] [Google Scholar]
- 14.Potter J. Some nasal tip deformities due to alar cartilage abnormalities. Plast Reconstr Surg (1946) 1954;13:358–66. doi: 10.1097/00006534-195405000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Rees TD, Guy CL, Converse JM. Repair of the cleft lip-nose: Addendum to the synchronous technique with full-thickness skin grafting of the nasal vestibule. Plast Reconstr Surg. 1966;37:47–50. [PubMed] [Google Scholar]
- 16.Dibbell DG. Cleft lip nasal reconstruction: Correcting the classic unilateral defect. Plast Reconstr Surg. 1982;69:264–71. doi: 10.1097/00006534-198202000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Farrior RT. The problem of the unilateral cleft-lip nose. A composite operation for revision of the secondary deformity. Laryngoscope. 1962;72:289–352. doi: 10.1288/00005537-196203000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Gubisch W. How to obtain symmetry in a unilaterally cleft nose. Eur J Plast Surg. 1982;2:264–70. [Google Scholar]
- 19.Millard DR., Jr Earlier correction of the unilateral cleft lip nose. Plast Reconstr Surg. 1982;70:64–73. doi: 10.1097/00006534-198207000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Koopmann CF, Jr, Krause CJ. Secondary cleft lip rhinoplasty: An external approach. Facial Plast Surg. 1988;5:167–77. doi: 10.1055/s-2008-1064748. [DOI] [PubMed] [Google Scholar]
- 21.Ayhan M, Gorgu M, Erdogan B, Aytug Z, Aksungur E, Sýlýstrelý O, et al. Various applications of chondrocutaneous composite grafts in secondary cleft lip nose patients. J Craniofac Surg. 2006;17:1065–71. doi: 10.1097/01.scs.0000231628.10511.bb. [DOI] [PubMed] [Google Scholar]
- 22.Turkaslan T, Turan A, Yogun N, Ozsoy Z. A novel approach to cleft lip nose deformity: Posterior dome graft technique. J Craniofac Surg. 2008;19:1359–63. doi: 10.1097/SCS.0b013e3181849d9a. [DOI] [PubMed] [Google Scholar]
- 23.Flores RL, Sailon AM, Cutting CB. A novel cleft rhinoplasty procedure combining an open rhinoplasty with the Dibbell and Tajima techniques: A 10-year review. Plast Reconstr Surg. 2009;124:2041–7. doi: 10.1097/PRS.0b013e3181bcf100. [DOI] [PubMed] [Google Scholar]
- 24.Huempfner-Hierl H, Hemprich A, Hierl T. Results of a prospective anthropometric and functional study about aaesthetics and nasal respiration after secondary rhinoplasty in cleft lip and palate patients. J Craniofac Surg. 2009;20(Suppl 2):1863–75. doi: 10.1097/SCS.0b013e3181b6c6fb. [DOI] [PubMed] [Google Scholar]
- 25.Sandor GK, Ylikontiola LP. Patient evaluation of outcomes of external rhinoplasty for unilateral cleft lip and palate. Int J Oral Maxillofac Surg. 2006;35:407–11. doi: 10.1016/j.ijom.2006.01.020. [DOI] [PubMed] [Google Scholar]
- 26.Pitak-Arnnop P, Hemprich A, Dhanuthai K, Pausch NC. Outcome research on secondary cleft rhinoplasty: The Leipzig experience. J Plast Reconstr Aesthetic Surg. 2011;64:277–8. doi: 10.1016/j.bjps.2010.06.015. [DOI] [PubMed] [Google Scholar]


